Inequality in the Distribution and Utilization of Healthcare Resources in Kazakhstan (2002–2023): A Spatiotemporal Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Area
2.2. Data Sources
2.3. Variables
2.4. Inequality Indices Measurement
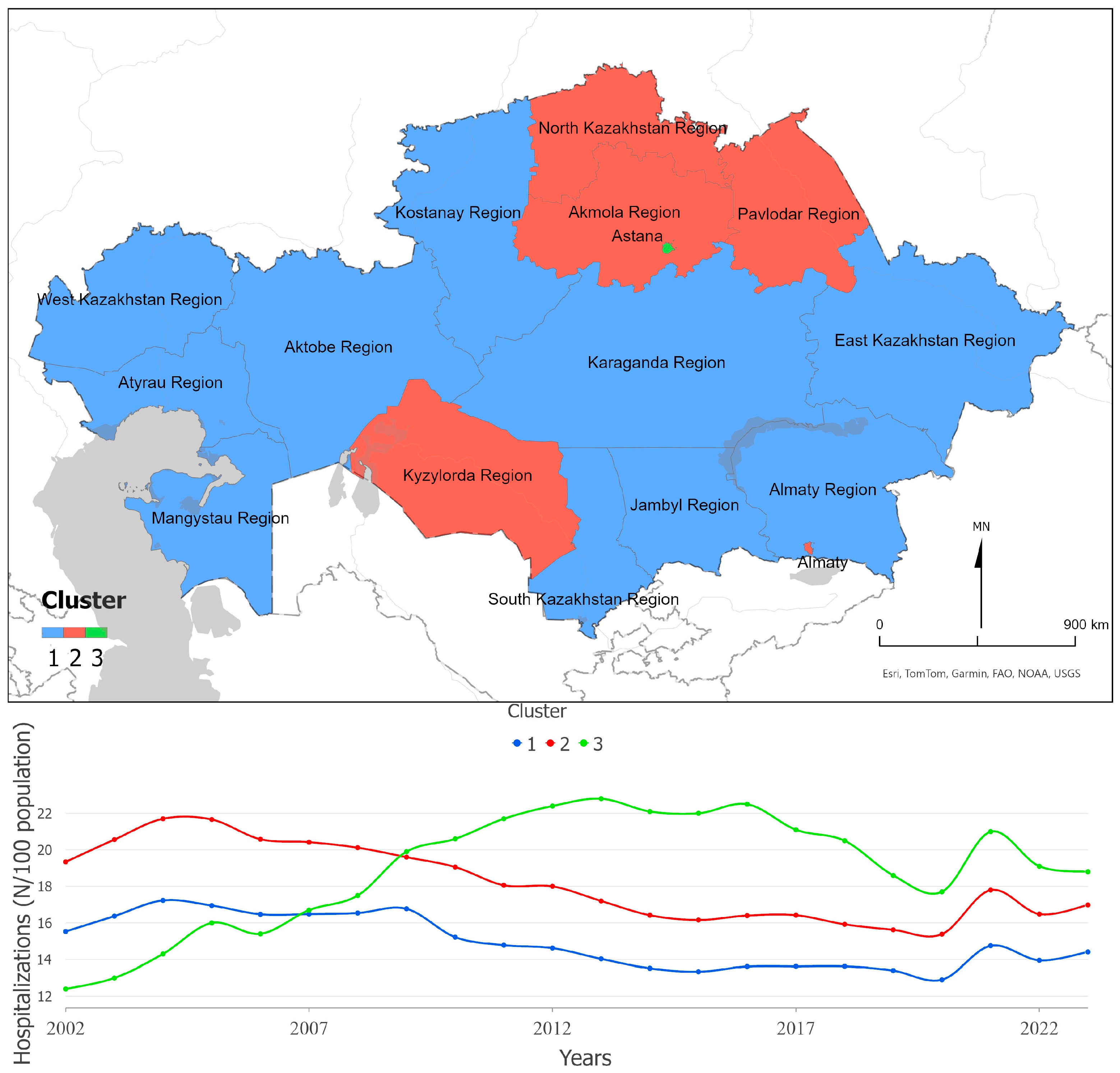
2.5. Statistical Analysis
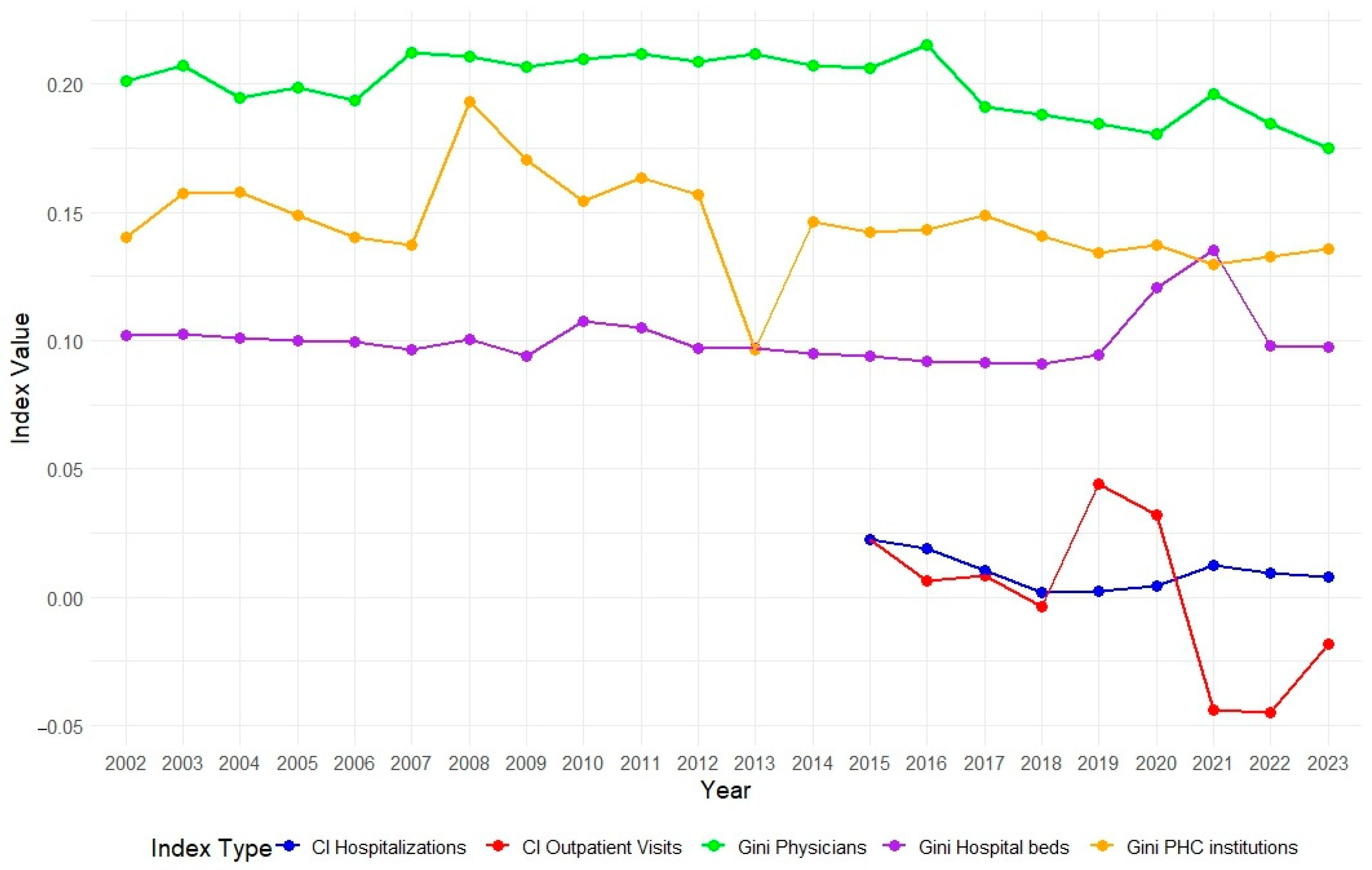
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Universal Health Coverage (UHC). Available online: https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc) (accessed on 18 July 2023).
- Takura, T.; Miura, H. Socioeconomic Determinants of Universal Health Coverage in the Asian Region. Int. J. Environ. Res. Public Health 2022, 19, 2376. [Google Scholar] [CrossRef]
- Wagstaff, A.; Neelsen, S. A Comprehensive Assessment of Universal Health Coverage in 111 Countries: A Retrospective Observational Study. Lancet Glob. Health 2020, 8, e39–e49. [Google Scholar] [CrossRef]
- Semenova, Y.; Lim, L.; Salpynov, Z.; Gaipov, A.; Jakovljevic, M. Historical Evolution of Healthcare Systems of Post-Soviet Russia, Belarus, Kazakhstan, Kyrgyzstan, Tajikistan, Turkmenistan, Uzbekistan, Armenia, and Azerbaijan: A Scoping Review. Heliyon 2024, 10, e29550. [Google Scholar] [CrossRef]
- Kumar, A.B.; Izekenova, A.; Abikulova, A. Inpatient Care in Kazakhstan: A Comparative Analysis. J. Res. Med. Sci. 2013, 18, 549–553. [Google Scholar] [PubMed]
- On Approval of the Concept of Development of Healthcare of the Republic of Kazakhstan Until 2026—IPS “Adilet”. Available online: https://adilet.zan.kz/rus/docs/P2200000945 (accessed on 28 November 2024).
- On Compulsory Social Medical Insurance—“Adilet” LIS. Available online: https://adilet.zan.kz/eng/docs/Z1500000405?utm_source=chatgpt.com (accessed on 29 October 2025).
- Spankulova, L.; Karatayev, M.; Clarke, M.L. Trends in Socioeconomic Health Inequalities in KazakhstanNational Household Surveys Analysis. Communist Post-Communist Stud. 2020, 53, 177–190. [Google Scholar] [CrossRef]
- Kireyeva, A.A.; Nurbatsin, A.S.; Khalitova, M.M. Assessing Inequality of Income Distribution and Education in the Regions of Kazakhstan. Econ. Reg. 2023, 19, 741–752. [Google Scholar] [CrossRef]
- Measuring and Decomposing Socioeconomic-Related Inequality in the Use of Oral Health Services Among Chinese Adults—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/32959367/ (accessed on 14 February 2025).
- Su, M.; Zhang, T.; Zhang, W.; Li, Z.; Fan, X. Decomposition Analysis on the Equity of Health Examination Utilization for the Middle-Aged and Elderly People in China: Based on Longitudinal CHARLS Data from 2011 to 2018. BMC Public Health 2024, 24, 998. [Google Scholar] [CrossRef]
- Yang, X.; Lin, C.; Qin, J.; Zhang, Y.; Zhang, L. Analysis on Equity of Health Service Utilization and Influencing Factors in Patients with Hypertension in China: A Longitudinal Study. BMC Health Serv. Res. 2024, 24, 1644. [Google Scholar] [CrossRef]
- Andersen, R.M. Revisiting the Behavioral Model and Access to Medical Care: Does It Matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Everybody’s Business—Strengthening Health Systems to Improve Health Outcomes. Available online: https://www.who.int/publications/i/item/everybody-s-business----strengthening-health-systems-to-improve-health-outcomes (accessed on 30 October 2025).
- Nazia, N.; Butt, Z.A.; Bedard, M.L.; Tang, W.-C.; Sehar, H.; Law, J. Methods Used in the Spatial and Spatiotemporal Analysis of COVID-19 Epidemiology: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 8267. [Google Scholar] [CrossRef]
- Zhang, J.-C.; Liu, W.-D.; Liang, Q.; Hu, J.-L.; Norris, J.; Wu, Y.; Bao, C.-J.; Tang, F.-Y.; Huang, P.; Zhao, Y.; et al. Spatial Distribution and Risk Factors of Influenza in Jiangsu Province, China, Based on Geographical Information System. Geospat Health 2014, 8, 429–435. [Google Scholar] [CrossRef]
- Lan, Y.; Delmelle, E. Space-Time Cluster Detection Techniques for Infectious Diseases: A Systematic Review. Spat. Spatio-Temporal Epidemiol. 2023, 44, 100563. [Google Scholar] [CrossRef]
- Hosseinpoor, A.R.; Stewart Williams, J.A.; Itani, L.; Chatterji, S. Socioeconomic Inequality in Domains of Health: Results from the World Health Surveys. BMC Public Health 2012, 12, 198. [Google Scholar] [CrossRef]
- About Kazakhstan. Available online: https://beta.egov.kz/article/19305 (accessed on 15 February 2025).
- Республиканский Центр Развития Здравоохранения. Available online: https://nrchd.kz/medical-statistics (accessed on 14 February 2025).
- Публикации—Agency for Strategic Planning and Reforms of the Republic of Kazakhstan Bureau of National Statistics. Available online: https://stat.gov.kz/en/industries/labor-and-income/stat-life/publications/ (accessed on 14 February 2025).
- Conindex: Estimation of Concentration Indices—PMC. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC4819995/ (accessed on 14 February 2025).
- Montero, P.; Vilar, J.A. TSclust: An R Package for Time Series Clustering. J. Stat. Softw. 2015, 62, 1–43. [Google Scholar] [CrossRef]
- Oliveira, S.; Ribeiro, A.I.; Nogueira, P.; Rocha, J. Simulating the Effects of Mobility Restrictions in the Spread of SARS-CoV-2 in Metropolitan Areas in Portugal. PLoS ONE 2022, 17, e0274286. [Google Scholar] [CrossRef]
- Spatiotemporal Dynamics of COVID-19 Infections in Mainland Portugal. Available online: https://www.mdpi.com/2071-1050/14/16/10370 (accessed on 14 February 2025).
- Abramson, J.H. WINPEPI (PEPI-for-Windows): Computer Programs for Epidemiologists. Epidemiol. Perspect. Innov. 2004, 1, 6. [Google Scholar] [CrossRef]
- Clegg, L.X.; Hankey, B.F.; Tiwari, R.; Feuer, E.J.; Edwards, B.K. Estimating Average Annual per Cent Change in Trend Analysis. Stat. Med. 2009, 28, 3670–3682. [Google Scholar] [CrossRef] [PubMed]
- Hamed, K.H. Exact Distribution of the Mann–Kendall Trend Test Statistic for Persistent Data. J. Hydrol. 2009, 365, 86–94. [Google Scholar] [CrossRef]
- Al-Sheddi, A.; Kamel, S.; Almeshal, A.S.; Assiri, A.M. Distribution of Primary Healthcare Centers Between 2017 and 2021 Across Saudi Arabia. Cureus 2023, 15, e41932. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; He, H.; Liu, X.; Wei, H.; Feng, Q.; Wei, B. Health Resource Allocation in Western China from 2014 to 2018. Arch. Public Health 2023, 81, 30. [Google Scholar] [CrossRef] [PubMed]
- Jobalayeva, B.; Khismetova, Z.; Glushkova, N.; Kozhekenova, Z.; Abzaliyeva, A.; Berikuly, D.; Semenova, Y. The Impact of Incentive Scheme on Rural Healthcare Workforce Availability: A Case Study of Kazakhstan. Hum. Resour. Health 2024, 22, 23. [Google Scholar] [CrossRef]
- Dong, E.; Xu, J.; Sun, X.; Xu, T.; Zhang, L.; Wang, T. Differences in Regional Distribution and Inequality in Health-Resource Allocation on Institutions, Beds, and Workforce: A Longitudinal Study in China. Arch. Public Health 2021, 79, 78. [Google Scholar] [CrossRef]
- Woldemichael, A.; Takian, A.; Akbari Sari, A.; Olyaeemanesh, A. Inequalities in Healthcare Resources and Outcomes Threatening Sustainable Health Development in Ethiopia: Panel Data Analysis. BMJ Open 2019, 9, e022923. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, A.; Nasiri Pour, A.A.; Tabibi, S.J.; Raeisi, P. Developing a Hospital Bed Distribution Model in Iran. Jorjani Biomed. J. 2018, 6, 60–76. [Google Scholar] [CrossRef]
- Wang, Z.; Dong, L.; Xing, X.; Liu, Z.; Zhou, Y. Disparity in Hospital Beds’ Allocation at the County Level in China: An Analysis Based on a Health Resource Density Index (HRDI) Model. BMC Health Serv. Res. 2023, 23, 1293. [Google Scholar] [CrossRef]
- Singh, A. Shortage and Inequalities in the Distribution of Specialists across Community Health Centres in Uttar Pradesh, 2002–2012. BMC Health Serv. Res. 2019, 19, 331. [Google Scholar] [CrossRef]
- Erdenee, O.; Paramita, S.A.; Yamazaki, C.; Koyama, H. Distribution of Health Care Resources in Mongolia Using the Gini Coefficient. Hum. Resour. Health 2017, 15, 56. [Google Scholar] [CrossRef] [PubMed]
- Population Situation Analysis Kazakhstan. Available online: https://kazakhstan.unfpa.org/en/publications/population-situation-analysis-kazakhstan (accessed on 14 February 2025).
- Horev, T.; Pesis-Katz, I.; Mukamel, D.B. Trends in Geographic Disparities in Allocation of Health Care Resources in the US. Health Policy 2004, 68, 223–232. [Google Scholar] [CrossRef]
- Lucevic, A.; Péntek, M.; Kringos, D.; Klazinga, N.; Gulácsi, L.; Brito Fernandes, Ó.; Boncz, I.; Baji, P. Unmet Medical Needs in Ambulatory Care in Hungary: Forgone Visits and Medications from a Representative Population Survey. Eur. J. Health Econ. 2019, 20, 71–78. [Google Scholar] [CrossRef]
- Mollahaliloðlu, S.; Uðurluoðlu, Ö.; Iþýk, O.; Kosdak, M.; Taþkaya, S. Factors Affecting the Work of Physicians in Rural Areas of Turkey. Rural Remote Health 2015, 15, 3048. [Google Scholar]
- Rój, J.; Jankowiak, M. Socioeconomic Determinants of Health and Their Unequal Distribution in Poland. Int. J. Environ. Res. Public Health 2021, 18, 10856. [Google Scholar] [CrossRef]
- Zhang, T.; Xu, Y.; Ren, J.; Sun, L.; Liu, C. Inequality in the Distribution of Health Resources and Health Services in China: Hospitals versus Primary Care Institutions. Int. J. Equity Health 2017, 16, 42. [Google Scholar] [CrossRef]
- Equity in Public Health Spending in Ethiopia: A Benefit Incidence Analysis|Health Policy and Planning|Oxford Academic. Available online: https://academic.oup.com/heapol/article/36/Supplement_1/i4/6426100 (accessed on 28 November 2024).
- Selvaraj, S.; Karan, A.K.; Mao, W.; Hasan, H.; Bharali, I.; Kumar, P.; Ogbuoji, O.; Chaudhuri, C. Did the Poor Gain from India’s Health Policy Interventions? Evidence from Benefit-Incidence Analysis, 2004–2018. Int. J. Equity Health 2021, 20, 159. [Google Scholar] [CrossRef]
- Kirigia, D.; Okungu, V.; Chuma, J. Distribution of Public Health Care Spending: A Comparative Analysis of Sub-Saharan Africa, Asia, Latin America and High Income Countries. Afr. J. Health Econ. 2023, 2, 47–72. [Google Scholar] [CrossRef]
- Ginsburg, P.B.; Koretz, D.M. Bed Availability and Hospital Utilization: Estimates of the “Roemer Effect”. Health Care Financ. Rev. 1983, 5, 87–92. [Google Scholar] [PubMed]
- Delamater, P.L.; Messina, J.P.; Grady, S.C.; WinklerPrins, V.; Shortridge, A.M. Do More Hospital Beds Lead to Higher Hospitalization Rates? A Spatial Examination of Roemer’s Law. PLoS ONE 2013, 8, e54900. [Google Scholar] [CrossRef] [PubMed]
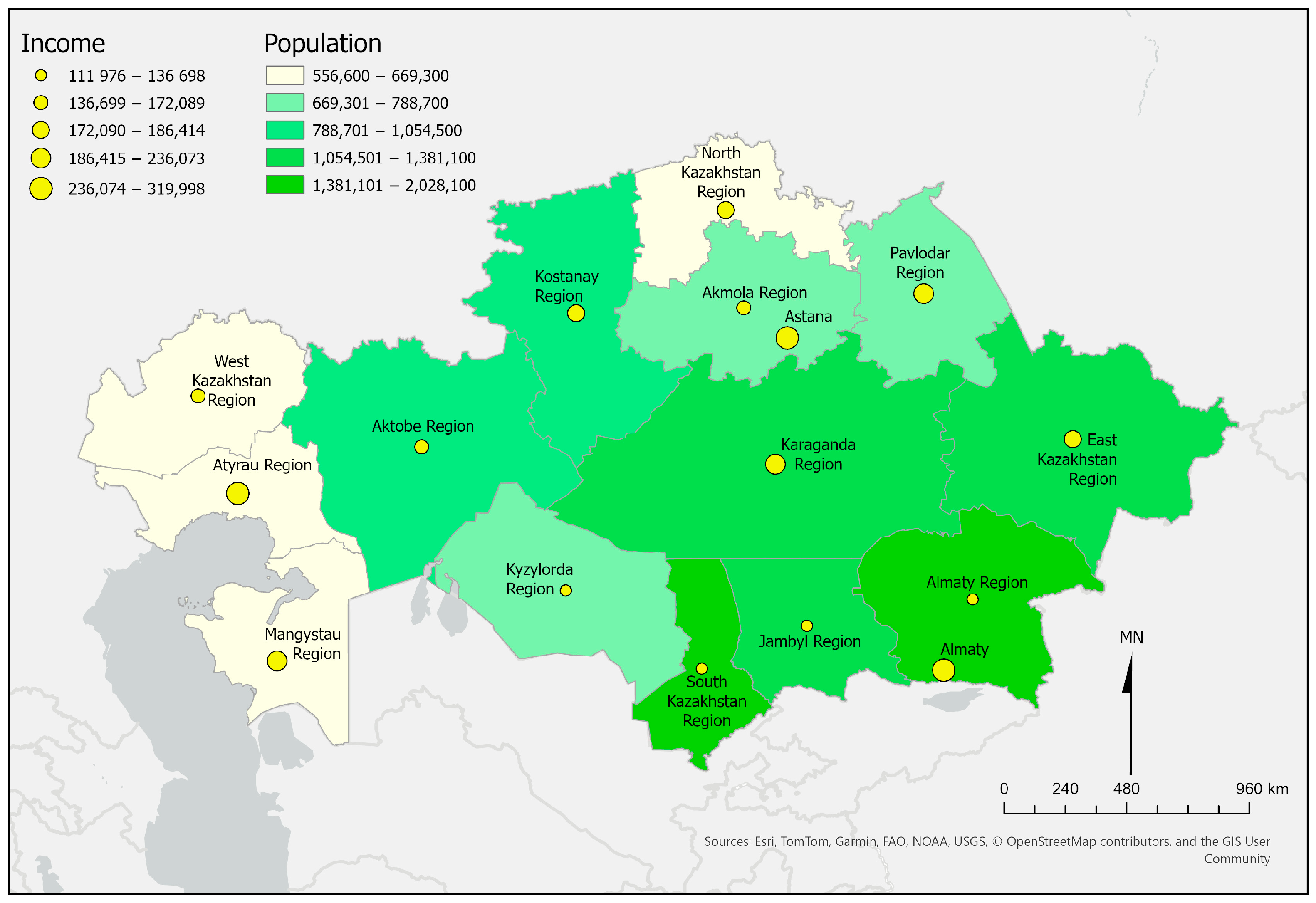

| Region | Primary Care Institutions per 10,000 Population | Hospital Beds per 10,000 Population | Outpatient Visits per Person per Year | Hospitalizations per 100 Population | Physicians per 10,000 Population | Per Capita Income in KZT * |
|---|---|---|---|---|---|---|
| Pavlodar Region | 2.24 | 50.30 | 5.20 | 16.60 | 40.85 | 199,404 |
| Jambyl Region | 1.76 | 45.20 | 5.40 | 14.40 | 29.11 | 129,051 |
| Kostanay Region | 1.71 | 52.60 | 4.50 | 14.30 | 30.49 | 178,837 |
| Mangystau Region | 1.24 | 30.70 | 4.60 | 12.90 | 31.54 | 231,263 |
| Karaganda Region | 1.78 | 53.30 | 5.40 | 16.50 | 47.12 | 236,073 |
| Kyzylorda Region | 1.91 | 53.50 | 5.90 | 18.00 | 35.56 | 136,698 |
| East Kazakhstan Region | 2.21 | 49.90 | 5.20 | 17.00 | 42.86 | 186,414.5 |
| Aktobe Region | 2.46 | 39.20 | 5.60 | 14.10 | 48.67 | 163,509 |
| Atyrau Region | 1.86 | 35.80 | 5.60 | 12.90 | 30.10 | 319,998 |
| South Kazakhstan Region | 1.06 | 37.80 | 5.60 | 15.90 | 35.90 | 111,976.5 |
| Akmola Region | 1.74 | 54.90 | 4.20 | 15.80 | 26.31 | 168,301 |
| Almaty Region | 1.50 | 42.50 | 6.50 | 12.70 | 24.36 | 129,880 |
| North Kazakhstan Region | 2.88 | 62.20 | 4.80 | 18.50 | 32.61 | 178,495 |
| Almaty | 1.59 | 41.80 | 5.50 | 16.00 | 64.94 | 288,339 |
| West Kazakhstan Region | 1.95 | 48.60 | 5.40 | 13.40 | 33.01 | 172,089 |
| Astana | 1.34 | 43.40 | 4.80 | 18.80 | 73.74 | 272,742 |
| Indicator | Gini Index (Std. Error) | p-Value |
|---|---|---|
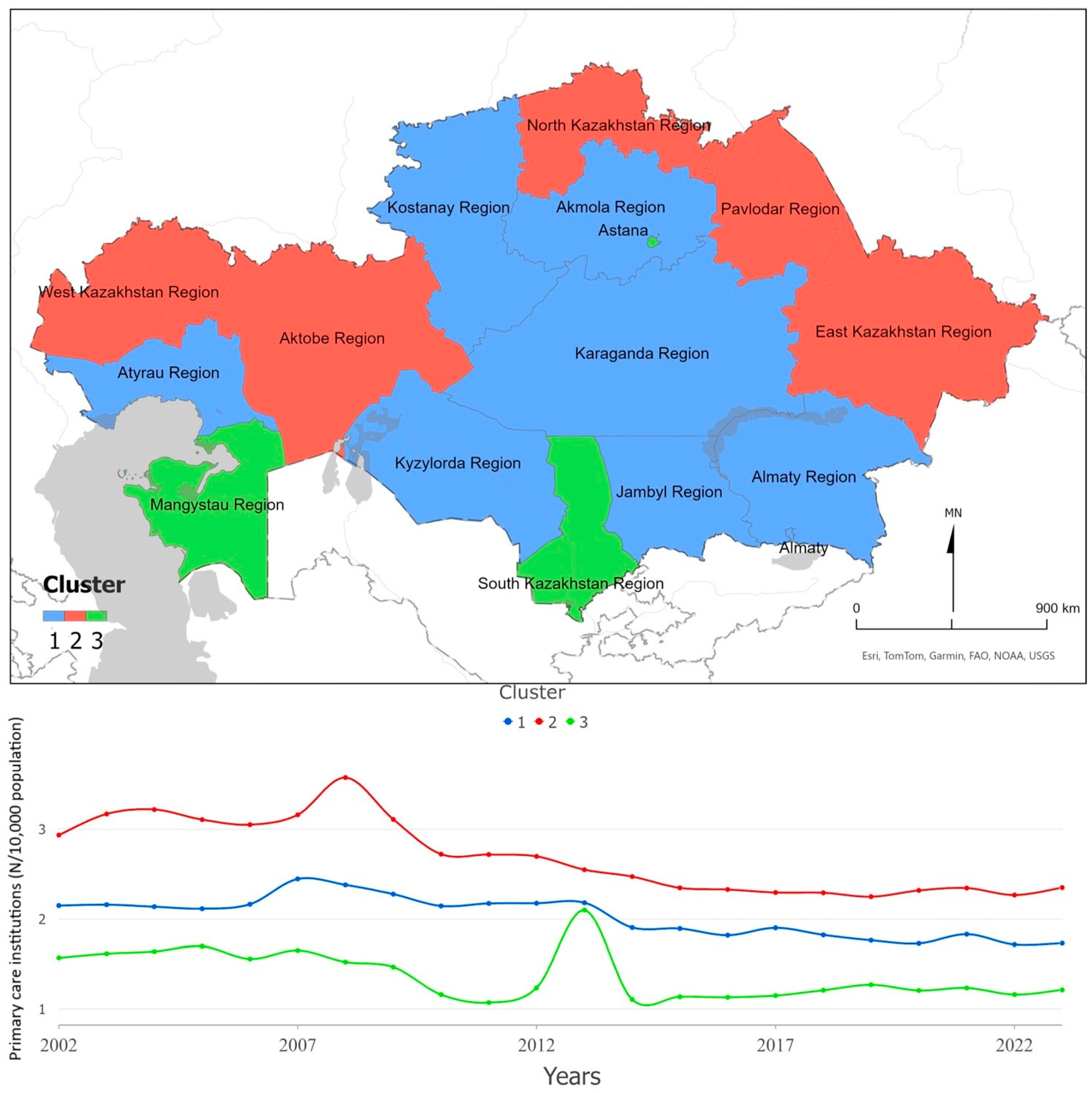
| Primary care institutions per 10,000 | 0.14 (0.11) | <0.001 |
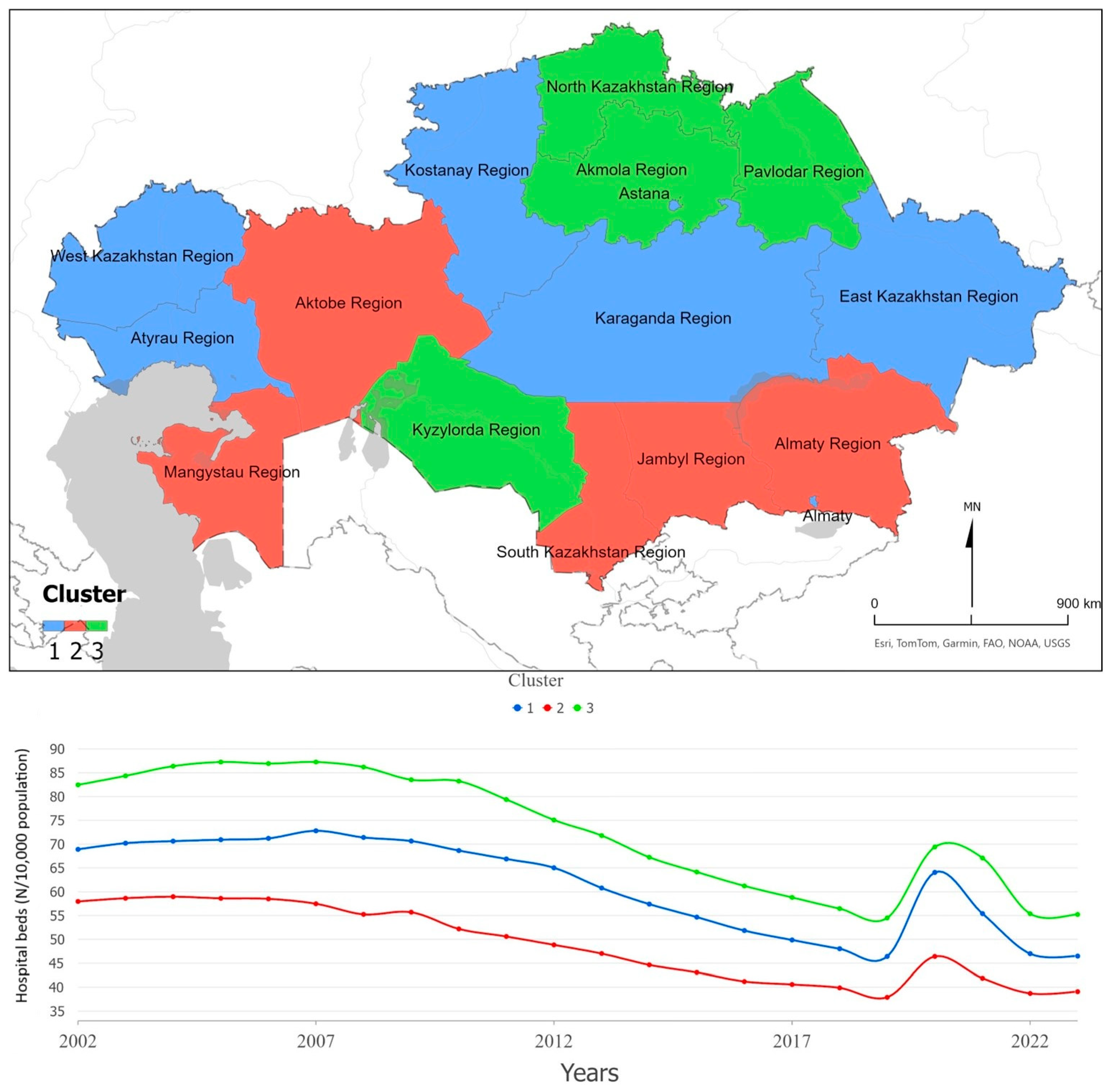
| Hospital beds per 10,000 | 0.1 (0.005) | <0.001 |
| Physicians per 10,000 | 0.18 (0.02) | <0.001 |
| Indicator | Concentration Index (Std. Error) | p-Value |
|---|---|---|
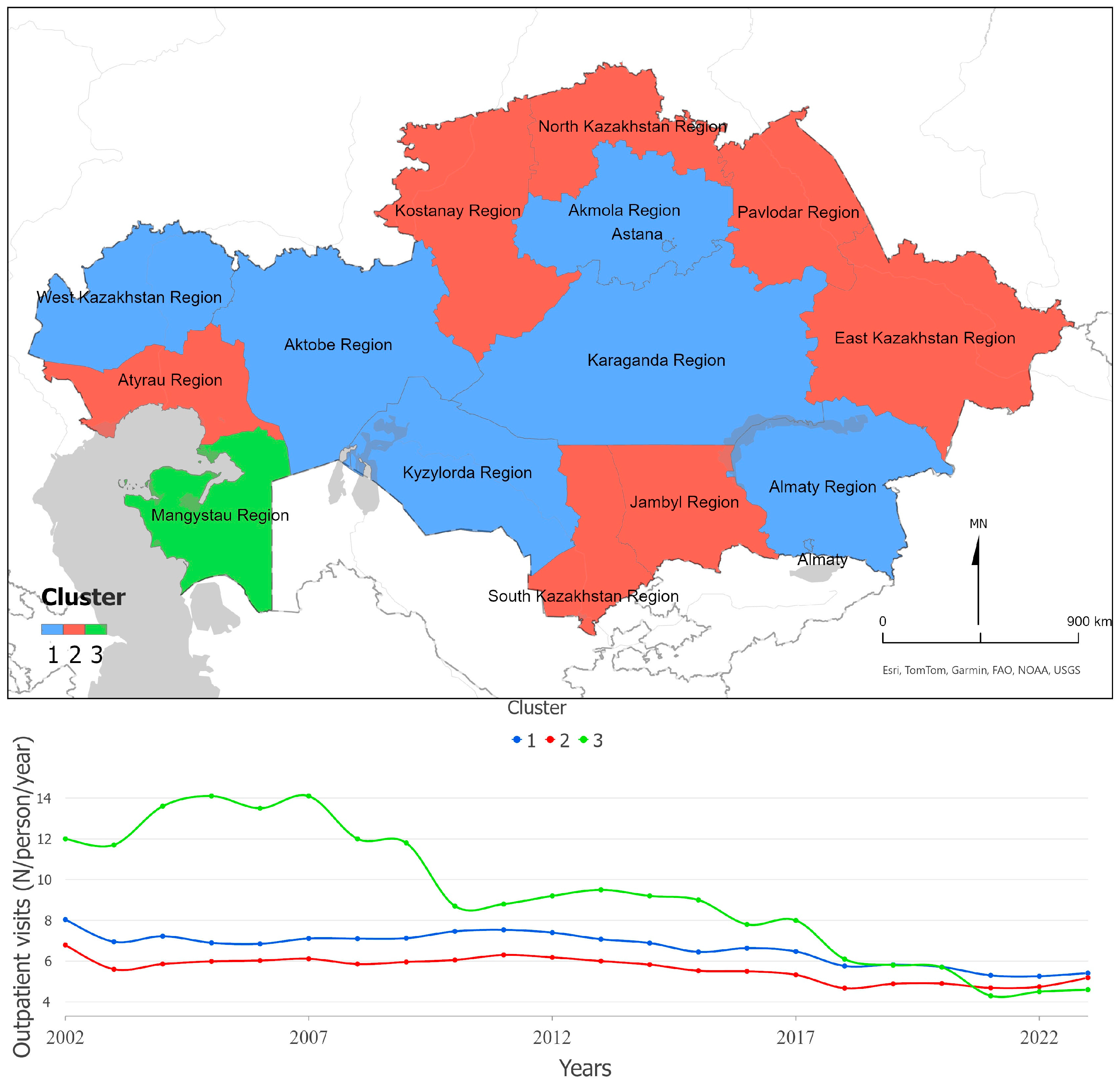
| Outpatient visits per person per year | −0.018 (0.02) | 0.26 |
| Hospitalizations per 100 | 0.007 (0.02) | 0.69 |
| Index | Relative Increase | 95% CI for Average Annual Percentage Change |
|---|---|---|
| Gini physicians | 0.06% | −0.52 to 0.41% |
| Gini hospital beds | 1.32% | 0.87 to 1.77% |
| Gini PHC institutions | 0.24% | −0.65 to 1.13% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shaltynov, A.; Abenova, M.; Baibussinova, A.; Semenova, Y.; Omarov, N.; Tanatarova, G.; Sepbossynova, A.; Rocha, J. Inequality in the Distribution and Utilization of Healthcare Resources in Kazakhstan (2002–2023): A Spatiotemporal Analysis. Int. J. Environ. Res. Public Health 2025, 22, 1762. https://doi.org/10.3390/ijerph22111762
Shaltynov A, Abenova M, Baibussinova A, Semenova Y, Omarov N, Tanatarova G, Sepbossynova A, Rocha J. Inequality in the Distribution and Utilization of Healthcare Resources in Kazakhstan (2002–2023): A Spatiotemporal Analysis. International Journal of Environmental Research and Public Health. 2025; 22(11):1762. https://doi.org/10.3390/ijerph22111762
Chicago/Turabian StyleShaltynov, Askhat, Madina Abenova, Assel Baibussinova, Yuliya Semenova, Nazarbek Omarov, Gulnaz Tanatarova, Aigerim Sepbossynova, and Jorge Rocha. 2025. "Inequality in the Distribution and Utilization of Healthcare Resources in Kazakhstan (2002–2023): A Spatiotemporal Analysis" International Journal of Environmental Research and Public Health 22, no. 11: 1762. https://doi.org/10.3390/ijerph22111762
APA StyleShaltynov, A., Abenova, M., Baibussinova, A., Semenova, Y., Omarov, N., Tanatarova, G., Sepbossynova, A., & Rocha, J. (2025). Inequality in the Distribution and Utilization of Healthcare Resources in Kazakhstan (2002–2023): A Spatiotemporal Analysis. International Journal of Environmental Research and Public Health, 22(11), 1762. https://doi.org/10.3390/ijerph22111762







