Abstract
Obesity is a global epidemic with substantial health and economic impacts, making scalable weight management strategies essential. A comprehensive synthesis of eHealth interventions for weight management is needed to guide clinical practice. This umbrella review evaluated mobile and web-based interventions for weight loss in adults with overweight or obesity, compared to conventional or non-intervention controls. Systematic reviews were identified across five electronic databases from inception to February 2025. Two reviewers independently selected studies and assessed methodological quality using AMSTAR 2. Pooled estimates were calculated using random-effects models. Eleven systematic reviews (261 primary studies, 62,407 participants) were included. Mobile app interventions yielded a significant reduction in body weight (MD = −1.32 kg; I2 = 82%), as did long-term eHealth interventions (MD = −1.13 kg; I2 = 76%). Most meta-analyses showed high heterogeneity. Web-based interventions showed no significant effect. In conclusion, mobile apps and long-term eHealth interventions resulted in modest but statistically significant reductions in body weight, body mass index, and waist circumference. The evidence for web-based approaches remains inconclusive. Further research should focus on low-resource settings, primary care, and the integration of emerging technologies such as artificial intelligence. (PROSPERO CRD42025644218).
1. Introduction
Obesity and overweight are highly prevalent conditions that have reached epidemic proportions. In 2020, 2.2 billion adults were affected by overweight or obesity, with projections reaching 2.5 billion by 2025 and 3.3 billion by 2030 [1]. Overweight and obesity are significant risk factors for a wide range of noncommunicable diseases (NCDs), including cardiovascular disease, dyslipidemia, type 2 diabetes, certain cancers, and musculoskeletal and respiratory disorders [1]. Apart from its physical health consequences, obesity is closely linked to psychological disorders such as depression, anxiety, and eating disorders, significantly impacting the quality of life and life expectancy of these individuals [2,3].
These projections follow a concerning historical trend, with a significant increase in global deaths linked to high body mass index (BMI), which rose from 1.46 million in 1990 to 3.79 million in 2021 (a 153.97% increase). Similarly, Disability-Adjusted Life Years (DALYs) rose from 48.04 million to 128.52 million over the same period (a 167.57% increase) [4]. This burden has also translated into substantial economic costs. The World Obesity Federation (2024) projects an annual impact of USD 4.32 trillion by 2035, representing almost 3% of the global GDP [2]. For instance, Rocha et al. (2024) [5] reported that the Brazilian Health System (Sistema Único de Saúde [SUS]) spent USD 377.30 million on hospitalizations and high- and medium-complexity procedures to control NCDs attributable to high BMI in Brazil.
In response to this challenge, researchers and public health bodies have championed digital health technologies as scalable and promising strategies for weight management. The widespread use of smartphones and wearable devices has enabled mobile applications that support self-monitoring, behavior change, and personalized feedback [6,7]. Many of these tools incorporate behavioral models such as the Information-Motivation-Behavioral Skills (IMB) model to improve user adherence [8]. Despite these advantages, the evidence remains inconsistent regarding the effectiveness of digital interventions compared to conventional treatments (those without digital technologies) or no intervention [9,10]. Furthermore, as the COVID-19 pandemic significantly accelerated digital health adoption, much of the existing evidence predates this pivotal shift [11]. While telehealth has expanded rapidly, challenges such as limited access, digital literacy, and long-term adherence persist [11,12,13].
To establish a clear conceptual framework, this review adopts the following terminology based on established definitions in the literature. Digital health is used as the broadest term, encompassing all applications of information and communication technologies in the health domain. A major subfield within this is electronic health (eHealth), which refers more specifically to the use of the internet and related technologies to deliver health information and services. Within the scope of this review, we analyze two primary modalities of eHealth: mobile health (mHealth), which involves interventions delivered specifically via mobile devices such as smartphones and tablets (e.g., applications, SMS messages), and web-based interventions, which are primarily delivered through websites. Figure 1 illustrates this hierarchical relationship. Throughout this paper, we use eHealth as a general term when discussing interventions collectively, and specify ‘mHealth’ or ‘web-based’ when referring to findings from these distinct modalities.
Figure 1.
Conceptual framework of digital health terminology used in this review. The diagram illustrates the hierarchical relationship between digital health as the overarching field, eHealth as a major subfield, and mHealth and web-based interventions as the primary eHealth modalities analyzed.
In the primary healthcare (PHC) context, digital health interventions, particularly mobile and web-based applications, hold significant promise. They offer accessible, scalable, and cost-effective solutions for weight management, potentially complementing traditional strategies used in the PHC context. Given the critical role of PHC in addressing obesity through preventive care and health promotion, robust evaluation of digital interventions is essential to inform international evidence-based practices and policies in diverse healthcare settings. Moreover, as Senbekov et al. (2020) [12] reported, digital health innovations require rigorous validation, especially in the absence of formal regulation.
Given this context, this study aims to synthesize and critically appraise the evidence on the effectiveness of mobile applications and web-based interventions for weight loss in overweight and obese adults, compared to conventional treatments without digital technologies or no intervention. Our findings suggest that mobile app and long-term eHealth interventions are effective for weight management in overweight and obese adults, while the effectiveness of web-based interventions remains inconclusive. Further research is needed in primary care and low-resource settings.
2. Materials and Methods
This umbrella review of systematic reviews adopted a meta-review strategy to evaluate the effectiveness of eHealth interventions, specifically mobile applications and web-based programs for weight loss in overweight and obese adults. In this study, eHealth interventions were defined as both mobile health (mHealth) applications (e.g., smartphone apps) and web-based programs, which were analyzed together when appropriate and separately in relevant subgroup analyses. This approach was chosen due to the multifactorial complexity of overweight and obesity and the need to consolidate dispersed and heterogeneous evidence, especially considering the lack of synthesis of post-COVID-19 studies.
The reporting of this meta-review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [14] (Table S1) and was prospectively registered on PROSPERO (Centre for Reviews and Dissemination, University of York, York, UK) under the registration number CRD42025644218.
2.1. Eligibility Criteria
The review question was defined according to the PICOS framework:
- Population: Adults (≥18 years) diagnosed with overweight or obesity (BMI ≥ 25).
- Intervention: Use of mobile or web-based applications specifically designed as strategies for weight loss.
- Comparator: Conventional treatment for overweight or obesity, including diet, exercise, behavioral therapy, pharmacological interventions, or minimal/no intervention, excluding digital technologies. Pharmacological interventions were considered an acceptable component of conventional treatment for comparator groups, as information about their use tends to be underreported or insufficiently detailed in systematic reviews. This a priori criterion was set to prevent the exclusion of potentially relevant reviews.
- Outcomes: At least one of the following: reduction in BMI, waist circumference, body fat percentage, or overall weight loss.
- Study design: Systematic reviews with meta-analyses, available in full text, assessing the effectiveness of mobile applications and web-based interventions compared to conventional treatments in adults with overweight or obesity. Systematic reviews including the general population were eligible if they performed separate analyses for adults and children. Exclusion criteria comprised clinical trials, abstracts, opinion pieces, narrative (non-systematic) reviews, and scoping reviews. No restrictions were applied regarding language or publication year at any stage of the search or screening process. However, all systematic reviews included in this umbrella review were published in English, and no potentially eligible reviews in other languages were retrieved. This a priori approach aligns with best practices for umbrella reviews and maximizes the comprehensiveness and temporal scope of the evidence, which is crucial in the rapidly evolving field of digital health.
Studies evaluating telemedicine interventions not involving mobile or web applications specifically designed for obesity management, interventions targeting conditions other than overweight/obesity, artificial intelligence-based apps or chatbots, and wearable device-based interventions (e.g., fitness trackers, smartwatches) were excluded.
2.2. Information Sources and Search Strategy
We performed electronic searches between 30 January and 7 February 2025, in five databases: Cochrane Library, Virtual Health Library, PubMed/MEDLINE, ScienceDirect, and Web of Science.
We developed the search strategy based on the PICOS framework using a combination of keywords derived from MeSH® (Medical Subject Headings, National Library of Medicine, Bethesda, MD, USA) and DeCS® (Health Sciences Descriptors, BIREME, São Paulo, Brazil). However, searches were conducted using free-text terms in all databases. The terms were related to three key concepts: the population (“overweight”, “obesity”, “body weight”); the intervention (“mobile application”, “web-based intervention”, “mHealth”, “digital health”, “telehealth”); and the outcomes (“weight loss”, “body mass index”, “waist circumference”, “body fat”). Boolean operators (“AND” and “OR”) were used to combine these concepts and maximize search sensitivity.
As described above, no lower year limit was applied; all systematic reviews available in each database up to February 2025 were eligible for inclusion. Where possible, searches were limited to title and abstract fields, and publication type filters were applied to identify systematic reviews or meta-analyses.
The complete search strategy for each database is provided in File S1.
2.3. Study Selection and Data Extraction
All search results were exported and imported into the Rayyan platform (Qatar Computing Research Institute, Doha, Qatar) for screening. Rayyan’s automated tool was used to identify and remove duplicate records before title and abstract screening. Two independent reviewers (FFSC and CPBA) performed title/abstract and full-text screening. Disagreements were resolved through discussion to achieve consensus. Inter-rater agreement was assessed using Cohen’s Kappa coefficient, calculated in R (R Foundation for Statistical Computing, Vienna, Austria) (package ‘irr’). Reasons for full-text exclusion were documented and summarized. Final inclusion was determined by consensus following mutual review of extracted data (FFSC and CPBA).
2.4. Methodological Quality Assessment
The methodological quality of the included systematic reviews was assessed using the AMSTAR 2 tool [15], with both reviewers discussing and reaching a consensus on each assessment.
2.5. Assessment of Risk of Bias Across Studies
Publication bias was planned to be assessed in the included systematic reviews using funnel plot asymmetry and formal statistical tests (e.g., Egger’s or Begg’s test) when available. These assessments were extracted and summarized to evaluate the potential for cumulative reporting bias across studies.
2.6. Assessment of Overlap Among Primary Studies
To evaluate the degree of overlap among primary studies included in the systematic reviews, we constructed an overlap matrix and then calculated the Corrected Covered Area (CCA) according to the method proposed by Pieper et al. (2014) [16]. All lists of primary studies were standardized and merged, with duplicates removed to ensure an accurate count of unique studies.
2.7. Quantitative Synthesis and Subgroup Definitions
Meta-analyses were performed for all subgroups where clinical and methodological homogeneity allowed. Given the substantial heterogeneity in intervention types, comparators, outcomes, and study populations across the included systematic reviews, a single global meta-analysis pooling all interventions would not be methodologically appropriate. Instead, random-effects meta-analyses were conducted post hoc for clinically meaningful subgroups, including smartphone app interventions, web-based interventions (with and without human contact), and outcomes related to weight, BMI, waist circumference, and body fat percentage, as well as analyses stratified by intervention duration (short-term [≤6 months] and long-term [≥12 months]).
The principal summary measures were mean differences (MD) and standardized mean differences (SMD), both reported with 95% confidence intervals.
For each eligible meta-analysis, we systematically selected a single representative effect size to avoid double counting and ensure comparability. The following hierarchy of criteria was strictly applied in all cases:
- Effect size corresponding to the longest follow-up period was selected whenever available;
- If multiple effect sizes were available at the same follow-up, preference was given to estimates based on intention-to-treat (ITT) analysis;
- In case of further ties, the result with the largest sample size was chosen.
This approach was applied systematically across all included reviews and subgroups, ensuring methodological consistency and minimizing selection bias. Where at least two eligible effect sizes were available, quantitative synthesis was performed; single-study estimates were described narratively. All meta-analyses were conducted in R (version 4.4.3, R Foundation for Statistical Computing, Vienna, Austria) using the ‘meta’ package. Heterogeneity was assessed using the I2 statistic for each meta-analysis.
For each subgroup, effect sizes were filtered and harmonized using regular expressions and explicit inclusion/exclusion logic to match clinical definitions (e.g., excluding SMS/telephone from smartphone app analyses).
3. Results
3.1. Study Selection
We retrieved 281 records from five databases. After removing 58 confirmed duplicates, 223 unique records remained for title and abstract screening. Inter-rater agreement at this stage was substantial (κ = 0.805), with 195 records excluded and 28 full-text articles assessed for eligibility. The full-text review yielded almost perfect agreement between reviewers (κ = 0.928). The code used to assess inter-rater agreement is available in File S2.
After consensus, 12 systematic reviews were selected for data extraction. However, one study (Li et al., 2024) [17] was excluded due to the absence of reported primary study data. As this information was not apparent from the publication, the authors were contacted for clarification and confirmed that the paper was a conference abstract presenting only partial results, with no access to primary study data. Consequently, the final sample comprised 11 systematic reviews. Collectively, these reviews synthesized data from 261 primary studies, encompassing a total of 62,407 participants. The subsequent analyses on geographical distribution and income level are based on the subset of these studies for which country data were reported. The study selection process is summarized in Figure 2, and the reasons for full-text exclusions are listed in Table S2.
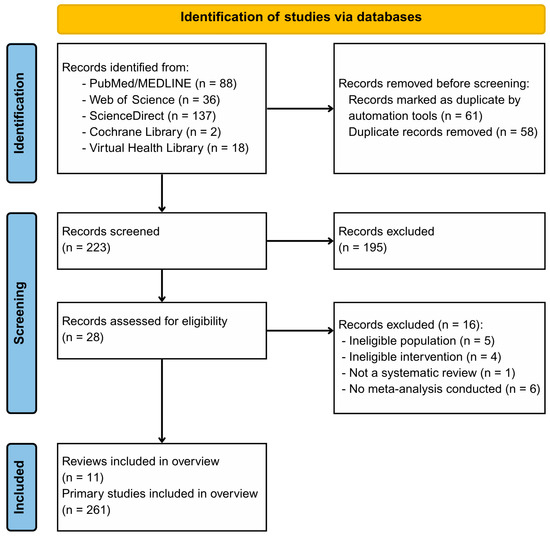
Figure 2.
PRISMA Flow diagram for identification of systematic reviews and primary studies. Note: One review was excluded post-screening, as it was identified as a conference abstract without primary study data, resulting in a final sample of 11 reviews.
3.2. Study Characteristics
The 11 systematic reviews [9,10,18,19,20,21,22,23,24,25,26], were published between 2010 and 2024 and covered a broad range of digital health interventions for weight management in adults with overweight or obesity. On average, each review included 23.7 primary studies (SD = 21.8, median = 18, range 6–84) and a mean sample size of 5673 participants (SD = 6159, median = 2630, range 632–24,010).
Most reviews focused on adults, although a minority also included individuals at risk for metabolic disease [18,23] or with prediabetes [25]. The most common interventions in the meta-analyses were mobile health (mHealth), such as smartphone apps, SMS, and wearables [10,18,19,20,22,23]. These were followed by web-based digital interventions [9,21,24,26] and a single mixed intervention including both web and mobile components [25]. In these studies, comparison groups most frequently received usual care, were placed on a wait-list, or had a minimal intervention. The intervention duration was typically short-term, with a median of 6 months (range 3–24 months).
The primary outcome reported across all reviews was the change in body weight (kg), expressed as mean difference (MD) or standardized mean difference (SMD). Secondary outcomes included BMI, waist circumference, body fat percentage, and adherence or dropout rates. Risk of bias and methodological quality were variably assessed; all reviews reported at least moderate quality by AMSTAR 2 criteria (Figure 3).
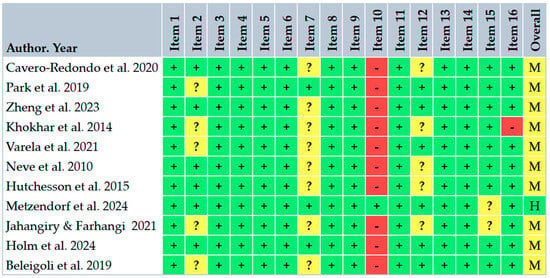
Figure 3.
Critical appraisal of included reviews according to AMSTAR 2 criteria [15]. Green (+) = yes; yellow (?) = partial yes; red (−) = no; (H) = high confidence; (M) = moderate confidence [9,10,18,19,20,21,22,23,24,25,26].
Among the 254 primary studies for which country or region was reported, 149 (58.7%) were from North America, 38 (15.0%) from Europe, 33 (13.0%) from Oceania, 33 (13.0%) from Asia, and 1 study (0.4%) was multisite. Figure 4 depicts the capture areas of these primary studies.
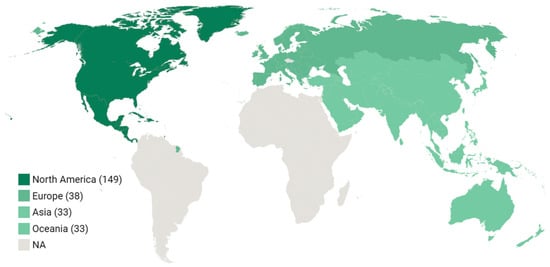
Figure 4.
Regional distribution of primary studies.
Regarding country income classification, of the 254 studies with available data, the vast majority, 237 studies (93.3%), were conducted in high-income countries. Additionally, seven studies (2.8%) took place in upper-middle-income countries and seven studies (2.8%) in lower-middle-income countries. The multisite study (0.4%) and two studies from Asia without a specified country (0.8%) were not classified by income level.
The primary studies included across reviews were published between 1999 and 2024, with a median publication year of 2013 and the majority published after 2010. Notably, three systematic reviews included primary studies published during or after the COVID-19 pandemic (2020 or later), reflecting the recent evolution in eHealth interventions. A summary of included reviews and their main characteristics are provided in Table 1.

Table 1.
Characteristics of selected reviews.
3.3. Overlap Among Primary Studies
After deduplication and standardization, 212 unique primary studies were identified across the 11 included systematic reviews out of a total of 261 initial study inclusions. This reduction from the nominal total reflects substantial overlap among reviews: many of the same primary studies were included in more than one systematic review, sometimes under minor citation variations or reported as separate entries for different analyses or follow-ups. This rigorous harmonization prevents artificial inflation of the evidence base, as recommended in the methodology for umbrella reviews. The resulting Corrected Covered Area (CCA) was 2.3%, indicating slight overlap according to established thresholds [16]. The low degree of overlap suggests minimal risk of evidence inflation or redundancy in our umbrella review. Further details and the complete overlap matrix are provided in Table S3.
3.4. Risk of Bias Within Studies
Among the 11 included systematic reviews, the most frequently used tool for risk of bias assessment was the Cochrane Risk of Bias tool (original or RoB 2), applied in 7 reviews [10,18,19,21,23,25,26]. The Jadad scale was used in two reviews [20,24], and the Joanna Briggs Institute instrument (JBI-MAStARI) was used in two reviews [9,22]. One review [18] additionally used the ROBINS-I tool for non-randomized studies. One review [26] assessed the risk of bias using GRADE domains rather than a standalone tool. All reviews reported some method of risk of bias assessment for the included primary studies.
3.5. Risk of Bias Across Studies
Of the eleven included systematic reviews, eight (73%) formally evaluated publication bias in their meta-analyses using funnel plot inspection and/or statistical tests such as Egger’s or Begg’s test [10,18,19,20,21,22,24,25]. Among these, seven reviews (64%) reported no evidence of publication bias for their primary outcomes, whereas one review [18] identified significant publication bias using Egger’s test and funnel plot asymmetry. Three reviews [9,23,26] did not report a formal assessment of publication bias.
3.6. Representative Effect Sizes from Individual Studies
A total of 26 effect sizes were extracted from the eligible meta-analyses included in this umbrella review. Of these, four were standardized effect sizes (Cohen’s d, standardized mean difference [SMD]), fifteen were unstandardized effect sizes (mean difference in kilograms, BMI in kg/m2, risk ratio [RR]), and seven were classified as other effect measures, including odds ratios, proportions, or effect sizes not clearly defined as standardized or unstandardized. These results cover main outcomes such as weight loss, weight change, BMI change, and waist circumference.
Table 2 presents these effect sizes together with their 95% confidence intervals (CIs), PICO categories, heterogeneity (I2), publication bias, and strength of evidence according to the umbrella review methodology. When available, the GRADE rating for certainty of evidence is also included.

Table 2.
Representative effect sizes from individual studies.
The directions of both standardized and unstandardized effect sizes are presented as originally reported. The number of p-values for representative effect sizes is also provided in Table 2.
3.7. Moderators
We summarized the results from moderator analyses conducted across the included meta-analyses (full details available in Table 3). Out of the 11 meta-analyses included, 10 (91%) reported conducting some form of moderator analysis. Most examined mobile health (mHealth) interventions (e.g., smartphone apps, SMS, wearables) [10,18,22,23], web-based digital interventions [9,21,24,26], or eHealth lifestyle interventions that included both web-based and mobile components [25]. Commonly tested moderators included sample characteristics (such as age, sex, baseline BMI, and region) and intervention features (such as comparator type, platform/device, intervention duration, presence of behavioral counseling, feedback frequency, and digital contact intensity).

Table 3.
Moderator analyses.
Among the ten reviews reporting moderator analyses, two meta-analyses (18%) conducted formal meta-regression to statistically assess the contribution of moderators to heterogeneity [18,26]. In both cases, intervention type, comparator group, and intervention duration were identified as significant moderators influencing weight loss outcomes.
The remaining eight meta-analyses (73%) conducted only subgroup analyses without formal meta-regression modeling. For instance, Khokhar et al. (2014) [20] stratified results by device type (mobile phone vs. PDA), while others evaluated intervention duration, feedback mechanisms, geographical region, or participant characteristics.
Across studies, frequently reported significant moderators included shorter intervention duration (<6 months), smartphone-based delivery, inclusion of human contact or behavioral counseling, and trials conducted in specific regions (particularly North America and Asia). However, these effects were not always consistent; in some cases, moderator effects were limited to specific subgroups or were not sustained at longer follow-up durations or when compared to active control groups.
3.8. Quantitative Synthesis and Subgroup Meta-Analyses
Meta-analyses were conducted for each clinically and methodologically homogeneous subgroup with sufficient data. The complete code used for data preprocessing, selection of representative effect sizes, and statistical analyses is available in File S3.
Results for smartphone app interventions, web-based interventions (with and without human contact), and outcomes related to weight, BMI, waist circumference, and body fat, as well as analyses stratified by intervention duration (short-term and long-term), are summarized below, following best practices for umbrella reviews in this field [27,28].
3.8.1. Mobile App Interventions
A random-effects meta-analysis pooling studies evaluating mobile application interventions exclusively (i.e., smartphone apps, excluding SMS and telephone-based technologies) demonstrated a statistically significant pooled mean difference in weight loss of −1.32 kg (95% CI: −2.54 to −0.11; I2 = 86.1%) compared to usual care or minimal intervention (Figure 5). The significant heterogeneity observed indicates considerable variability across studies regarding app features, target populations, and intervention designs, suggesting caution in generalizing these results.
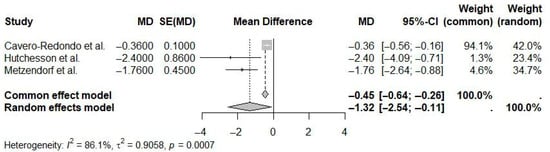
Figure 5.
Pooled effect of mobile app interventions versus usual care on weight loss in overweight and obese adults (random-effects meta-analysis). The diamond represents the overall pooled mean difference and its 95% confidence interval. The vertical dotted line indicates the line of no effect (mean difference = 0) [18,22,23].
3.8.2. Web-Based Interventions with Human Contact
In analyses restricted to web-based interventions incorporating human contact (e.g., coaching or support), the pooled mean difference in weight loss was −1.30 kg (95% CI: −2.80 to 0.20; I2 = 0.0%) compared to controls (Figure 6). Although this effect was not statistically significant, the direction favored interventions with human support. The absence of observed heterogeneity suggests high consistency among the included studies.
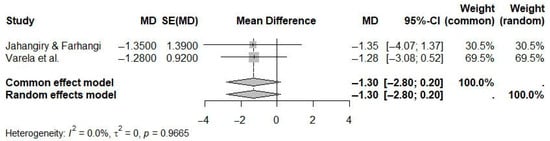
Figure 6.
Pooled effect of web-based interventions with human contact versus controls on weight loss (random-effects meta-analysis). See the legend of Figure 5 for explanation of symbols and lines [21,24].
3.8.3. Web-Based Interventions Without Human Contact
For web-based interventions without human contact, the pooled mean difference in weight loss was −1.15 kg (95% CI: −2.78 to 0.49; I2 = 96.5%) (Figure 7). This effect was not statistically significant, and the very high heterogeneity highlights substantial variability among the intervention characteristics and study populations.
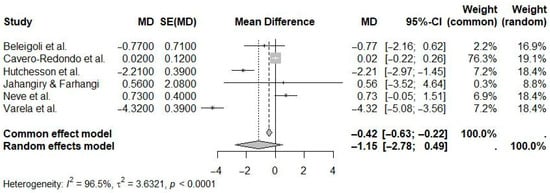
Figure 7.
Pooled effect of web-based interventions without human contact versus controls on weight loss (random-effects meta-analysis). See the legend of Figure 5 for explanation of symbols and lines [9,18,21,22,24,26].
3.8.4. Weight Outcome
A random-effects meta-analysis of studies reporting weight outcomes demonstrated a statistically significant pooled mean difference of −1.43 kg (95% CI: −2.24 to −0.62; I2 = 94.4%) favoring eHealth interventions compared to controls (Figure 8). Although statistically significant, the very high heterogeneity underscores considerable variation in intervention methods and study populations.
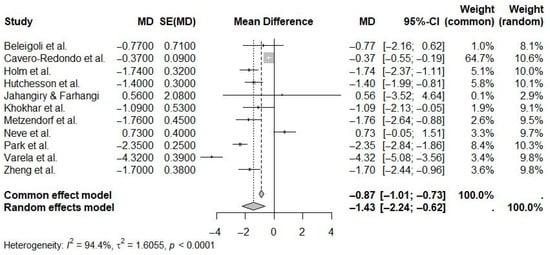
Figure 8.
Pooled effect of eHealth interventions versus controls on weight loss (random-effects meta-analysis). See the legend of Figure 5 for explanation of symbols and lines [9,10,18,19,20,21,22,23,24,25,26].
3.8.5. BMI Outcome
Studies assessing BMI outcomes yielded a statistically significant pooled mean difference of −0.58 kg/m2 (95% CI: −0.75 to −0.40; I2 = 42.3%), favoring eHealth interventions compared to controls (Figure 9). The moderate heterogeneity suggests greater consistency in BMI outcomes compared to weight outcomes.
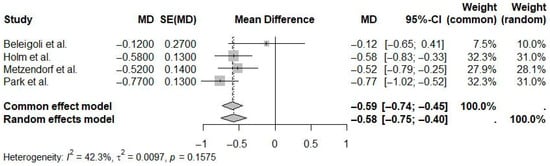
Figure 9.
Pooled effect of eHealth interventions versus controls on BMI reduction (random-effects meta-analysis). See the legend of Figure 5 for explanation of symbols and lines [10,23,25,26].
3.8.6. Waist Circumference Outcome
The pooled mean difference for waist circumference was statistically significant at −1.53 cm (95% CI: −2.04 to −1.01; I2 = 0.0%), favoring eHealth interventions (Figure 10). No heterogeneity was observed, indicating high consistency among the results of the included studies.
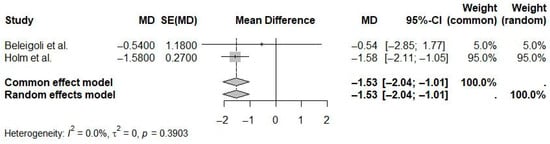
Figure 10.
Pooled effect of eHealth interventions versus controls on waist circumference reduction (random-effects meta-analysis). See the legend of Figure 5 for explanation of symbols and lines [25,26].
3.8.7. Short-Term eHealth Interventions (≤6 Months)
A random-effects meta-analysis evaluating short-term eHealth interventions (≤6 months) indicated a pooled mean difference in weight loss of −1.06 kg (95% CI: −2.27 to 0.15; I2 = 85.2%) compared to controls (Figure 11). This effect was not statistically significant, with high heterogeneity suggesting significant variability in interventions and study populations.
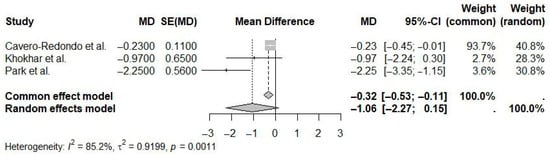
Figure 11.
Pooled effect of short-term (≤6 Months) eHealth interventions versus controls on weight loss (random-effects meta-analysis). See the legend of Figure 5 for explanation of symbols and lines [10,18,20].
3.8.8. Long-Term eHealth Interventions (≥12 Months)
For long-term eHealth interventions (≥12 months), the pooled mean difference in weight loss was statistically significant at −1.13 kg (95% CI: −2.17 to −0.09; I2 = 79.8%) compared to controls (Figure 12). The moderate to high heterogeneity highlights notable variability in intervention characteristics and populations across studies.
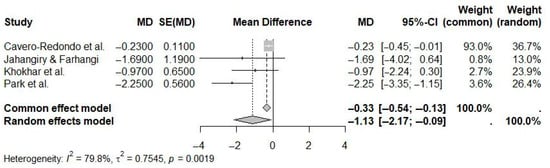
Figure 12.
Pooled effect of long-term (≥12 Months) eHealth interventions versus controls on weight loss (random-effects meta-analysis). See the legend of Figure 5 for explanation of symbols and lines [10,18,20,24].
Additional subgroup analysis was performed for body fat percentage outcomes. However, this outcome was derived from a single systematic review, precluding umbrella meta-analysis. The reported effect size (MD = −1.40%, 95% CI: −2.93 to 0.13) (Figure 13) represents the pooled estimate from this single review.
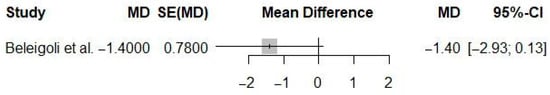
Figure 13.
Pooled mean difference in body fat percentage for eHealth interventions compared to controls (single-review estimate). See the legend of Figure 5 for explanation of symbols and lines [26].
3.9. Qualitative Synthesis
Qualitative findings indicate that mHealth interventions, particularly those emphasizing lifestyle self-monitoring, effectively enhance autonomy, self-management, and user empowerment, thereby increasing adherence rates compared to traditional methods [18]. Smartphones, due to their widespread accessibility, ease of use, and ability to reduce clinical burden by decreasing the frequency of in-person contacts, emerged as pivotal technological tools in this context [18].
Despite encouraging short-term results, the long-term sustainability of mHealth interventions remains uncertain. Qualitative synthesis from the included systematic reviews suggested that the primary role of mHealth interventions may be more appropriate as initial catalysts rather than stand-alone solutions for long-term weight maintenance [10,20]. Holistic and integrated mHealth programs, which comprehensively address nutrition, physical activity, and mental health, have demonstrated multifaceted benefits; however, sustained engagement tends to diminish without sufficient human interaction [19].
Web-based interventions notably depend on frequent, personalized feedback from healthcare professionals, highlighting human interaction as essential to enhance user motivation, adherence, and safety [9,21]. Additionally, structured behavioral components, goal-setting, and consistent self-monitoring significantly enhance the effectiveness of these interventions [22,24,25]. Despite initial successes, web-based programs often face challenges in sustaining long-term weight loss, underscoring the necessity for continuous user engagement and strategically designed digital features to preserve achieved outcomes [26].
4. Discussion
This umbrella review yields two main findings: first, the modest but significant effectiveness of mobile app and long-term eHealth interventions, and second, the inconclusive evidence for stand-alone web-based approaches.
Specifically, mobile app interventions, particularly those delivered via smartphones, significantly reduce body weight compared to usual care or minimal interventions (MD = −1.32 kg; 95% CI: −2.54 to −0.11). Additionally, long-term eHealth interventions (≥12 months) achieved statistically significant weight reduction (MD = −1.13 kg; 95% CI: −2.17 to −0.09). Similarly, eHealth interventions resulted in significant reductions in BMI (MD = −0.58 kg/m2) and waist circumference (MD = −1.53 cm). However, web-based interventions, regardless of human support, did not yield statistically significant weight loss compared to controls. Despite the favorable direction of effect for web-based interventions with human support, their confidence intervals crossed the null value. Moderate to high heterogeneity (I2 > 80%) was evident across most analyses, with notably high heterogeneity observed in web-based interventions without human support.
4.1. Comparison with Previous Umbrella Reviews
These findings refine and update the results reported by Sorgente et al. (2017) [29], who found that web-based interventions yielded small but statistically significant weight reductions in overweight and obese individuals, particularly when personalized feedback was included. Similarly, Singh et al. (2024) [30] reported an average weight reduction of −1.89 kg (95% CI: −2.42 to −1.36) across diverse digital health strategies, alongside increased physical activity (+1329 steps/day) and reduced sedentary behavior (−426 min/week), reinforcing the overall effectiveness of digital interventions.
While our results align directionally with these findings, our review provides a more precise and specific conclusion: mobile apps are the most consistent modality for effective weight loss, considering that recent data show that web-based interventions, even with added human support, generally failed to achieve statistical significance in pooled analyses for weight loss.
4.2. Context and Need for Research in Diverse Settings
As also highlighted by König et al. (2025) [31], most studies included in both our review and prior literature were conducted in high-income countries. This imbalance creates a notable gap in evidence from lower- and middle-income regions. This evidence gap is especially acute in Latin America and the African continent, regions that were significantly underrepresented in the included studies.
To enhance the policy relevance and generalizability of eHealth research, merely conducting more studies in these underrepresented regions is not sufficient; the interventions themselves must be contextually appropriate. Future research should, therefore, prioritize the development and validation of culturally adapted interventions, ensuring that content, language, and behavioral cues are resonant with local social norms and dietary habits. Furthermore, addressing the digital divide is critical. Study protocols must incorporate digital literacy strategies, such as initial user training and ongoing technical support, to ensure that technological barriers do not prevent access for the most vulnerable populations [32,33,34]. Only by addressing both cultural context and digital literacy can the full potential of these technologies be realized equitably on a global scale.
Future studies must also address vulnerable populations and individuals managed within PHC, which present specific needs and challenges for intervention delivery and adherence. Such studies should evaluate not only efficacy but also barriers to access, digital literacy, cultural adaptation, and integration with existing public health strategies.
4.3. Factors Influencing Digital Intervention Outcomes
In addition to quantitative results, qualitative insights from included reviews help explain differences in adherence and sustainability of digital interventions. Mobile health interventions focusing on lifestyle self-monitoring commonly reported improved user autonomy, empowerment, and engagement due to easy accessibility and reduced dependence on in-person contacts [18]. However, maintaining long-term engagement appeared challenging without sufficient human interaction, especially in comprehensive interventions targeting multiple behaviors such as nutrition, physical activity, and mental health [19,20]. Similarly, web-based programs highlighted the critical role of structured behavioral elements (goal-setting, self-monitoring, and particularly regular personalized feedback from health professionals) as key determinants of effectiveness [9,21,22,24,25,26].
These qualitative insights underline the importance of strategically designed interventions that sustain engagement through ongoing human support and user-centered features.
4.4. Implications for Clinical Practice and Public Health Policy
The observed efficacy of mHealth interventions, particularly those incorporating behavior change components and long-term monitoring, underscores their potential as tools to support weight management within both primary care and broader public health strategies.
However, the long-term sustainability and cost-effectiveness of these interventions are critical for their integration into health systems. While the literature demonstrates effectiveness, most interventions are evaluated within time-limited, grant-funded research contexts, leaving their long-term viability uncertain. Similarly, a significant gap exists in formal cost-effectiveness analyses. For policymakers and healthcare providers to make informed decisions, future research must move beyond efficacy and incorporate rigorous analyses of implementation models and cost-effectiveness.
The successful integration of these digital tools into public health systems requires more than just technological innovation. As noted by Cao et al. (2022) [32], digital health solutions must be embedded within broader health strategies, supported by robust governance, ongoing workforce training, investment in digital infrastructure, and systematic evaluation. Examining emerging public policy models illustrates these principles in action.
For instance, one direct public eHealth solution is the “Peso Saudável” (Healthy Weight) functionality, integrated into the Brazilian Health System’s eHealth platform (Conecte SUS). This resource provides users with a tool for self-monitoring their weight and guidance on making healthy lifestyle changes, representing an innovative strategy to support obesity care within the primary healthcare system [35].
In England, the National Health Service (NHS) Digital Weight Management Programme provides a contrasting commissioning model. This 12-week program, accessible via primary care referral, delivers both behavioral and nutritional support. An evaluation of over 63,000 referrals demonstrated clinically meaningful weight loss (an average of −2.2 kg for program finishers and −3.9 kg for completers), with equitable effectiveness observed across diverse socioeconomic and ethnic groups [36].
Despite these advances, challenges persist. In low- and middle-income settings, such as with the NUTRES SMS program in Mexico, implementation was challenged by barriers, including limited mobile access and poor connectivity, underscoring how the digital divide can limit the real-world impact of even well-received interventions [37]. Furthermore, while large-scale deployments, such as “Peso Saudável,” are valuable case studies, many still lack published, peer-reviewed efficacy data.
In this context, pilot programs, feasibility studies, and contextual adaptations are essential to ensure that digital interventions are equitable, accessible, and effective across diverse populations. The success of public and community mHealth interventions depends not only on the technology but on its deep integration with human support, its adaptation to local infrastructure, and a steadfast commitment to evaluation and equity to maximize its population-level impact.
4.5. Equity and Accessibility Considerations
One limitation of digital interventions, as reported by Lozada-Tequeanes et al. (2024) [37], is the risk of excluding individuals with low digital literacy, limited access to devices, or inaccessible connectivity. In this context, researchers, developers, and policymakers must prioritize cultural tailoring, simplified interfaces, inclusive design, and public policies of digital inclusion to avoid deepening health disparities.
As reported by Mahou et al. (2021) [33], individuals with higher income and education levels were significantly more likely to use digital health services, underscoring socio-economic inequalities in access. To truly promote digital health equity, as emphasized by Lawrence (2022) [34], it is essential to address barriers at multiple levels. At the design stage, technologies must consider the lived experiences and preferences of diverse populations, avoiding algorithmic or interface-level biases that may marginalize specific groups. At the implementation level, interventions must be aligned with the realities of healthcare infrastructure and integrated into trusted points of care. Engagement strategies should also acknowledge user concerns, such as privacy, autonomy, and digital fatigue, especially among historically underserved populations. Given the complexity of this reality, equity-focused research and inclusive design are thus not only ethical imperatives but also efficacy determinants.
4.6. The Emerging Role of Artificial Intelligence in Digital Weight Management
Although artificial intelligence (AI) was not a focus of the interventions included in this umbrella review, recent developments in AI-driven health technologies have begun to reshape the landscape of digital weight management. Tools leveraging AI, such as adaptive feedback systems, chatbots, and predictive analytics, promise greater personalization and real-time adjustment to user needs, potentially improving adherence and outcomes compared to conventional digital strategies. In addition to these software-based solutions, recent advances also encompass hardware platforms, such as smartwatches and other wearable devices, which can provide real-time monitoring and adaptive feedback when integrated with AI-driven digital health interventions [38,39,40].
Despite this potential, the current evidence base for AI-enabled interventions in weight management remains limited, with few robust randomized controlled trials or high-quality systematic reviews available for critical appraisal. This fact is likely due to the novelty of these technologies and the time required for rigorous evaluation and reporting in the literature [41].
This umbrella review highlights significant limitations within the current eHealth literature, such as inconsistent evidence for web-based interventions and high methodological heterogeneity across most analyses. As the field advances toward integrating more advanced technologies, such as AI, it is imperative that these existing shortcomings are not replicated. Evaluating AI presents its own critical challenges, particularly regarding transparency, reproducibility, and algorithmic bias [41]. To pre-emptively address these issues, future research must adopt rigorous methodologies [12]. For instance, to improve reproducibility and mitigate bias, study protocols should include a systematic and justified selection of the AI models analyzed, prioritize experiments using direct Application Programming Interfaces over public web interfaces, and standardize deterministic model settings (e.g., ‘temperature’ = 0). By implementing such standards from the outset, the field has an opportunity to build a trustworthy and equitable evidence base for AI in weight management, preventing the cycle of inconclusive findings that have affected other areas of eHealth.
4.7. Methodological Considerations and Limitations
One important methodological consideration in this umbrella review concerns the inclusion of pharmacological interventions as part of the conventional treatment in comparator groups. Because information regarding the use of pharmacotherapy in comparators tends to be underreported or not explicitly detailed in systematic reviews, we opted a priori not to exclude reviews solely based on insufficient specification about medication use. While our critical appraisal indicated a low risk of bias from this source across the included evidence, the lack of detailed reporting may limit the ability to exclude potential confounding from unreported pharmacotherapy entirely. This approach was chosen to ensure comprehensiveness and external validity. However, future reviews should encourage the systematic reporting of all active components in comparator arms.
Furthermore, this review used comprehensive search strategies, dual independent screening, and overlap quantification. Subgroup and moderator analyses helped clarify effect sizes and their potential modifiers. Still, the high heterogeneity, reliance on studies from high-income settings, and variability in intervention designs remain significant limitations. Most included studies had short-term interventions, and only a minority evaluated long-term outcomes. The sustainability of weight loss beyond the intervention period remains uncertain.
5. Conclusions
This umbrella review confirms that mobile app interventions and long-term eHealth strategies produce modest but significant reductions in body weight, BMI, and waist circumference in overweight and obese adults, whereas the evidence for stand-alone web-based interventions remains inconclusive. The current evidence base is largely derived from studies in high-income countries, with limited representation from low- and middle-income regions and primary care settings.
We therefore issue a clear call to action for researchers, practitioners, and policymakers. Researchers must prioritize culturally tailored, methodologically rigorous studies in underrepresented and vulnerable populations, incorporating digital literacy strategies and robust assessments of sustainability and cost-effectiveness. Emerging technologies, such as AI models in the context of digital health integrations, highlight the need for high-quality trials and comprehensive reviews to clarify the impact, safety, and equity of AI-enabled interventions. Practitioners should integrate evidence-based digital tools as adjuncts to comprehensive weight management strategies, ensuring equitable access and sustained patient engagement. Policymakers have a responsibility to invest in the development, evaluation, and sustainable implementation of digital health solutions, establishing supportive frameworks for funding, data governance, and digital infrastructure.
Ultimately, collaborative efforts among researchers, practitioners, and policymakers remain essential to fully realize the population-level benefits of digital interventions in addressing the global challenge of obesity.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/ijerph22071152/s1, Table S1: PRISMA Checklist; File S1: Electronic Search Strategy; File S2: R Scripts for Cohen’s Kappa Coefficient Calculation; Table S2: Reasons for Full-Text Exclusion; Table S3: Overlap of primary studies; File S3: R Scripts for Data Extraction, Subgroup Selection, and Meta-Analyses.
Author Contributions
Conceptualization, F.d.F.S.C. and C.P.B.d.A.; methodology, F.d.F.S.C. and C.P.B.d.A.; software, F.d.F.S.C.; validation, F.d.F.S.C. and C.P.B.d.A.; formal analysis, F.d.F.S.C. and C.P.B.d.A.; investigation, F.d.F.S.C. and C.P.B.d.A.; resources, F.d.F.S.C. and C.P.B.d.A.; data curation, F.d.F.S.C.; writing—original draft preparation, F.d.F.S.C.; writing—review and editing, F.d.F.S.C. and C.P.B.d.A.; visualization, F.d.F.S.C.; supervision, C.P.B.d.A.; project administration, F.d.F.S.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are derived from previously published systematic reviews and meta-analyses available in public domain databases (Cochrane Library, LILACS, PubMed, ScienceDirect, and Web of Science). The detailed electronic search strategies are provided in File S1. The original contributions and extracted data are included in the article and Supplementary Material. Additional data or materials can be requested from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AI | Artificial Intelligence |
| AMSTAR 2 | A MeaSurement Tool to Assess Systematic Reviews (version 2) |
| BIB | BibTeX file format |
| BMI | Body Mass Index |
| CCA | Corrected Covered Area |
| CI | Confidence Interval |
| COVID-19 | Coronavirus Disease 2019 |
| DALYs | Disability-Adjusted Life Years |
| eHealth | Electronic Health |
| GDP | Gross Domestic Product |
| GRADE | Grading of Recommendations, Assessment, Development and Evaluation |
| IMB | Information-Motivation-Behavioral Skills |
| ITT | Intention-To-Treat |
| JBI-MAStARI | Joanna Briggs Institute Meta-Analysis of Statistics Assessment and Review Instrument |
| MD | Mean Difference |
| mHealth | Mobile Health |
| NBIB | Native BibTeX format |
| PDA | Personal Digital Assistant |
| PHC | Primary Healthcare |
| PICOS | Population, Intervention, Comparator, Outcome, Study design |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PROSPERO | International Prospective Register of Systematic Reviews |
| R | Programming language and statistical computing environment |
| RoB | Risk of Bias |
| ROBINS-I | Risk Of Bias In Non-Randomized Studies-of Interventions |
| RR | Risk Ratio |
| SMD | Standardized Mean Difference |
| SUS | Sistema Único de Saúde |
References
- World Health Organization. WHO Discussion Paper on Obesity; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- World Obesity Federation. Obesity Atlas. 2024. Available online: https://data.worldobesity.org/publications/WOF-Obesity-Atlas-v7.pdf (accessed on 24 May 2024).
- Tchang, B.G.; Saunders, K.H.; Igel, L.I.; Best, C.; Aronne, L.J. Pharmacologic treatment of overweight and obesity in adults. Emerg. Top. Life Sci. 2021, 5, 337–356. [Google Scholar]
- Liu, C.; Zhang, Z.; Wang, B.; Meng, T.; Li, C.; Zhang, X. Global health impacts of high BMI: A 30-year analysis of trends and disparities across regions and demographics. Diabetes Res. Clin. Pract. 2024, 217, 111883. [Google Scholar] [CrossRef] [PubMed]
- Rocha, L.P.; Machado, I.E.; Fogal, A.S.; de Sousa, C.A.C.; Malta, D.C. Burden of disease and direct costs to the health system attributable to high body mass index in Brazil. Public Health 2024, 233, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Massoomi, M.R.; Handberg, E.M. Increasing and evolving role of smart devices in modern medicine. Eur. Cardiol. Rev. 2019, 14, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Sherrington, A.; Newham, J.J.; Bell, R.; Adamson, A.; McColl, E.; Araujo-Soares, V. Systematic review and meta-analysis of internet-delivered interventions providing personalized feedback for weight loss in overweight and obese adults. Obes. Rev. 2016, 17, 541–551. [Google Scholar] [CrossRef] [PubMed]
- Park, N.Y.; Jang, S. Effects of mHealth practice patterns on improving metabolic syndrome using the information–motivation–behavioral skills model. Nutrients 2024, 16, 2099. [Google Scholar] [CrossRef] [PubMed]
- Neve, M.; Morgan, P.J.; Jones, P.R.; Collins, C.E. Effectiveness of web-based interventions in achieving weight loss and weight loss maintenance in overweight and obese adults: A systematic review with meta-analysis. Obes. Rev. 2010, 11, 306–321. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H.; Hwang, J.; Choi, Y.K. Effect of mobile health on obese adults: A systematic review and meta-analysis. Healthc. Inform. Res. 2019, 25, 12–26. [Google Scholar] [CrossRef] [PubMed]
- Clipper, B. The influence of the COVID-19 pandemic on technology adoption in health care. Nurse Lead. 2020, 18, 500–503. [Google Scholar] [CrossRef] [PubMed]
- Senbekov, M.; Saliev, T.; Bukeyeva, Z.; Almabayeva, A.; Zhanaliyeva, M.; Aitenova, N.; Toishibekov, Y.; Fakhradiyev, I. The recent progress and applications of digital technologies in healthcare: A review. Int. J. Telemed. Appl. 2020, 2020, 8830200. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Zhang, M.; Qian, Y.; Yang, H.; Xu, X.; Wu, S.; Zhang, Y.; Deng, Y.; Wang, X. Exploring the Influence of Event Criticality, Disruption, and Novelty on mHealth App Use and Empowerment: Cross-sectional Study in China During COVID-19. Int. J. Environ. Res. Public Health 2023, 20, 834. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- Pieper, D.; Antoine, S.L.; Mathes, T.; Neugebauer, E.A.; Eikermann, M. Systematic review finds overlapping reviews were not mentioned in every other overview. J. Clin. Epidemiol. 2014, 67, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Li, S.-J.; Zhou, Y.; Ma, H.-M.; Wang, A.-Q.; Tang, X.-Y.; Pei, R.-Y.; Piao, M.-H. Effects of Mobile Applications on Weight-Related, Behavior and Metabolic Outcomes for Adults with Overweight and Obesity: A Systematic Review and Meta-Analysis. In Innovation in Applied Nursing Informatics; Strudwick, G., Hardiker, N.R., Rees, G., Cook, R., Lee, Y.J., Eds.; IOS Press: Amsterdam, The Netherlands, 2024; pp. 386–391. [Google Scholar]
- Cavero-Redondo, I.; Martinez-Vizcaino, V.; Fernandez-Rodriguez, R.; Saz-Lara, A.; Pascual-Morena, C.; Álvarez-Bueno, C. Effect of behavioral weight management interventions using lifestyle mHealth self-monitoring on weight loss: A systematic review and meta-analysis. Nutrients 2020, 12, 1977. [Google Scholar] [CrossRef] [PubMed]
- Zheng, S.; Edney, S.M.; Goh, C.H.; Tai, B.C.; Mair, J.L.; Castro, O.; Salamanca-Sanabria, A.; Kowatsch, T.; van Dam, R.M.; Müller-Riemenschneider, F. Effectiveness of holistic mobile health interventions on diet, and physical, and mental health outcomes: A systematic review and meta-analysis. eClinicalMedicine 2023, 63, 102309. [Google Scholar] [CrossRef] [PubMed]
- Khokhar, B.; Jones, J.; Ronksley, P.E.; Armstrong, M.J.; Caird, J.; Rabi, D. Effectiveness of mobile electronic devices in weight loss among overweight and obese populations: A systematic review and meta-analysis. BMC Obes. 2014, 1, 22. [Google Scholar] [CrossRef] [PubMed]
- Varela, C.; Oda-Montecinos, C.; Andrés, A.; Saldaña, C. Effectiveness of web-based feedback interventions for people with overweight and obesity: Systematic review and network meta-analysis of randomized controlled trials. J. Eat. Disord. 2021, 9, 75. [Google Scholar] [CrossRef] [PubMed]
- Hutchesson, M.J.; Rollo, M.E.; Krukowski, R.; Ells, L.; Harvey, J.; Morgan, P.J.; Callister, R.; Plotnikoff, R.; Collins, C.E. eHealth interventions for the prevention and treatment of overweight and obesity in adults: A systematic review with meta-analysis. Obes. Rev. 2015, 16, 376–392. [Google Scholar] [CrossRef] [PubMed]
- Metzendorf, M.I.; Wieland, L.S.; Richter, B. Mobile health (m-health) smartphone interventions for adolescents and adults with overweight or obesity. Cochrane Database Syst. Rev. 2024, 2, CD013591. [Google Scholar] [CrossRef] [PubMed]
- Jahangiry, L.; Farhangi, M.A. Obesity paradigm and web-based weight loss programs: An updated systematic review and meta-analysis of randomized controlled trials. J. Health Popul. Nutr. 2021, 40, 16. [Google Scholar] [CrossRef] [PubMed]
- Holm, T.F.; Udsen, F.W.; Giese, I.E.; Færch, K.; Jensen, M.H.; von Scholten, B.J.; Hangaard, S. The effectiveness of digital health lifestyle interventions on weight loss in people with prediabetes: A systematic review, meta-analysis, and meta-regression. J. Diabetes Sci. Technol. 2024, 18, 539–554. [Google Scholar]
- Beleigoli, A.M.; Andrade, A.Q.; Cançado, A.G.; Paulo, M.N.; Diniz, M.D.; Ribeiro, A.L. Web-based digital health interventions for weight loss and lifestyle habit changes in overweight and obese adults: Systematic review and meta-analysis. J. Med. Internet Res. 2019, 21, e9609. [Google Scholar] [CrossRef] [PubMed]
- Ioannidis, J.P.A. Integration of evidence from multiple meta-analyses: A primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. CMAJ 2009, 181, 488–493. [Google Scholar] [CrossRef] [PubMed]
- Aromataris, E.; Fernandez, R. Umbrella Reviews. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; Joanna Briggs Institute: Adelaide, Australia, 2023; Available online: https://jbi-global-wiki.refined.site/space/MANUAL/46873621/9.3.8+Synthesis+of+findings (accessed on 24 May 2024).
- Sorgente, A.; Pietrabissa, G.; Manzoni, G.M.; Re, F.; Simpson, S.; Perona, S.; Rossi, A.; Cattivelli, R.; Innamorati, M.; Jackson, J.B.; et al. Web-based interventions for weight loss or weight loss maintenance in overweight and obese people: A systematic review of systematic reviews. J. Med. Internet Res. 2017, 19, e229. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Verma, A.; Marupuru, S.; Rana, P.; Sharma, S.; Gupta, R.; Kamal, R.; Madaan, R.; Gupta, A.; Arora, R. Efficacy of eHealth, mHealth, and Digital Health Interventions on Physical Activity, Sedentary Behavior, and Weight Loss: An Umbrella Review and Meta-Analysis of Meta-Analyses. npj Digit. Med. 2024, 7, 63. [Google Scholar] [CrossRef] [PubMed]
- König, L.M.; Western, M.J.; Denton, A.H.; Krukowski, R.A. Umbrella review of social inequality in digital interventions targeting physical activity, diet, and weight outcomes. NPJ Digit. Med. 2025, 8, 46. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Zhang, G.; Liu, D. The Impact of Using mHealth Apps on Improving Public Health Satisfaction during the COVID-19 Pandemic: A Digital Content Value Chain Perspective. Healthcare 2022, 10, 479. [Google Scholar] [CrossRef] [PubMed]
- Mahou, X.; Barral, B.; Fernández, Á.; Bouzas-Lorenzo, R.; Cernadas, A. eHealth and mHealth Development in Spain: Promise or Reality? Int. J. Environ. Res. Public Health 2021, 18, 13055. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, K. Digital Health Equity. In Digital Health; Lin, S., Ed.; Exon Publications: Brisbane, Australia, 2022; Chapter 9. [Google Scholar]
- Oliveira, T.F.V.; Dias, P.C.; Tavares, M.C.G.C.F.; Leite, I.C.; Jaime, P.C. Fortalecimento das ações de cuidado às pessoas com obesidade no contexto da pandemia de COVID-19: O caso do Brasil. Cien. Saude Colet. 2023, 28, 3673–3685. [Google Scholar] [CrossRef]
- Taylor, K.; Indulkar, T.; Thompson, B.; Pinkard, C.; Barron, E.; Frost, T.; Jayawardane, P.; Davies, N.; Bakhai, C.; Forouhi, N.G.; et al. Early outcomes of referrals to the English National Health Service Digital Weight Management Programme. Obesity 2024, 32, 1083–1092. [Google Scholar] [CrossRef] [PubMed]
- Lozada-Tequeanes, A.L.; Théodore, F.L.; Kim-Herrera, E.; García-Guerra, A.; Quezada-Sánchez, A.D.; Alvarado-Casas, R.; Bonvecchio, A. Effectiveness and Implementation of a Text Messaging mHealth Intervention to Prevent Childhood Obesity in Mexico in the COVID-19 Context: Mixed Methods Study. JMIR mHealth uHealth 2024, 12, e55509. [Google Scholar] [CrossRef] [PubMed]
- Chew, H.S.J.; Chew, N.W.; Loong, S.S.E.; Lim, S.L.; Tam, W.S.W.; Chin, Y.H.; Chao, A.M.; Dimitriadis, G.K.; Gao, Y.; So, J.B.Y.; et al. Effectiveness of an artificial intelligence–assisted app for improving eating behaviors: Mixed methods evaluation. J. Med. Internet Res. 2024, 26, e46036. [Google Scholar] [CrossRef] [PubMed]
- Chew, H.S.J. The Use of Artificial Intelligence-Based Conversational Agents (Chatbots) for Weight Loss: Scoping Review and Practical Recommendations. JMIR Med. Inform. 2022, 10, e32578. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Huhulea, E.N.; Abraham, E.; Bienenstock, R.; Aifuwa, E.; Hirani, R.; Schulhof, A.; Tiwari, R.K.; Etienne, M. The role of artificial intelligence in obesity risk prediction and management: Approaches, insights, and recommendations. Medicina 2025, 61, 358. [Google Scholar] [CrossRef] [PubMed]
- Weeks, W.B. Using artificial intelligence to advance public health. Int. J. Public Health 2023, 68, 1606716. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).