Investigating Fall-Related Factors in Community-Dwelling Older Women Through Structural Equation Modeling Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
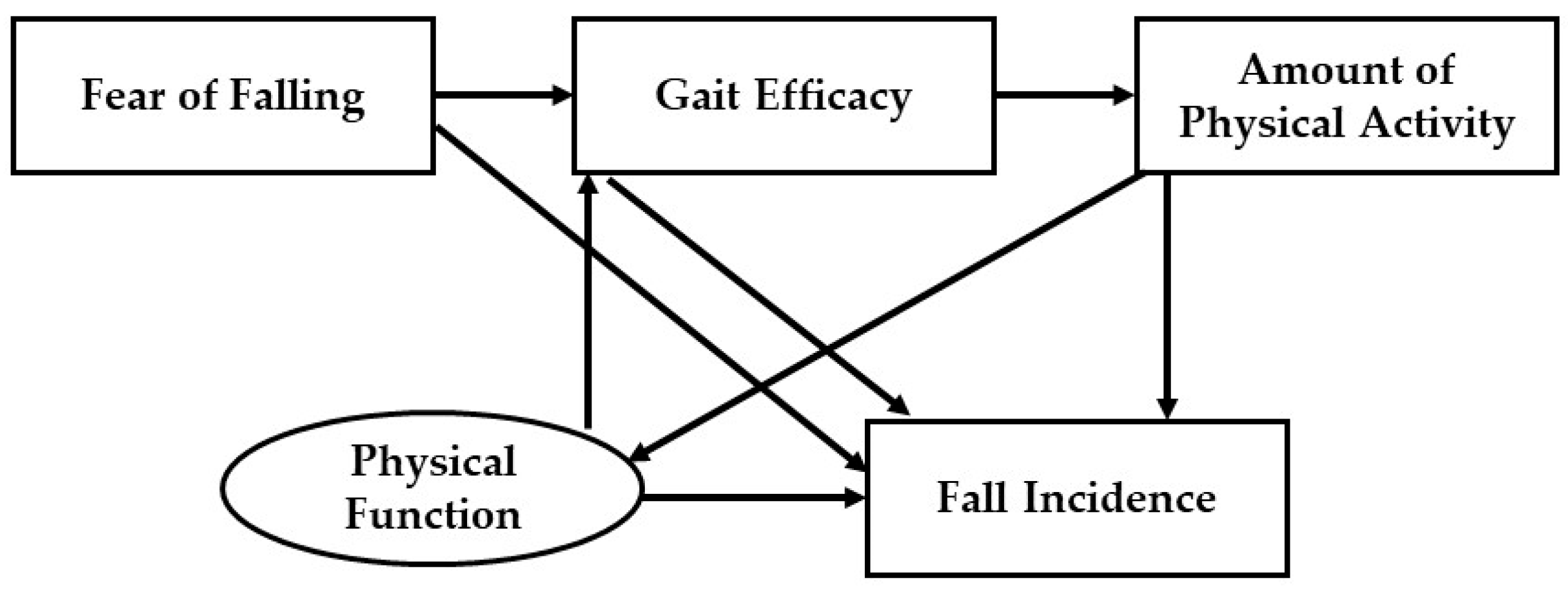
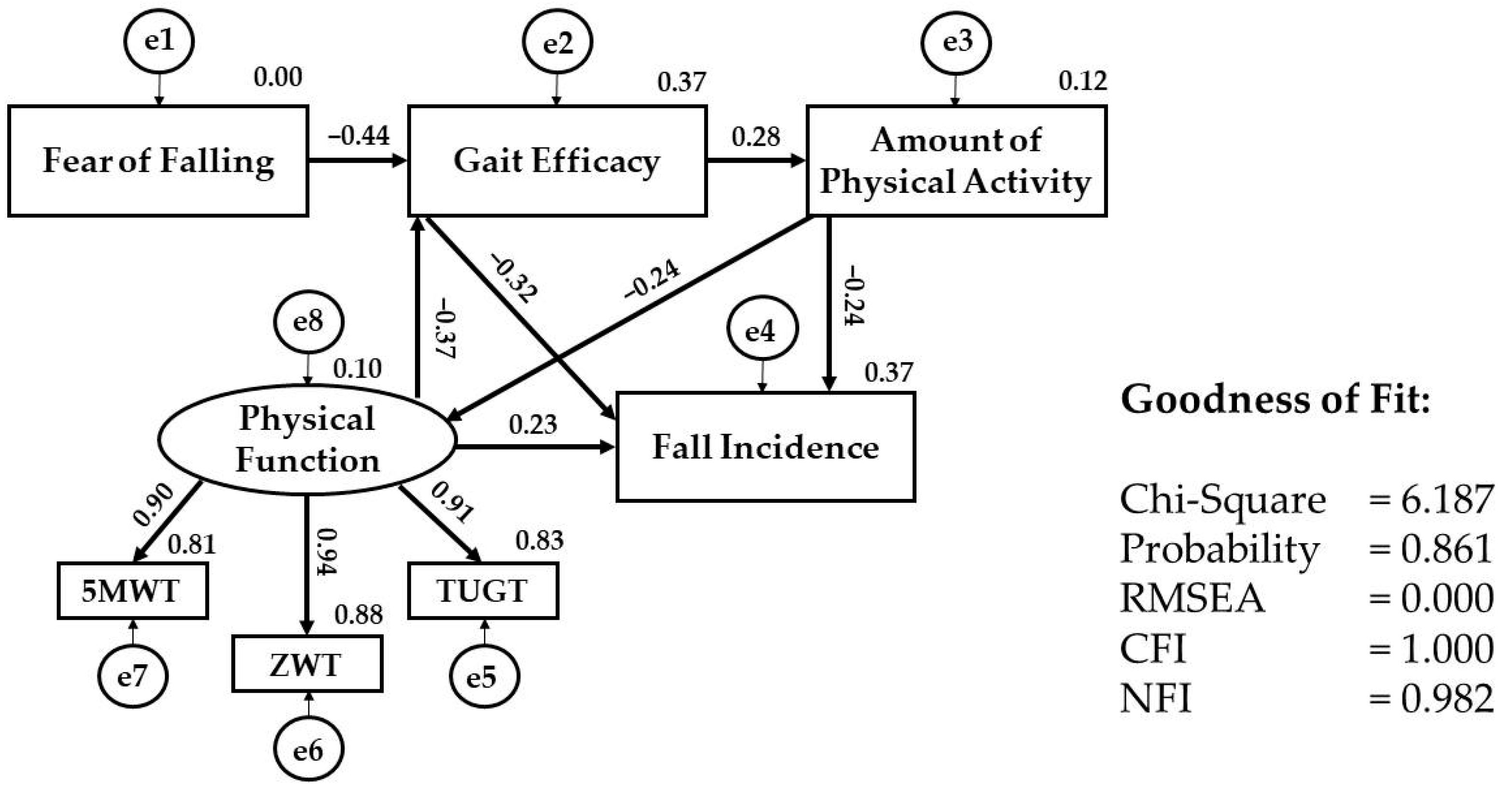
2.2. Structural Equation Modeling
2.3. Participants
2.4. Measurements
2.5. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. SEM Examination
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SEM | Structural equation modeling |
| Short FES-I | Short Fall Efficacy Scale International |
| 5MWT | Five-Meter Walking Test |
| TUGT | Timed Up and Go Test |
| ZWT | Zig-Zag Walking Test |
| CFA | Confirmatory factor analysis |
| CFI | Comparative fit index |
| NFI | Normed fit index |
| GFI | Goodness-of-fit index |
| RMSEA | Root mean square error of approximation |
References
- Adam, C.E.; Fitzpatrick, A.L.; Leary, C.S.; Ilango, S.D.; Phelan, E.A.; Semmens, E.O. The Impact of Falls on Activities of Daily Living in Older Adults: A Retrospective Cohort Analysis. PLoS ONE 2024, 19, e029401. [Google Scholar] [CrossRef]
- Harper, A.; Wilkinson, I. Falls in Older Adults: Causes, Assessment and Management. Medicine 2024, 52, 677–682. [Google Scholar] [CrossRef]
- Salari, N.; Darvishi, N.; Ahmadipanah, M.; Shohaimi, S.; Mohammadi, M. Global Prevalence of Falls in The Older Adults: A Comprehensive Systematic Review and Meta-analysis. J. Orthop. Surg. Res. 2022, 17, 334. [Google Scholar] [CrossRef] [PubMed]
- Sebastiani, C.; Wong, J.Y.X.; Litt, A.; Loewen, J.; Reece, K.; Conlin, N.; Dunand, T.; Montero Odasso, M.; D’Amore, C.; Saunders, S.; et al. Mapping Sex and Gender Differences in Falls Among Older Adults: A Scoping Review. J. Am. Geriatr. Soc. 2024, 72, 903–915. [Google Scholar] [CrossRef]
- Suh, M.; Kim, D.H.; Cho, I.; Ham, O.K. Age and Gender Differences in Fall-Related Factors Affecting Community-Dwelling Older Adults. J. Nurs. Res. 2023, 31, e270. [Google Scholar] [CrossRef]
- Gale, C.R.; Cooper, C.; Sayer, A.A. Prevalence and Risk Factors for Falls in Older Men and Women: The English Longitudinal Study of Ageing. Age Ageing 2016, 45, 789–794. [Google Scholar] [CrossRef] [PubMed]
- Halter, J.B.; Ouslander, J.G.; Studenski, S.; Asthana, S.; Supiano, M.A.; Ritchie, C. Hazzard’s Geriatric Medicine and Gerontology, 7th ed.; McGraw-Hill Education: New York, NY, USA, 2017; pp. 724–731. [Google Scholar]
- Patton, S.; Vincenzo, J.; Lefler, L. Gender Differences in Older Adults’ Perceptions of Falls and Fall Prevention. Health Promot. Pract. 2022, 23, 785–792. [Google Scholar] [CrossRef]
- Lavedán, A.; Viladrosa, M.; Jürschik, P.; Botigué, T.; Nuín, C.; Masot, O.; Lavedán, R. Fear of Falling in Community-Dwelling Older Adults: A Cause of Falls, a Consequence, or Both? PLoS ONE 2018, 13, e0194967. [Google Scholar] [CrossRef]
- Dai, B.; Ware, W.B.; Giuliani, C.A. A Structural Equation Model Relating Physical Function, Pain, Impaired Mobility (IM), and Falls in Older Adults. Arch. Gerontol. Geriatr. 2012, 55, 645–652. [Google Scholar] [CrossRef]
- dos Santos, E.P.R.; Ohara, D.G.; Patrizzi, L.J.; de Walsh, I.A.P.; Silva, C.d.F.R.; da Silva Neto, J.R.; Oliveira, N.G.N.; Matos, A.P.; Iosimuta, N.C.R.; Pinto, A.C.P.N.; et al. Investigating Factors Associated with Fear of Falling in Community-Dwelling Older Adults through Structural Equation Modeling Analysis: A Cross-Sectional Study. J. Clin. Med. 2023, 12, 545. [Google Scholar] [CrossRef]
- Cui, Y.; Liu, B.; Qin, M.Z.; Liu, Q.; Ye, H.; Zhou, J. Effects of Early Mental State Changes on Physical Functions in Elderly Patients with A History of Falls. BMC Geriatr. 2023, 23, 564. [Google Scholar] [CrossRef] [PubMed]
- Ko, J.; Park, Y.M. Menopause and The Loss of Skeletal Muscle Mass in Women. Iran. J. Public Health 2021, 50, 413–414. [Google Scholar] [CrossRef] [PubMed]
- Hadjistavropoulos, T.; Delbaere, K. The Psychology of Fall Risk: Fear, Anxiety, Depression, and Balance Confidence. In Falls in Older People: Risk Factors, Strategies for Prevention and Implications for Practice, 5th ed.; Lord, S.R., Sherrington, C., Naganathan, V., Eds.; Cambridge University Press: Cambridge, UK, 2021; pp. 161–171. [Google Scholar]
- Lee, D.; Tak, S.H. A Concept Analysis of Fear of Falling in Older Adults: Insights from Qualitative Research Studies. BMC Geriatr. 2023, 23, 651. [Google Scholar] [CrossRef]
- Pauelsen, M.; Nyberg, L.; Röijezon, U.; Vikman, I. Both Psychological Factors and Physical Performance Are Associated with Fall-Related Concerns. Aging Clin. Exp. Res. 2018, 30, 1079–1085. [Google Scholar] [CrossRef]
- Perera, S.; VanSwearingen, J.; Shuman, V.; Brach, J.S. Assessing Gait Efficacy in Older Adults: An Analysis Using Item Response Theory. Gait Posture 2020, 77, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-efficacy: Toward a Unifying Theory of Behavioral Change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef]
- McAuley, E.; Konopack, J.F.; Morris, K.S.; Motl, R.W.; Hu, L.; Doerksen, S.E.; Rosengren, K. Physical Activity and Functional Limitations in Older Women: Influence of Self-Efficacy. J. Gerontol. B Psychol. Sci. Soc. Sci. 2006, 61, 270–277. [Google Scholar] [CrossRef]
- McAuley, E.; Szabo, A.; Gothe, N.; Olson, E.A. Self-Efficacy: Implications for Physical Activity, Function, and Functional Limitations in Older Adults. Am. J. Lifestyle Med. 2011, 5, 361–369. [Google Scholar] [CrossRef]
- Hair, J., Jr.; Black, W.C.; Babin, B.J.; Anderson, A. Multivariate Data Analysis, 8th ed.; Aincow, A., Ed.; Cengage Learning EMEA: Hampshire, UK, 2021; pp. 603–647. [Google Scholar]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A. Statistical Power Analyses Using G*Power 3.1: Tests for Correlation and Regression Analyses. Behav. Res. Methods. 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Malta, M.; Cardoso, L.O.; Bastos, F.I.; Magnanini, M.M.F.; Passos da Silva, C.M.F. STROBE Initiative: Guidelines on Reporting Observational Studies. Rev. Saúde Pública 2010, 44, 559–565. [Google Scholar] [CrossRef]
- Kamide, N.; Shiba, Y.; Sakamoto, M.; Sato, H. Reliability and Validity of The Short Falls Efficacy Scale-International for Japanese Older People. Aging Clin. Exp. Res. 2018, 30, 1371–1377. [Google Scholar] [CrossRef] [PubMed]
- Newell, A.M.; Vanswearingen, J.M.; Hile, E.; Brach, J.S. The Modified Gait Efficacy Scale: Establishing The Psychometric Properties in Older Adults. Phys. Ther. 2012, 92, 318–328. [Google Scholar] [CrossRef] [PubMed]
- Salbach, N.M.; Mayo, N.E.; Higgins, J.; Ahmed, S.; Finch, L.E.; Richards, C.L. Responsiveness and Predictability of Gait Speed and Other Disability Measures in Acute Stroke. Arch. Phys. Med. Rehabil. 2001, 82, 1204–1212. [Google Scholar] [CrossRef]
- Masuda, S.; Suganuma, K.; Kaneko, C.; Hoshina, K.; Suzuki, T.; Serita, T.; Sakakibara, R. Prediction of Falls Using A 3-m Zigzag Walk Test. J. Phys. Ther. Sci. 2013, 25, 1051–1054. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bischoff, H.A.; Stähelin, H.B.; Monsch, A.U.; Iversen, M.D.; Weyh, A.; von Dechend, M. Identifying A Cut-Off Point for Normal Mobility: A Comparison of The Timed “Up and Go” Test in Community-Dwelling and Institutionalised Elderly Women. Age Ageing 2003, 32, 315–320. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the Probability for Falls in Community-Dwelling Older Adults Using the Timed Up & Go Test. Phys. Ther. 2000, 80, 896–903. [Google Scholar]
- Tanita Corporation. Instruction Manual of Accelerometer EZ-064, Tanita Co., Ltd., Tokyo, Japan. Available online: https://www.tanita.co.jp/support/manual/EZ-064 (accessed on 13 March 2023).
- Shanthi, R. Multivariate Data Analysis Using SPSS and AMOS; Ambica, C., Ed.; MJP Publisher: Chennai, India, 2019; pp. 413–432. [Google Scholar]
- Ikegami, S.; Takahashi, J.; Uehara, M.; Tokida, R.; Nishimura, H.; Sakai, A.; Kato, H. Physical Performance Reflects Cognitive Function, Fall Risk, and Quality of Life in Community-Dwelling Older People. Sci. Rep. 2019, 9, 12242. [Google Scholar] [CrossRef]
- Schumacher, B.T.; Bellettiere, J.; LaMonte, M.J.; Evenson, K.R.; Di, C.; Lee, I.M.; Sleet, D.A.; Eaton, C.B.; Lewis, C.E.; Margolis, K.L.; et al. Accelerometer-Measured Daily Steps, Physical Function, and Subsequent Fall Risk in Older Women: The Objective Physical Activity and Cardiovascular Disease in Older Women Study. J. Aging Phys. Act. 2022, 30, 635–645. [Google Scholar] [CrossRef]
- Lord, S.R.; Ward, J.A.; Williams, P.; Anstey, K.J. Physiological Factors Associated with Falls in Older Community-Dwelling Women. J. Am. Geriatr. Soc. 1994, 42, 1110–1117. [Google Scholar] [CrossRef]
- Taniguchi, M.; Sawano, S.; Maegawa, S.; Ikezoe, T.; Ichihashi, N. Physical Activity Mediates the Relationship between Gait Function and Fall Incidence after Total Knee Arthroplasty. J. Knee Surg. 2021, 34, 1205–1211. [Google Scholar] [CrossRef]
- Kwok, W.S.; Khalatbari-Soltani, S.; Dolja-Gore, X.; Byles, J.; Oliveira, J.S.; Pinheiro, M.B.; Sherrington, C. Differences in Falls and Physical Activity in Older Women from Two Generations. J. Gerontol. A Biol. Sci. Med. Sci. 2024, 79, glae033. [Google Scholar] [CrossRef] [PubMed]
- Lee, J. The Association Between Physical Activity and Risk of Falling in Older Adults: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Geriatr. Nurs. 2020, 41, 747–753. [Google Scholar] [CrossRef]
- Asim, M.; Aftab, M.; Bhatti, S.H.; Ahmad, T.; Ali Shah, S.M.; Akram, M. Identifying Factors Causing Decline in Physical Functionality of Geriatric Population. Eur. J. Inflamm. 2021, 19, 20587392211026109. [Google Scholar] [CrossRef]
- Hu, J.; Xia, Q.; Jiang, Y.; Zhou, P.; Li, Y. Risk Factors of Indoor Fall Injuries in Community-Dwelling Older Women: A Prospective Cohort Study. Arch. Gerontol. Geriatr. 2015, 60, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-Efficacy in Changing Societies. Cambridge University Press: Cambridge, UK, 2002; pp. 25–33. [Google Scholar]
- Nur’amalia, R. Perspective Review: The Influence of Gait Efficacy on Improving Physical Activity in Community-Dwelling Older Adults. ICON J. 2023, 8, 4–6. [Google Scholar] [CrossRef]
- Fushimi, T.; Fujihira, K.; Takase, H.; Miyashita, M. Relationships among Physical Activity, Physical Function, and Food Intake in Older Japanese Adults Living in Urban Areas: A Cross-Sectional Study. Geriatrics 2023, 8, 41. [Google Scholar] [CrossRef]
- Ferrero-Hernández, P.; Farías-Valenzuela, C.; Jofré-Saldía, E.; Marques, A.; Kovalskys, I.; Gómez, G.; Rigotti, A.; Cortés, L.Y.; García, M.Y.; Pareja, R.G.; et al. Physical Activity and Daily Steps Cut Offs Points for Overweight/Obesity Prevention among Eight Latin American Countries. Sci. Rep. 2022, 12, 18827. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Craig, C.L.; Aoyagi, Y.; Bell, R.C.; Croteau, K.A.; De Bourdeaudhuij, I.; Ewald, B.; Gardner, A.W.; Hatano, Y.; Lutes, L.D.; et al. How Many Steps/Day Are Enough? For Older Adults and Special Populations. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 80. [Google Scholar] [CrossRef]
- Mailey, E.L.; Huberty, J.; Dinkel, D.; McAuley, E. Physical Activity Barriers and Facilitators among Working Mothers and Fathers. BMC Public Health 2014, 14, 657. [Google Scholar] [CrossRef]
- Toyoda, H.; Hayashi, C.; Okano, T. Associations Between Physical Function, Falls, and The Fear of Falling among Older Adults Participating in A Community-Based Physical Exercise Program: A Longitudinal Multilevel Modeling Study. Arch. Gerontol. Geriatr. 2022, 102, 104752. [Google Scholar] [CrossRef]
- Julius, L.M.; Brach, J.S.; Wert, D.M.; Vanswearingen, J.M. Perceived Effort of Walking: Relationship with Gait, Physical Function and Activity, Fear of Falling, and Confidence in Walking in Older Adults with Mobility Limitations. Phys. Ther. 2012, 92, 1268–1277. [Google Scholar] [CrossRef] [PubMed]
- Xing, L.; Bao, Y.; Wang, B.; Shi, M.; Wei, Y.; Huang, X.; Dai, Y.; Shi, H.; Gai, X.; Luo, Q.; et al. Falls Caused by Balance Disorders in The Elderly with Multiple Systems Involved: Pathogenic Mechanisms and Treatment Strategies. Front. Neurol. 2023, 14, 1128092. [Google Scholar] [CrossRef] [PubMed]
- VanSwearingen, J.M.; Perera, S.; Brach, J.S.; Wert, D.; Studenski, S.A. Impact of Exercise to Improve Gait Efficiency on Activity and Participation in Older Adults with Mobility Limitations: A Randomized Controlled Trial. Phys. Ther. 2011, 91, 1740–1751. [Google Scholar] [CrossRef]
- Jin, B. Older Adults and Learning and Teaching. New Dir. Adult Cont. Educ. 2024, 2024, 82–91. [Google Scholar] [CrossRef]
| Characteristics | Total (N = 90) Mean ± SD/Number (%) | Fallers (N = 19) Mean ± SD/Number (%) | Non-Fallers (N = 71) Mean ± SD/Number (%) | p-Value | |
|---|---|---|---|---|---|
| Age (years) | 68.0 ± 6.4 | 67.6 ± 5.1 | 68.2 ± 6.7 | 0.730 a | |
| Educational Background | Less than middle school | 71 (78.9) | 16 (84.2) | 55 (77.5) | 0.753 b |
| Middle and high school | 19 (21.1) | 3 (15.8) | 16 (22.5) | ||
| Living Status | Living alone | 10 (11.1) | 3 (15.8) | 7 (9.9) | 0.435 b |
| Living with spouse/children, relatives | 80 (88.9) | 16 (84.2) | 64 (90.1) | ||
| Toilet Use | Sit | 24 (26.7) | 6 (31.6) | 18 (25.4) | 0.586 c |
| Squat | 66 (73.3) | 13 (68.4) | 53 (74.6) | ||
| Stair Use | Yes | 30 (33.3) | 6 (31.6) | 24 (33.8) | 0.855 c |
| No | 60 (66.7) | 13 (68.4) | 47 (66.2) | ||
| Working Status | Yes | 22 (24.4) | 5 (26.3) | 17 (23.9) | 1.000 b |
| No | 68 (75.6) | 14 (73.7) | 54 (76.1) | ||
| Health Status | Good | 65 (72.2) | 13 (68.4) | 52 (73.2) | 0.677 c |
| Not good | 25 (27.8) | 6 (31.6) | 19 (26.8) | ||
| Physical Function | 5 MWT usual walk (second) | 8.2 ± 2.4 | 10.2 ± 3.3 | 7.7 ± 1.8 | <0.001 a |
| ZWT average 1st and 2nd walk (second) | 13.3 ± 4.7 | 17.1 ± 6.9 | 12.3 ± 3.3 | <0.001 a | |
| TUGT average 1st and 2nd walk (second) | 13.7 ± 4.2 | 17.1 ± 5.9 | 12.8 ± 3.1 | <0.001 a | |
| Fear of Falling | Short FES I | 11.4 ± 4.3 | 12.0 ± 4.8 | 11.3 ± 4.1 | 0.517 a |
| Gait Efficacy | mGES | 84.7 ± 15.6 | 69.4 ± 21.3 | 88.9 ± 10.6 | <0.001 a |
| Amount of Physical Activity | Number of steps (steps/day) | 3560.2 ± 3022.9 | 1029.2 ± 782.1 | 4237.5 ± 3042.5 | <0.001 a |
| Path | β (Estimator) | S.E. | p-Value |
|---|---|---|---|
| Fear of falling → Gait efficacy | −0.444 | 0.308 | <0.001 |
| Gait efficacy → Fall incidence | −0.318 | 0.003 | 0.001 |
| Amount of Physical activity → Fall incidence | −0.243 | 0.000 | 0.009 |
| Physical function→ Fall incidence | 0.233 | 0.011 | 0.020 |
| Gait efficacy → Amount of Physical activity | 0.283 | 20.700 | 0.008 |
| Physical function → Gait efficacy | −0.369 | 0.370 | <0.001 |
| Physical activity → Physical function | −0.236 | 0.000 | 0.038 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nur’amalia, R.; Kato, M.; Yokogawa, M.; Taniguchi, Y.; Irwan, A.M. Investigating Fall-Related Factors in Community-Dwelling Older Women Through Structural Equation Modeling Analysis. Int. J. Environ. Res. Public Health 2025, 22, 906. https://doi.org/10.3390/ijerph22060906
Nur’amalia R, Kato M, Yokogawa M, Taniguchi Y, Irwan AM. Investigating Fall-Related Factors in Community-Dwelling Older Women Through Structural Equation Modeling Analysis. International Journal of Environmental Research and Public Health. 2025; 22(6):906. https://doi.org/10.3390/ijerph22060906
Chicago/Turabian StyleNur’amalia, Riskah, Mayumi Kato, Masami Yokogawa, Yoshimi Taniguchi, and Andi Masyitha Irwan. 2025. "Investigating Fall-Related Factors in Community-Dwelling Older Women Through Structural Equation Modeling Analysis" International Journal of Environmental Research and Public Health 22, no. 6: 906. https://doi.org/10.3390/ijerph22060906
APA StyleNur’amalia, R., Kato, M., Yokogawa, M., Taniguchi, Y., & Irwan, A. M. (2025). Investigating Fall-Related Factors in Community-Dwelling Older Women Through Structural Equation Modeling Analysis. International Journal of Environmental Research and Public Health, 22(6), 906. https://doi.org/10.3390/ijerph22060906








