Abstract
Climate change is among the most significant challenges of the 21st century, with global warming, heat stress, floods, and drought occurring in various parts of the globe, including Africa. The impact of climate change on health is becoming increasingly substantial on the African continent due to weaknesses in economies, infrastructure, and healthcare systems. This review explores the relationship between climate change and emerging and re-emerging infectious diseases in Africa and highlights possible solutions. It was conducted by summarizing and synthesizing related information from relevant scientific publications. This review reveals that climate change significantly contributes to Africa’s emerging and re-emerging infectious diseases, including Ebola, Marburg, Lassa fever, dengue fever, malaria, and cholera. The impact of climate change on infectious diseases is variable across the continent, with countries in West and Central Africa experiencing more significant climate change-instigated disease burdens. Multisectoral cooperation between climate change actors, environmental health researchers, policy makers, and political leaders centered in the One Health approach is necessary to develop and implement resilient interventions for climate change-induced emerging and re-emerging infections and related health hazards.
1. Introduction
The change in global climate systems owing to excessive greenhouse gas emissions is among the greatest challenges of the 21st century [1], and has significant implications for human health. Climate change impacts developing countries the most [2]. It transcends boundaries to contribute to extreme weather-induced disasters, posing systemic risks to economies, water and food systems, agriculture, infrastructure, and public health [3]. Additionally, it can aggravate over half of human pathogenic diseases through its effects on transmission pathways, resulting in pathogenic diseases, mainly bacterial and viral infectious diseases [4]. Therefore, climate change and the emergence and re-emergence of infectious diseases are interconnected.
Africa contributes the least to greenhouse gas emissions, yet it is one of the most severely climate change-impacted continents [5]. Climate change exacerbates health challenges such as malnutrition, water scarcity, and inadequate sanitation, which may contribute to the emergence and re-emergence of infectious diseases such as Zika, Rift Valley Fever, cholera, and Ebola and may compound existing ones like malaria [6,7,8]. Therefore, the health implications of climate change in Africa are significantly concerning.
Climate change significantly affects infectious diseases endemic in Africa such as Ebola, malaria, dengue fever, and cholera due to Africa’s diverse ecosystem [8]. Rising temperatures and changing rainfall patterns create favorable conditions for disease vectors such as mosquitoes and ticks [7,8,9,10]. Some diseases spread to new regions due to changes in temperature and rainfall patterns [8,11,12]. Consequently, vector-borne diseases are emerging at a high rate, with nearly a quarter of them comprising zoonotic diseases that can be traced to wildlife origins [13].
The Intergovernmental Panel on Climate Change (IPCC) noted that Africa is highly vulnerable to the health effects of climate change as early as 2001 [14]. It attributed this vulnerability to six factors, namely limited water resources; food insecurity from declining agricultural production; threats to natural resource productivity and biodiversity; vector- and water-borne diseases driven by inadequate health infrastructure; coastal areas vulnerable to sea-level rise; and worsening desertification [14]. However, previous studies have mainly focused on the impacts of climate change on health in the global North [15,16]. Therefore, similar studies are needed in Africa [17]. This narrative review summarizes and synthesizes the available scientific evidence on the relationship between climate change and emerging and re-emerging infectious diseases in Africa to contribute to a better understanding of this complex relationship, reveal evidence gaps, and possibly inform the development of policies for the prevention of infectious diseases through climate-based interventions.
2. Climate Change and the Rise of Emerging and Re-Emerging Infectious Diseases in Africa
2.1. Making the Case: The Impacts of Climate Change and Climate Hazards on the Disease Burden in Africa
United Nations Climate Change [18] observes that the warmer temperatures and higher rainfall increase in Africa facilitate the emergence of new diseases in regions where they were previously not present. The increased incidences of vector-borne diseases such as malaria and dengue are among the most significant impacts of climate change on human health in Africa since 3% of malaria-related deaths and 4% of dengue-related deaths are attributable to climate change [17]. Mosquitoes, which are the main vectors of these diseases, thrive best in environments with high temperatures and increased rainfall, which are their ideal breeding conditions [19]. The continued warming and decreasing rainfall over northern and southern Africa and the increased rainfall over the Sahel region provide such ideal breeding conditions [20]. Since projections foresee a rise of more than 2 °C in the mean annual temperature in Africa [17], the burden of vector-borne diseases is likely to increase.
Climate change is also impacting the availability of clean water and sanitation, which potentially increases the risk of water-borne diseases such as cholera, dysentery, and typhoid fever [21,22]. Scarcity of water resources due to prolonged droughts, such as in East Africa, or floods, such as in West Africa, leads to inadequate water for drinking, sanitation, and hygiene, increasing the incidence of diarrheal diseases [23]. Africa has the largest burden of food-borne diseases. This is mainly driven by the unavailability of safe water, which is worsened by global warming [23]. The limited climate resilience across Africa worsens access to clean water, hygiene infrastructure, and sanitation [24], thus increasing the incidence of water-borne diseases.
2.1.1. Climate Change and Re-Emerging Infectious Diseases
Climate change is influencing the emergence and re-emergence of infectious diseases worldwide, including in Africa [13,16,25,26]. Specifically, climate change is impacting the geographic distribution and abundance of vectors like mosquitoes and ticks, and animal hosts such as bats and rodents [25,26]. Besides spreading infections, the vectors and hosts affect human behavior and overall health. Therefore, the re-emerging infectious diseases increase the pressure on the few resources available for disease control and prevention in Africa. The lack of public health resources compromises the comprehensiveness of public health responses to emerging and re-emerging diseases [27], leading to prolonged presence and further spread of the infections.
Climate change substantially influences the occurrence of zoonotic diseases in humans. For instance, the Ebola, Marburg, and Lassa viruses originate from bats and rodents and spread to humans through contact with infected bodily fluids [28]. Climate change alters the ranges and behaviors of these animals, making it easier for them to come in contact with humans and increasing the likelihood of disease transmission [29]. Humans also invade forests and rangelands through deforestation and changes in land use in search of natural resources due to climate change-instigated deficiencies in the resources in human habitats [30]. Therefore, as climate change progresses it predisposes Africans to higher risks of zoonotic diseases.
Increased contact with non-human primates is contributing to the re-emergence of zoonoses such as yellow fever [31], which is transmitted to humans by mosquitoes after infecting non-human primates. Temperature and rainfall patterns affect mosquito abundance and distribution, while deforestation creates new habitats for non-human primates, thus enhancing the spread of viral infections like yellow fever [30]. Therefore, increasing changes in the activities of humans and non-human primates in response to environmental changes present threats for the emergence and re-emergence of zoonotic diseases.
2.1.2. Climate Hazards and Specific Infectious Diseases in Africa
The correlation between climatic hazards and infectious diseases in Africa is complex and varies by region due to diverse climatic conditions, environmental factors, and socioeconomic determinants [18]. The distribution of the climate change-influenced emergence of Ebola, Marburg, and Lassa fever in Africa varies across the continent [32,33]. Therefore, the incidences of hemorrhagic fevers due to emerging and re-emerging viruses in various regions in Africa are as diverse as the climatic conditions of the regions.
Climatic factors play a role in Ebola outbreaks in Africa even though the Ebola virus is mainly transmitted through contact with the bodily fluids of infected persons [34]. Changes in rainfall, vegetation, and forest cover affect the frequency and severity of Ebola outbreaks. For example, heavy rains cause an abundance of fruits, which provides food for natural hosts of the virus such as bats (Figure 1) [35]. During these periods, heightened interactions between humans and infected animals can lead to outbreaks [31]. Moreover, deforestation and encroachment into forested areas can contribute to the emergence and spread of Ebola [30,36]. Therefore, climate change and the resultant human activities increase the risk of Ebola in Africa.
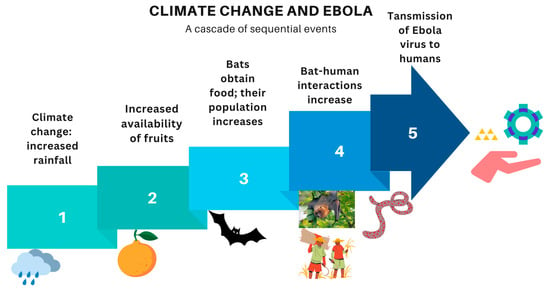
Figure 1.
An illustration of how heavy rainfall due to climate change causes Ebola outbreaks in humans.
The Marburg virus, which is in the Filoviridae family with Ebola, causes outbreaks that show some correlations with climatic factors. Marburg outbreaks are more common in locations with many natural hosts, such as fruit bats [37]. Climate-related factors such as changes in rainfall and temperature can trigger ecological changes, including alterations in the distribution and behavior of bats [38]. For example, a species of bat, Rousettus aegyptiacus, increases its activity in residential areas during cold seasons, thus increasing the likelihood of transfer of the Marburg virus from them to humans [39]. Outbreaks have been reported in different countries, each with unique characteristics, including climatic and ecological factors, making it challenging to identify consistent regional patterns.
The presence of the Lassa virus, a member of the family Arenaviridae that is rodent-transmitted, mainly in West Africa as a cause of hemorrhagic fevers in humans, could be influenced by climate change [40]. While the relationship between climatic hazards and Lassa fever is not as well established as with Ebola and Marburg, correlations between climate change and the incidence of Lassa fever have been observed [41]. During the dry season in West Africa, which is associated with an increase in Lassa fever cases, rodents—the primary carriers of the virus—may seek food and shelter in human dwellings due to a scarcity of food resources, increasing the chances of human contact and transmission [42].
Meteorological factors influence the incidence of Mpox, an infectious zoonotic disease caused by the Mpox virus of the family Poxviridae. Key meteorological variables such as temperature, humidity, and precipitation significantly affect the transmission dynamics of Mpox [43]. Warmer temperatures and changing rainfall patterns may alter the distribution and survival of the primary reservoir hosts—rodents—potentially increasing human exposure. Additionally, deforestation and habitat loss, which are exacerbated by climate change, drive wildlife, including rodents and non-human primates, closer to human settlements, increasing the risk of zoonotic spillovers such as Mpox [31]. A recent study that analyzed data from 52 countries on daily confirmed Mpox cases while considering climate types, the mean surface air temperature, and precipitation found that temperature and precipitation significantly impacted Mpox prevalence in South America [44]. Hence, Mpox outbreaks are likely to increase as climate change causes adverse weather conditions.
Climate hazards significantly compound malaria in the malarious regions of Africa, where malaria is already a leading cause of morbidity and mortality. Most of the two million additional malaria cases in 84 malaria-endemic countries between 2020 and 2021 were in Africa, with countries in Western Africa leading in age-standardized incidence rates and mortality rates [45]. Malaria epidemics often happen after periods of heavy rainfall and rising temperatures in the tropics, which allow malaria-carrying mosquitoes to survive at higher altitudes [18]. Malaria incidence rates in Africa largely declined from 2000 to 2018 in a temperature-dependent manner; countries such as Uganda and Mozambique reported high incidence rates [46]. Climate-based modeling predictions show that the prevalence of malaria is likely to diminish in the near and far futures in West Africa as the climate in the Sahel region becomes unsuitable for Anopheles mosquitoes [47]. Therefore, the fight against malaria in Africa is likely to benefit from climate change.
Dengue fever, another mosquito-borne viral disease, is also becoming a significant public health threat in Africa in the context of climate change. Temperature and dengue incidence are positively correlated [48]. Hence, the prevalence of dengue is likely to increase as global warming occurs. According to the World Health Organization (WHO) [49], dengue incidences have grown dramatically worldwide in recent decades, with cases reported to the WHO increasing from 505,430 in 2000 to 5.2 million in 2019. Recent dengue fever outbreaks in East and West Africa have been linked to rising temperatures and rainfall [50]. Critically, the risks of dengue fever may change in tropical and subtropical areas as vectors thrive in environments that are altered by climate change [48]. Therefore, dengue-endemic regions are expected to expand in the face of climate change, which favors the vector dynamics of Aedes mosquitoes.
Cholera, a water-borne disease, is also closely linked to climatic hazards. Over a quarter million cases of cholera were reported in 19 African countries between January 2023 and January 2024 [51]. Frequent and severe floods contaminate water sources with fecal matter, increasing the risk of cholera outbreaks [52]. In displacement camps established to respond to climate change-related disasters, cholera is the most common cause of outbreaks with fecal–oral transmission [53]. Access to clean water and healthcare services is reduced with the destruction of infrastructure due to floods, landslides, and other climate change-related emergencies [52], further exacerbating the spread of cholera. The Southern African Development Community (SADC) recommended the inclusion of climate change-targeting interventions in the multisectoral response to cholera re-emergence as peak numbers of cholera cases and deaths were reported in their member states [51].
2.2. Health Systems and Social Implications of Climate Change-Triggered Emerging and Re-Emerging Infectious Diseases
Climatic hazards can lead to disruptions of routine healthcare services and disorient social systems [54,55]. Extreme weather events can displace populations, destroy health facilities, and disrupt healthcare services. Thus, they can decrease the availability of essential health services, with long-term implications for the health of populations [56], especially for vulnerable groups such as children and pregnant women.
The increased burden of infectious disease outbreaks due to climate change can lead to increased healthcare costs, reduced productivity, and decreased economic growth [57]. Agriculture, which is the economic backbone of the West African countries affected by Ebola, significantly deteriorates as farmers abandon their farms to avoid infection [58]. According to Smith et al. [57], the Ebola epidemic in West Africa demonstrated the serious and unanticipated economic toll of an emerging infectious disease. For example, Liberia’s Gross Domestic Product (GDP) decreased from 8.7% to 0.7% due to Ebola and lowered commodity prices while in Sierra Leone (excluding iron ore) the GDP decreased from 5.3% to 0.8% [57]. Therefore, climate change-related Ebola outbreaks are economically costly and can exacerbate existing social inequalities, leading to a cycle of poverty and ill health.
2.3. Key Challenges and Trends in Climate Change-Triggered Infectious Diseases
Reports of flood events have increased, with Nigeria experiencing its worst flood in 2022, losing more than 610 people [59]. In March 2023, severe flooding killed dozens and affected more than 300, 000 in Ethiopia and Somalia [60]. Such disaster events lead to loss of life, destruction of property, displacement of people, and increases in infectious disease burdens, as experienced by countries like Guinea, Mali, Sierra Leone, Burkina Faso, Ghana, Niger, the Central African Republic, and Nigeria [59]. Hence, heavy floods not only increase the emergence and re-emergence of infectious diseases but also limit countries’ capacities to respond to the diseases due to the economic implications of flooding.
Perpetual droughts co-occur with floods in Africa, which further threatens humanity, fauna, and flora. Consequently, the prevalence of vectors that thrive in dry conditions increases. For example, sandflies breed in dry conditions and bite humans to transmit Leishmania species, causing Leishmaniasis [61]. Rodents migrate to homesteads during drought seasons in search of water and food, thus increasing the occurrence of infections such as hantavirus, the plague, and leptospirosis [62]. Fecal–oral transmission of waterborne pathogens such as Vibrio cholerae and Shigella species increases during droughts due to the scarcity of drinking water. Thus, diarrheal diseases are common during droughts [63]. As a result, the burden of emerging and re-emerging diseases is increasing as climate change-driven drought seasons hit Africa, considering that most countries have poor sewerage and sanitation systems.
3. Mitigating the Impacts of Climate-Induced Health Hazards
African countries must undertake deliberate actions to mitigate the impacts of climate-induced health hazards. A One Health approach that transcends human health, animal health, and the environment is recommended for coordinated mitigation and adaption [64]. The first action would be implementing climate-resilient health systems [65]. African states must integrate climate adaptation into health system planning, resource allocation, and service delivery, including investment in infrastructure and health workforce development, ensuring access to essential medicines and supplies and establishing effective disease surveillance and response systems [66]. Secondly, community-based health programs should be strengthened since they provide a country’s first line of defense against infectious diseases. Governments should prioritize inclusive community-based health programs that engage local communities in identifying, preventing, and managing climate-induced health hazards [67].
Thirdly, fighting climate change-triggered infectious diseases necessitates improving water, sanitation, and hygiene (WASH) infrastructure. African countries should invest in climate-resilient WASH infrastructure, including sustainable safe water supplies, sanitation facilities, and hygiene promotion programs, to prevent water-borne diseases and improve health outcomes [68]. Protecting the WASH infrastructure from climate hazards calls for the establishment of early warning systems that integrate meteorological, environmental, and health data to enhance the detection of climate-induced health hazards and to respond promptly and effectively [69]. Therefore, early warning systems slow the spread of infectious diseases by protecting and optimizing the utility of the available resources.
Additionally, African countries should promote research and innovation in developing new vaccines, diagnostic tools, and treatments for climate-sensitive diseases and should explore innovative approaches to health service delivery [70]. They can leverage regional and international collaboration to learn from countries that affordably established diagnostic and vaccine manufacturing systems in response to the COVID-19 pandemic for the cost-effective manufacture of vaccines, tests, and drugs [71]. This includes establishing partnerships with research institutions, donor agencies, and international organizations to develop and implement climate-resilient health programs [72]. Developments should consider social determinants of health such as poverty to ensure accessibility and affordability of the innovative drugs, vaccines, and tests for most Africans in the African Continental Free Trade Area (AfCFTA), thus promoting universal healthcare and reducing dependency on imports. Overall, all interventions require sustained political commitment, investment, and collaboration at both the national and international levels for long-term results [73]. Therefore, multisectoral stakeholders should collaborate with African governments to design systems that will address the effects of climate change and create robust systems to withstand those effects and possibly reverse them (Figure 2).
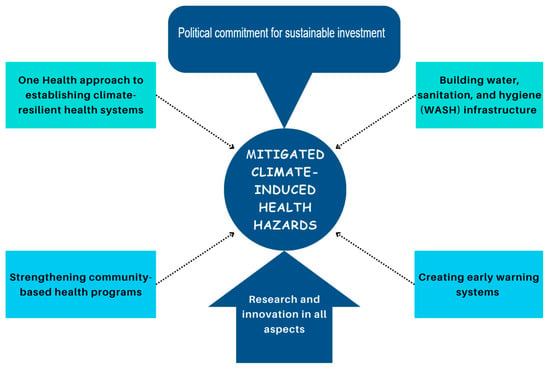
Figure 2.
A mind-map showing a multi-pronged approach to mitigating climate-induced health hazards.
4. Conclusions
This review highlights the relationship between climate change and emerging and re-emerging infectious diseases in Africa. It shows that climate change and climate hazards have substantial effects on the emergence and re-emergence of infectious diseases, particularly vector-borne diseases and diseases with fecal–oral transmission, in Africa. While some regional similarities exist in the correlations between climatic hazards and infectious diseases in Africa, the impact can vary by region due to the diversity of environmental, economic, and political factors. Climate hazards disrupt routine healthcare services, economic systems, and social structures. Thus, a multisectoral approach that involves strengthening public health systems, improving access to clean water and sanitation, and developing early warning systems to identify and respond to disease outbreaks is essential. Strengthening regional and international collaboration related to research, policy development, and technological advancements and political commitments related to establishing resilience to climate-induced health hazards in Africa should also be prioritized.
Author Contributions
Conceptualization, R.K.D.A. and K.B.N.; methodology, R.K.D.A., D.K. and K.B.N.; resources, K.B.N.; writing—original draft preparation, R.K.D.A. and D.K.; writing—review and editing, R.K.D.A., D.K. and K.B.N.; visualization, D.K. and K.B.N.; supervision, K.B.N.; project administration, K.B.N.; funding acquisition, K.B.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the World Health Organization Regional Office for Africa and “The APC was funded by World Health Organization Regional Office for Africa”.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
We acknowledge the WHO Regional Office for Africa for its support in accessing full-text articles when conducting this literature review.
Conflicts of Interest
D.K. is the director of Medright Consulting LTD but he co-authored this manuscript as an independent consultant. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The funders had no role in the design of this study; the collection, analyses, or interpretation of the data; the writing of the manuscript; or the decision to publish the results.
Abbreviations
The following abbreviations are used in this manuscript:
| AfCFTA | African Continental Free Trade Area |
| COVID-19 | Coronavirus Disease 2019 |
| GDP | Gross Domestic Product |
| IPCC | Intergovernmental Panel on Climate Change (IPCC) |
| Mpox | Monkey Pox |
| SADC | Southern African Development Community |
| WASH | water, sanitation, and hygiene |
| WHO | World Health Organization |
References
- Kabir, M.; Habiba, U.E.; Khan, W.; Shah, A.; Rahim, S.; De los Rios-Escalante, P.R.; Farooqi, Z.U.R.; Ali, L. Climate change due to increasing concentration of carbon dioxide and its impacts on environment in 21st century; a mini review. J. King Saud Univ. Sci. 2023, 35, 102693. [Google Scholar] [CrossRef]
- Chinowsky, P.; Hayles, C.; Schweikert, A.; Strzepek, N.; Strzepek, K.; Schlosser, C.A. Climate change: Comparative impact on developing and developed countries. Eng. Proj. Organ. J. 2011, 1, 67–80. [Google Scholar] [CrossRef]
- Rocque, R.J.; Beaudoin, C.; Ndjaboue, R.; Cameron, L.; Poirier-Bergeron, L.; Poulin-Rheault, R.A.; Fallon, C.; Tricco, A.C.; Witteman, H.O. Health effects of climate change: An overview of systematic reviews. BMJ Open 2021, 11, e046333. [Google Scholar] [CrossRef] [PubMed]
- Mora, C.; McKenzie, T.; Gaw, I.M.; Dean, J.M.; von Hammerstein, H.; Knudson, T.A.; Setter, R.O.; Smith, C.Z.; Webster, K.M.; Patz, J.A.; et al. Over half of known human pathogenic diseases can be aggravated by climate change. Nat. Clim. Change 2022, 12, 869–875. [Google Scholar] [CrossRef]
- Althor, G.; Watson, J.E.M.; Fuller, R.A. Global mismatch between greenhouse gas emissions and the burden of climate change. Sci. Rep. 2016, 6, 20281. [Google Scholar] [CrossRef]
- Lafferty, K.D. The ecology of climate change and infectious diseases. Ecology 2009, 90, 888–900. [Google Scholar] [CrossRef]
- Wu, X.; Lu, Y.; Zhou, S.; Chen, L.; Xu, B. Impact of climate change on human infectious diseases: Empirical evidence and human adaptation. Environ. Int. 2016, 86, 14–23. [Google Scholar] [CrossRef]
- Kurane, I. The Effect of Global Warming on Infectious Diseases. Osong Public Health Res. Perspect. 2010, 1, 4–9. [Google Scholar] [CrossRef]
- Semenza, J.C.; Rocklöv, J.; Ebi, K.L. Climate Change and Cascading Risks from Infectious Disease. Infect. Dis. Ther. 2022, 11, 1371–1390. [Google Scholar] [CrossRef]
- Medlock, J.M.; Leach, S.A. Effect of climate change on vector-borne disease risk in the UK. Lancet Infect. Dis. 2015, 15, 721–730. [Google Scholar] [CrossRef]
- Caminade, C.; McIntyre, K.M.; Jones, A.E. Impact of recent and future climate change on vector-borne diseases. Ann. N. Y. Acad. Sci. 2019, 1436, 157–173. [Google Scholar] [CrossRef] [PubMed]
- Hauser, N.; Conlon, K.C.; Desai, A.; Kobziar, L.N. Climate Change and Infections on the Move in North America. Infect. Drug Resist. 2021, 14, 5711–5723. [Google Scholar] [CrossRef] [PubMed]
- Chala, B.; Hamde, F. Emerging and Re-emerging Vector-Borne Infectious Diseases and the Challenges for Control: A Review. Front. Public Health 2021, 9, 715759. [Google Scholar] [CrossRef]
- IPCC. AR5 Climate Change 2014: Impacts, Adaptation, and Vulnerability. 2014. Available online: https://www.ipcc.ch/site/assets/uploads/2018/02/WGIIAR5-PartB_FINAL.pdf (accessed on 5 February 2024).
- Hoogeveen, D.; Atleo, C.G.; Patrick, L.; Kennedy, A.M.; Leduc, M.; Parkes, M.W.; Takaro, T.K.; Gislason, M.K. On the possibility of decolonising planetary health: Exploring new geographies for collaboration. Lancet Planet. Health 2023, 7, e179–e183. [Google Scholar] [CrossRef]
- Kulkarni, M.A.; Duguay, C.; Ost, K. Charting the evidence for climate change impacts on the global spread of malaria and dengue and adaptive responses: A scoping review of reviews. Glob. Health 2022, 18, 1. [Google Scholar] [CrossRef]
- Giesen, C.; Roche, J.; Redondo-Bravo, L.; Ruiz-Huerta, C.; Gomez-Barroso, D.; Benito, A.; Herrador, Z. The impact of climate change on mosquito-borne diseases in Africa. Pathog. Glob. Health 2020, 114, 287–301. [Google Scholar] [CrossRef]
- World Meteorological Organization. State of the Climate in Africa; WMO: Geneva, Switzerland, 2020; Available online: https://library.wmo.int/viewer/57196/download?file=1253_en_%282%29.pdf&type=pdf&navigator=1 (accessed on 6 March 2024).
- Khezzani, B.; Baymakova, M.; Khechekhouche, E.A.; Tsachev, I. Global warming and mosquito-borne diseases in Africa: A narrative review. Pan Afr. Med. J. 2023, 44, 70. [Google Scholar] [CrossRef]
- Acosta, D.; Barrow, A.; Mahamadou, I.S.; Assuncao, V.S.; Edwards, M.E.; McKune, S.L. Climate change and health in the Sahel: A systematic review. R. Soc. Open Sci. 2024, 11, 231602. [Google Scholar] [CrossRef]
- Davies, G.I.; McIver, L.; Kim, Y.; Hashizume, M.; Iddings, S.; Chan, V. Water-borne diseases and extreme weather events in Cambodia: Review of impacts and implications of climate change. Int. J. Environ. Res. Public Health 2015, 12, 191–213. [Google Scholar] [CrossRef]
- Williams, P.C.M.; Bartlett, A.W.; Howard-Jones, A.; McMullan, B.; Khatami, A.; Britton, P.N.; Marais, B.J. Impact of climate change and biodiversity collapse on the global emergence and spread of infectious diseases. J. Paediatr. Child Health 2021, 57, 1811–1818. [Google Scholar] [CrossRef]
- Cissé, G. Food-borne and water-borne diseases under climate change in low- and middle-income countries: Further efforts needed for reducing environmental health exposure risks. Acta Trop. 2019, 194, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.; Colwell, R. Climate change and the resurgence of waterborne diseases: Focus on Sub-Saharan Africa. Field Actions Sci. Rep. 2025, 27, 66–70. Available online: http://journals.openedition.org/factsreports/ (accessed on 6 February 2025).
- El-sayed, A.; Kamel, M. Climatic changes and their role in emergence and re-emergence of diseases. Environ. Sci. Pollut. Res. 2020, 27, 22336–22352. [Google Scholar] [CrossRef]
- Ashraf, A.; Darzi, M.M.; Wani, B.M. Climate change and infectious diseases of animals: A review. J. Entomol. Zool. Stud. 2017, 5, 1470–1477. [Google Scholar]
- Polgreen, P.M.; Polgreen, E.L. Emerging and re-emerging pathogens and diseases, and health consequences of a changing climate. In Infectious Diseases; Elsevier: Amsterdam, The Netherlands, 2016; pp. 41–48. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC7149782/pdf/main.pdf (accessed on 5 February 2025).
- Edward, M.; Heniedy, A.M.; Saminu, A.; Florence, J.J.; Ahmed, D.A.; Engmann, S.T.; Onyeaghala, C.; Ahmed, D.A.; Engmann, S.T.; Onyeaghala, C.; et al. Climate change and contagion: The emerging threat of zoonotic diseases in Africa. Infect. Ecol. Epidemiol. 2025, 15, 2441534. [Google Scholar] [CrossRef]
- Pecl, G.T.; Araújo, M.B.; Bell, J.D.; Blanchard, J.; Bonebrake, T.C.; Chen, I.; Clark, T.D.; Colwell, R.K.; Danielsen, F.; Evengård, B.; et al. Biodiversity redistribution under climate change: Impacts on ecosystems and human well-being. Science 2017, 355, eaai9214. [Google Scholar] [CrossRef]
- Tazerji, S.S.; Nardini, R.; Safdar, M.; Shehata, A.A.; Magalh, P. An Overview of Anthropogenic Actions as Drivers for Emerging and Re-Emerging Zoonotic Diseases. Pathogens 2022, 11, 1376. [Google Scholar] [CrossRef]
- Liang, J.; Wang, X.; Wu, Z.; Hao, Q.; Liu, X. Biological invasions facilitate zoonotic disease emergences. Nat. Commun. 2022, 13, 1762. [Google Scholar] [CrossRef]
- Talisuna, A.O.; Okiro, E.A.; Yahaya, A.A.; Stephen, M.; Bonkoungou, B.; Musa, E.O.; Minkoulou, E.M.; Okeibunor, J.; Impouma, B.; Djingarey, H.M.; et al. Spatial and temporal distribution of infectious disease epidemics, disasters and other potential public health emergencies in the World Health Organisation Africa region, 2016–2018. Glob. Health 2020, 16, 9. [Google Scholar] [CrossRef]
- Bagcchi, S. News Haemorrhagic fevers in Africa. Lancet Microbe 2021, 2, e496. [Google Scholar] [CrossRef]
- Juga, M.L.; Nyabadza, F.; Chirove, F. An Ebola virus disease model with fear and environmental transmission dynamics. Infect. Dis. Model. 2021, 6, 545–559. [Google Scholar] [CrossRef] [PubMed]
- Howard, C.R.; Fletcher, N.F.; Howard, C.R.; Fletcher, N.F. Emerging virus diseases: Can we ever expect the unexpected ? Emerging virus diseases: Can we ever expect the unexpected ? Emerg. Microbes Infect. 2012, 1, 1–9. [Google Scholar] [CrossRef]
- Lindahl, J.F.; Grace, D. The consequences of human actions on risks for infectious diseases: A review. Infect. Ecol. Epidemiol. 2015, 5, 30048. [Google Scholar] [CrossRef] [PubMed]
- Pigott, D.M.; Golding, N.; Mylne, A.; Huang, Z.; Weiss, D.J.; Brady, O.J. Mapping the zoonotic niche of Marburg virus disease in Africa. Trans. R. Soc. Trop. Med. Hyg. 2015, 109, 366–378. [Google Scholar] [CrossRef]
- Mcmichael, A.J.; Lindgren, E. Climate change: Present and future risks to health, and necessary responses. J. Intern. Med. 2011, 270, 401–413. [Google Scholar] [CrossRef]
- Wood, M.R.; Vries, J.L.D.; Epstein, J.H.; Markotter, W. Variations in small-scale movements of, Rousettus aegyptiacus, a Marburg virus reservoir across a seasonal gradient. Front. Zool. 2023, 20, 23. [Google Scholar] [CrossRef]
- Happi, A.N.; Happi, C.T.; Schoepp, R.J. Lassa Fever Diagnostics: Past, Present, and Future. Curr. Opin. Virol. 2019, 37, 132–138. [Google Scholar] [CrossRef]
- Redding, D.W.; Gibb, R.; Dan-nwafor, C.C.; Ilori, E.A.; Yashe, R.U.; Oladele, S.H.; Amedu, M.O.; Iniobong, A.; Att, L.A.; Donnelly, C.A.; et al. Geographical drivers and climate-linked dynamics of Lassa fever in Nigeria. Nat. Commun. 2021, 12, 5759. [Google Scholar] [CrossRef]
- Fichet-calvet, E.; Rogers, D.J. Risk Maps of Lassa Fever in West Africa. PLoS Negl. Trop. Dis. 2009, 3, e388. [Google Scholar] [CrossRef]
- Islam, M.A.; Sangkham, S.; Tiwari, A.; Vadiati, M.; Hasan, M.N.; Noor, S.T.A.; Mumin, J.; Bhattacharya, P.; Sherchan, S.P. Association between Global Monkeypox Cases and Meteorological Factors. Int. J. Environ. Res. Public Health 2022, 19, 15638. [Google Scholar] [CrossRef]
- Ojo, I.S.; Badero, O.J.; Rahman, M.A.; Aderinto, N.; Oral, O.; Robin, R.C.; Dansu, E.J.; Ogunjimi, T.; Ibidun, F. Impact of climatic variations on the global distribution and prevalence of Mpox disease: Analysis of data from 52 countries using linear regression and time forecasting analyses. medRxiv 2025. [Google Scholar] [CrossRef]
- Shi, D.; Wei, L.; Liang, H.; Yan, D.; Zhang, J.; Wang, Z. Trends of the Global, Regional and National Incidence, Mortality, and Disability-Adjusted Life Years of Malaria, 1990–2019: An Analysis of the Global Burden of Disease Study 2019. Risk Manag. Healthc. Policy 2023, 16, 1187–1201. [Google Scholar] [CrossRef] [PubMed]
- Leal Filho, W.; May, J.; May, M.; Nagy, G.J. Climate change and malaria: Some recent trends of malaria incidence rates and average annual temperature in selected sub-Saharan African countries from 2000 to 2018. Malar. J. 2023, 22, 248. [Google Scholar] [CrossRef] [PubMed]
- Diouf, I.; Adeola, A.M.; Abiodun, G.J.; Lennard, C.; Shirinde, J.M.; Yaka, P.; Ndione, J.A.; Gbobaniyi, E.O. Impact of future climate change on malaria in West Africa. Theor. Appl. Climatol. 2022, 147, 853–865. [Google Scholar] [CrossRef]
- Feng, F.; Ma, Y.; Qin, P.; Zhao, Y.; Liu, Z.; Wang, W.; Cheng, B. Temperature-Driven Dengue Transmission in a Changing Climate: Patterns, Trends, and Future Projections. GeoHealth 2024, 8, e2024GH001059. [Google Scholar] [CrossRef]
- World Health Organization. Dengue and severe dengue. In News; WHO: Geneva, Switzerland, 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue (accessed on 5 February 2025).
- Mwanyika, G.O.; Mboera, L.E.G.; Rugarabamu, S.; Ngingo, B.; Sindato, C.; Lutwama, J.J.; Paweska, J.T.; Misinzo, G. Dengue virus infection and associated risk factors in africa: A systematic review and meta-analysis. Viruses 2021, 13, 536. [Google Scholar] [CrossRef]
- Kaseya, J.; Dereje, N.; Tajudeen, R.; Ngongo, A.N.; Ndembi, N.; Fallah, M.P. Climate change and malaria, dengue and cholera outbreaks in Africa: A call for concerted actions. BMJ Glob. Health 2024, 9, e015370. [Google Scholar] [CrossRef]
- Acosta-España, J.D.; Romero-Alvarez, D.; Luna, C.; Rodriguez-Morales, A.J. Infectious disease outbreaks in the wake of natural flood disasters: Global patterns and local implications. Infez. Med. 2024, 32, 451–462. [Google Scholar] [CrossRef]
- Jaber, T.; Boelee, E.; Bleser, J.; Bartram, J.K. Outbreaks of faecal-orally transmitted diseases in displacement camps: A scoping review of pathogens, risk factors, exposure routes, and drivers of transmission. Glob. Public Health 2024, 19, 2380847. [Google Scholar] [CrossRef]
- Ramana Dhara, V.; Schramm, P.J.; Luber, G. Climate change & infectious diseases in India: Implications for health care providers. Indian J. Med. Res. 2013, 138, 847–852. Available online: https://journals.lww.com/ijmr/fulltext/2013/38060/climate_change___infectious_diseases_in_india_.8.aspx (accessed on 5 February 2025).
- Machalaba, C.; Romanelli, C.; Stoett, P.; Baum, S.E.; Bouley, T.A.; Daszak, P.; Karesh, W.B. Climate change and health: Transcending silos to find solutions. Ann. Glob. Health 2015, 81, 445–458. [Google Scholar] [CrossRef]
- Romanello, M.; Di Napoli, C.; Drummond, P.; Green, C.; Kennard, H.; Lampard, P.; Scamman, D.; Arnell, N.; Ayeb-Karlsson, S.; Ford, L.B.; et al. The 2022 report of the Lancet Countdown on health and climate change: Health at the mercy of fossil fuels. Lancet 2022, 400, 1619–1654. [Google Scholar] [CrossRef]
- Smith, K.M.; Machalaba, C.C.; Seifman, R.; Feferholtz, Y.; Karesh, W.B. Infectious disease and economics: The case for considering multi-sectoral impacts. One Health 2019, 7, 100080. [Google Scholar] [CrossRef]
- Omoleke, S.A.; Mohammed, I.; Saidu, Y.; Health, W.; Ive, O. Ebola viral disease in West Africa: A threat to global health, economy and political stability. J. Public Health Afr. 2016, 7, 534. [Google Scholar] [CrossRef]
- Opoku, S.K.; Filho, W.L.; Hubert, F.; Adejumo, O. Climate change and health preparedness in Africa: Analysing trends in six African countries. Int. J. Environ. Res. Public Health 2021, 18, 4672. [Google Scholar] [CrossRef]
- NASA. Heavy Rains Hit Drought-Stricken Horn of Africa. Earth Observatory. Available online: https://earthobservatory.nasa.gov/images/151208/heavy-rains-hit-drought-stricken-horn-of-africa (accessed on 5 February 2025).
- Trájer, A.J.; Ali, R. The potential effects of climate change on the climatic suitability patterns of the Western Asian vectors and parasites of cutaneous leishmaniasis in the mid- and late twenty—First century. Theor. Appl. Climatol. 2024, 155, 1897–1914. [Google Scholar] [CrossRef]
- Mgode, G.F.; Mhamphi, G.G.; Massawe, A.W.; Machang, R.S. Leptospira Seropositivity in Humans, Livestock and Wild Animals in a Semi-Arid Area of Tanzania. Pathogens 2021, 10, 696. [Google Scholar] [CrossRef]
- Alexander, K.A.; Heaney, A.K.; Shaman, J. Hydrometeorology and flood pulse dynamics drive diarrheal disease outbreaks and increase vulnerability to climate change in surface-water-dependent populations: A retrospective analysis. PLoS Med. 2018, 15, e1002688. [Google Scholar] [CrossRef]
- Gebreyes, W.A.; Dupouy-Camet, J.; Newport, M.J.; Oliveira, C.J.B.; Schlesinger, L.S.; Saif, Y.M.; Kariuki, S.; Saif, L.J.; Saville, W.; Wittum, T.; et al. The Global One Health Paradigm: Challenges and Opportunities for Tackling Infectious Diseases at the Human, Animal, and Environment Interface in Low-Resource Settings. PLoS Negl. Trop. Dis. 2014, 8, e3257. [Google Scholar] [CrossRef]
- Blom, I.M.; Beagley, J.; Quintana, A.V. The COP26 health commitments: A springboard towards environmentally sustainable and climate-resilient health care systems? J. Clim. Change Health 2022, 6, 100136. [Google Scholar] [CrossRef]
- Ansah, E.W.; Amoadu, M.; Obeng, P.; Sarfo, J.O. Health systems response to climate change adaptation: A scoping review of global evidence. BMC Public Health 2024, 24, 2015. [Google Scholar] [CrossRef] [PubMed]
- Amnuaylojaroen, T.; Parasin, N. Human health adaptation strategies to climate-induced extreme weather events: A systematic review. Earth 2024, 5, 724–742. [Google Scholar] [CrossRef]
- Liu, Q.; Deng, J.; Yan, W.; Qin, C.; Du, M.; Wang, Y.; Zhang, S.; Liu, M.; Liu, J. Burden and trends of infectious disease mortality attributed to air pollution, unsafe water, sanitation, and hygiene, and non-optimal temperature globally and in different socio-demographic index regions. Glob. Health Res. Policy 2024, 9, 23. [Google Scholar] [CrossRef]
- Asaaga, F.A.; Tomude, E.S.; Rickards, N.J.; Hassall, R.; Sarkar, S.; Purse, B.V. Informing climate-health adaptation options through mapping the needs and potential for integrated climate-driven early warning forecasting systems in South Asia-A scoping review. PLoS ONE 2024, 19, e0309757. [Google Scholar] [CrossRef]
- Liao, H.; Lyon, C.J.; Ying, B.; Hu, T. Climate change, its impact on emerging infectious diseases and new technologies to combat the challenge. Emerg. Microbes Infect. 2024, 13, 2356143. [Google Scholar] [CrossRef]
- Kamara, J.; Essien, U.; Labrique, A. A new era for African health systems: Market shaping and the African Continental Free Trade Area (AfCFTA). Public Health Chall. 2024, 3, e172. [Google Scholar] [CrossRef]
- Obame-Nkoghe, J.; Agossou, A.E.; Mboowa, G.; Kamgang, B.; Caminade, C.; Duke, D.C.; Githeko, A.K.; Ogega, O.M.; Engone Elloué, N.; Sarr, F.B.; et al. Climate-influenced vector-borne diseases in Africa: A call to empower the next generation of African researchers for sustainable solutions. Infect. Dis. Poverty 2024, 13, 26. [Google Scholar] [CrossRef]
- Dal, S. Africa Climate Summit 2023: Climate Change and the Social Dimension. Africania 2024, 4, 41–61. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).