Nursing Students’ Knowledge Among Healthcare-Associated Infections: A Systematic Review
Abstract
1. Introduction
Objective of the Study
2. Materials and Methods
2.1. Study Design
2.2. Search Methods
2.3. Inclusion and Exclusion Criteria
- (a)
- Primary studies;
- (b)
- Original studies;
- (c)
- Literature reviews;
- (d)
- Articles that evaluated nursing students’ understanding of healthcare-associated infections;
- (e)
- Articles in English.
- (a)
- Guidelines;
- (b)
- Dissertations, oral presentations, methodological or theoretical descriptions or individual clinical cases;
- (c)
- Studies that did not evaluate nursing students’ understanding of healthcare-associated infections;
- (d)
- Articles written in languages other than English.
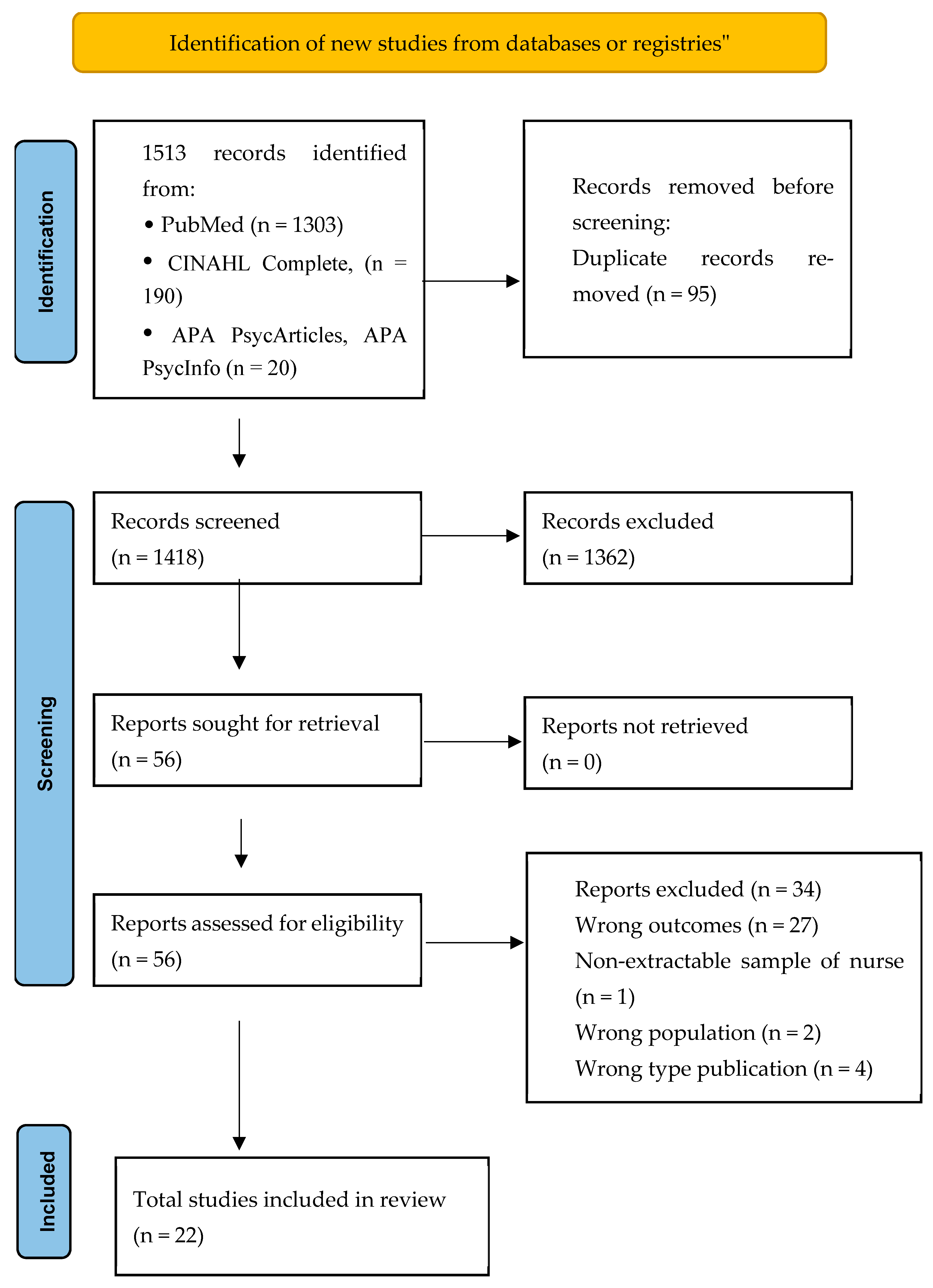
2.4. Search Outcome
2.5. Quality Appraisal
2.6. Data Synthesis
3. Results
Characteristics of the Studies
4. Discussion
4.1. Implications and Recommendations for Further Research
4.2. Strengths and Limitation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HAIs | Healthcare-associated infections |
| WHO | World Health Organization |
| IPC | Prevention and Control Measures |
References
- Khan, H.A.; Baig, F.K.; Mehboob, R. Nosocomial Infections: Epidemiology, Prevention, Control and Surveillance. Asian Pac. J. Trop. Biomed. 2017, 7, 478–482. [Google Scholar] [CrossRef]
- Puro, V.; Coppola, N.; Frasca, A.; Gentile, I.; Luzzaro, F.; Peghetti, A.; Sganga, G. Pillars for Prevention and Control of Healthcare-Associated Infections: An Italian Expert Opinion Statement. Antimicrob. Resist. Infect. Control 2022, 11, 87. [Google Scholar] [CrossRef] [PubMed]
- Allegranzi, B.; Nejad, S.B.; Pittet, D. The Burden of Healthcare–associated Infection. Hand Hyg. Handb. Med. Prof. 2017, 1–7. [Google Scholar]
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M.; et al. Attributable Deaths and Disability-Adjusted Life-Years Caused by Infections with Antibiotic-Resistant Bacteria in the EU and the European Economic Area in 2015: A Population-Level Modelling Analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Pezhman, B.; Fatemeh, R.; Amir, R.; Mahboobeh, R.; Mohammad, F. Nosocomial Infections in an Iranian Educational Hospital: An Evaluation Study of the Iranian Nosocomial Infection Surveillance System. BMC Infect. Dis. 2021, 21, 1256. [Google Scholar] [CrossRef]
- World Health Organization. World Health Organization Report on the Burden of Endemic Health Care-Associated Infection Worldwide. In Report on the Burden of Endemic Health Care-Associated Infection Worldwide; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Gidey, K.; Gidey, M.T.; Hailu, B.Y.; Gebreamlak, Z.B.; Niriayo, Y.L. Clinical and Economic Burden of Healthcare-Associated Infections: A Prospective Cohort Study. PLoS ONE 2023, 18, e0282141. [Google Scholar] [CrossRef]
- Raoofi, S.; Pashazadeh Kan, F.; Rafiei, S.; Hosseinipalangi, Z.; Noorani Mejareh, Z.; Khani, S.; Abdollahi, B.; Seyghalani Talab, F.; Sanaei, M.; Zarabi, F.; et al. Global Prevalence of Nosocomial Infection: A Systematic Review and Meta-Analysis. PLoS ONE 2023, 18, e0274248. [Google Scholar] [CrossRef]
- Suetens, C.; Latour, K.; Kärki, T.; Ricchizzi, E.; Kinross, P.; Moro, M.L.; Jans, B.; Hopkins, S.; Hansen, S.; Lyytikäinen, O.; et al. Prevalence of Healthcare-Associated Infections, Estimated Incidence and Composite Antimicrobial Resistance Index in Acute Care Hospitals and Long-Term Care Facilities: Results from Two European Point Prevalence Surveys, 2016 to 2017. Eurosurveillance 2018, 23, 1800516. [Google Scholar] [CrossRef]
- Ministero della Salute Piano Nazionale Di Contrasto All’Antibiotico-Resistenza (PNCAR) 2022–2025. 2022. Available online: https://www.aifa.gov.it/documents/20142/1807239/PNCAR_2022-2025.pdf (accessed on 20 October 2025).
- Haque, M.; Sartelli, M.; McKimm, J.; Abu Bakar, M.B. Health Care-Associated Infections—An Overview. Infect. Drug Resist. 2018, 11, 2321–2333. [Google Scholar] [CrossRef]
- Ioannou, P.; Astrinaki, E.; Vitsaxaki, E.; Bolikas, E.; Christofaki, D.; Salvaraki, A.; Lagoudaki, E.; Ioannidou, E.; Karakonstantis, S.; Saplamidou, S.; et al. A Point Prevalence Survey of Healthcare-Associated Infections and Antimicrobial Use in Public Acute Care Hospitals in Crete, Greece. Antibiotics 2022, 11, 1258. [Google Scholar] [CrossRef]
- Rafa, E.; Wałaszek, M.Z.; Wałaszek, M.J.; Domański, A.; Różańska, A. The Incidence of Healthcare-Associated Infections, Their Clinical Forms, and Microbiological Agents in Intensive Care Units in Southern Poland in a Multicentre Study from 2016 to 2019. Int. J. Environ. Res. Public. Health 2021, 18, 2238. [Google Scholar] [CrossRef]
- Blot, S.; Ruppé, E.; Harbarth, S.; Asehnoune, K.; Poulakou, G.; Luyt, C.-E.; Rello, J.; Klompas, M.; Depuydt, P.; Eckmann, C.; et al. Healthcare-Associated Infections in Adult Intensive Care Unit Patients: Changes in Epidemiology, Diagnosis, Prevention and Contributions of New Technologies. Intensive Crit. Care Nurs. 2022, 70, 103227. [Google Scholar] [CrossRef] [PubMed]
- Salem, O.A. Knowledge and Practices of Nurses in Infection Prevention and Control within a Tertiary Care Hospital. Ann. Med. Health Sci. Res. 2019, 9, 422–425. [Google Scholar]
- Nofal, M.; Subih, M.; Al-Kalaldeh, M.; Al Hussami, M. Factors Influencing Compliance to the Infection Control Precautions among Nurses and Physicians in Jordan: A Cross-Sectional Study. J. Infect. Prev. 2017, 18, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Russell, D.; Dowding, D.W.; McDonald, M.V.; Adams, V.; Rosati, R.J.; Larson, E.L.; Shang, J. Factors for Compliance with Infection Control Practices in Home Healthcare: Findings from a Survey of Nurses’ Knowledge and Attitudes toward Infection Control. Am. J. Infect. Control 2018, 46, 1211–1217. [Google Scholar] [CrossRef]
- Bajunaid, R.M.; Saeed, A.; Bostaji, M.; Farsi, N.J. Hand Hygiene Compliance and Improvement Interventions in the Eastern Mediterranean Region: A Systematic Review and Meta-Analysis. Infect. Prev. Pract. 2024, 6, 100363. [Google Scholar] [CrossRef]
- Schreiber, P.W.; Sax, H.; Wolfensberger, A.; Clack, L.; Kuster, S.P.; Swissnoso. The Preventable Proportion of Healthcare-Associated Infections 2005–2016: Systematic Review and Meta-Analysis. Infect. Control Hosp. Epidemiol. 2018, 39, 1277–1295. [Google Scholar] [CrossRef]
- World Health Organization. Global Strategy on Infection Prevention and Control; World Health Organization: Geneva, Switzerland, 2024; ISBN 92-4-008051-1. [Google Scholar]
- Parreira, P.; Santos-Costa, P.; Pardal, J.; Neves, T.; Bernardes, R.A.; Serambeque, B.; Sousa, L.B.; Graveto, J.; Silén-Lipponen, M.; Korhonen, U.; et al. Nursing Students’ Perceptions on Healthcare-Associated Infection Control and Prevention Teaching and Learning Experience in Portugal. J. Pers. Med. 2022, 12, 180. [Google Scholar] [CrossRef]
- Labrague, L.J.; McEnroe–Petitte, D.M.; Van De Mortel, T.; Nasirudeen, A.M.A. A Systematic Review on Hand Hygiene Knowledge and Compliance in Student Nurses. Int. Nurs. Rev. 2018, 65, 336–348. [Google Scholar] [CrossRef]
- Salminen, L.; Stolt, M.; Saarikoski, M.; Suikkala, A.; Vaartio, H.; Leino-Kilpi, H. Future Challenges for Nursing Education—A European Perspective. Nurse Educ. Today 2010, 30, 233–238. [Google Scholar] [CrossRef]
- Taneva, D.; Paskaleva, D.; Gyurova-Kancheva, V. Nursing Education in Some European Higher Education Area (EHEA) Member Countries: A Comparative Analysis. Iran. J. Public Health 2023, 52, 1418–1427. [Google Scholar] [CrossRef]
- Ojo, O.O.; Ojo, O. Assessing Students’ Knowledge of Healthcare-Associated Infections: A Global Perspective. Br. J. Nurs. 2017, 26, 1121–1126. [Google Scholar] [CrossRef]
- da Silva, M.S.G.O.; Ferreira, M.M.S.V.; Feijo, N.M. Knowledge of Nursing Students on Infection Prevention and Control Measures: Scoping Review Protocol. Online Braz. J. Nurs. 2023, 22, e20236606. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Joanna Briggs Institute. The Joanna Briggs Institute Critical Appraisal Tools for Use in JBI Systematic Reviews. Crit. Apprais. Checkl. Anal. Cross Sect. Stud. 2017, 1, 1–7. [Google Scholar]
- NIH, N. Study Quality Assessment Tools; National Heart, Lung, and Blood Institute (NHLBI): Bethesda, MD, USA, 2021. [Google Scholar]
- D’Alessandro, D.; Agodi, A.; Auxilia, F.; Brusaferro, S.; Calligaris, L.; Ferrante, M.; Montagna, M.T.; Mura, I.; Napoli, C.; Pasquarella, C.; et al. Prevention of Healthcare Associated Infections: Medical and Nursing Students’ Knowledge in Italy. Nurse Educ. Today 2014, 34, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Majidipour, P.; Aryan, A.; Janatolmakan, M.; Khatony, A. Knowledge and Performance of Nursing Students of Kermanshah-Iran Regarding the Standards of Nosocomial Infections Control: A Cross-Sectional Study. BMC Res. Notes 2019, 12, 485. [Google Scholar] [CrossRef]
- Tavolacci, M.-P.; Ladner, J.; Bailly, L.; Merle, V.; Pitrou, I.; Czernichow, P. Prevention of Nosocomial Infection and Standard Precautions: Knowledge and Source of Information Among Healthcare Students. Infect. Control Hosp. Epidemiol. 2008, 29, 642–647. [Google Scholar] [CrossRef]
- Mohammedi, S.B.; Gillois, P.; Landelle, C. Nursing Students’knowledge and Effectiveness of Teaching in Infection Prevention and Control. BMC Nurs. 2025, 24, 850. [Google Scholar] [CrossRef]
- Alriyami, M.; Al Omari, O.; Al-Daken, L.; Alriyami, T.; Al Rashdi, R.; Al Shukaili, S.; Al-Alawi, T.; Al Qadire, M. Assessing Knowledge of Nosocomial Infection among Omani Student Nurses: A Cross-Sectional Study. Br. J. Nurs. 2022, 31, 66–70. [Google Scholar] [CrossRef]
- Brosio, F.; Kuhdari, P.; Stefanati, A.; Guidi, E.; Lupi, S.; Sulcaj, N.; Bergamini, M.; Gabutti, G. Knowledge and behaviour of nursing students on the prevention of healthcare associated infections. J. Prev. Med. Hyg. 2017, 58, E99–E104. [Google Scholar] [CrossRef]
- Mazhar, L.; Safdar, A.; Nisa, W.T.; Nadeem, F.; Zahid, J.; Shakir, A.; Muzammil, M. Exploring the Knowledge and Practices of Standard Infection Control Precautions among BSc Nursing Students. Crit. Rev. Soc. Sci. Stud. 2025, 3, 2360–2369. [Google Scholar] [CrossRef]
- Syed, W.; Al-Rawi, M.B.A. Assessment of Hand-Washing Knowledge and Practice among Nursing Undergraduates in Saudi Arabia. Can. J. Infect. Dis. Med. Microbiol. 2024, 2024, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, S.; Cho, Y.; Bhuju, C.; Cha, K.; Chung, M.; Pun, K. Knowledge, Perception and Confidence in Performance on Infection Prevention and Control Measures among the Nursing Students. Kathmandu Univ. Med. J. 2023, 84, 383–388. [Google Scholar]
- Sharma, M.; Bachani, R. Knowledge, Attitude, Practice, and Perceived Barriers for the Compliance of Standard Precautions among Medical and Nursing Students in Central India. Int. J. Environ. Res. Public Health 2023, 20, 5487. [Google Scholar] [CrossRef]
- Thakker, V.; Jadhav, P. Knowledge of Hand Hygiene in Undergraduate Medical, Dental, and Nursing Students: A Cross-Sectional Survey. J. Fam. Med. Prim. Care 2015, 4, 582. [Google Scholar] [CrossRef]
- AL-Rawajfah, O.M.; Tubaishat, A. Nursing Students’ Knowledge and Practices of Standard Precautions: A Jordanian Web-Based Survey. Nurse Educ. Today 2015, 35, 1175–1180. [Google Scholar] [CrossRef]
- Ojulong, J.; Mitonga, K.; Iipinge, S. Knowledge and Attitudes of Infection Prevention and Control among Health Sciences Students at University of Namibia. Afr. Health Sci. 2014, 13, 1071. [Google Scholar] [CrossRef]
- Blomgren, P.; Hultin, L.; Westerbergh, J.; Hjelm, K. Attitudes and Perceptions Toward Hand Hygiene Among Nursing Students and Nurses: A Cross–Sectional Comparative Survey. J. Adv. Nurs. 2025. [Google Scholar] [CrossRef]
- Khubrani, A.; Albesher, M.; Alkahtani, A.; Alamri, F.; Alshamrani, M.; Masuadi, E. Knowledge and Information Sources on Standard Precautions and Infection Control of Health Sciences Students at King Saud Bin Abdulaziz University for Health Sciences, Saudi Arabia, Riyadh. J. Infect. Public Health 2018, 11, 546–549. [Google Scholar] [CrossRef]
- Bello, A.; Emannuel, B.O.; Adegoke, B.; Bello, A. Nosocomial Infections: Knowledge and Source of Information among Clinical Health Care Students in Ghana. Int. J. Gen. Med. 2011, 4, 571–574. [Google Scholar] [CrossRef]
- Mitchell, B.G.; Say, R.; Wells, A.; Wilson, F.; Cloete, L.; Matheson, L. Australian Graduating Nurses’ Knowledge, Intentions and Beliefs on Infection Prevention and Control: A Cross-Sectional Study. BMC Nurs. 2014, 13, 43. [Google Scholar] [CrossRef]
- Gould, D.; Drey, N. Student Nurses’ Experiences of Infection Prevention and Control during Clinical Placements. Am. J. Infect. Control 2013, 41, 760–763. [Google Scholar] [CrossRef] [PubMed]
- Colosi, A.; Ergasti, G.; Murzilli, G.; Paolini, V.; Semeraro, V.; Trapani, M.; D’Alessandro, D. Healthcare Students and Their Knowledge of Healthcare Infections. Ann Ig 2011, 23, 1–6. [Google Scholar]
- Darawad, M.W.; Al-Hussami, M. Jordanian Nursing Students’ Knowledge of, Attitudes towards, and Compliance with Infection Control Precautions. Nurse Educ. Today 2013, 33, 580–583. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Gardner, G.E.; Chang, A.M. Taiwanese Nursing Students’ Knowledge, Application and Confidence with Standard and Additional Precautions in Infection Control. J. Clin. Nurs. 2009, 18, 1105–1112. [Google Scholar] [CrossRef]
- Rahiman, F.; Chikte, U.; Hughes, G.D. Nursing Students’ Knowledge, Attitude and Practices of Infection Prevention and Control Guidelines at a Tertiary Institution in the Western Cape: A Cross Sectional Study. Nurse Educ. Today 2018, 69, 20–25. [Google Scholar] [CrossRef]
- Yurrebaso Macho, A.; Ward Mayens, A.L.; Picado Valverde, E.M.; Guzmán Ordaz, R.; Juanes Méndez, J.A.; Pérez Iglesias, J.L.; Mirón Canelo, J.A.; Pinto, M.D.R.; Costa Reis, A.M.D.S.; Simões, J.A.; et al. Nursing Students’ Perceptions on Healthcare-Associated Infection Control and Prevention Teaching and Learning Experience: Development and Validation of a Scale in Four European Countries. Front. Psychol. 2021, 12, 701208. [Google Scholar] [CrossRef]
- Cabezas, C. Tuberculosis En Personal y Estudiantes de Salud: Un Tema Pendiente Para Los Servicios de Salud y La Universidad. Rev. Peru. Med. Exp. Salud Pública 2012, 29, 179–180. [Google Scholar] [CrossRef]
- Tapias-Vargas, L.F.; Torres, S.A.; Tapias-Vargas, L.; Santamaría, C.M.; Valencia-Ángel, L.I.; Orozco-Vargas, L.C. Accidentes Biológicos En Médicos Residentes de Bucaramanga, Colombia. Rev. Colomb. Cir. 2010, 25, 290–299. [Google Scholar]
- Gammon, J.; Hunt, J.; Duffy, L.; Humphreys, I.; Hinkin, J.; Watkins, A. Impact of an Educational Intervention on Hand Hygiene Practice among Nursing Students, with a Focus on Hand Drying Efficacy. J. Infect. Prev. 2024, 25, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Colet, P.C.; Cruz, J.P.; Alotaibi, K.A.; Colet, M.K.A.; Islam, S.M.S. Compliance with Standard Precautions among Baccalaureate Nursing Students in a Saudi University: A Self-Report Study. J. Infect. Public Health 2017, 10, 421–430. [Google Scholar] [CrossRef] [PubMed]
- Loftus, S. Embodied Knowledge and Thinking in Professional Education. In Embodiment and Professional Education: Body, Practice, Pedagogy; Springer: Berlin/Heidelberg, Germany, 2022; pp. 43–54. [Google Scholar]
- Ewertsson, M.; Bagga-Gupta, S.; Allvin, R.; Blomberg, K. Tensions in Learning Professional Identities–Nursing Students’ Narratives and Participation in Practical Skills during Their Clinical Practice: An Ethnographic Study. BMC Nurs. 2017, 16, 48. [Google Scholar] [CrossRef] [PubMed]
- Manan, A.; Kaukab, S.R.; Ahmed, A.; Najeebullah. Knowledge, Attitude and Practices of Undergraduate Nursing Students Regarding Surgical Site Infections. Soc. Sci. Rev. Arch. 2024, 2, 1491–1500. [Google Scholar] [CrossRef]
- Aloush, S.M. Nursing Students’ Knowledge about Ventilator-Associated Pneumonia Prevention Guidelines: Effectiveness of a Teaching Program. Am. J. Infect. Control 2017, 45, 544–546. [Google Scholar] [CrossRef]
- Manning, J. Communication Studies about Sex: Implications for Relationships, Health, Culture, and Identity. A Review. El Prof. Inf. 2021, 30, e300114. [Google Scholar] [CrossRef]
- Erasmus, V.; Daha, T.J.; Brug, H.; Richardus, J.H.; Behrendt, M.D.; Vos, M.C.; Van Beeck, E.F. Systematic Review of Studies on Compliance with Hand Hygiene Guidelines in Hospital Care. Infect. Control Hosp. Epidemiol. 2010, 31, 283–294. [Google Scholar] [CrossRef]
- Carter, E.J.; Mancino, D.; Hessels, A.J.; Kelly, A.M.; Larson, E.L. Reported Hours of Infection Education Received Positively Associated with Student Nurses’ Ability to Comply with Infection Prevention Practices: Results from a Nationwide Survey. Nurse Educ. Today 2017, 53, 19–25. [Google Scholar] [CrossRef]
- Bergamini, M.; Cucchi, A.; Stefanati, A.; Cavallaro, A.; Gabutti, G. Knowledge of Preventive Measures against Occupational Risks and Spread of Healthcare-Associated Infections among Nursing Students. An Epidemiological Prevalence Study from Ferrara, Italy. J. Prev. Med. Hyg. 2009, 50, 96–101. [Google Scholar]
- Olowookere, E.I.; Omonijo, D.O.; Odukoya, J.A.; Anyaegbunam, M.C. Exploring the Effect of Gender and Personality Characteristics on Educational Performance. J. Educ. Soc. Res. 2020, 10, 99. [Google Scholar] [CrossRef]
- Parajuli, M.; Thapa, A. Gender Differences in the Academic Performance of Students. J. Dev. Soc. Eng. 2017, 3, 39–47. [Google Scholar] [CrossRef]
- Jamaluddin, I.Z.; Ahmad, A. Knowledge and Practice Towards Cleaning Medical Equipment among Nursing Students in a Malaysian Public University. Int. J. Care Sch. 2024, 7, 51–57. [Google Scholar] [CrossRef]
- Valičević, G.; Friganović, A.; Kurtović, B.; Rotim, C.; Ledinski Fičko, S.; Krupa, S. Knowledge of Sepsis in Nursing Students—A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 12443. [Google Scholar] [CrossRef] [PubMed]
- Abdul Wahab, P.; Mohd Adie, F.A. Knowledge and Compliance of Standard Precautions Among The Undergraduate Nursing Students. Int. J. Care Sch. 2021, 4, 15–21. [Google Scholar] [CrossRef]
- Shukhali, K.A.; Sultan, A.; Iqbal, J.; Bibi, A.; Farooq, U.; Thapur, D.M.B.; Khalid, A.Y.; Ali, N.; Munir, D.W.; Yousef, A.; et al. Association of infection control knowledge with demographic variables among nursing students at private institute in karachi. J. Popul. Ther. Clin. Pharmacol. 2023, 30, 2145–2152. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, R.; Zhou, Z.; Hong, M.; Huang, Z.; Wen, H.; Peng, L. Comparison of the Conceive-Design-Implement-Operate Model and Lecture-Based Learning in Teaching the “Healthcare-Associated Infections” Course. Front. Med. 2025, 12, 1505588. [Google Scholar] [CrossRef]
- Mikkelsen, J.; Reime, M.H.; Harris, A.K. Nursing Students’ Learning of Managing Cross-Infections—Scenario-Based Simulation Training versus Study Groups. Nurse Educ. Today 2008, 28, 664–671. [Google Scholar] [CrossRef]
- Nget, M.; Neth, B.; Sokchhay, Y.; Vouch, P.; Kry, C.; Soksombat, T.; Gnan, C.; Thida, D.; Koponen, L.; Silén-Lipponen, M.; et al. Nursing Students’ Learning Experience with Healthcare-Associated Infection Prevention and Control (HAI-PC) in Asian Countries: An Exploratory Qualitative Study. J. Investig. Med. 2024, 5, 57–71. [Google Scholar] [CrossRef]
- Reime, M.H.; Harris, A.; Aksnes, J.; Mikkelsen, J. The Most Successful Method in Teaching Nursing Students Infection Control—E-Learning or Lecture? Nurse Educ. Today 2008, 28, 798–806. [Google Scholar] [CrossRef]
- Santos-Costa, P.; Paiva-Santos, F.; Graveto, J.; PrevInf Group. Nursing Students’ Perceptions of a Novel Education Approach to Prevention and Control of Healthcare-Associated Infections: Insights from PrevInf Pilot Study. Nurs. Rep. 2024, 14, 1494–1503. [Google Scholar] [CrossRef]
- Chang, S.O.; Sohng, K.-Y.; Kim, K.; Won, J.; Choi, M.-J.; Chaung, S.-K. Exploring How to Conduct Infection Prevention and Control Education in Undergraduate Nursing Programs in Korea: Focus Group Interview Analysis. J. Korean Acad. Fundam. Nurs. 2019, 26, 210–220. [Google Scholar] [CrossRef]
| P | Nursing students |
| E | Healthcare-associated infections (HAIs) |
| O | Knowledge of HAIs |
| Database | Search String |
|---|---|
| PubMed | (“students, nursing” [MeSH Terms] OR (“students” [All Fields] AND “nursing” [All Fields]) OR “nursing students” [All Fields] OR (“nursing” [All Fields] AND “student” [All Fields]) OR “nursing student” [All Fields] OR ((“undergraduate” [All Fields] OR “undergraduate s” [All Fields] OR “undergraduated” [All Fields] OR “undergraduates” [All Fields]) AND (“student s” [All Fields] OR “students” [MeSH Terms] OR “students” [All Fields] OR “student” [All Fields] OR “students s” [All Fields]) AND “nurs *” [All Fields])) AND (((“cross” [All Fields] OR “crosse” [All Fields] OR “crossed” [All Fields] OR “crosses” [All Fields] OR “crossing” [All Fields] OR “crossings” [All Fields]) AND “infect *” [All Fields]) OR (“cross infection” [MeSH Terms] OR (“cross” [All Fields] AND “infection” [All Fields]) OR “cross infection” [All Fields] OR (“healthcare” [All Fields] AND “associated” [All Fields] AND “infection” [All Fields]) OR “healthcare associated infection” [All Fields]) OR ((“hospital s” [All Fields] OR “hospitalisation” [All Fields] OR “hospitalization” [MeSH Terms] OR “hospitalization” [All Fields] OR “hospitalised” [All Fields] OR “hospitalising” [All Fields] OR “hospitality” [All Fields] OR “hospitalisations” [All Fields] OR “hospitalizations” [All Fields] OR “hospitalize” [All Fields] OR “hospitalized” [All Fields] OR “hospitalizing” [All Fields] OR “hospitals” [MeSH Terms] OR “hospitals” [All Fields] OR “hospital” [All Fields]) AND “infect *” [All Fields]) OR ((“nosocomial” [All Fields] OR “nosocomially” [All Fields] OR “nosocomials” [All Fields]) AND “infect *” [All Fields])) AND (“knowledge” [MeSH Terms] OR “knowledge” [All Fields] OR “knowledge s” [All Fields] OR “knowledgeability” [All Fields] OR “knowledgeable” [All Fields] OR “knowledgeably” [All Fields] OR “knowledges” [All Fields] OR (“awareness” [MeSH Terms] OR “awareness” [All Fields] OR “aware” [All Fields] OR “awarenesses” [All Fields]) OR (“compete” [All Fields] OR “competed” [All Fields] OR “competences” [All Fields] OR “competencies” [All Fields] OR “competently” [All Fields] OR “competents” [All Fields] OR “competes” [All Fields] OR “competing” [All Fields] OR “mental competency” [MeSH Terms] OR (“mental” [All Fields] AND “competency” [All Fields]) OR “mental competency” [All Fields] OR “competence” [All Fields] OR “competency” [All Fields] OR “competent” [All Fields]) OR “attitude *” [All Fields] OR “perception *” [All Fields] OR “practice *” [All Fields]) |
| Database | Search String |
|---|---|
| CINAHL | (Nursing students or student nurses or undergraduate student nurses or pre-licensure nurse) AND (cross infection or hospital acquired infections or healthcare associated infections) AND (knowledge or education or understanding or awareness or competence OR attitude or perception * or practice *) |
| Database | Search String |
|---|---|
| APA PsycArticles APA PsycInfo | (Nursing students or student nurses or undergraduate student nurses or pre-licensure nurse) AND (cross infection or hospital acquired infections or healthcare associated infections) AND (knowledge or education or understanding or awareness or competence OR attitude or perception * or practice *) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giordano, V.; Palazzo, C.; Mercuri, C.; Verde, V.; Rea, T.; Doldo, P.; Guillari, A. Nursing Students’ Knowledge Among Healthcare-Associated Infections: A Systematic Review. Int. J. Environ. Res. Public Health 2025, 22, 1609. https://doi.org/10.3390/ijerph22111609
Giordano V, Palazzo C, Mercuri C, Verde V, Rea T, Doldo P, Guillari A. Nursing Students’ Knowledge Among Healthcare-Associated Infections: A Systematic Review. International Journal of Environmental Research and Public Health. 2025; 22(11):1609. https://doi.org/10.3390/ijerph22111609
Chicago/Turabian StyleGiordano, Vincenza, Chiara Palazzo, Caterina Mercuri, Vittoria Verde, Teresa Rea, Patrizia Doldo, and Assunta Guillari. 2025. "Nursing Students’ Knowledge Among Healthcare-Associated Infections: A Systematic Review" International Journal of Environmental Research and Public Health 22, no. 11: 1609. https://doi.org/10.3390/ijerph22111609
APA StyleGiordano, V., Palazzo, C., Mercuri, C., Verde, V., Rea, T., Doldo, P., & Guillari, A. (2025). Nursing Students’ Knowledge Among Healthcare-Associated Infections: A Systematic Review. International Journal of Environmental Research and Public Health, 22(11), 1609. https://doi.org/10.3390/ijerph22111609






