The Perinatal Multisite Psychiatry Databank: A Cohort Update
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Sociodemographic Characteristics
3.2. Psychiatric History and Current Psychiatric Diagnoses
3.2.1. Personal Psychiatric History
3.2.2. Family History of Psychiatric Disorders
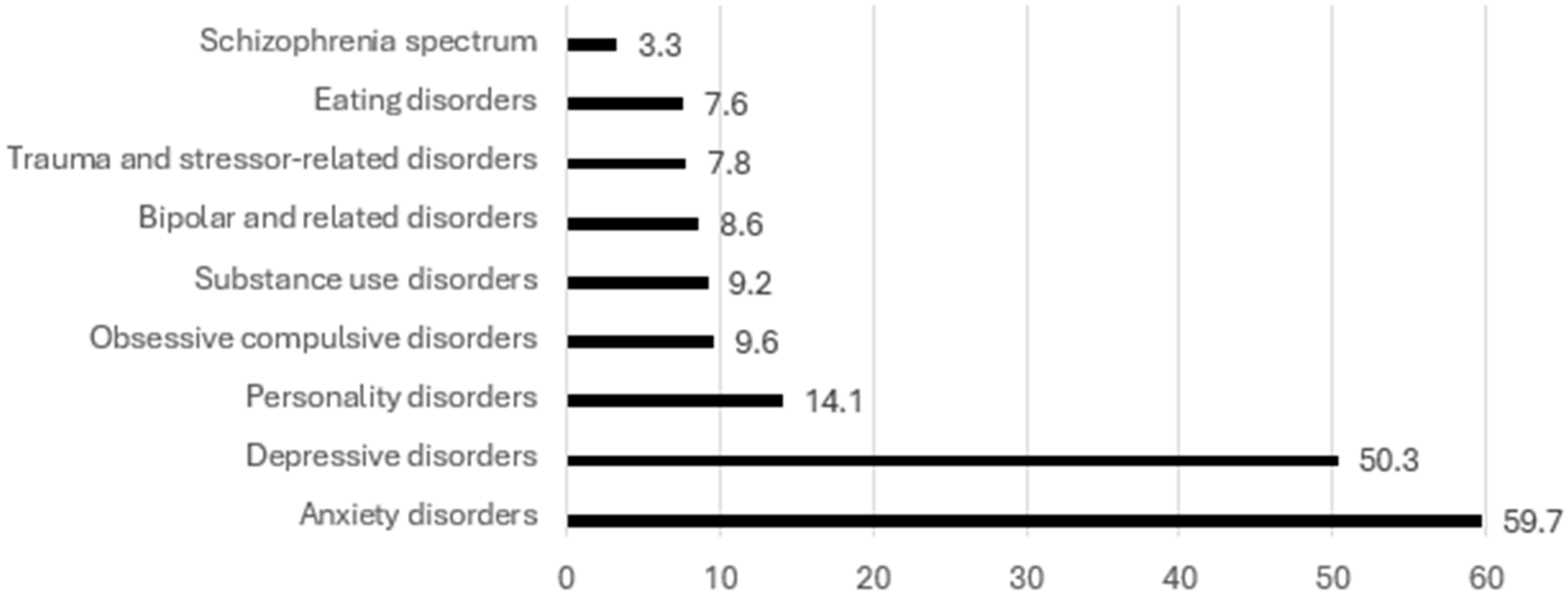
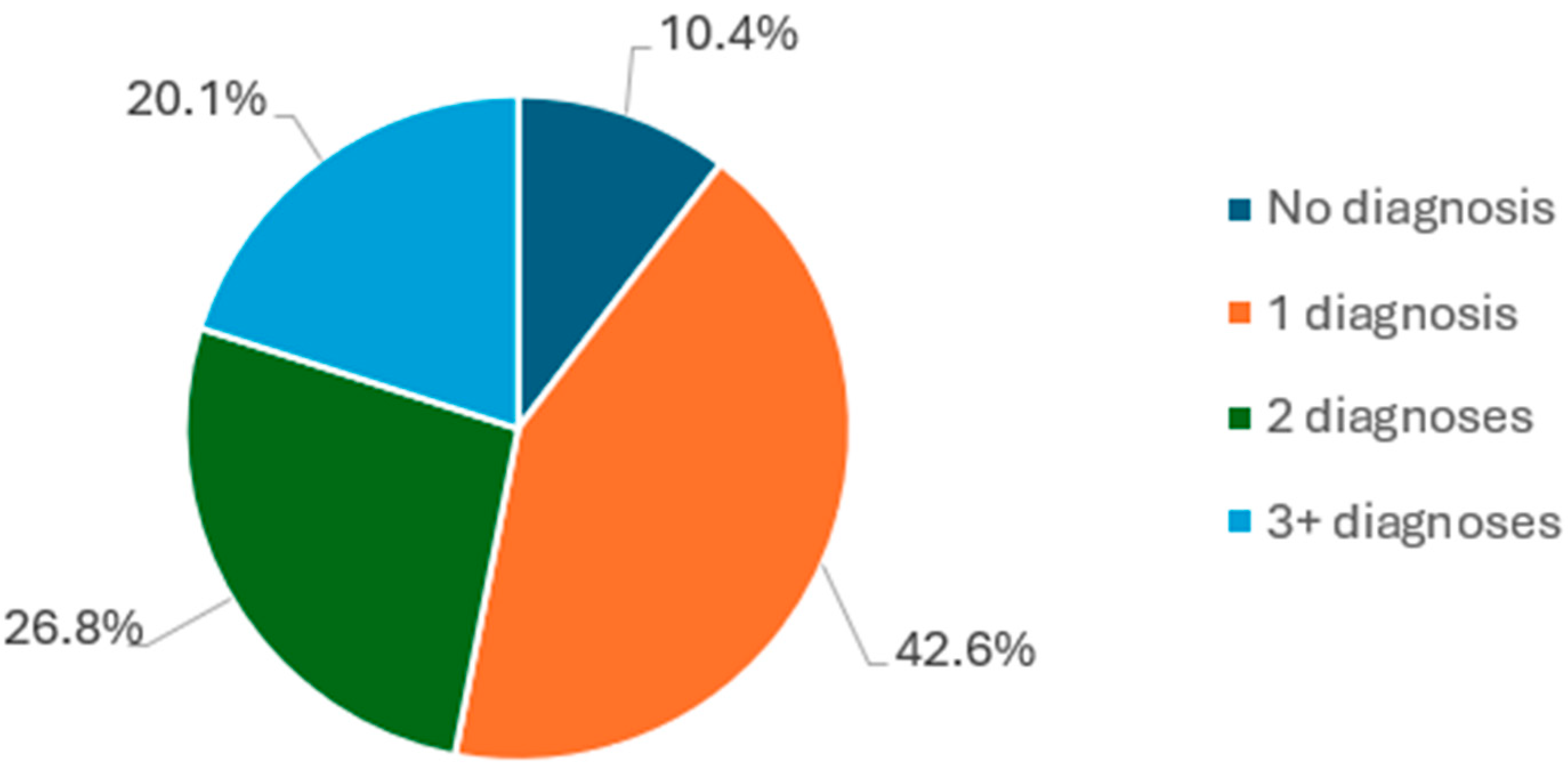
3.2.3. Current Psychiatric Diagnoses
3.3. Treatments
3.4. The Course of Perinatal Depressive and Anxiety Symptoms
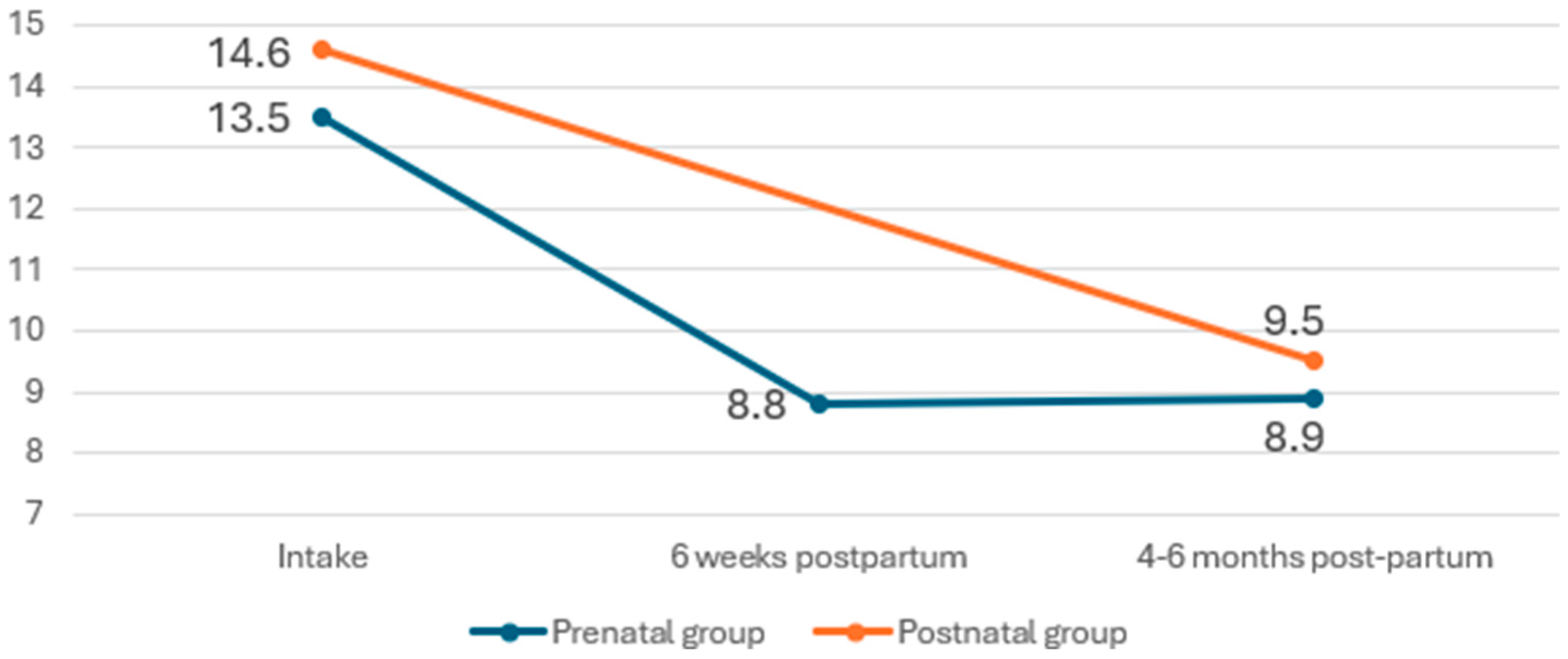
3.4.1. Depressive Symptoms
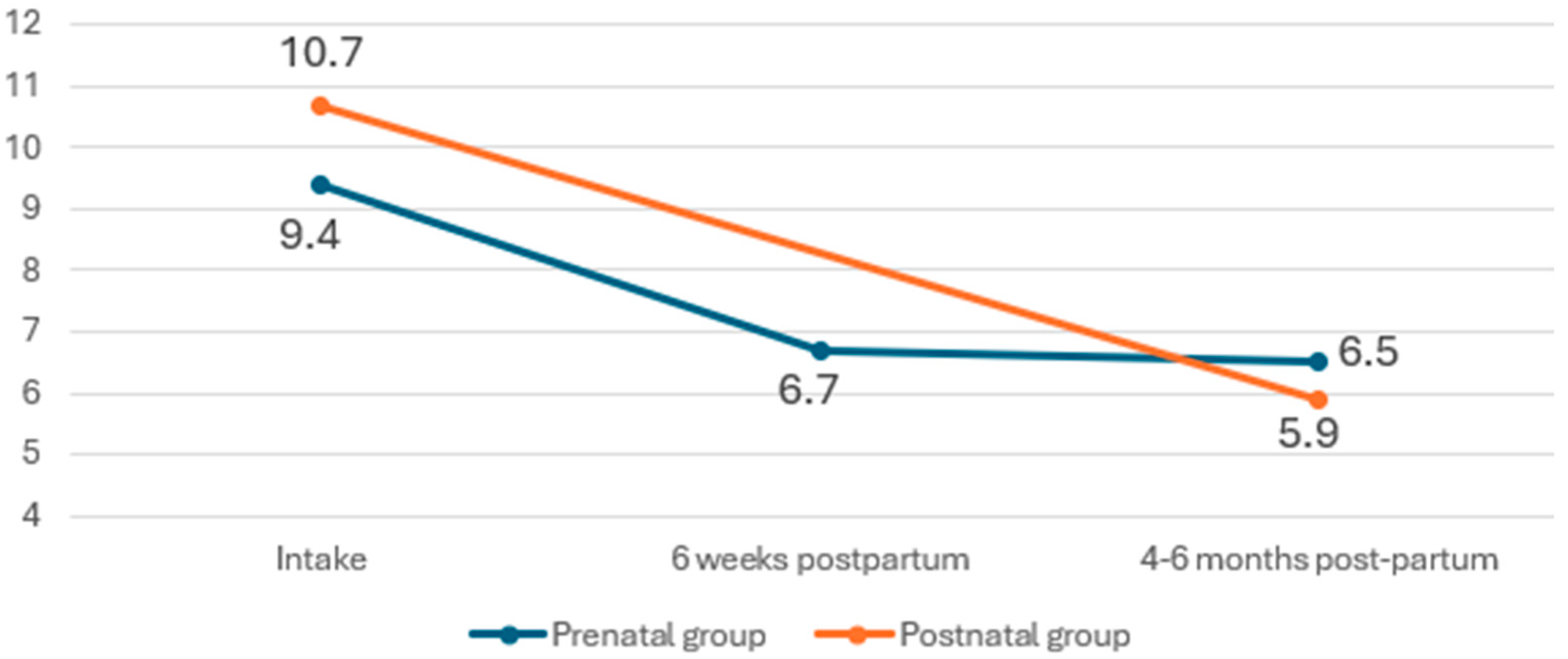
3.4.2. Anxiety Symptoms
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PMD | Perinatal Multisite Databank |
| EPDS | Edinburgh Postnatal Depression Scale |
| GAD | Generalized Anxiety Disorder |
References
- Andersson, L.; Sundström-Poromaa, I.; Wulff, M.; Aström, M.; Bixo, M. Depression and anxiety during pregnancy and six months postpartum: A follow-up study. Acta Obstet. Et Gynecol. Scand. 2006, 85, 937–944. [Google Scholar] [CrossRef]
- Maternal Mental Health in Canada, 2018/2019. Available online: https://www150.statcan.gc.ca/n1/en/daily-quotidien/190624/dq190624b-eng.pdf?st=o6Jzy_ep (accessed on 25 May 2024).
- Fawcett, E.J.; Fairbrother, N.; Cox, M.L.; White, I.R.; Fawcett, J.M. The Prevalence of Anxiety Disorders During Pregnancy and the Postpartum Period: A Multivariate Bayesian Meta-Analysis. J. Clin. Psychiatry 2019, 80, 1181. [Google Scholar] [CrossRef] [PubMed]
- Kendell, R.E.; Chalmers, J.C.; Platz, C. Epidemiology of puerperal psychoses. Br. J. Psychiatry 1987, 150, 662–673. [Google Scholar] [CrossRef] [PubMed]
- Viguera, A.C.; Whitfield, T.; Baldessarini, R.J.; Newport, D.J.; Stowe, Z.; Reminick, A.; Zurick, A.; Cohen, L.S. Risk of recurrence in women with bipolar disorder during pregnancy: Prospective study of mood stabilizer discontinuation. Am. J. Psychiatry 2007, 164, 1817–1824. [Google Scholar] [CrossRef]
- Vladimirova, R.; Stoyanova, V.; Milanova, V. Bipolar affective disorder, pregnancy and childbirth: Clinical characteristics and heredity. Biotechnol. Biotechnol. Equip. 2016, 30, 976–983. [Google Scholar] [CrossRef]
- Howard, L.M.; Khalifeh, H. Perinatal mental health: A review of progress and challenges. World Psychiatry 2020, 19, 313–327. [Google Scholar] [CrossRef] [PubMed]
- Russell, E.J.; Fawcett, J.M.; Mazmanian, D. Risk of obsessive-compulsive disorder in pregnant and postpartum women: A meta-analysis. J. Clin. Psychiatry 2013, 74, 377–385. [Google Scholar] [CrossRef]
- Friedman, S.H.; Reed, E.; Ross, N.E. Postpartum Psychosis. Curr. Psychiatry Rep. 2023, 25, 65–72. [Google Scholar] [CrossRef]
- Grigoriadis, S.; Wilton, A.S.; Kurdyak, P.A.; Rhodes, A.E.; VonderPorten, E.H.; Levitt, A.; Cheung, A.; Vigod, S.N. Perinatal suicide in Ontario, Canada: A 15-year population-based study. Can. Med. Assoc. J. 2017, 189, E1085–E1092. [Google Scholar] [CrossRef]
- Santé Mentale et Troubles Mentaux. Available online: https://www.inspq.qc.ca/sites/default/files/documents/information-perinatale/sante-mentale.pdf (accessed on 3 June 2024).
- Saharoy, R.; Potdukhe, A.; Wanjari, M.; Taksande, A.B. Postpartum Depression and Maternal Care: Exploring the Complex Effects on Mothers and Infants. Cureus 2023, 15, e41381. [Google Scholar] [CrossRef]
- Wazana, A.; Székely, E.; Oberlander, T.F. Prenatal Stress and Child Development; Springer: Cham, Switzerland, 2021. [Google Scholar]
- Weinberger, M.; Oddone, E.Z.; Henderson, W.G.; Smith, D.M.; Huey, J.; Giobbie-Hurder, A.; Feussner, J.R. Multisite Randomized Controlled Trials in Health Services Research: Scientific Challenges and Operational Issues. Med. Care 2001, 39, 627–634. [Google Scholar] [CrossRef]
- Higgins, N.; Howard, L. Database use in psychiatric research: An international review. Eur. J. Psychiatry 2005, 19, 19–30. [Google Scholar] [CrossRef]
- James, A.; Costello, M. The Benefits of Incorporating Clinical Research into Physician Practices. Available online: https://www.elligohealthresearch.com/wp-content/uploads/Elligo_PhysicianPaper_11-15-19_VF.pdf (accessed on 25 October 2024).
- Flynn, L. The Benefits and Challenges of Multisite Studies: Lessons Learned. AACN Adv. Crit. Care 2009, 20, 388–391. [Google Scholar] [CrossRef] [PubMed]
- Kattan, W.; Avigan, L.; Hayton, B.; Barkin, J.L.; St-André, M.; Nguyen, T.V.; Schwartz, H.; Poulin, M.J.; Stikarovska, I.; Wolde-Giorghis, R.; et al. Creating a Multisite Perinatal Psychiatry Databank: Purpose and Development. Int. J. Environ. Res. Public Health 2020, 17, 9352. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Population Du Québec Selon L’âge Et Le Genre. Available online: https://statistique.quebec.ca/vitrine/egalite/dimensions-egalite/demographie/population-quebec-selon-age-et-sexe?onglet=groupes-population (accessed on 2 October 2024).
- Série « Perspective Géographique », Recensement De La Population De 2021. Available online: https://www12.statcan.gc.ca/census-recensement/2021/as-sa/fogs-spg/Page.cfm?lang=F&topic=9&dguid=2021A00052466023 (accessed on 2 October 2024).
- Furtado, M.; Chow, C.H.T.; Owais, S.; Frey, B.N.; Van Lieshout, R.J. Risk factors of new onset anxiety and anxiety exacerbation in the perinatal period: A systematic review and meta-analysis. J. Affect. Disord. 2018, 238, 626–635. [Google Scholar] [CrossRef]
- Yang, K.; Wu, J.; Chen, X. Risk factors of perinatal depression in women: A systematic review and meta-analysis. BMC Psychiatry 2022, 22, 63. [Google Scholar] [CrossRef]
- Répartition De La Population De 25 à 64 ans Selon le Plus Haut Niveau De Scolarité Atteint, La Région Administrative, L’âge Et Le Sexe, Québec, 1990–2023. Available online: https://statistique.quebec.ca/fr/document/repartition-de-la-population-de-25-a-64-ans-selon-le-plus-haut-niveau-de-scolarite-atteint-la-region-administrative-lage-et-le-sexe-quebec/tableau/repartition-de-la-population-de-25-a-64-ans-selon-le-plus-haut-niveau-de-scolarite-atteint-la-region-administrative-lage-et-le-sexe-quebec#tri_tertr=50040009500000000&tri_sexe=10&tri_age=365&tri_stat=8404 (accessed on 2 October 2024).
- Silverman, M.E.; Reichenberg, A.; Savitz, D.A.; Cnattingius, S.; Lichtenstein, P.; Hultman, C.M.; Larsson, H.; Sandin, S. The risk factors for postpartum depression: A population-based study. Depress. Anxiety 2017, 34, 178–187. [Google Scholar] [CrossRef]
- ter Meulen, W.G.; Draisma, S.; van Hemert, A.M.; Schoevers, R.A.; Kupka, R.W.; Beekman, A.T.F.; Penninx, B.W.J.H. Depressive and anxiety disorders in concert–A synthesis of findings on comorbidity in the NESDA study. J. Affect. Disord. 2021, 284, 85–97. [Google Scholar] [CrossRef]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Koretz, D.; Merikangas, K.R.; Rush, A.J.; Walters, E.E.; Wang, P.S. The Epidemiology of Major Depressive Disorder Results from the National Comorbidity Survey Replication (NCS-R). JAMA 2003, 289, 3095–3105. [Google Scholar] [CrossRef] [PubMed]
- Craemer, K.A.; Garland, C.E.; Sayah, L.; Duffecy, J.; Geller, S.E.; Maki, P.M. Perinatal mental health in low-income urban and rural patients: The importance of screening for comorbidities. Gen. Hosp. Psychiatry 2023, 83, 130–139. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Practice Guideline for the Treatment of Patients with Major Depressive Disorder, 3rd ed.; American Psychiatric Association: Washington, DC, USA, 2010; pp. 69–71. [Google Scholar]
- Katzman, M.A.; Bleau, P.; Blier, P.; Chokka, P.; Kjernisted, K.; Van Ameringen, M.; the Canadian Anxiety Guidelines Initiative Group on behalf of the Anxiety Disorders Association of Canada/Association Canadienne des troubles anxieux and McGill University. Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC Psychiatry 2014, 14, S1. [Google Scholar] [CrossRef] [PubMed]
- Buist, A.; Gotman, N.; Yonkers, K.A. Generalized anxiety disorder: Course and risk factors in pregnancy. J. Affect. Disord. 2011, 131, 277–283. [Google Scholar] [CrossRef]
- Kee, M.Z.L.; Cremaschi, A.; De Iorio, M.; Chen, H.; Montreuil, T.; Nguyen, T.V.; Côté, S.M.; O’Donnell, K.J.; Giesbrecht, G.F.; Letourneau, N.; et al. Perinatal Trajectories of Maternal Depressive Symptoms in Prospective, Community-Based Cohorts Across 3 Continents. JAMA Netw. Open 2023, 6, e2339942. [Google Scholar] [CrossRef]

| Measure | Intake | 6 Weeks Postpartum | 4–6 Months Postpartum |
|---|---|---|---|
| Contact information and demographics—full version | ✓ | ||
| Questions on exercise | ✓ | ✓ | ✓ |
| Questions on complementary alternative medicine (CAM) | ✓ | ||
| Newborn and birth information | ✓ | ||
| Demographics—update | ✓ | ✓ | |
| The Edinburgh Postnatal Depression Scale (EPDS) | ✓ | ✓ | ✓ |
| The Generalized Anxiety Disorder (GAD)-7 | ✓ | ✓ | ✓ |
| The Antenatal Risk Questionnaire (ARNQ)—full version | ✓ | ||
| Postnatal Risk Questionnaire (PRNQ) | Last 3 questions ✓ | Full version ✓ | |
| The Cambridge Worry Scale (CWS) | ✓ | ||
| The Relationship Questionnaire (RQ) | ✓ | ||
| The Adverse Childhood Experiences Questionnaire (ACE) | ✓ | ||
| The Postpartum Bonding Questionnaire (PBQ) | ✓ | ✓ | |
| Pregnancy Risk Assessment Monitoring System Questionnaire (PRAMS)—14 questions | ✓ | ✓ | |
| The Barkin Index of Maternal Functioning (BIMF) | ✓ | ✓ | |
| Clinician history-taking form | ✓ | ||
| Quality assurance questionnaire (added in June 2021) | ✓ | ✓ | |
| COVID-19 module (between October 2020 and February 2024) | ✓ |
| Measure | Intake | 4–6 Months Postpartum |
|---|---|---|
| Contact information and demographics—full version | ✓ | |
| Questions on exercise | ✓ | ✓ |
| Questions on complementary alternative medicine (CAM) | ✓ | |
| Newborn and birth information | ✓ | |
| Demographics—update | ✓ | |
| The Edinburgh Postnatal Depression Scale (EPDS) | ✓ | ✓ |
| The Generalized Anxiety Disorder (GAD)-7 | ✓ | ✓ |
| Postnatal Risk Questionnaire (PRNQ)—full | ✓ | ✓ |
| The Relationship Questionnaire (RQ) | ✓ | |
| The Adverse Childhood Experiences Questionnaire (ACE) | ✓ | |
| The Postpartum Bonding Questionnaire (PBQ) | ✓ | ✓ |
| Pregnancy Risk Assessment Monitoring System Questionnaire (PRAMS)—14 questions | ✓ | ✓ |
| The Barkin Index of Maternal Functioning (BIMF) | ✓ | ✓ |
| Clinician history-taking form | ✓ | |
| Quality assurance questionnaire (added in June 2021) | ✓ | |
| COVID-19 module (between October 2020 and February 2024) | ✓ |
| Variable | Variable Choice | n (%) |
|---|---|---|
| Pregnancy status at intake (N = 693) | Pregnant | 522 (75.3) |
| Postpartum | 171 (24.7) | |
| Age (n = 609), years | Mean (SD) | 32.7 (4.8) |
| Minimum | 19 | |
| Maximum | 48 | |
| Parity (n = 502) | Current one is their first pregnancy/baby | 179 (35.7) |
| One or more prior deliveries | 323 (64.3) | |
| Marital status (n = 682) | Married or living with partner | 599 (87.8) |
| Single, not living with partner, separated, divorced, or widowed | 83 (12.2) | |
| Immigration status | Canadian citizen † | 578 (84.9) |
| (n = 681) | Permanent resident | 66 (9.7) |
| Temporary resident | 27 (4.0) | |
| Refugee | 10 (1.5) | |
| Ethnicity * (N = 693) | Caucasian | 472 (68.1) |
| Black | 56 (8.1) | |
| Middle Eastern | 40 (5.8) | |
| Asian | 46 (6.6) | |
| Hispanic | 34 (4.9) | |
| Indigenous | 7 (1.0) | |
| Other | 58 (8.4) | |
| Education (n = 681) | High school or lower | 111 (16.3) |
| CÉGEP ** | 144 (21.1) | |
| Bachelor’s | 254 (37.3) | |
| Master’s | 138 (20.3) | |
| Doctorate | 34 (5.0) | |
| Annual household | Under CAD 39,999 | 115 (17.1) |
| income (n = 674) | CAD 40,000–59,999 | 80 (11.9) |
| CAD 60,000–79,000 | 63 (9.3) | |
| CAD 80,000–99,999 | 102 (15.1) | |
| CAD 100,000–120,000 | 106 (15.7) | |
| Over CAD 120,000 | 208 (30.9) | |
| Work status | Currently working | 295 (43.3) |
| (n = 681) *** | - Employed full-time | 250 (85.6) |
| - Employed part-time | 42 (14.4) | |
| Not currently working * | 386 (56.7) | |
| - Full-time homemaker | 35 (5.1) | |
| - Student | 27 (3.9) | |
| - Maternal leave | 184 (26.6) | |
| - Medical leave | 108 (15.6) | |
| - Unemployed | 48 (6.9) |
| Psychiatric Diagnosis | N (%) |
|---|---|
| Anxiety disorders | 370 (53.4) |
| - Generalized anxiety disorder | 262 (37.8) |
| - Panic | 60 (8.7) |
| - Social anxiety | 53 (7.6) |
| - Specific phobia | 37 (5.3) |
| - Other anxiety disorders | 102 (14.7) |
| Depressive disorders | 247 (35.6) |
| - Major depressive disorder | 210 (30.3) |
| - Other depressive disorders | 62 (8.9) |
| Adjustment disorder | 97 (14.0) |
| Trauma and stressor-related disorders | 83 (12.0) |
| - Posttraumatic stress disorder | 48 (6.9) |
| - Other trauma and stressor-related disorders | 35 (5.1) |
| Personality disorders | 81 (11.7) |
| - Borderline | 52 (7.5) |
| - Obsessive–compulsive | 30 (4.3) |
| - Other personality disorders | 12 (1.7) |
| Obsessive compulsive and related disorders | 72 (10.4) |
| Attention deficit/hyperactivity disorder | 71 (10.2) |
| Bipolar and related disorders | 48 (6.9) |
| - Bipolar type I | 24 (3.5) |
| - Bipolar type II | 16 (2.3) |
| - Other bipolar and related disorders | 8 (1.2) |
| Substance use disorder | 36 (5.2) |
| Eating disorders | 27 (3.9) |
| - Anorexia nervosa | 13 (1.9) |
| - Other eating disorders | 13 (1.9) |
| Schizophrenia spectrum and other psychotic disorders | 17 (2.5) |
| - Schizophrenia | 7 (1.0) |
| - Schizoaffective | 6 (0.9) |
| - Other schizophrenia spectrum and other psychotic disorders | 5 (0.7) |
| Somatic disorders | 8 (1.2) |
| Treatment Type | N (%) |
|---|---|
| Psychotherapy | 490 (70.7) |
| Moderate physical activity | 86 (12.4) |
| Medical leave | 62 (8.9) |
| Antidepressant | 267 (38.5) |
| Antipsychotic | 77 (11.1) |
| Benzodiazepine | 42 (6.1) |
| Mood stabilizer | 6 (0.9) |
| Non-benzodiazepine hypnotics | 7 (1.0) |
| Stimulants | 4 (0.6) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aumais, M.; Ateba, F.F.; Wolde-Giorghis, R.; Keeren, K.; Hayton, B.; Kalache, S.; Collin, I.; Schwartz, H.; Gust, K.; Poulin, M.-J.; et al. The Perinatal Multisite Psychiatry Databank: A Cohort Update. Int. J. Environ. Res. Public Health 2025, 22, 684. https://doi.org/10.3390/ijerph22050684
Aumais M, Ateba FF, Wolde-Giorghis R, Keeren K, Hayton B, Kalache S, Collin I, Schwartz H, Gust K, Poulin M-J, et al. The Perinatal Multisite Psychiatry Databank: A Cohort Update. International Journal of Environmental Research and Public Health. 2025; 22(5):684. https://doi.org/10.3390/ijerph22050684
Chicago/Turabian StyleAumais, Mariane, Francois Freddy Ateba, Rahel Wolde-Giorghis, Kathelijne Keeren, Barbara Hayton, Sawsan Kalache, Isabelle Collin, Hannah Schwartz, Kirsten Gust, Marie-Josée Poulin, and et al. 2025. "The Perinatal Multisite Psychiatry Databank: A Cohort Update" International Journal of Environmental Research and Public Health 22, no. 5: 684. https://doi.org/10.3390/ijerph22050684
APA StyleAumais, M., Ateba, F. F., Wolde-Giorghis, R., Keeren, K., Hayton, B., Kalache, S., Collin, I., Schwartz, H., Gust, K., Poulin, M.-J., Wassef, A., Tardif, K., St-André, M., Stikarovska, I., Zelkowitz, P., Herba, C. M., & Szekely, E. (2025). The Perinatal Multisite Psychiatry Databank: A Cohort Update. International Journal of Environmental Research and Public Health, 22(5), 684. https://doi.org/10.3390/ijerph22050684






