Economic and Humanistic Burden of Multimorbidity in the United States: A Longitudinal Study of Expenditure and Quality of Life Trajectories, 2019–2022
Highlights
- Multimorbidity is an increasing public health challenge associated with rising health care utilization and declining quality of life.
- This longitudinal study leverages nationally representative data (2019–2022) to determine how specific combinations of discordant diseases (e.g., cancer co-occurring with respiratory disease) drive divergent trajectories in healthcare expenditures and quality of life.
- This study provides longitudinal evidence of persistent disparities in healthcare expenditures and quality of life among multimorbid individuals.
- Findings identify population groups experiencing disproportionately high costs and poorer health-related quality of life.
- Health systems and payers should adopt cluster-based risk segmentation to target high-volatility profiles (such as the cancer + respiratory cluster) for proactive case management and admission prevention.
- Findings support the need for integrated, patient-centered approaches to managing chronic disease in adults.
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
2.2. Study Population and MM Clusters
2.2.1. Disease Ascertainment
2.2.2. Disease Domains
- Cardiometabolic disease was defined using four MEPS diagnosis indicators: Diabetes mellitus, coronary heart disease, hypertension, and hyperlipidemia. A respondent was classified as having cardiometabolic disease if at least one indicator was equal to 1.
- Respiratory diseases included asthma and emphysema.
- Cancer was defined using both the general cancer diagnosis variable and site-specific cancer indicators, including bladder, breast, lung, prostate, colorectal, and lymphatic malignancies.
2.2.3. Disease Timeframe and Treatment Status
MM Cluster Construction
- No target conditions;
- Respiratory only;
- Cardiometabolic only;
- Cancer only;
- Cardio–respiratory;
- Cancer–respiratory combination;
- Cancer–cardiometabolic and three-domain multimorbidity (cancer + cardiometabolic + respiratory).
2.2.4. Disease Burden vs. Disease Count
2.3. Outcome Variables
- Economic burden: Measured by (I) Total Annual Healthcare Expenditures (sum of all the payments from all sources) and (II) Total Annual OOP spending (direct payments made by patients/families). All costs were inflation-adjusted to 2022 U.S. dollars using the Medical Care component of the Consumer Price Index (CPI);
- Humanistic burden: Assessed using the Veterans RAND-12 (VR-12) health survey, a validated instrument yielding two summary scores: (I) the Physical Component Summary (PCS) and (II) the Mental Component Summary (MCS). These scores are standardized to a mean of 50, with lower scores indicating poorer quality of life;
- Healthcare utilization: Measured by the annual number of inpatient-hospital stays per person.
2.4. Covariates
2.5. Statistical Analysis
Sensitivity Analysis
2.6. Missing Data Handling
3. Results
3.1. Baseline Characteristics of the Study Population
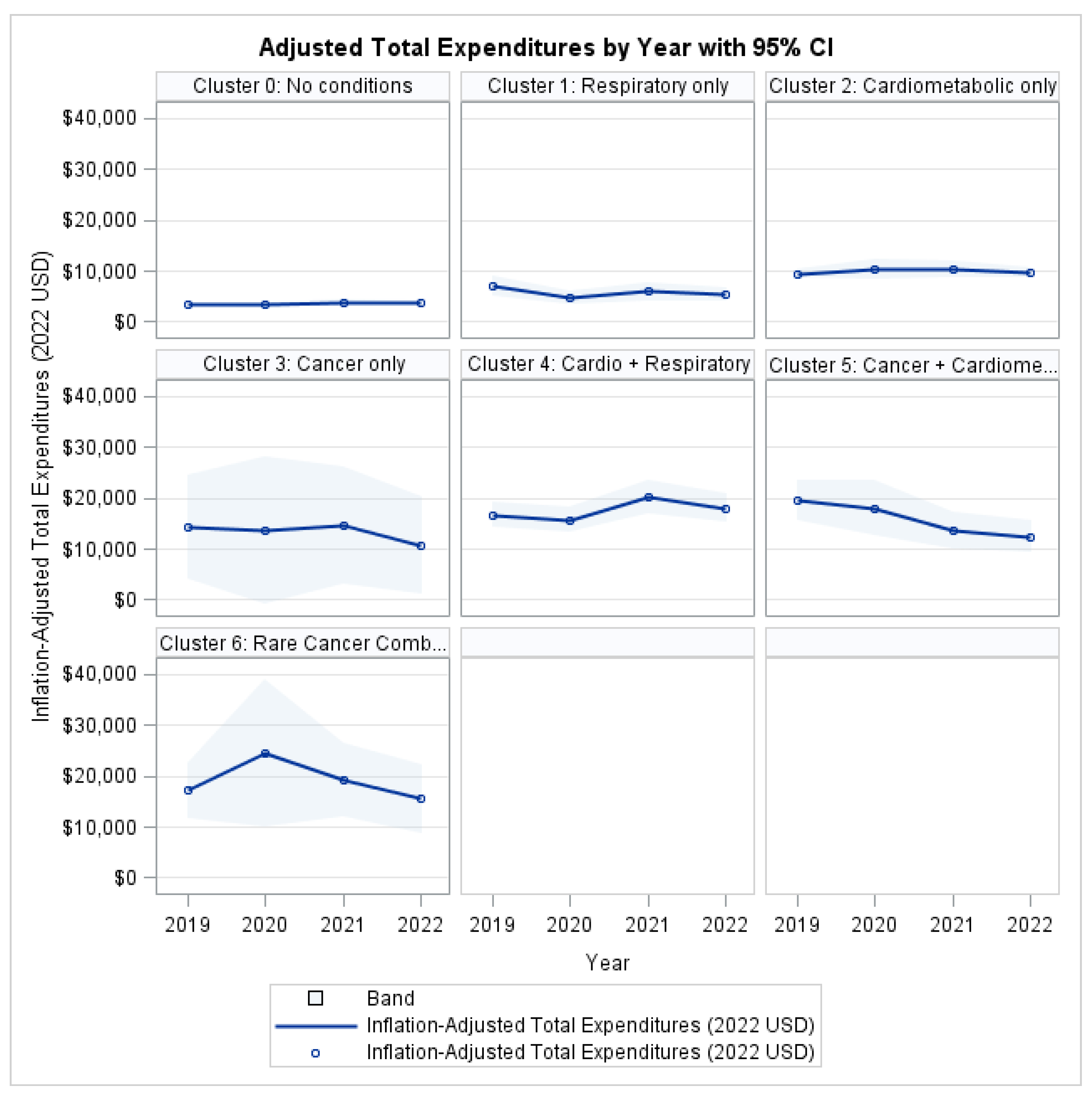
3.2. System-Level Economic Burden: Total Healthcare Expenditures
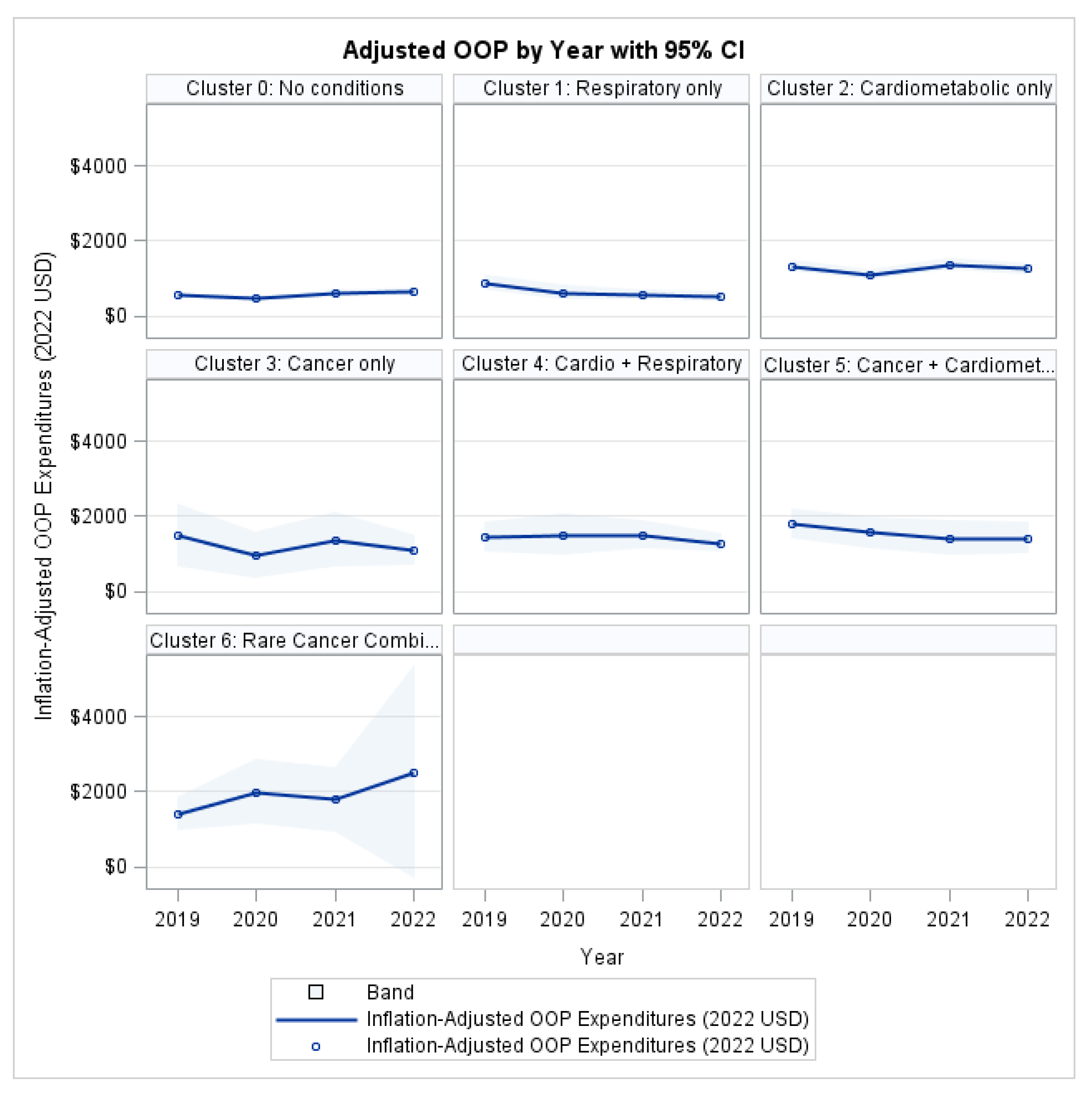
3.3. Patient Financial Burden: OOP Expenditures
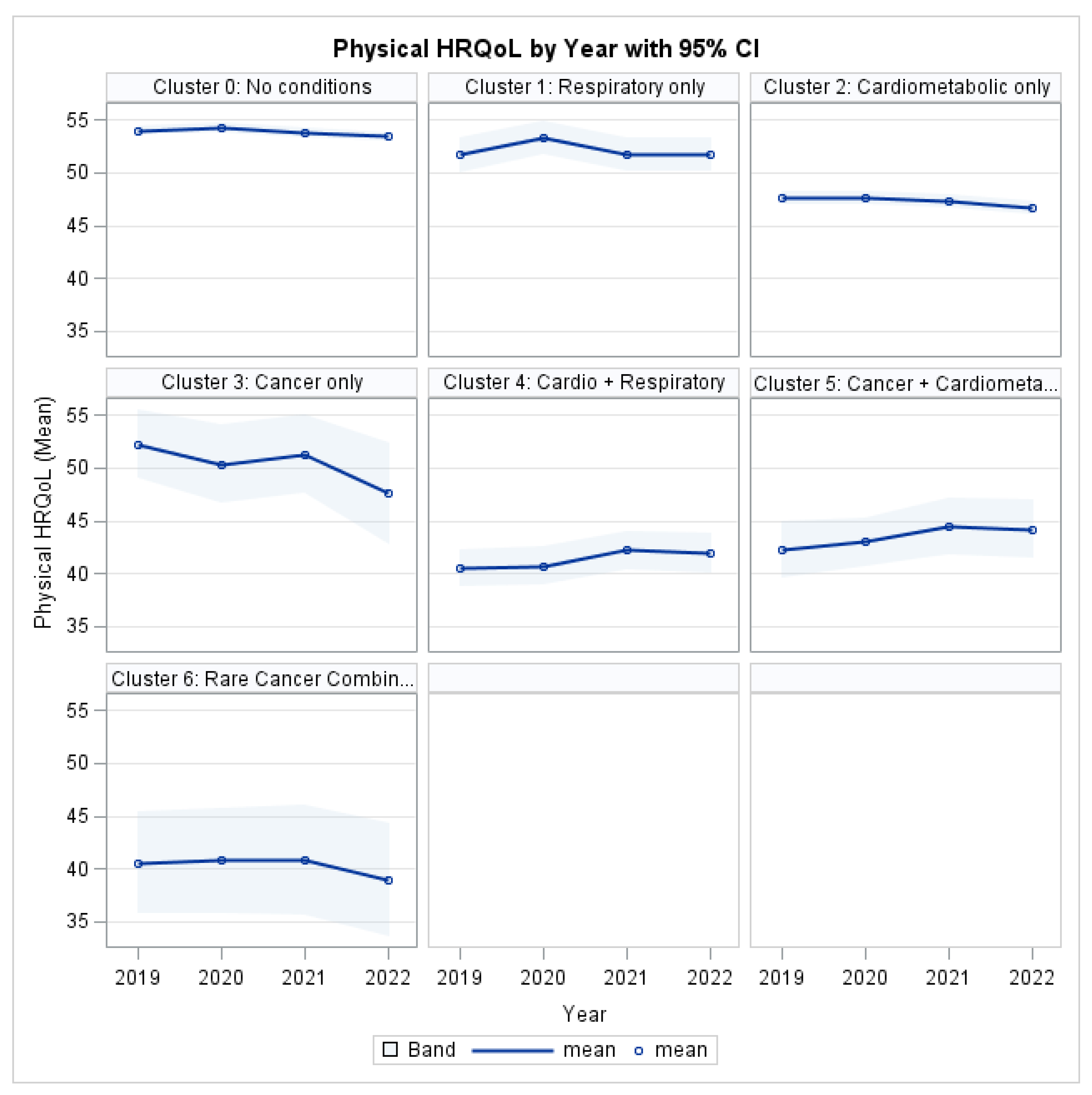
3.4. Humanistic Burden: Physical HRQL
3.5. Humanistic Burden: Mental HRQL
3.6. Healthcare Utilization: Inpatient Stays
3.7. Multivariable Model Estimates
3.8. Sensitivity Analyses: Role of Disease Counts Within Axes
3.8.1. Total Healthcare Expenditures (Table 2)
3.8.2. Out-of-Pocket Expenditures (Table 3)
3.8.3. Physical HRQL (PCS) (Table 4)
3.8.4. Mental HRQL (MCS) (Table 5)
3.8.5. Inpatient Hospital Stays (Table 6)
4. Discussion
4.1. Economic Burden and Disease Configuration
4.2. Patient-Level Financial Burden
4.3. Quality of Life and Functional Burden
4.4. Hospitalization Risk and Disease Intensity
4.5. Implications for Policy, Prevention, and Care Delivery
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CDC | Centers for Disease Control and Prevention |
| HRQL | Health Related Quality of Life |
| MCC | Multiple chronic conditions |
| MEPS | Medical Expenditure Panel Survey |
| MM | Multimorbidity |
| OOP | Out of Pocket |
| GEE | Generalized Estimating Equation |
References
- Aborode, A.T.M.; Oginni, O.; Abacheng, M.M.; Edima, O.; Lamunu, E.; Folorunso, T.N.M.; Oko, C.I.M.; Iretiayo, A.R.M.; Lawal, L.M.; Amarachi, R.B.; et al. Healthcare debts in the United States: A silent fight. Ann. Med. Surg. 2025, 87, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Watson, K.B.; Wiltz, J.L.; Nhim, K.; Kaufmann, R.B.; Thomas, C.W.; Greenlund, K.J. Trends in Multiple Chronic Conditions Among US Adults, By Life Stage, Behavioral Risk Factor Surveillance System, 2013–2023. Prev. Chronic Dis. 2025, 22, E15. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zhou, W.; Cui, Y.; Cao, K.; Chen, M.; Qu, R.; Miao, J.; Qi, J.; Wu, X.; Chen, J.; et al. Global, regional, and national characteristics of the main causes of increased disease burden due to the covid-19 pandemic: Time-series modelling analysis of global burden of disease study 2021. BMJ 2025, 390, e083868. [Google Scholar] [CrossRef]
- Félix, I.B.; Henriques, A. Medication adherence and related determinants in older people with multimorbidity: A cross-sectional study. Nurs. Forum 2021, 56, 834–843. [Google Scholar] [CrossRef] [PubMed]
- Nobili, A.; Marengoni, A.; Tettamanti, M.; Salerno, F.; Pasina, L.; Franchi, C.; Iorio, A.; Marcucci, M.; Corrao, S.; Licata, G.; et al. Association between clusters of diseases and polypharmacy in hospitalized elderly patients: Results from the REPOSI study. Eur. J. Intern. Med. 2011, 22, 597–602. [Google Scholar] [CrossRef]
- Richard, P.; Walker, R.; Alexandre, P. The burden of out of pocket costs and medical debt faced by households with chronic health conditions in the United States. PLoS ONE 2018, 13, e0199598. [Google Scholar] [CrossRef] [PubMed]
- Khera, R.; Valero-Elizondo, J.; Okunrintemi, V.; Saxena, A.; Das, S.R.; de Lemos, J.A.; Krumholz, H.M.; Nasir, K. Association of Out-of-Pocket Annual Health Expenditures with Financial Hardship in Low-Income Adults with Atherosclerotic Cardiovascular Disease in the United States. JAMA Cardiol. 2018, 3, 729–738. [Google Scholar] [CrossRef] [PubMed]
- García-Pardo, M.; Chang, A.; Schmid, S.; Dong, M.; Brown, M.C.; Christiani, D.; Tindel, H.A.; Brennan, P.; Chen, C.; Zhang, J.; et al. Respiratory and Cardiometabolic Comorbidities and Stages I to III NSCLC Survival: A Pooled Analysis from the International Lung Cancer Consortium. J. Thorac. Oncol. 2023, 18, 313–323. [Google Scholar] [CrossRef] [PubMed]
- Freisling, H.; Viallon, V.; Lennon, H.; Bagnardi, V.; Ricci, C.; Butterworth, A.S.; Sweeting, M.; Muller, D.; Romieu, I.; Bazelle, P.; et al. Lifestyle factors and risk of multimorbidity of cancer and cardiometabolic diseases: A multinational cohort study. BMC Med. 2020, 18, 5. [Google Scholar] [CrossRef] [PubMed]
- Soley-Bori, M.; Ashworth, M.; Bisquera, A.; Dodhia, H.; Lynch, R.; Wang, Y.; Fox-Rushby, J. Impact of multimorbidity on healthcare costs and utilisation: A systematic review of the UK literature. Br. J. Gen. Pract. 2021, 71, e39–e46. [Google Scholar] [CrossRef] [PubMed]
- Cox, C.; Ortaliza, J.; Wager, E.; Amin, K. Health Policy 101, Health Care Costs and Affordability. KFF: N.d. Available online: https://www.kff.org/health-costs/health-policy-101-health-care-costs-and-affordability/?entry=table-of-contents-introduction (accessed on 19 October 2025).
- Williams, J.S.; Egede, L.E. The Association Between Multimorbidity and Quality of Life, Health Status and Functional Disability. Am. J. Med Sci. 2016, 352, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Fortin, M.; Lapointe, L.; Hudon, C.; Vanasse, A.; Ntetu, A.L.; Maltais, D. Multimorbidity and quality of life in primary care: A systematic review. Health Qual. Life Outcomes 2004, 2, 51. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.W.; Al-Busaidi, I.S.; Caya, R.; Bricca, A.; Mangin, D.; Wilson, R.; Abbott, J.H. Effectiveness of interventions for the management of multimorbidity in primary care and community settings: Systematic review and meta-analysis. Fam. Pract. 2025, 42, cmaf085. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | Unweighted n (Weighted %) | Weighted N |
|---|---|---|
| Clusters | ||
| Cluster 0: No Conditions | 2862 (59.76) | 201,351,877 |
| Cluster 1: Respiratory Only | 384 (7.53) | 25,382,546 |
| Cluster 2: Cardiometabolic Only | 1723 (25.08) | 84,519,951 |
| Cluster 3: Cancer Only | 42 (0.58) | 1,954,930 |
| Cluster 4: Cardio + Respiratory | 368 (4.85) | 16,339,563 |
| Cluster 5: Cancer + Cardiometabolic | 141 (1.65) | 5,566,711 |
| Cluster 6: “Rare Cancer Combination” | 87 (1.12) | 3,779,979 |
| Total | 5565 (100.0) | 336,940,627 |
| Gender | ||
| Male | 2617 (49.37) | 166,358,534 |
| Female | 2948 (50.63) | 170,582,093 |
| Race/Ethnicity | ||
| Hispanic | 1381 (19.2) | 64,601,815 |
| Non-Hispanic White | 2857 (58.2) | 196,242,452 |
| Non-Hispanic Black | 884 (12.5) | 42,154,385 |
| Non-Hispanic Asian | 254 (6.2) | 20,970,510 |
| Non-Hispanic Other/Mixed | 185 (3.8) | 12,971,464 |
| Insurance Status | ||
| Insured | 4719 (89.9) | 292,270,727 |
| Uninsured | 613 (10.1) | 32,799,348 |
| Educational Level | ||
| No Degree | 756 (9.06) | 30,412,716 |
| Less than 16 (Underage) | 1046 (24) | 80,553,438 |
| GED | 181 (2.3) | 7,816,499 |
| High School Diploma | 1792 (29.7) | 99,794,996 |
| Bachelor’s Degree | 835 (16.3) | 54,856,816 |
| Master’s Degree | 412 (8.0) | 26,875,052 |
| Doctorate Degree | 112 (2.2) | 7,394,810 |
|
Other Degree Income Status | 405 (8.3) | 28,013,149 |
| Poor/Negative | 1134 (13.5) | 44,059,680 |
| Near Poor | 318 (4.005) | 13,223,863 |
| Low Income | 783 (11.7) | 38,200,651 |
| Middle Income | 1447 (28.12) | 91,783,368 |
| High Income | 1770 (42.62) | 139,109,119 |
| Predictor | Primary | Sensitivity | |||
|---|---|---|---|---|---|
| DF | χ2 | p-Value | χ2 | p-Value | |
| Year | 3 | 1.50 | 0.6817 | 2.12 | 0.5489 |
| Cluster | 6 | 62.54 | <0.001 | 21.11 | 0.0018 |
| Cluster-Year | 18 | 12.89 | 0.7980 | 12.31 | 0.8309 |
| Age | 1 | 55.73 | <0.001 | 43.80 | <0.001 |
| Race | 4 | 8.00 | 0.0914 | 8.61 | 0.0717 |
| Sex | 1 | 2.00 | 0.1577 | 2.41 | 0.1207 |
| Insurance Status | 1 | 0.32 | 0.5697 | 0.33 | 0.5662 |
| Educational Level | 7 | 6.17 | 0.5200 | 6.99 | 0.4297 |
| Poverty Cat | 4 | 7.10 | 0.1308 | 6.94 | 0.1392 |
| Cardiometabolic burden (count category) | 2 | — | — | 10.47 | 0.0053 |
| Respiratory burden (count category) | 1 | — | — | 4.87 | 0.0273 |
| Cancer burden (count category) | 0 | — | — | 0.00 | — |
| Predictor | Primary | Sensitivity | |||
|---|---|---|---|---|---|
| DF | χ2 | p-Value | χ2 | p-Value | |
| Year | 3 | 1.82 | 0.6110 | 10.37 | 0.0157 |
| Cluster | 6 | 9.74 | 0.1361 | 3.51 | 0.7424 |
| Cluster-Year | 18 | 23.57 | 0.1696 | 22.57 | 0.2075 |
| Age | 1 | 43.97 | <0.001 | 40.18 | <0.001 |
| Race | 4 | 29.11 | <0.001 | 28.82 | <0.001 |
| Sex | 1 | 5.94 | 0.0148 | 6.28 | 0.0122 |
| Insurance Status | 1 | 5.57 | 0.0182 | 5.77 | 0.0163 |
| Educational Level | 7 | 32.26 | <0.001 | 33.75 | <0.001 |
| Poverty Cat | 4 | 36.75 | <0.001 | 38.10 | <0.001 |
| Cardiometabolic burden (count category) | 2 | — | — | 5.04 | 0.0803 |
| Respiratory burden (count category) | 1 | — | — | 0.03 | 0.8622 |
| Cancer burden (count category) | 0 | — | — | 0.00 | — |
| Predictor | Primary | Sensitivity | |||
|---|---|---|---|---|---|
| DF | χ2 | p-Value | χ2 | p-Value | |
| Year | 3 | 3.05 | 0.3837 | 11.56 | 0.0091 |
| Cluster | 6 | 93.82 | <0.001 | 29.62 | <0.001 |
| Cluster-Year | 18 | 28.51 | 0.0547 | 28.62 | 0.0533 |
| Age | 1 | 142.50 | <0.001 | 132.08 | <0.001 |
| Race | 4 | 13.76 | 0.0081 | 11.57 | 0.0208 |
| Sex | 1 | 7.55 | 0.0060 | 9.10 | 0.0026 |
| Insurance Status | 1 | 0.73 | 0.3940 | 0.42 | 0.5150 |
| Educational Level | 7 | 83.01 | <0.001 | 73.95 | <0.001 |
| Poverty Cat | 4 | 30.97 | <0.001 | 28.81 | <0.001 |
| Cardiometabolic burden (count category) | 2 | — | — | 29.54 | <0.001 |
| Respiratory burden (count category) | 1 | — | — | 14.44 | 0.001 |
| Cancer burden (count category) | 0 | — | — | 0.00 | — |
| Predictor | Primary | Sensitivity | |||
|---|---|---|---|---|---|
| DF | χ2 | p-Value | χ2 | p-Value | |
| Year | 3 | 3.02 | 0.3880 | 6.47 | 0.0909 |
| Cluster | 6 | 63.14 | <0.001 | 17.62 | 0.0072 |
| Cluster-Year | 18 | 19.12 | 0.3842 | 19.13 | 0.3836 |
| Age | 1 | 31.37 | <0.001 | 33.57 | <0.001 |
| Race | 4 | 31.19 | <0.001 | 29.59 | <0.001 |
| Sex | 1 | 17.61 | <0.001 | 18.37 | <0.001 |
| Insurance Status | 1 | 0.37 | 0.5407 | 0.46 | 0.4960 |
| Educational Level | 7 | 16.31 | 0.0225 | 16.30 | 0.0225 |
| Poverty Cat | 4 | 27.84 | <0.001 | 26.89 | <0.001 |
| Cardiometabolic burden (count category) | 2 | — | — | 2.16 | 0.3391 |
| Respiratory burden (count category) | 1 | — | — | 8.70 | 0.0032 |
| Cancer burden (count category) | 0 | — | — | 0.00 | — |
| Predictor | Primary | Sensitivity | |||
|---|---|---|---|---|---|
| DF | χ2 | p-Value | χ2 | p-Value | |
| Year | 3 | 2.67 | 0.4450 | 1.48 | 0.6869 |
| Cluster | 6 | 45.34 | <0.001 | 9.27 | 0.1591 |
| Cluster-Year | 18 | 16.91 | 0.5294 | 17.00 | 0.5231 |
| Age | 1 | 26.53 | <0.001 | 20.87 | <0.001 |
| Race | 4 | 18.88 | 0.001 | 17.12 | 0.0018 |
| Sex | 1 | 9.11 | 0.0025 | 9.17 | 0.0025 |
| Insurance Status | 1 | 10.98 | <0.001 | 10.33 | 0.0013 |
| Educational Level | 7 | 12.49 | 0.0856 | 13.88 | 0.0533 |
| Poverty Cat | 4 | 36.23 | <0.001 | 34.62 | <0.001 |
| Cardiometabolic burden (count category) | 2 | — | — | 11.12 | 0.0038 |
| Respiratory burden (count category) | 1 | — | — | 0.21 | 0.6480 |
| Cancer burden (count category) | 0 | — | — | 0.00 | — |
| Predictor | Total Expenditure (β, SE) | OOP Spending (β, SE) | HRQL (β, SE) | MHRQL (β, SE) | Inpatient Stay (β, SE) |
|---|---|---|---|---|---|
| Intercept | 1.6394 (0.2988) *** | 0.1655 (0.2501) | 51.841 (0.6679) *** | 55.5064 (0.7729) *** | −3.6957 (0.3196) *** |
| Year 2020 | −0.0878 (0.1318) | −0.0951 (0.088) | 0.2088 (0.2907) | −0.7259 (0.3271) * | −0.117 (0.1862) |
| Year 2021 | 0.0196 (0.1161) | 0.1925 (0.1075) | −0.3434 (0.2906) | −0.8623 (0.4135) * | −0.2314 (0.1949) |
| Year 2022 | 0.0546 (0.1163) | 0.2792 (0.1241) * | −0.8471 (0.3036) ** | −0.8893 (0.3922) * | −0.1703 (0.2029) |
| Year 2019 | 0 | 0 | 0 | 0 | 0 |
| Cluster 1 | 0.6143 (0.3167) | 0.4428 (0.194) * | −2.97 (0.9675) ** | −2.0464 (1.1865) | 0.9 (0.3906) * |
| Cluster 2 | 0.2955 (0.1107) ** | 0.2482 (0.1034) * | −2.6836 (0.5291) *** | −3.0669 (0.5242) *** | 0.4252 (0.1877) * |
| Cluster 3 | 0.7983 (0.3867) * | 0.2535 (0.2905) | 0.8423 (1.413) | −2.263 (1.9058) | −0.353 (0.5998) |
| Cluster 4 | 0.8477 (0.1356) *** | 0.3845 (0.1464) ** | −8.882 (1.1141) *** | −7.0427 (1.2378) *** | 1.3714 (0.2199) *** |
| Cluster 5 | 0.8078 (0.2041) *** | 0.2641 (0.1614) | −6.2555 (1.6793) *** | −2.5273 (1.0655) * | 1.0251 (0.3412) ** |
| Cluster 6 | 0.6554 (0.1994) *** | 0.1539 (0.1708) | −7.5567 (2.2901) *** | −5.0189 (2.3153) * | 0.7784 (0.3882) * |
| Cluster 0 | 0 | 0 | 0 | 0 | 0 |
| Cluster 1 * 2020 | −0.3679 (0.3461) | −0.2827 (0.2834) | 1.5721 (0.7308) * | −0.5376 (1.0892) | −0.5106 (0.5322) |
| Cluster 1 * 2021 | −0.1865 (0.4016) | −0.5406 (0.2709) * | 0.5117 (1.0193) | −1.6289 (1.4962) | −0.3658 (0.436) |
| Cluster 1 * 2022 | −0.1429 (0.356) | −0.6569 (0.2519) ** | 1.0222 (0.8444) | −0.2179 (1.0701) | −0.7937 (0.5586) |
| Cluster 1 * 2019 | 0 | 0 | 0 | 0 | 0 |
| Cluster 2 * 2020 | 0.2096 (0.2095) | −0.1083 (0.1205) | −0.2525 (0.438) | 0.5686 (0.5058) | −0.0086 (0.248) |
| Cluster 2 * 2021 | 0.0284 (0.1555) | −0.1755 (0.1523) | −0.2621 (0.4563) | 0.8014 (0.5459) | −0.0062 (0.2426) |
| Cluster 2 * 2022 | 0.0203 (0.1434) | −0.3156 (0.1545) * | −0.3481 (0.5148) | 1.1999 (0.5388) * | 0.1474 (0.2658) |
| 0 | 0 | 0 | 0 | 0 | |
| Cluster 3 * 2020 | −0.4571 (0.4719) | −0.4671 (0.2211) * | −2.9505 (1.3218) * | −0.9183 (1.7336) | 0.5186 (0.9603) |
| Cluster 3 * 2021 | −0.2138 (0.4408) | −0.3621 (0.3148) | −2.3027 (1.2667) | 0.2669 (1.9602) | 1.0066 (0.7945) |
| Cluster 3 * 2022 | −0.5104 (0.4769) | −0.7058 (0.3291) * | −4.0024 (1.8366) * | −0.6806 (1.2431) | 0.336 (1.0067) |
| 0 | 0 | 0 | 0 | 0 | |
| Cluster 4 * 2020 | 0.0185 (0.179) | 0.2184 (0.1801) | −0.3961 (0.6981) | 0.3825 (0.8119) | −0.7701 (0.2964) ** |
| Cluster 4 * 2021 | 0.121 (0.185) | −0.1855 (0.1995) | 1.8452 (0.8372) * | 1.572 (1.1359) | −0.1425 (0.289) |
| Cluster 4 * 2022 | 0.0042 (0.1824) | −0.3973 (0.2114) | 1.6648 (1.0005) | 1.583 (1.1588) | −0.2905 (0.3004) |
| 0 | 0 | 0 | 0 | 0 | |
| Cluster 5 * 2020 | 0.0311 (0.2515) | 0.0172 (0.1967) | 0.3442 (1.4126) | 1.908 (1.0444) | 0.1415 (0.3385) |
| Cluster 5 * 2021 | −0.3528 (0.2346) | −0.3801 (0.2385) | 2.0813 (1.6573) | 0.0674 (1.1054) | −0.495 (0.4914) |
| Cluster 5 * 2022 | −0.3595 (0.2567) | −0.3284 (0.2337) | 3.6614 (1.6793) * | −1.4388 (1.1153) | −0.502 (0.4958) |
| 0 | 0 | 0 | 0 | 0 | |
| Cluster 6 * 2020 | 0.5145 (0.3369) | 0.6363 (0.3253) | −0.1405 (1.3824) | −0.1176 (1.2862) | −0.3143 (0.5769) |
| Cluster 6 * 2021 | 0.1524 (0.3142) | 0.2486 (0.3151) | 0.9395 (2.0668) | 0.0705 (1.6144) | 0.6911 (0.7746) |
| Cluster 6 * 2022 | −0.0269 (0.2627) | 0.399 (0.4359) | −1.1645 (1.9254) | 2.1807 (1.6471) | 0.446 (0.4983) |
| Age | 0.017 (0.0022) *** | 0.0145 (0.0019) *** | −0.1799 (0.0118) *** | 0.0695 (0.0125) *** | 0.0195 (0.0038) *** |
| Non-Hispanic White Only | 0.1366 (0.1372) | 0.3377 (0.0963) *** | −1.1236 (0.4102) ** | −2.5622 (0.4848) *** | 0.2578 (0.1369) |
| Non-Hispanic Black Only | −0.0828 (0.1599) | −0.1051 (0.1247) | −1.6349 (0.6772) * | −2.0684 (0.7586) ** | 0.3037 (0.1788) |
| Non-Hispanic Asian Only | −0.2312 (0.2084) | 0.0162 (0.2105) | −0.3892 (0.6542) | −1.0795 (0.8591) | −0.5849 (0.2774) * |
| Non-Hispanic other or Multiple race | 0.1547 (0.1929) | 0.2763 (0.1992) | −3.159 (1.2) ** | −4.5762 (1.8109) * | 0.6699 (0.3154) * |
| Hispanic | 0 | 0 | 0 | 0 | 0 |
| Male | −0.1009 (0.0692) | −0.1533 (0.0611) * | 0.9432 (0.3435) ** | 1.574 (0.3735) *** | −0.3 (0.0972) ** |
| Female | 0 | 0 | 0 | 0 | 0 |
| Insured | 0.1763 (0.3123) | −0.4573 (0.1626) ** | −0.2925 (0.3432) | 0.2859 (0.4658) | 0.6996 (0.2391) ** |
| Not Insured | 0 | 0 | 0 | 0 | 0 |
| GED | −0.246 (0.203) | −0.3692 (0.1854) * | −0.3603 (1.2369) | −3.0719 (1.4205) * | −0.2891 (0.2715) |
| High School Diploma | −0.1386 (0.1587) | 0.0064 (0.1567) | 1.5719 (0.6049) ** | −0.0133 (0.7887) | −0.1383 (0.1666) |
| Bachelor’s Degree | −0.1637 (0.1763) | 0.2953 (0.1619) | 4.0425 (0.6571) *** | −0.3895 (0.8568) | −0.347 (0.1934) |
| Master’s Degree | −0.0146 (0.184) | 0.3647 (0.1628) * | 5.2604 (0.707) *** | 0.5715 (0.868) | −0.0448 (0.2121) |
| Doctorate Degree | −0.0036 (0.2816) | 0.2549 (0.2107) | 4.7453 (1.0213) *** | 1.5504 (1.0668) | −0.3047 (0.337) |
| Other Degree | 0.1966 (0.2605) | 0.1664 (0.1772) | 2.7293 (0.7824) *** | −0.7796 (0.9432) | −0.2146 (0.2114) |
| Underage 16 | −0.291 (0.2188) | 0.1678 (0.1871) | 1.9473 (0.9395) * | 3.1659 (2.2247) | −0.9439 (0.3275) ** |
| No degree | 0 | 0 | 0 | 0 | 0 |
| Poor | 0.16 (0.162) | −0.5473 (0.1026) *** | −2.2308 (0.3912) *** | −2.2475 (0.4524) *** | 0.7851 (0.1424) *** |
| Near Poor | 0.009 (0.1068) | −0.5371 (0.1282) *** | −1.1582 (0.4567) * | −1.4672 (0.5017) ** | 0.7467 (0.1756) *** |
| Low Income | −0.0791 (0.0998) | −0.2481 (0.0863) ** | −1.3477 (0.3755) *** | −1.1105 (0.3749) ** | 0.7495 (0.1522) *** |
| Middle Income | −0.1731 (0.0936) | −0.1977 (0.0699) ** | −0.5375 (0.2673) * | −1.0593 (0.3021) *** | 0.2567 (0.111) * |
| High Income | 0 | 0 | 0 | 0 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alliu, I.; Thapa, S.; Yu, L.; Shehaj, B.; Asifat, O. Economic and Humanistic Burden of Multimorbidity in the United States: A Longitudinal Study of Expenditure and Quality of Life Trajectories, 2019–2022. Int. J. Environ. Res. Public Health 2025, 22, 1870. https://doi.org/10.3390/ijerph22121870
Alliu I, Thapa S, Yu L, Shehaj B, Asifat O. Economic and Humanistic Burden of Multimorbidity in the United States: A Longitudinal Study of Expenditure and Quality of Life Trajectories, 2019–2022. International Journal of Environmental Research and Public Health. 2025; 22(12):1870. https://doi.org/10.3390/ijerph22121870
Chicago/Turabian StyleAlliu, Ibrahim, Subash Thapa, Lili Yu, Blerta Shehaj, and Olamide Asifat. 2025. "Economic and Humanistic Burden of Multimorbidity in the United States: A Longitudinal Study of Expenditure and Quality of Life Trajectories, 2019–2022" International Journal of Environmental Research and Public Health 22, no. 12: 1870. https://doi.org/10.3390/ijerph22121870
APA StyleAlliu, I., Thapa, S., Yu, L., Shehaj, B., & Asifat, O. (2025). Economic and Humanistic Burden of Multimorbidity in the United States: A Longitudinal Study of Expenditure and Quality of Life Trajectories, 2019–2022. International Journal of Environmental Research and Public Health, 22(12), 1870. https://doi.org/10.3390/ijerph22121870






