Climate Change and Air Pollution-Related Health Effects on Pain
Abstract
1. Introduction
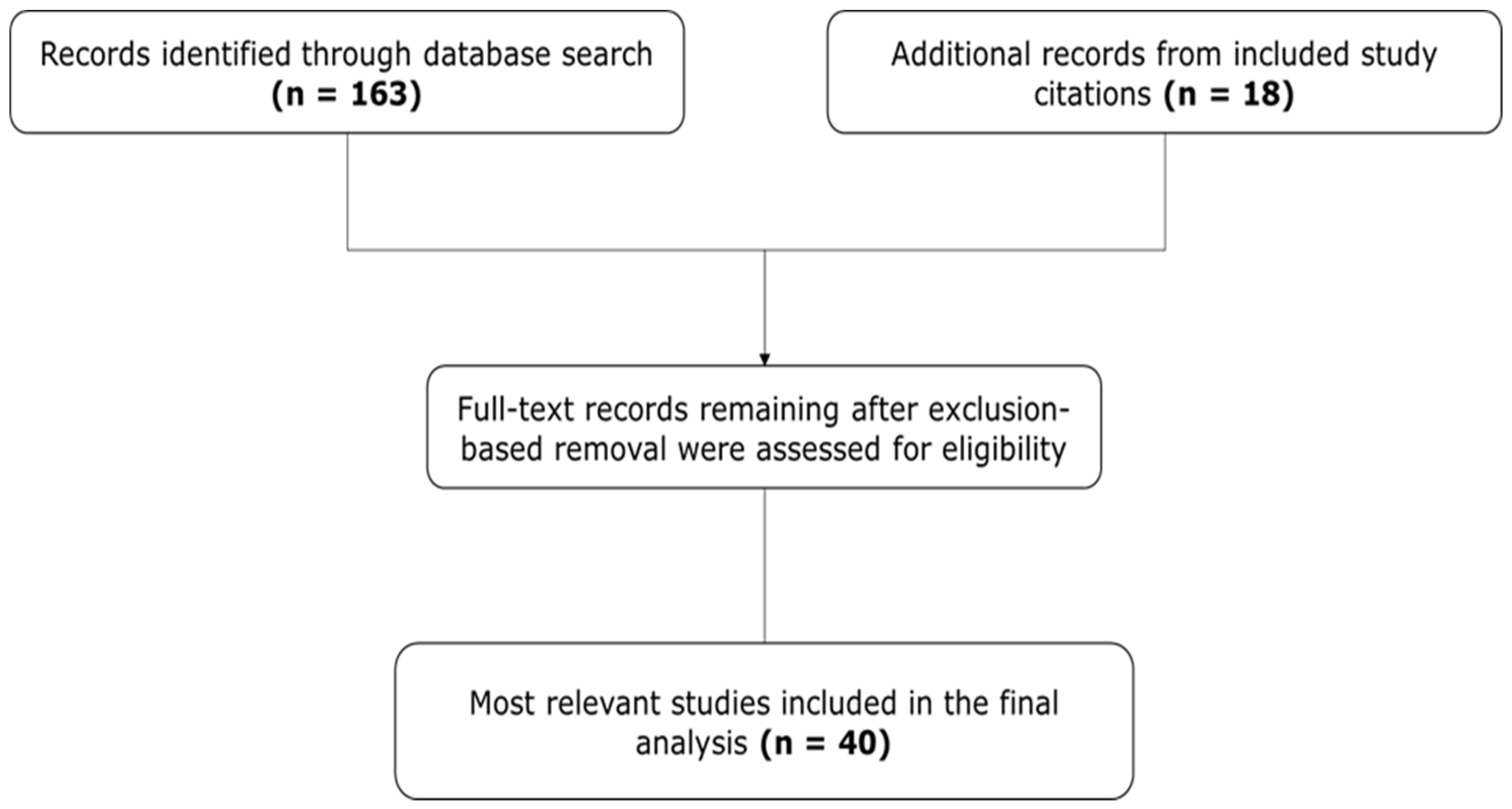
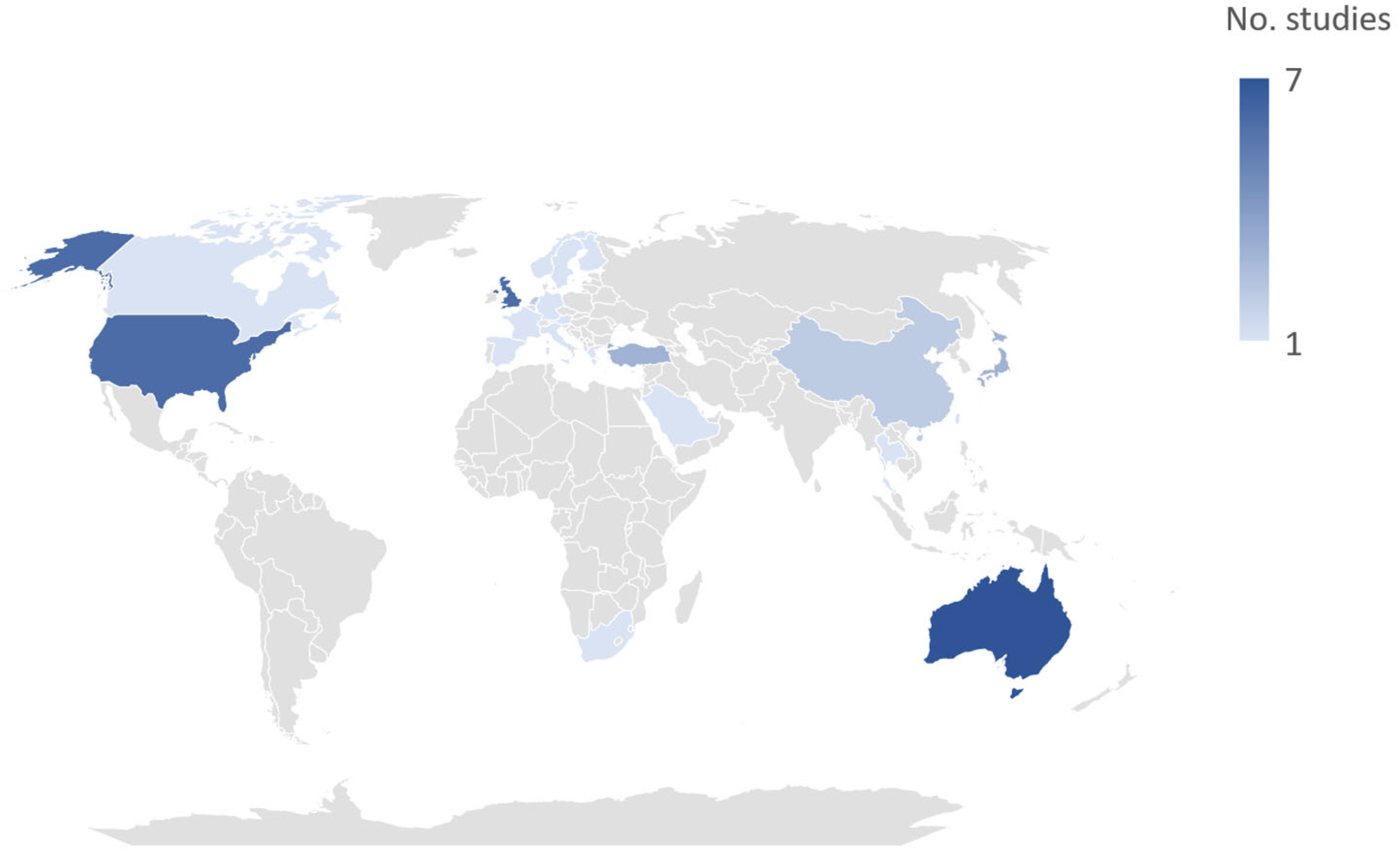
2. Materials and Methods
3. Results
3.1. Chronic Pain (Multiple Conditions)
3.2. Chronic Musculoskeletal Pain
| Study | Study Design and Participants | Key Findings |
|---|---|---|
| Multiple musculoskeletal conditions | ||
| Jena et al., 2017 [23] | Retrospective US Medicare insurance claims database analysis linking rainfall data to outpatient visits for joint or back pain; included >1.5 million adults aged ≥ 65 years (62% women; mean [SD] age, 77 [0.3] years) and >11.6 million outpatient visits |
|
| Ziade et al., 2021 [22] | Prospective, correlational analysis of data from 94 consecutive adult (≥18 years) pts (74.5% female; mean [SD] age, 56.4 [13.5] years) with chronic rheumatic disease (OA, RA, or SpA) consulting at 2 rheumatology clinics in Lebanon; pain assessed on NRS (rated 0–10) and correlated with air pollution parameters |
|
| OA | ||
| Timmermans et al., 2014 [16] | Analysis of baseline data from the European Project on OSteoArthritis included 712 older pts with OA (72.0% female; mean [SD] age, 73.5 [5.5] years) from 6 European countries (Germany, Spain, Sweden, UK, Netherlands, Italy) |
|
| Ferreira et al., 2016 [9] | Web-based case-crossover study of 171 of 345 pts in Australia (64% female; mean [SD] age, 61.7 [8.7] years) with ≥1 knee OA exacerbation |
|
| Peultier et al., 2017 [26] | Prospective study of 113 pts in France with knee OA (69.0% female; mean [SD] age, 65.3 [9.2] years) |
|
| Fu et al., 2020 [28] | Web-based case-crossover study of 129 pts aged ≥ 40 years (86% female; mean [SD] age, 62.9 [8.0] years) in Australia with hip OA and ≥1 episode of pain exacerbation |
|
| Chen et al., 2021 [29] | Analysis of outpatient data from Beijing’s Medical Claims for Employees (urban employees) database from January 2010–December 2017 in conjunction with air pollution data; included 9,797,446 adult knee OA outpatient visits (pts: 63.6% female, 63.8% elderly) |
|
| Thomas et al., 2021 [25] | Web-based, case-crossover study in 744 adults (aged ≥ 40 years) in UK with knee OA (61% female; mean [SD] age, 62.1 [10.2] years) followed over 13 weeks; pts was asked, “Did the weather feel generally cold and damp?” during periods with and without OA pain flare |
|
| Xue et al., 2021 [24] | Cross-sectional study evaluating the association between self-reported weather sensitivity and clinical symptoms and structural abnormalities of the knee in a subsample of pts from a multicenter, prospective cohort study in China; analysis included 80 pts aged > 38 years with OA of the knee (75% women) |
|
| Rheumatoid arthritis | ||
| Mandl et al., 2021 [31] | Daily correlation of clinical data from the Care for RA database with Austrian meteorological data over 12 years; included 461 patients (mean [SD] age, 55.3 [14.5] years) |
|
| Joly-Chevrier et al., 2023 [30] | Correlation of data from the RHUMADATATM clinical registry with Canadian meteorological data; included 14,200 weather-matched PROs (74.6% women) |
|
| Fibromyalgia | ||
| Smedslund et al., 2014 [33] | Analysis of data from the intervention group of a randomized, controlled trial of Web-based counseling, during which women in Norway with chronic widespread pain of FM recorded pain, activities, emotions, and thoughts 3 times/day over 5 weeks; data were correlated with meteorological variables; included 50 women (mean [SD] age, 43.0 [11.0] years) |
|
| Hayashi et al., 2021 [34] | Retrospective analysis of data from medical records of consecutive patients aged > 20 years with FM during their first visit to a tertiary care center in Japan; correlated weather sensitivity b with pain intensity measured with an NRS (scores, 0–10) and QOL as assessed with the EQ-5D-3L scale; included 64 pts (75% female; mean [SD] age, 50 [16] years) |
|
| Gout arthritis | ||
| Neogi et al., 2014 [8] | Internet-based case-crossover survey of triggers of recurrent gout arthritis included 619 adults aged ≥ 18 years with a recent history of gout residing in the US (78% male; median [range] age, 54 [21–88] years) |
|
| Orthopedic implants | ||
| Alakhras et al., 2020 [32] | Interview of 100 consecutive patients aged ≥ 14 years (56% male) with orthopedic implants followed up at an orthopedic department in Riyadh, KSA |
|
3.3. Acute Musculoskeletal Pain
3.4. Postoperative Pain
3.5. Headache
| Study | Study Design and Participants | Key Findings |
|---|---|---|
| Vodonos et al., 2015 [44] | Retrospective cohort study correlating ED visits to a medical center in southern Israel with meteorological parameters and air pollutant levels in 18,065 patients aged ≥ 18 years (56.6% female, 59.9% < 40 years) with 22,021 ED visits for headache |
|
| Yilmaz et al., 2015 [11] | Retrospective study correlating ED visits to a regional hospital in Turkey for migraine with meteorological data over a 12-month period; included 3491 patients (72% female; mean [SD] age, 36 [11] years) |
|
| Pogačar et al., 2019 [17] | Cross-sectional study assessing perception of heat stress during heat waves among workers from Slovenia (n = 216, 57.4% male) and Greece (n = 70, 77.1% male) who spent > 1/3 of their workdays outdoors |
|
| Li et al., 2019 [45] | Prospective diary-based cohort study of 98 adults aged ≥ 18 years with migraine in the greater Boston, Massachusetts, area (88% female; mean [SD] age, 35 [12] years); total of 4406 days and 870 migraine headache episodes; fixed-effects models accounted for potential confounders (e.g., age, sex, socioeconomic status) |
|
| Wright et al., 2019 [41] | Cross-sectional survey about heat-related health effects experienced by individuals in Gauteng province, South Africa, during hot weather; included data from 136 households/580 individuals |
|
| Boonruksa et al., 2020 [42] | Survey of 183 sugarcane workers (≥18 years of age) in Thailand who worked in the field (cutters, n = 90; 58.9% male; mean [SD] age, 42.0 [11.0] years) or in factories (n = 93; 94.6% male; mean [SD] age, 39.3 [7.5] years) during hottest month of harvesting; data on ambient temperatures and physiological stress also recorded |
|
| Lew et al., 2020 [46] | Case-crossover study using data from a database linking weather data with US administrative claims data; used conditional logistic regression to analyze the relationship between meteorological changes and severe migraines a in patients with and without prophylactic migraine treatment; included 34,776 patients with ≥ 1 severe migraine |
|
| Akgün et al., 2021 [48] | Prospective analysis of weather parameters and frequency and severity of headache attacks recorded in diaries by 50 pts with episodic migraine (64% female; mean [SD] age, 37.0 [11.3] years; 188 headache attacks recorded) and 50 pts with episodic TTH (80% female; mean [SD] age, 34.4 [13.2] years; 233 headache attacks recorded); study in Turkey |
|
| Van Casteren 2021 [47] | Cross-sectional, Web-based questionnaire among 6786 Dutch adults with migraine (84.4% female; mean [SD] age, 41.9 [12.1] years in females, 45.7 [13.1] years in males) |
|
| Katsuki et al., 2023 [40] | Retrospective, observational cross-sectional study in Japan; weather data and AI used to investigate the effects of weather parameters on headache occurrence; analysis included data from 4375 users of a smartphone app with an electronic diary who had moderate/severe headaches (89.2% female; mean [SD] age, 34.0 [11.2] years); 336,951 headache events; models accounted for variations in sex, age, date, and regional district |
|
| Taggart et al., 2024 [43] | Analysis of heat-related illness/injury data from a mine industry company in Australia over an 11-year period (March 2012–2023) |
|
3.6. Dysmenorrhea
3.7. Chest Pain
4. Discussion
4.1. Pain Variability Across Conditions
4.2. Exacerbating Conditions
4.2.1. Air Pollution
4.2.2. Physiological Vulnerabilities
4.2.3. Age
4.2.4. Socioeconomic Status
5. Research Gaps and Future Perspectives
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BMP | Barometric pressure |
| CGRP | Calcitonin gene-related peptide |
| CI | Confidence interval |
| CO | Carbon monoxide |
| ED | Emergency department |
| EPA | Environmental pain approach |
| EPOSA | European Project on Osteoarthritis |
| LBP | Low-back pain |
| LIC | Low-income countries |
| NO | Nitric oxide |
| NO2 | Nitrogen dioxide |
| NOx | Nitric oxides |
| O3 | Ozone |
| OA | Osteoarthritis |
| OR | Odds ratio |
| PM | Particulate matter |
| PR | Prevalence ratios |
| PROs | Patient-reported outcomes |
| QoL | Quality of Life |
| RA | Rheumatoid arthritis |
| RR | Relative risk |
| SD | Standard deviation |
| TRP | Transient receptor potential |
| TTH | Tension-type headache |
References
- Calvin, K.; Dasgupta, D.; Krinner, G.; Mukherji, A.; Thorne, P.W.; Trisos, C.; Romero, J.; Aldunce, P.; Barrett, K.; Blanco, G.; et al. IPCC, 2023: Climate Change 2023: Synthesis Report. Contribution of Working Groups I, II and III to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change, 1st ed.; Lee, H., Romero, J., Eds.; Intergovernmental Panel on Climate Change (IPCC): Geneva, Switzerland, 2023. [Google Scholar]
- State of Global Air Report 2024|State of Global Air. Available online: https://www.stateofglobalair.org/resources/report/state-global-air-report-2024 (accessed on 16 October 2025).
- Xu, J.; Su, Z.; Liu, C.; Nie, Y.; Cui, L. Climate Change, Air Pollution and Chronic Respiratory Diseases: Understanding Risk Factors and the Need for Adaptive Strategies. Environ. Health Prev. Med. 2025, 30, 7. [Google Scholar] [CrossRef]
- Ebi, K.L.; Hess, J.J. Health Risks Due To Climate Change: Inequity In Causes And Consequences: Study Examines Health Risks Due to Climate Change. Health Aff. 2020, 39, 2056–2062. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.J. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment; U.S. Global Change Research Program. J. Am. Plan. Assoc. 2016, 82, 418–419. [Google Scholar] [CrossRef]
- Adegboye, O.A.; Alele, F.O.; Castellanos, M.E.; Pak, A.; Emeto, T.I. Editorial: Environmental Stressors, Multi-Hazards and Their Impact on Health. Front. Public Health 2023, 11, 1231955. [Google Scholar] [CrossRef] [PubMed]
- Heidari, H.; Lawrence, D.A. Climate Stressors and Physiological Dysregulations: Mechanistic Connections to Pathologies. Int. J. Environ. Res. Public Health 2023, 21, 28. [Google Scholar] [CrossRef]
- Neogi, T.; Chen, C.; Niu, J.; Chaisson, C.; Hunter, D.J.; Choi, H.; Zhang, Y. Relation of Temperature and Humidity to the Risk of Recurrent Gout Attacks. Am. J. Epidemiol. 2014, 180, 372–377. [Google Scholar] [CrossRef][Green Version]
- Ferreira, M.L.; Hunter, D.J.; Fu, A.; Raihana, S.; Urquhart, D.; Ferreira, P.H. Come Rain or Shine: Is Weather a Risk Factor for Musculoskeletal Pain? A Systematic Review with Meta-Analysis of Case-Crossover Studies. Semin. Arthritis Rheum. 2024, 65, 152392. [Google Scholar] [CrossRef]
- Shulman, B.S.; Marcano, A.I.; Davidovitch, R.I.; Karia, R.; Egol, K.A. Nature’s Wrath—The Effect of Weather on Pain Following Orthopaedic Trauma. Injury 2016, 47, 1841–1846. [Google Scholar] [CrossRef]
- Yilmaz, M.; Gurger, M.; Atescelik, M.; Yildiz, M.; Gurbuz, S. Meteorologic Parameters and Migraine Headache: ED Study. Am. J. Emerg. Med. 2015, 33, 409–413. [Google Scholar] [CrossRef]
- Elser, H.; Morello-Frosch, R.; Jacobson, A.; Pressman, A.; Kioumourtzoglou, M.-A.; Reimer, R.; Casey, J.A. Air Pollution, Methane Super-Emitters, and Oil and Gas Wells in Northern California: The Relationship with Migraine Headache Prevalence and Exacerbation. Environ. Health 2021, 20, 45. [Google Scholar] [CrossRef]
- Wu, T.; Doyle, C.; Ito, J.; Ramesh, N.; Ernest, D.K.; Crespo, N.C.; Hsu, F.-C.; Oren, E. Cold Exposures in Relation to Dysmenorrhea among Asian and White Women. Int. J. Environ. Res. Public Health 2023, 21, 56. [Google Scholar] [CrossRef] [PubMed]
- Koder, J.; Dunk, J.; Rhodes, P. Climate Distress: A Review of Current Psychological Research and Practice. Sustainability 2023, 15, 8115. [Google Scholar] [CrossRef]
- Hamilton, J. “Alchemizing Sorrow Into Deep Determination”: Emotional Reflexivity and Climate Change Engagement. Front. Clim. 2022, 4, 786631. [Google Scholar] [CrossRef]
- Timmermans, E.J.; Van Der Pas, S.; Schaap, L.A.; Sánchez-Martínez, M.; Zambon, S.; Peter, R.; Pedersen, N.L.; Dennison, E.M.; Denkinger, M.; Castell, M.V.; et al. Self-Perceived Weather Sensitivity and Joint Pain in Older People with Osteoarthritis in Six European Countries: Results from the European Project on OSteoArthritis (EPOSA). BMC Musculoskelet. Disord. 2014, 15, 66. [Google Scholar] [CrossRef]
- Pogačar, T.; Žnidaršič, Z.; Kajfež Bogataj, L.; Flouris, A.D.; Poulianiti, K.; Črepinšek, Z. Heat Waves Occurrence and Outdoor Workers’ Self-Assessment of Heat Stress in Slovenia and Greece. Int. J. Environ. Res. Public Health 2019, 16, 597. [Google Scholar] [CrossRef]
- Patel, R.; Sergeant, J.; McBeth, J.; Schultz, D.; Sanders, C.; Cook, L.; Ainsworth, J.; Dixon, W. AB1042 Patient Beliefs Regarding Associations between Weather and Pain; An Analysis of Enrolment Questionnaires within “Cloudy with A Chance of Pain”. Ann. Rheum. Dis. 2016, 75, 1258. [Google Scholar] [CrossRef]
- Dixon, W.G.; Beukenhorst, A.L.; Yimer, B.B.; Cook, L.; Gasparrini, A.; El-Hay, T.; Hellman, B.; James, B.; Vicedo-Cabrera, A.M.; Maclure, M.; et al. How the Weather Affects the Pain of Citizen Scientists Using a Smartphone App. npj Digit. Med. 2019, 2, 105. [Google Scholar] [CrossRef]
- Schultz, D.M.; Beukenhorst, A.L.; Yimer, B.B.; Cook, L.; Pisaniello, H.L.; House, T.; Gamble, C.; Sergeant, J.C.; McBeth, J.; Dixon, W.G. Weather Patterns Associated with Pain in Chronic-Pain Sufferers. Bull. Am. Meteorol. Soc. 2020, 101, E555–E566. [Google Scholar] [CrossRef]
- Yimer, B.B.; Schultz, D.M.; Beukenhorst, A.L.; Lunt, M.; Pisaniello, H.L.; House, T.; Sergeant, J.C.; McBeth, J.; Dixon, W.G. Heterogeneity in the Association between Weather and Pain Severity among Patients with Chronic Pain: A Bayesian Multilevel Regression Analysis. PR9 2022, 7, e963. [Google Scholar] [CrossRef]
- Ziadé, N.; Bouzamel, M.; Mrad-Nakhlé, M.; Abi Karam, G.; Hmamouchi, I.; Abouqal, R.; Farah, W. Prospective Correlational Time-Series Analysis of the Influence of Weather and Air Pollution on Joint Pain in Chronic Rheumatic Diseases. Clin. Rheumatol. 2021, 40, 3929–3940. [Google Scholar] [CrossRef]
- Jena, A.B.; Olenski, A.R.; Molitor, D.; Miller, N. Association between Rainfall and Diagnoses of Joint or Back Pain: Retrospective Claims Analysis. BMJ 2017, 359, j5326. [Google Scholar] [CrossRef] [PubMed]
- Xue, Y.; Chen, Y.; Jiang, D.; Wang, L.; Wang, X.; Li, M.; Wu, Y.; Zhang, M.; Pang, J.; Zhan, H.; et al. Self-Reported Weather Sensitivity Is Associated with Clinical Symptoms and Structural Abnormalities in Patients with Knee Osteoarthritis: A Cross-Sectional Study. Rheumatol. Ther. 2021, 8, 1405–1417. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.J.; Rathod-Mistry, T.; Parry, E.L.; Pope, C.; Neogi, T.; Peat, G. Triggers for Acute Flare in Adults with, or at Risk of, Knee Osteoarthritis: A Web-Based Case-Crossover Study in Community-Dwelling Adults. Osteoarthr. Cartil. 2021, 29, 956–964. [Google Scholar] [CrossRef] [PubMed]
- Peultier, L.; Lion, A.; Chary-Valckenaere, I.; Loeuille, D.; Zhang, Z.; Rat, A.-C.; Gueguen, R.; Paysant, J.; Perrin, P.P. Influence of Meteorological Elements on Balance Control and Pain in Patients with Symptomatic Knee Osteoarthritis. Int. J. Biometeorol. 2017, 61, 903–910. [Google Scholar] [CrossRef]
- Ferreira, M.L.; Zhang, Y.; Metcalf, B.; Makovey, J.; Bennell, K.L.; March, L.; Hunter, D.J. The Influence of Weather on the Risk of Pain Exacerbation in Patients with Knee Osteoarthritis—A Case-Crossover Study. Osteoarthr. Cartil. 2016, 24, 2042–2047. [Google Scholar] [CrossRef]
- Fu, K.; Metcalf, B.; Bennell, K.; Zhang, Y.; Deveza, L.; Robbins, S.; Ferreira, M.; Hunter, D. Association of Weather Factors with the Risk of Pain Exacerbations in People with Hip Osteoarthritis. Scand. J. Rheumatol. 2021, 50, 68–73. [Google Scholar] [CrossRef]
- Chen, H.; Wu, J.; Wang, M.; Wang, S.; Wang, J.; Yu, H.; Hu, Y.; Shang, S. Impact of Exposure to Ambient Fine Particulate Matter Pollution on Adults with Knee Osteoarthritis. Int. J. Environ. Res. Public Health 2021, 18, 9644. [Google Scholar] [CrossRef]
- Joly-Chevrier, M.; Coupal, L.; Choquette Sauvageau, L.; Choquette, D. POS0325 rheumatoid arthritis patients and weather patterns: A rhumadataTM study of 14,200 patient-reported outcomes matched with meteorological data. Ann. Rheum. Dis. 2023, 82, 408. [Google Scholar] [CrossRef]
- Mandl, P.; Studenic, P.; Alasti, F.; Kaltenberger, R.; Kerschbaumer, A.; Krennert, T.; Smolen, J.S.; Aletaha, D. POS0547 meteorological variables have different influence on core measures of disease activity in patients with rheumatoid arthritis. Ann. Rheum. Dis. 2021, 80, 508. [Google Scholar] [CrossRef]
- Alakhras, J.T.; Alakhras, T.M. Effect of Cold Weather on Patients with Orthopedic Implants. J. Taibah Univ. Med. Sci. 2020, 15, 325–328. [Google Scholar] [CrossRef]
- Smedslund, G.; Eide, H.; Kristjansdottir, Ó.B.; Nes, A.A.G.; Sexton, H.; Fors, E.A. Do Weather Changes Influence Pain Levels in Women with Fibromyalgia, and Can Psychosocial Variables Moderate These Influences? Int. J. Biometeorol. 2014, 58, 1451–1457. [Google Scholar] [CrossRef]
- Hayashi, K.; Miki, K.; Hayashi, N.; Hashimoto, R.; Yukioka, M. Weather Sensitivity Associated with Quality of Life in Patients with Fibromyalgia. BMC Rheumatol. 2021, 5, 14. [Google Scholar] [CrossRef] [PubMed]
- Steffens, D.; Maher, C.G.; Li, Q.; Ferreira, M.L.; Pereira, L.S.M.; Koes, B.W.; Latimer, J. Effect of Weather on Back Pain: Results From a Case-Crossover Study. Arthritis Care Res. 2014, 66, 1867–1872. [Google Scholar] [CrossRef] [PubMed]
- Duong, V.; Maher, C.G.; Steffens, D.; Li, Q.; Hancock, M.J. Does Weather Affect Daily Pain Intensity Levels in Patients with Acute Low Back Pain? A Prospective Cohort Study. Rheumatol. Int. 2016, 36, 679–684. [Google Scholar] [CrossRef] [PubMed]
- Beilken, K.; Hancock, M.J.; Maher, C.G.; Li, Q.; Steffens, D. Acute Low Back Pain? Do Not Blame the Weather—A Case-Crossover Study. Pain Med. 2016, 18, pnw126. [Google Scholar] [CrossRef]
- Kar, M.; Bayar Muluk, N.; Susaman, N.; Çetiner, H.; Cingi, C. How Do Different Climatic Conditions Affect the Quality of Life of Patients Following Septoplasty or Septorhinoplasty? J. Plast. Reconstr. Aesthetic Surg. 2023, 77, 54–62. [Google Scholar] [CrossRef]
- Migraine and Other Headache Disorders. Available online: https://www.who.int/news-room/fact-sheets/detail/headache-disorders (accessed on 16 October 2025).
- Katsuki, M.; Tatsumoto, M.; Kimoto, K.; Iiyama, T.; Tajima, M.; Munakata, T.; Miyamoto, T.; Shimazu, T. Investigating the Effects of Weather on Headache Occurrence Using a Smartphone Application and Artificial Intelligence: A Retrospective Observational Cross-sectional Study. Headache 2023, 63, 585–600. [Google Scholar] [CrossRef]
- Wright, C.Y.; Dominick, F.; Kapwata, T.; Bidassey-Manilal, S.; Engelbrecht, J.C.; Stich, H.; Mathee, A.; Matooane, M. Socio-Economic, Infrastructural and Health-Related Risk Factors Associated with Adverse Heat-Health Effects Reportedly Experienced during Hot Weather in South Africa. Pan Afr. Med. J. 2019, 34, 40. [Google Scholar] [CrossRef]
- Boonruksa, P.; Maturachon, T.; Kongtip, P.; Woskie, S. Heat Stress, Physiological Response, and Heat-Related Symptoms among Thai Sugarcane Workers. Int. J. Environ. Res. Public Health 2020, 17, 6363. [Google Scholar] [CrossRef]
- Taggart, S.M.; Girard, O.; Landers, G.J.; Wallman, K.E. Heat Exposure as a Cause of Injury and Illness in Mine Industry Workers. Ann. Work Expo. Health 2024, 68, 325–331. [Google Scholar] [CrossRef]
- Vodonos, A.; Novack, V.; Zlotnik, Y.; Ifergane, G. Ambient Air Pollution, Weather and Daily Emergency Department Visits for Headache. Cephalalgia 2015, 35, 1085–1091. [Google Scholar] [CrossRef]
- Li, W.; Bertisch, S.M.; Mostofsky, E.; Buettner, C.; Mittleman, M.A. Weather, Ambient Air Pollution, and Risk of Migraine Headache Onset among Patients with Migraine. Environ. Int. 2019, 132, 105100. [Google Scholar] [CrossRef]
- Lew, C.; Min, S.; Thiel, E.; Irwin, D. PND55 impact of barometric pressure changes and prophylactic migraine medication use on the occurrence of severe migraines: A case-crossover study using linked weather and claims data. Value Health 2020, 23, S269. [Google Scholar] [CrossRef]
- Van Casteren, D.S.; Verhagen, I.E.; Onderwater, G.L.; MaassenVanDenBrink, A.; Terwindt, G.M. Sex Differences in Prevalence of Migraine Trigger Factors: A Cross-Sectional Study. Cephalalgia 2021, 41, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Akgün, N.; Aciman Demirel, E.; Açikgöz, M.; Çelebi, U.; Köktürk, F.; Atasoy, H.T. The Effect of Weather Variables on the Severity, Duration, and Frequency of Headache Attacks in the Cases of Episodic Migraine and Episodic Tension-Type Headache. Turk. J. Med. Sci. 2021, 51, 1406–1412. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Ohde, S.; Urayama, K.Y.; Takahashi, O.; Fukui, T. Weather and Health Symptoms. Int. J. Environ. Res. Public Health 2018, 15, 1670. [Google Scholar] [CrossRef]
- Lin, S.-Y.; Yang, Y.-C.; Lin, C.-C.; Chang, C.Y.-Y.; Hsu, W.-H.; Wang, I.-K.; Lin, C.-D.; Hsu, C.-Y.; Kao, C.-H. Increased Incidence of Dysmenorrhea in Women Exposed to Higher Concentrations of NO, NO2, NOx, CO, and PM2.5: A Nationwide Population-Based Study. Front. Public Health 2021, 9, 682341. [Google Scholar] [CrossRef]
- Dawson, L.P.; Andrew, E.; Nehme, Z.; Bloom, J.; Cox, S.; Anderson, D.; Stephenson, M.; Lefkovits, J.; Taylor, A.J.; Kaye, D.; et al. Temperature-Related Chest Pain Presentations and Future Projections with Climate Change. Sci. Total Environ. 2022, 848, 157716. [Google Scholar] [CrossRef]
- Hyrkäs-Palmu, H.; Jaakkola, M.S.; Mäkikyrö, E.M.S.; Jaakkola, J.J.K. Subtypes of Asthma and Cold Weather-Related Respiratory Symptoms. Int. J. Environ. Res. Public Health 2022, 19, 8790. [Google Scholar] [CrossRef]
- Horvath, G.; Nagy, K.; Tuboly, G.; Nagy, E. Pain and Weather Associations—Action Mechanisms; Personalized Profiling. Brain Res. Bull. 2023, 200, 110696. [Google Scholar] [CrossRef]
- Iannone, L.F.; De Logu, F.; Geppetti, P.; De Cesaris, F. The Role of TRP Ion Channels in Migraine and Headache. Neurosci. Lett. 2022, 768, 136380. [Google Scholar] [CrossRef]
- Horváth, C. Alterations in Brain Temperatures as a Possible Cause of Migraine Headache. Med. Hypotheses 2014, 82, 529–534. [Google Scholar] [CrossRef]
- Gauer, R.; Meyers, B.K. Heat-Related Illnesses. Am. Fam. Physician 2019, 99, 482–489. [Google Scholar]
- Arca, K.N.; Halker Singh, R.B. Dehydration and Headache. Curr. Pain Headache Rep. 2021, 25, 56. [Google Scholar] [CrossRef] [PubMed]
- Misery, L. The Neuro-immuno-cutaneous System and Ultraviolet Radiation. Photodermatol. Photoimmunol. Photomed. 2000, 16, 78–81. [Google Scholar] [CrossRef] [PubMed]
- Upreti, G. Climate Change and Its Threat to Humanity in the Anthropocene. In Ecosociocentrism; Springer Nature: Cham, Switzerland, 2023; pp. 137–162. ISBN 978-3-031-41753-5. [Google Scholar]
- Sidun, N.M.; Gibbons, J.L. Women, Girls, and Climate Change: Human Rights, Vulnerabilities, and Opportunities. Int. J. Psychol. 2024, 59, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Casale, R.; Atzeni, F.; Bazzichi, L.; Beretta, G.; Costantini, E.; Sacerdote, P.; Tassorelli, C. Pain in Women: A Perspective Review on a Relevant Clinical Issue That Deserves Prioritization. Pain Ther. 2021, 10, 287–314. [Google Scholar] [CrossRef]
- Berrang-Ford, L.; Sietsma, A.J.; Callaghan, M.; Minx, J.C.; Scheelbeek, P.F.D.; Haddaway, N.R.; Haines, A.; Dangour, A.D. Systematic Mapping of Global Research on Climate and Health: A Machine Learning Review. Lancet Planet. Health 2021, 5, e514–e525. [Google Scholar] [CrossRef]
- Ebi, K.L.; Semenza, J.C. Community-Based Adaptation to the Health Impacts of Climate Change. Am. J. Prev. Med. 2008, 35, 501–507. [Google Scholar] [CrossRef]
- Woodward, A.; Smith, K.R.; Campbell-Lendrum, D.; Chadee, D.D.; Honda, Y.; Liu, Q.; Olwoch, J.; Revich, B.; Sauerborn, R.; Chafe, Z.; et al. Climate Change and Health: On the Latest IPCC Report. Lancet 2014, 383, 1185–1189. [Google Scholar] [CrossRef]
- Jevotovsky, D.S.; Oehlermarx, W.; Chen, T.; Ortiz, C.C.; Liu, A.; Sahni, S.; Kessler, J.L.; Poli, J.J.; Lau, R. Weathering the Pain: Ambient Temperature’s Role in Chronic Pain Syndromes. Curr. Pain Headache Rep. 2025, 29, 31. [Google Scholar] [CrossRef] [PubMed]
- Zyoud, S. Unveiling the Potential of Biomarkers in the Context of Climate Change: Analysis of Knowledge Landscapes, Trends, and Research Priorities. Reg. Environ. Change 2024, 24, 76. [Google Scholar] [CrossRef]
- Prada, D.; Baccarelli, A.A.; Kupsco, A.; Parks, R.M. Climate Change and Health: Understanding Mechanisms Will Inform Mitigation and Prevention Strategies. Nat. Med. 2024, 30, 1522–1524. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Jiménez, L.; Romero-Martín, M.; Spruell, T.; Steley, Z.; Gómez-Salgado, J. The Carbon Footprint of Healthcare Settings: A Systematic Review. J. Adv. Nurs. 2023, 79, 2830–2844. [Google Scholar] [CrossRef]
- Nelson, A.M.; Kelleher, D.C.; Ip, V.; Narouze, S. Environmental Pain Approach (EPA): Sustainability in Chronic Pain Practice. Pain. Med. 2023, 24, 573–575. [Google Scholar] [CrossRef]
- Habibi, P.; Razmjouei, J.; Moradi, A.; Mahdavi, F.; Fallah-Aliabadi, S.; Heydari, A. Climate Change and Heat Stress Resilient Outdoor Workers: Findings from Systematic Literature Review. BMC Public Health 2024, 24, 1711. [Google Scholar] [CrossRef]
- Venter, Z.S.; Hassani, A.; Stange, E.; Schneider, P.; Castell, N. Reassessing the Role of Urban Green Space in Air Pollution Control. Proc. Natl. Acad. Sci. USA 2024, 121, e2306200121. [Google Scholar] [CrossRef]
| Study | Study Design and Participants | Key Findings |
|---|---|---|
| Patel et al., 2016 [18] | Analysis of data from 5782 respondents aged ≥ 17 years with chronic pain (71% female) |
|
| Dixon et al., 2019 [19] | Multivariate case-crossover analysis of weather variables; included 2658 adults aged ≥ 17 years (83% female; mean [SD] age, 51 [12.6] years) with chronic pain (>3 months; including unspecified arthritis, OA, gout, RA, chronic headache/migraine, neuropathic pain, FM/chronic widespread pain, and other/no medical diagnosis); participants were followed for up to 15 months and scored days as either having no pain events or having pain events |
|
| Schultz et al., 2020 [20] | Analysis of data from 10,584 participants b (81% female; mean [SD] age, 48 [13.2] years [11]) with chronic pain (including unspecified arthritis, OA, gout, RA, chronic headache/migraine, neuropathic pain, FM/chronic widespread pain, and other/no medical diagnosis) examining the association between pain events (days with pain) at the population level and weather patterns (climate and atmospheric conditions) |
|
| Yimer et al., 2022 [21] | Bayesian multilevel model examined association between weather and pain; analysis included 6213 pts (82.4% female; mean [SD] age, 48.7 [13.0] years) with chronic pain conditions (including unspecified arthritis, OA, gout, RA, chronic headache/migraine, neuropathic pain, FM/chronic widespread pain, and other/no medical diagnosis); correlated pain data with objective weather data |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kushner, P.; Kalita, P.; Revel, F.B.; Oliver, C.; Nangineedi, M.; Cardosa, M. Climate Change and Air Pollution-Related Health Effects on Pain. Int. J. Environ. Res. Public Health 2025, 22, 1721. https://doi.org/10.3390/ijerph22111721
Kushner P, Kalita P, Revel FB, Oliver C, Nangineedi M, Cardosa M. Climate Change and Air Pollution-Related Health Effects on Pain. International Journal of Environmental Research and Public Health. 2025; 22(11):1721. https://doi.org/10.3390/ijerph22111721
Chicago/Turabian StyleKushner, Pamela, Pranab Kalita, Frédérique Bariguian Revel, Christie Oliver, Mounika Nangineedi, and Mary Cardosa. 2025. "Climate Change and Air Pollution-Related Health Effects on Pain" International Journal of Environmental Research and Public Health 22, no. 11: 1721. https://doi.org/10.3390/ijerph22111721
APA StyleKushner, P., Kalita, P., Revel, F. B., Oliver, C., Nangineedi, M., & Cardosa, M. (2025). Climate Change and Air Pollution-Related Health Effects on Pain. International Journal of Environmental Research and Public Health, 22(11), 1721. https://doi.org/10.3390/ijerph22111721





