Parent-Reported Health-Related Quality of Life (HRQoL) of NICU Graduates in Their First Year: A Prospective Cohort Study
Abstract
:1. Background
2. Methods
2.1. Setting and Population
2.2. The Infant Quality of Life Instrument (IQI)
2.3. Data and Statistical Analysis
3. Results
3.1. Background Characteristics
3.2. Parent-Reported Problems During the First Year After Birth
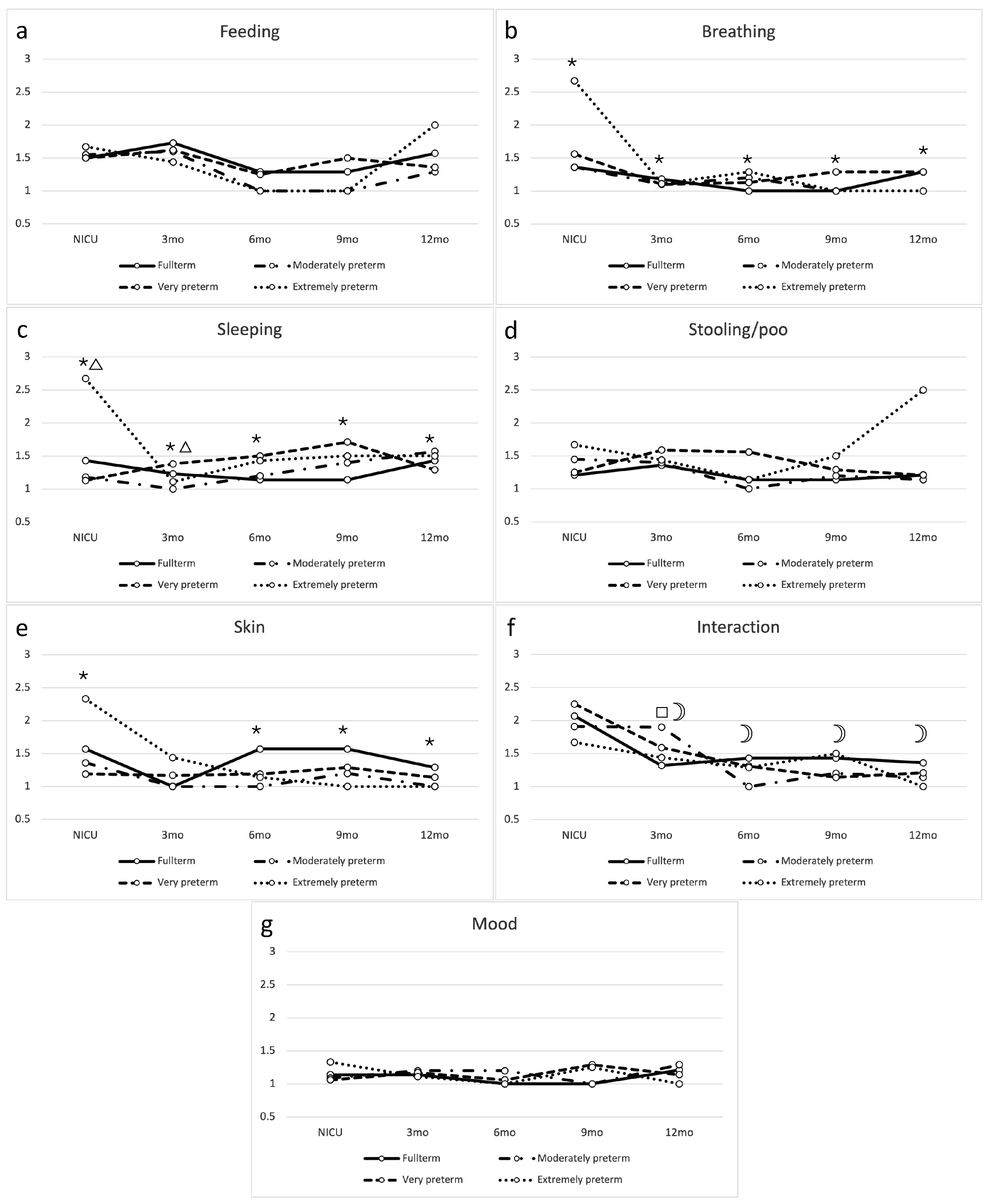
3.3. Trajectories Across Gestational Age Groups
4. Discussion
4.1. Strengths and Limitations
4.2. Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Busse, M.; Stromgren, K.; Thorngate, L.; Thomas, K.A. Parents’ responses to stress in the neonatal intensive care. Crit. Care Nurs. 2013, 33, 52–59. [Google Scholar] [CrossRef]
- Mooney-Leber, S.M.; Brummelte, S. Neonatal pain and reduced maternal care: Early-life stressors interacting to impact brain and behavioral development. Neuroscience 2017, 342, 21–36. [Google Scholar] [CrossRef] [PubMed]
- Stoll, B.J.; Hansen, N.I.; Bell, E.F.; Walsh, M.C.; Carlo, W.A.; Shankaran, S.; Laptook, A.R.; Sánchez, P.J.; Van Meurs, K.P.; Wyckoff, M.; et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. J. Am. Med. Assoc. 2015, 314, 1039–1051. [Google Scholar] [CrossRef] [PubMed]
- Platt, M.J. Outcomes in preterm infants. Public Health 2014, 128, 399–403. [Google Scholar] [CrossRef] [PubMed]
- Glass, H.C.; Costarino, A.T.; Stayer, S.A.; Brett, C.; Cladis, F.; Davis, P.J. Outcomes for extremely premature infants. Anesth. Analg. 2015, 120, 1337–1351. [Google Scholar] [CrossRef]
- de Kieviet, J.F.; Piek, J.P.; Aarnoudse-Moens, C.S.; Oosterlaan, J. Motor development in very preterm and very low-birth-weight children from birth to adolescence: A meta-analysis. J. Am. Med. Assoc. 2009, 302, 2235–2242. [Google Scholar] [CrossRef]
- Ahearne, C.E.; Boylan, G.B.; Murray, D.M. Short and long term prognosis in perinatal asphyxia: An update. Clin. Pediatr. 1962, 5, 67–74. [Google Scholar] [CrossRef]
- Medoff-Cooper, B.; Ravishankar, C. Nutrition and growth in congenital heart disease: A challenge in children. Curr. Opin. Cardiol. 2013, 28, 122–129. [Google Scholar] [CrossRef]
- Fourdain, S.; St-Denis, A.; Harvey, J.; Birca, A.; Carmant, L.; Gallagher, A.; Trudeau, N. Language development in children with congenital heart disease aged 12-24 months. Eur. J. Paediatr. Neurol. 2019, 23, 491–499. [Google Scholar] [CrossRef]
- Calderon, J.; Willaime, M.; Lelong, N.; Bonnet, D.; Houyel, L.; Ballon, M.; Goffinet, F.; Khoshnood, B. Population-based study of cognitive outcomes in congenital heart defects. Arch. Dis. Child. 2018, 103, 49–56. [Google Scholar] [CrossRef]
- Saigal, S.; Ferro, M.A.; Van Lieshout, R.J.; Schmidt, L.A.; Morrison, K.M.; Boyle, M.H. Health-related quality of life trajectories of extremely low birth weight survivors into adulthood. J. Pediatr. 2016, 179, 68–73.e1. [Google Scholar] [CrossRef] [PubMed]
- Gire, C.; Resseguier, N.; Brévaut-Malaty, V.; Marret, S.; Cambonie, G.; Souksi-Medioni, I.; Müller, J.-B.; Garcia, P.; Berbis, J.; Tosello, B.; et al. Quality of life of extremely preterm school-age children without major handicap: A cross-sectional observational study. Arch. Dis. Child. 2019, 104, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Roberts, G.; Burnett, A.C.; Lee, K.J.; Cheong, J.; Wood, S.J.; Anderson, P.J.; Doyle, L.W. Quality of life at age 18 years after extremely preterm birth in the post-surfactant era. J. Pediatr. 2013, 163, 1008–1013.e1. [Google Scholar] [CrossRef] [PubMed]
- Bilgin, A.; Wolke, D. Regulatory problems in very preterm and full-term infants over the first 18 months. J. Dev. Behav. Pediatr. 2016, 37, 298–305. [Google Scholar] [CrossRef]
- Mussatto, K.; Tweddell, J. Quality of life following surgery for congenital cardiac malformations in neonates and infants. Cardiol. Young 2005, 15, 174–178. [Google Scholar] [CrossRef]
- Jabrayilov, R.; van Asselt, A.D.I.; Vermeulen, K.M.; Volger, S.; Detzel, P.; Dainelli, L.; Krabbe, P.F.M. A descriptive system for the infant health-related quality of life instrument (IQI): Measuring health with a mobile app. PLoS ONE 2018, 13, e0203276. [Google Scholar] [CrossRef] [PubMed]
- Krabbe, P.F.M.; Jabrayilov, R.; Detzel, P.; Dainelli, L.; Vermeulen, K.M.; van Asselt, A.D.I. A two-step procedure to generate utilities for the infant health-related quality of life instrument (IQI). PLoS ONE 2020, 15, e0230852. [Google Scholar] [CrossRef]
- Hoogewerf, M.; Ter Horst, H.J.; Groen, H.; Nieuwenhuis, T.; Bos, A.F.; van Dijk, M.W.G. The prevalence of feeding problems in children formerly treated in a neonatal intensive care unit. J. Perinatol. 2017, 37, 578–584. [Google Scholar] [CrossRef]
- Gogou, M.; Haidopoulou, K.; Pavlou, E. Sleep and prematurity: Sleep outcomes in preterm children and influencing factors. World J. Pediatr. 2019, 15, 209–218. [Google Scholar] [CrossRef]
- Romeo, D.M.; Leo, G.; Lapenta, L.; Leone, D.; Turrini, I.; Brogna, C.; Gallini, F.; Cota, F.; Vento, G.; Mercuri, E. Sleep disorders in low-risk preschool very preterm children. Sleep Med. 2019, 63, 137–141. [Google Scholar] [CrossRef]
- Caravale, B.; Sette, S.; Cannoni, E.; Marano, A.; Riolo, E.; Devescovi, A.; De Curtis, M.; Bruni, O. Sleep characteristics and temperament in preterm children at two years of age. J. Clin. Sleep Med. 2017, 13, 1081–1088. [Google Scholar] [CrossRef] [PubMed]
- van Dokkum, N.H.; de Kroon, M.L.A.; Dijk, P.H.; Kraft, K.E.; Reijneveld, S.A.; Bos, A.F. Course of stress during the neonatal intensive care unit stay in preterm infants. Neonatology 2022, 119, 84–92. [Google Scholar] [CrossRef]
- Durankus, F.; Aladag Ciftdemir, N.; Vatansever Ozbek, U.; Duran, R.; Acunas, B. Comparison of sleep problems between term and preterm born preschool children. Sleep Med. 2020, 75, 484–490. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, N.; Piskernik, B.; Witting, A.; Fuiko, R.; Ahnert, L. Parent-child attachment in children born preterm and at term: A multigroup analysis. PLoS ONE 2018, 13, e0202972. [Google Scholar] [CrossRef]
- Pace, C.C.; Spittle, A.J.; Molesworth, C.M.-L.; Lee, K.J.; Northam, E.A.; Cheong, J.L.Y.; Davis, P.G.; Doyle, L.W.; Treyvaud, K.; Anderson, P.J. Evolution of depression and anxiety symptoms in parents of very preterm infants during the newborn period. J. Am. Med. Assoc. Pediatr. 2016, 170, 863–870. [Google Scholar] [CrossRef]
- Schecter, R.; Pham, T.; Hua, A.; Spinazzola, R.; Sonnenklar, J.; Li, D.; Papaioannou, H.; Milanaik, R. Prevalence and longevity of PTSD symptoms among parents of NICU infants analyzed across gestational age categories. Clin. Pediatr. 2020, 59, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Ronkainen, E.; Kaukola, T.; Marttila, R.; Hallman, M.; Dunder, T. School-age children enjoyed good respiratory health and fewer allergies despite having lung disease after preterm birth. Acta Paediatr. 2016, 105, 1298–1304. [Google Scholar] [CrossRef]
- Vieira, M.E.B.; Linhares, M.B.M. Quality of life of individuals born preterm: A systematic review of assessment approaches. Qual. Life Res. 2016, 25, 2123–2139. [Google Scholar] [CrossRef]
- Adams, S.Y.; Tucker, R.; Clark, M.A.; Lechner, B.E. “Quality of life”: Parent and neonatologist perspectives. J. Perinatol. 2020, 40, 1809–1820. [Google Scholar] [CrossRef]
- Jokovic, A.; Locker, D.; Guyatt, G. How well do parents know their children? implications for proxy reporting of child health-related quality of life. Qual. Life Res. 2004, 13, 1297–1307. [Google Scholar] [CrossRef]

| Full-Term (n = 31) | Moderately Late Preterm (n = 19) | Very Preterm (n = 45) | Extremely Preterm (n = 13) | |
|---|---|---|---|---|
| Gestational age (weeks) | 38 + 4 (SD 1.26) | 34 + 0 (SD 1.52) | 30 + 0 (SD 1.07) | 26 + 2 (SD 0.93) |
| Birth weight (grams) | 3489 (SD 629.45) | 2295 (SD 543.27) | 1468 (SD 288.22) | 960 (SD 155.41) |
| Sex | ||||
| Male | 17 (55%) | 10 (53%) | 26 (58%) | 9 (69%) |
| Female | 14 (45%) | 9 (47%) | 19 (42%) | 4 (31%) |
| Multiple birth | ||||
| Yes | 0 (0%) | 2 (11%) | 14 (31% | 1 (8%) |
| No | 31 (100%) | 17 (89%) | 31 (69%) | 12 (92%) |
| Firstborn child | ||||
| Yes | 12 (39%) | 7 (37%) | 32 (71%) | 9 (69%) |
| No | 17 (55%) | 9 (47%) | 12 (27%) | 4 (31%) |
| Surgery | ||||
| None | 23 (74%) | 13 (68%) | 45 (100%) | 11 (85%) |
| GI tract | 3 (10%) | 5 (26%) | 0 (0%) | 2 (15%) |
| Cardiac | 3 (10%) | 1 (5%) | 0 (0%) | 0 (0%) |
| Airway | 1 (3%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Urology | 1 (3%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Ventilation support | ||||
| None | 4 (13%) | 2 (11%) | 1 (2%) | 0 (0%) |
| High flow/low flow | 1 (3%) | 0 (0%) | 2 (4%) | 1 (8%) |
| CPAP | 3 (10%) | 6 (32%) | 28 (62%) | 3 (23%) |
| NIVM | 0 (0%) | 0 (0%) | 0 (0%) | 2 (15%) |
| Conventional | 21 (68%) | 11 (58%) | 14 (31%) | 5 (38%) |
| HFO | 2 (6%) | 0 (0%) | 0 (0%) | 2 (15%) |
| Total completed questionnaires | 67 | 38 | 89 | 25 |
| Number of completed HRQoL app questionnaire | ||||
| 1× | 12 (39%) | 7 (37%) | 19 (42%) | 6 (46%) |
| 2× | 10 (32%) | 6 (31%) | 14 (31%) | 3 (23%) |
| 3× | 3 (10%) | 5 (26%) | 6 (13%) | 3 (23%) |
| 4× | 4 (13%) | 1 (5%) | 6 (13%) | 1 (8%) |
| 5× | 2 (6%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Timing of completed HRQoL app questionnaires | ||||
| During NICU | 14 (21%) | 11 (29%) | 16 (18%) | 3 (12%) |
| 3 mo | 22 (33%) | 10 (26%) | 29 (33%) | 9 (36%) |
| 6 mo | 7 (10%) | 5 (13%) | 16 (18%) | 7 (28%) |
| 9 mo | 10 (15%) | 5 (13%) | 14 (16%) | 4 (16%) |
| 12 mo | 14 (21%) | 7 (18%) | 14 (16%) | 2 (8%) |
| NICU (n = 44) | 3 mo (n = 70) | 6 mo (n = 35) | 9 mo (n = 33) | 12 mo (n = 37) | p Value | |
| Feeding | 19 (43%) | 27 (39%) | 5 (14%) | 6 (18%) | 12 (32%) | 0.046 |
| Breathing | 18 (41%) | 7 (10%) | 5 (14%) | 4 (12%) | 7 (19%) | 0.052 |
| Sleeping | 12 (27%) | 16 (23%) | 12 (34%) | 14 (42%) | 11 (30%) | 0.233 |
| Stooling/poo | 11 (25%) | 27 (39%) | 9 (26%) | 8 (24%) | 8 (22%) | 0.264 |
| Skin | 18 (41%) | 7 (10%) | 7 (20%) | 6 (18%) | 6 (16%) | 0.071 |
| Interaction | 38 (86%) | 37 (53%) | 10 (29%) | 8 (24%) | 7 (19%) | <0.001 |
| Mood | 4 (9%) | 9 (13%) | 2 (6%) | 5 (15%) | 6 (16%) | 0.359 |
| Sex (Male vs. Female) | Multiple Birth (No vs. Yes) | First Born (No vs. Yes) | Surgery (No vs. Yes) | Ventilation Support (No vs. Yes) | |
| Feeding | 41 (32%) vs. 28 (31%) | 60 (31%) vs. 9 (33%) | 26 (33%) vs. 42 (33%) | 58 (31%) vs. 11 (31%) | 3 (18%) vs. 66 (33%) |
| Breathing | 30 (23%) vs. 11 (12%) * | 39 (20%) vs. 2 (7%) | 11 (14%) vs. 27 (21%) | 34 (18%) vs. 7 (20%) | 3 (18%) vs. 38 (19%) |
| Sleeping | 37 (29%) vs. 28 (31%) | 55 (29%) vs. 10 (37%) | 26 (33%) vs. 36 (29%) | 56 (30%) vs. 9 (26%) | 3 (8%) vs. 62 (31%) |
| Stooling/poo | 32 (25%) vs. 31 (34%) | 53 (28%) vs. 10 (37%) | 23 (29%) vs. 39 (31%) | 54 (29%) vs. 9 (26%) | 6 (35%) vs. 57 (28%) |
| Skin | 30 (23%) vs. 14 (15%) | 42 (22%) vs. 2 (7%) | 12 (15%) vs. 29 (23%) | 36 (20%) vs. 8 (23%) | 3 (18%) vs. 41 (20%) |
| Interaction | 56 (44%) vs. 44 (48%) | 89 (46%) vs. 11 (41%) | 27 (34%) vs. 3 (50%) * | 86 (47%) vs. 14 (40%) | 7 (41%) vs. 93 (46%) |
| Mood | 14 (11%) vs. 12 (13%) | 23 (12%) vs. 3 (11%) | 9 (11%) vs. 16 (13%) | 20 (11%) vs. 6 (17%) | 1 (6%) vs. 25 (12%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heuvink, P.; van Dokkum, N.H.; Van Braeckel, K.N.J.A.; Bouma, H.A.; Kraft, K.E.; Bos, A.F.; Krabbe, P.F.M. Parent-Reported Health-Related Quality of Life (HRQoL) of NICU Graduates in Their First Year: A Prospective Cohort Study. Int. J. Environ. Res. Public Health 2025, 22, 447. https://doi.org/10.3390/ijerph22030447
Heuvink P, van Dokkum NH, Van Braeckel KNJA, Bouma HA, Kraft KE, Bos AF, Krabbe PFM. Parent-Reported Health-Related Quality of Life (HRQoL) of NICU Graduates in Their First Year: A Prospective Cohort Study. International Journal of Environmental Research and Public Health. 2025; 22(3):447. https://doi.org/10.3390/ijerph22030447
Chicago/Turabian StyleHeuvink, Parel, Nienke H. van Dokkum, Koenraad N. J. A. Van Braeckel, Helene A. Bouma, Karianne E. Kraft, Arend F. Bos, and Paul F. M. Krabbe. 2025. "Parent-Reported Health-Related Quality of Life (HRQoL) of NICU Graduates in Their First Year: A Prospective Cohort Study" International Journal of Environmental Research and Public Health 22, no. 3: 447. https://doi.org/10.3390/ijerph22030447
APA StyleHeuvink, P., van Dokkum, N. H., Van Braeckel, K. N. J. A., Bouma, H. A., Kraft, K. E., Bos, A. F., & Krabbe, P. F. M. (2025). Parent-Reported Health-Related Quality of Life (HRQoL) of NICU Graduates in Their First Year: A Prospective Cohort Study. International Journal of Environmental Research and Public Health, 22(3), 447. https://doi.org/10.3390/ijerph22030447







