Benefits of an Innovative 90-Day Longevity Workplace Program on Health in the United Arab Emirates (UAE)
Abstract
1. Introduction
2. Materials and Methods
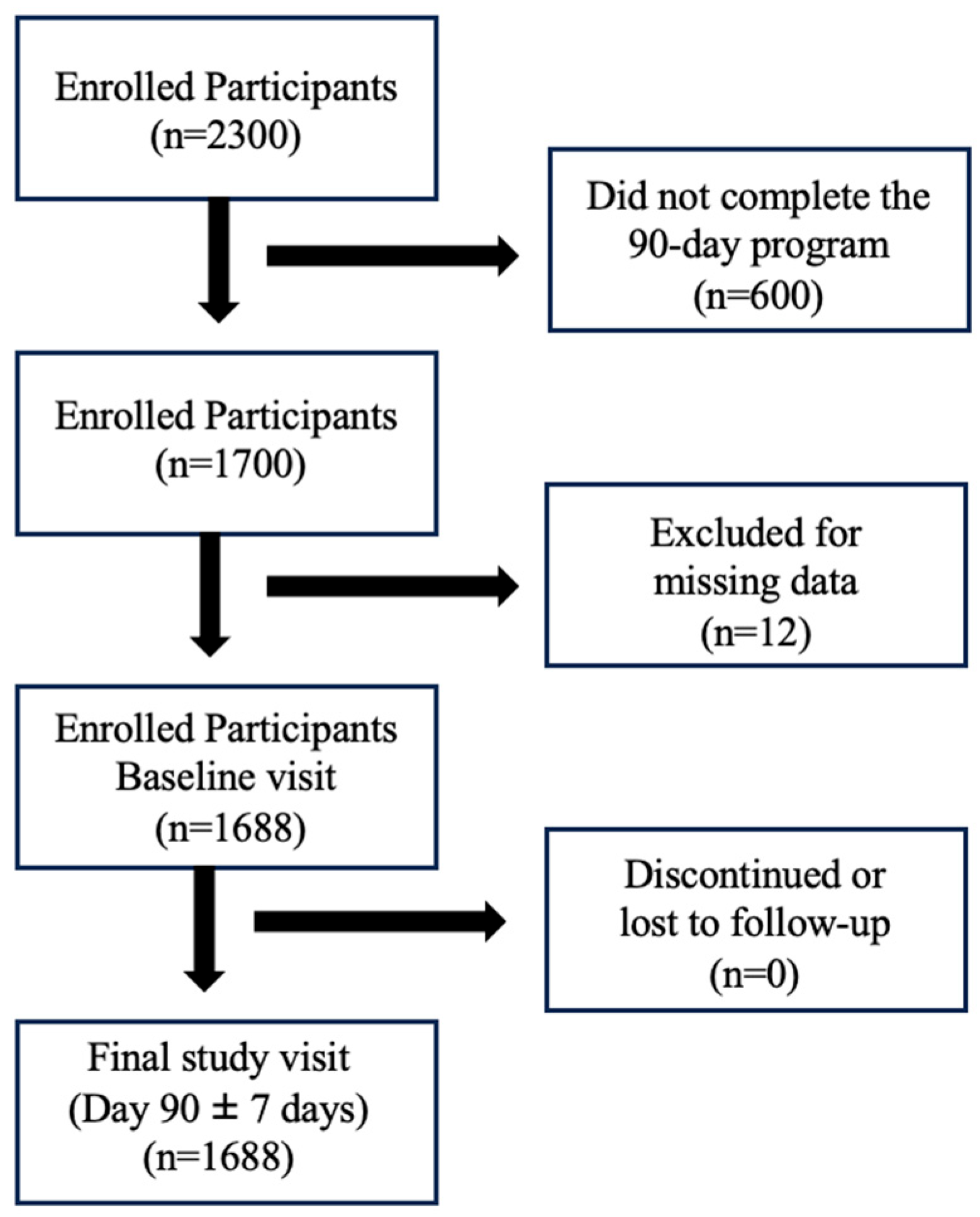
2.1. Study Design and Participants
2.2. Study Outcomes
2.3. Statistical Analysis
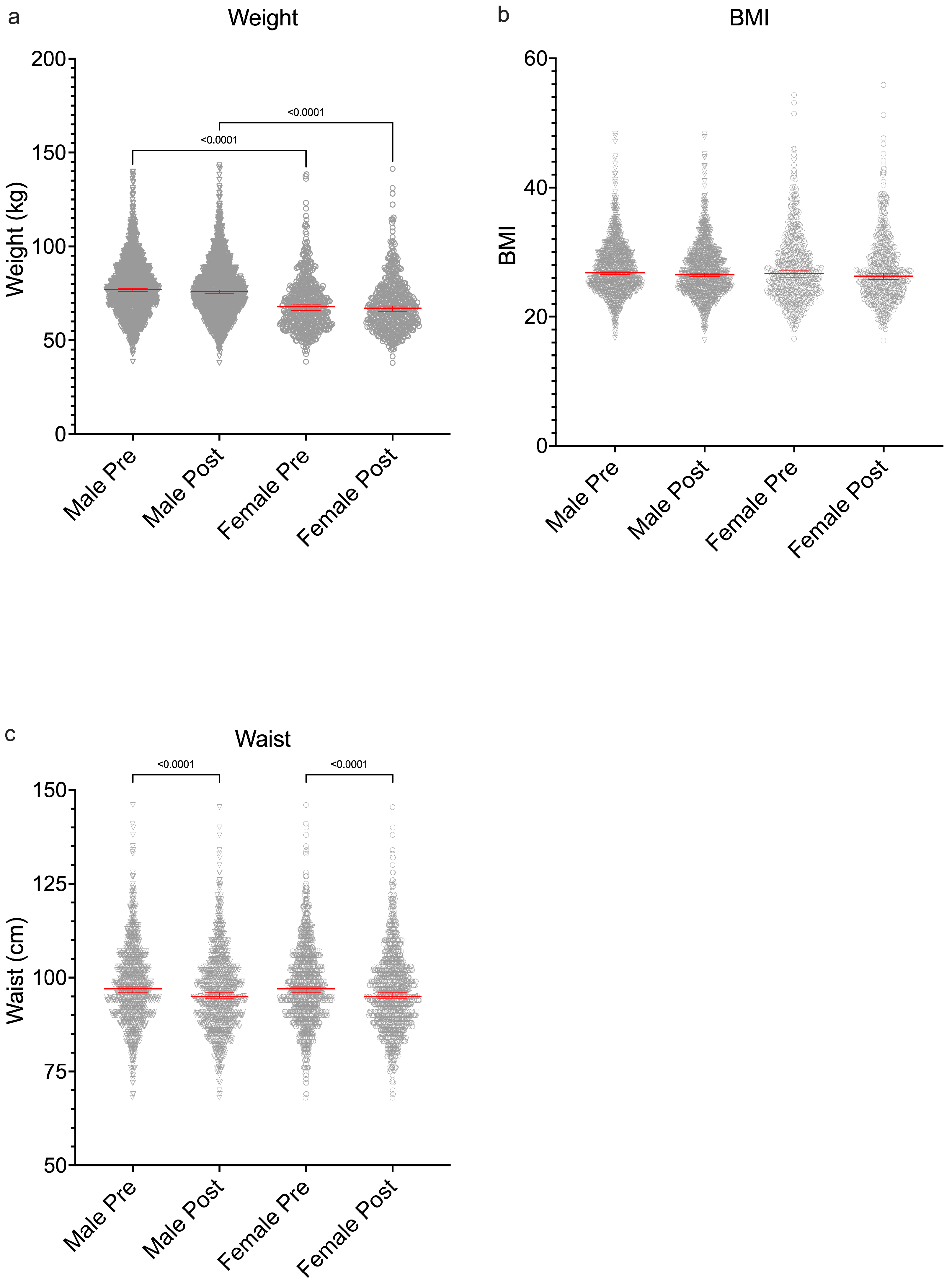
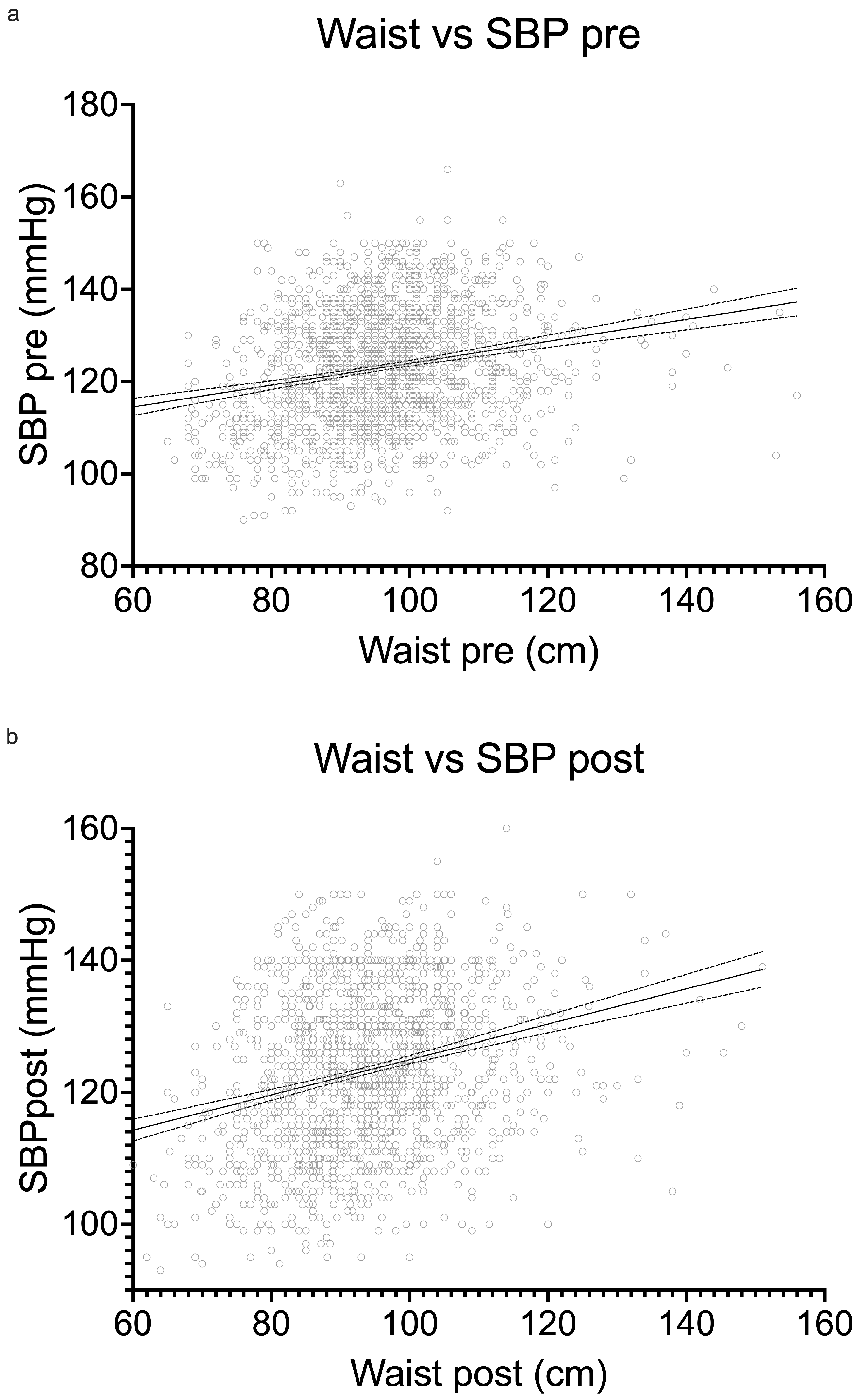
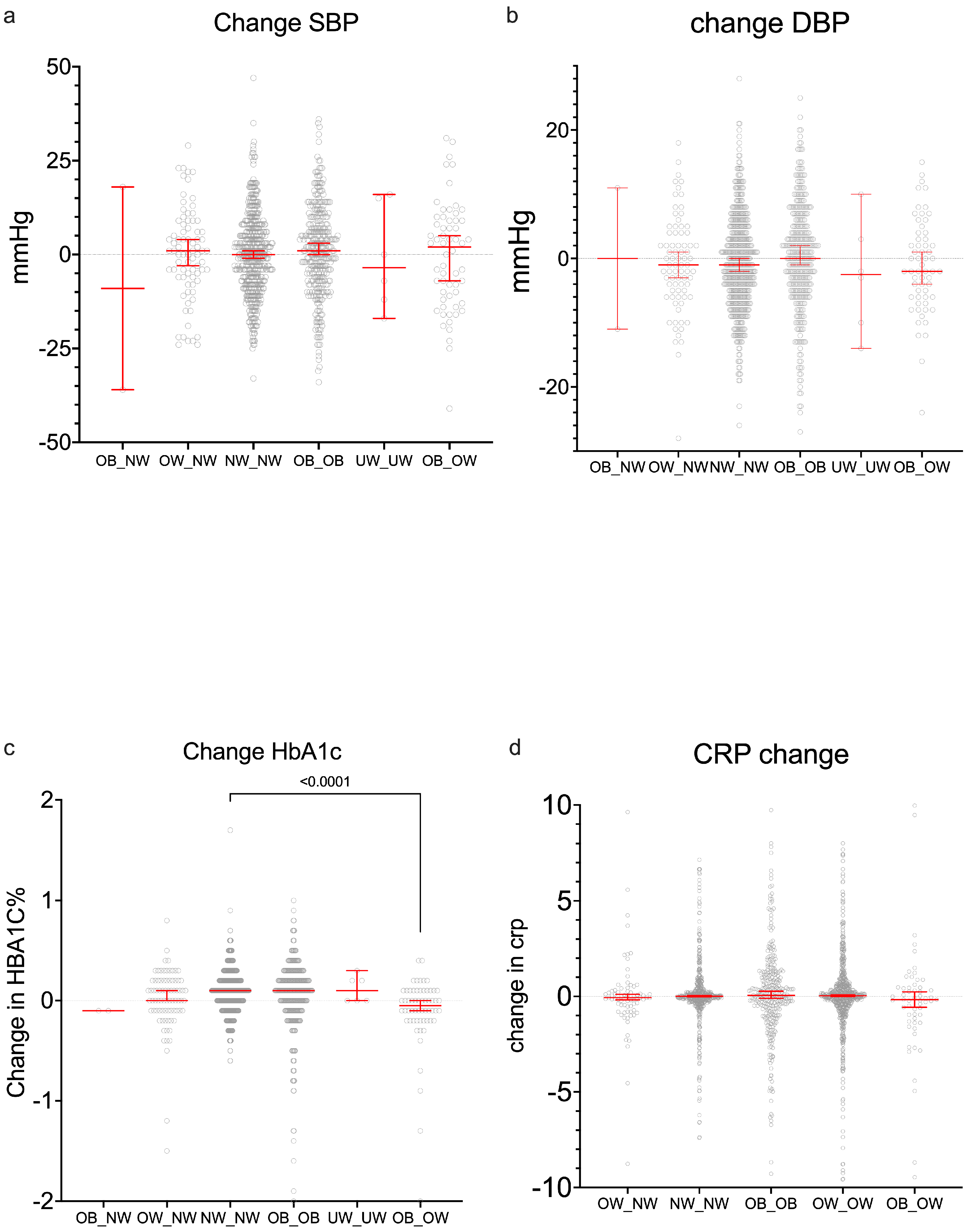
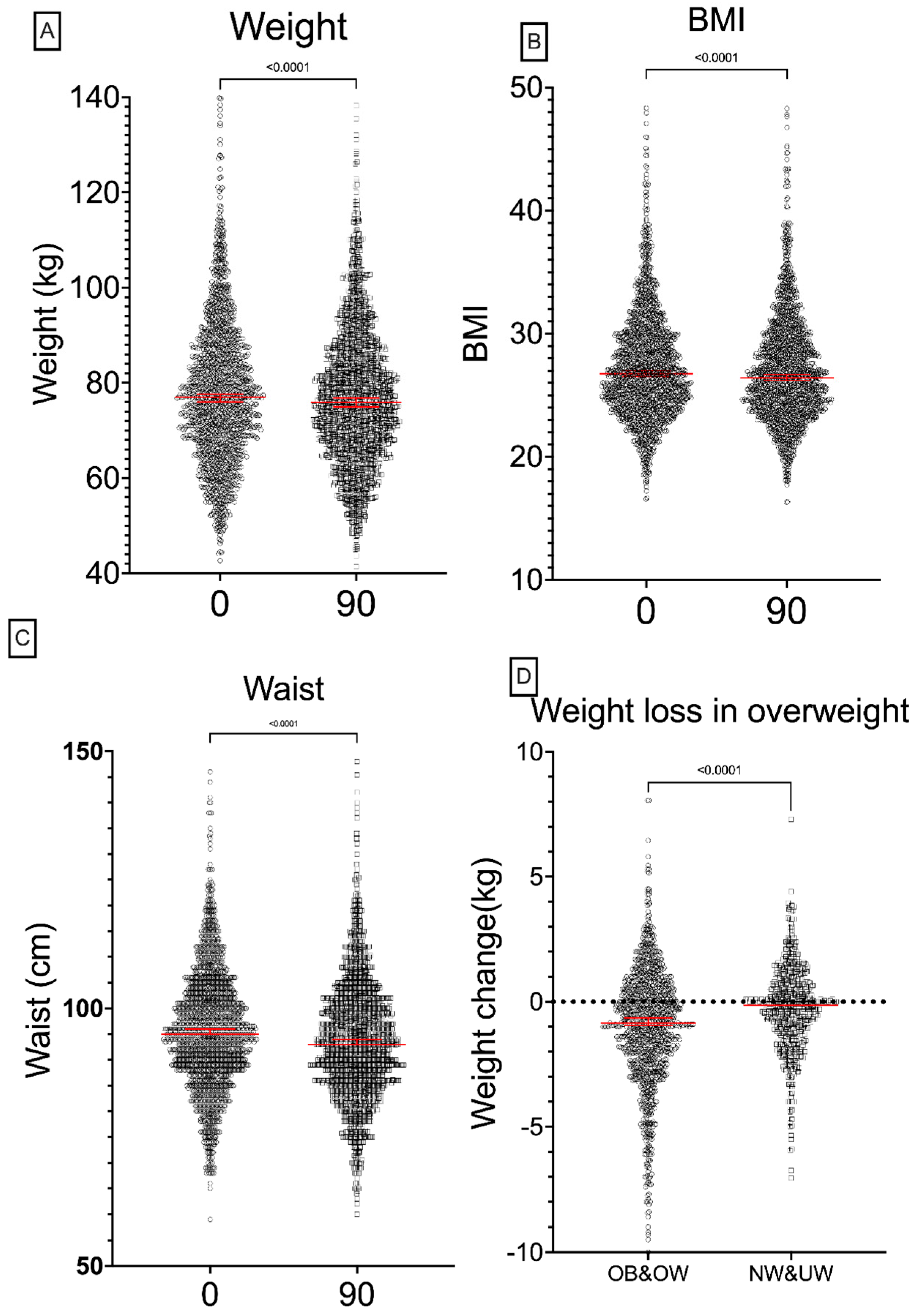
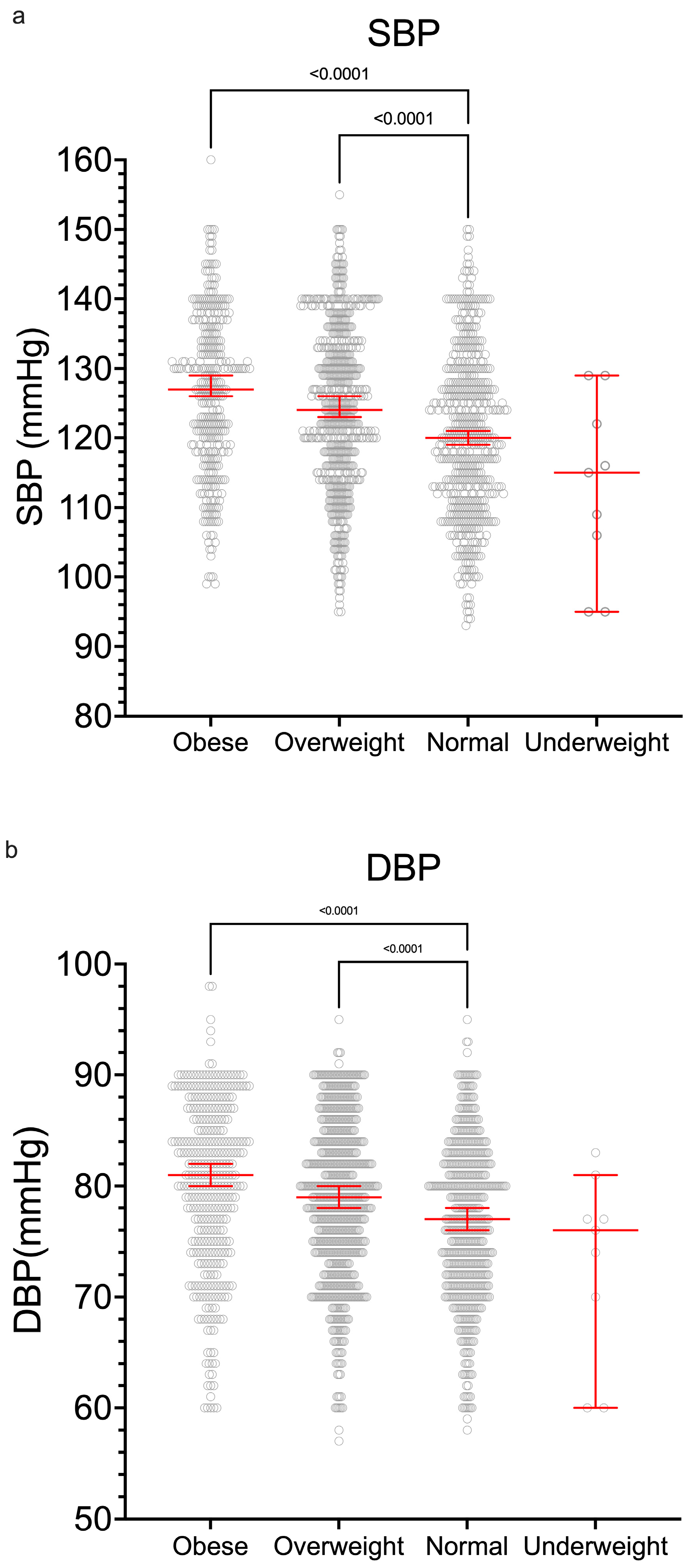
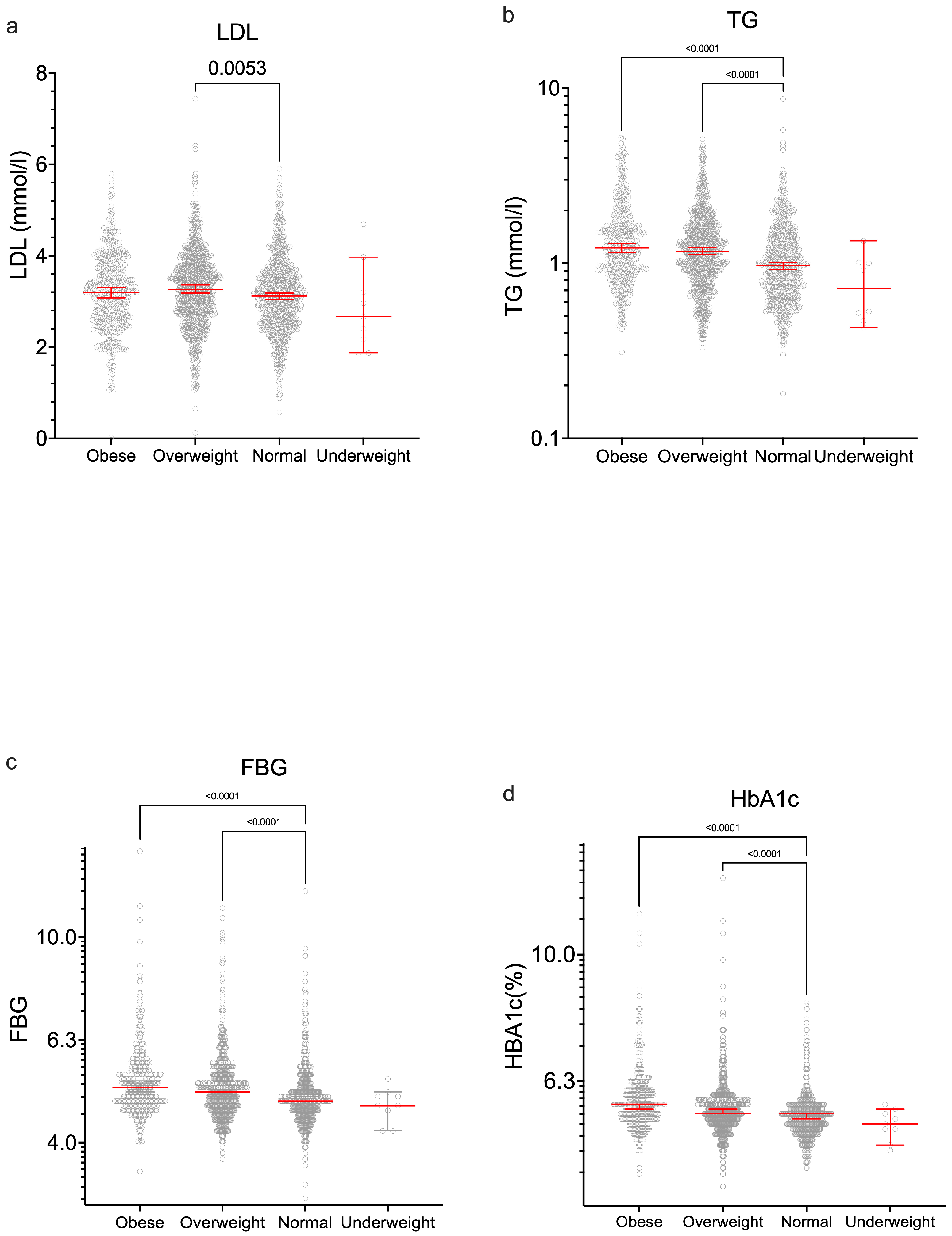
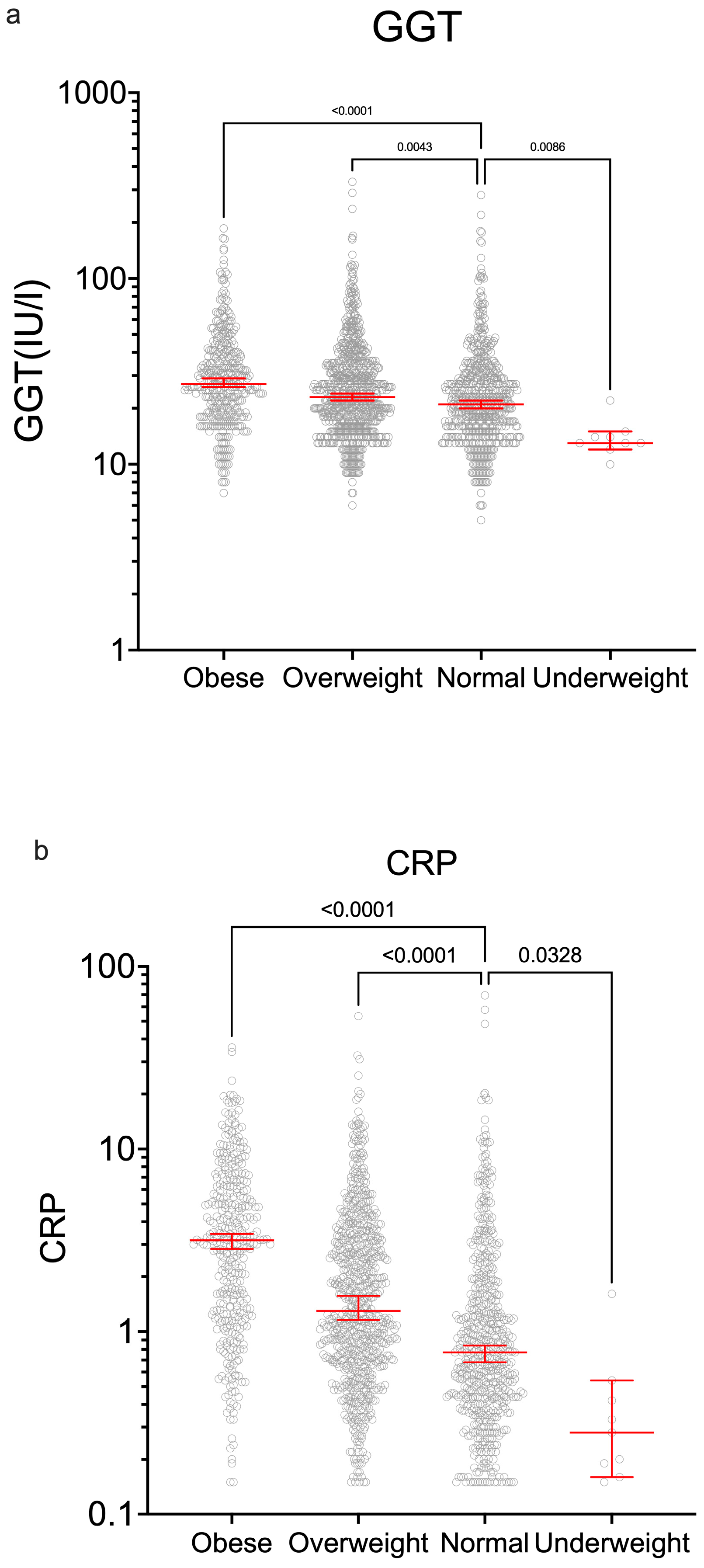
3. Results
Baseline Characteristics of Study Participants
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| CRP | C-reactive protein |
| DO | Dropout group |
| FBG | Fasting blood glucose |
| FC | Full cohort |
| GGT | Gamma-glutamyl transferase |
| HBA1c | Glycosylated hemoglobin |
| LDL | LDL cholesterol |
| NW | Normal weight |
| OB | Obese |
| OW | Overweight |
| PHLS | Pure Health 2K Longevity Study |
| UAE | United Arab Emirates |
| UW | Underweight |
Appendix A
| Nationality | Full | Complete | Dropout | Full % | Complete % | Dropout % |
|---|---|---|---|---|---|---|
| Indian | 839 | 676 | 163 | 36.5 | 40.0 | 9.7 |
| Emirati | 342 | 149.0 | 193 | 14.9 | 8.8 | 11.4 |
| Pakistani | 338 | 279 | 59 | 14.7 | 16.5 | 3.5 |
| Filipino | 191 | 162.0 | 29 | 8.3 | 9.6 | 1.7 |
| Egyptian | 99 | 72.0 | 27 | 4.3 | 4.3 | 1.6 |
| Jordanian | 91 | 62 | 29 | 4.0 | 3.7 | 1.7 |
| Sudanese | 76 | 59 | 17 | 3.3 | 3.5 | 1.0 |
| British | 37 | 25.0 | 12 | 1.6 | 1.5 | 0.7 |
| Syrian | 34 | 24 | 10 | 1.5 | 1.4 | 0.6 |
| Other | 253 | 180 | 73 | 11.0 | 10.7 | 11.9 |
References
- The WHO cross-national study of health behavior in school-aged children from 35 countries: Findings from 2001–2002. J. Sch. Health 2004, 74, 204–206. [CrossRef]
- Farhud, D.D. Impact of Lifestyle on Health. Iran. J. Public Health 2015, 44, 1442–1444. Available online: http://www.ncbi.nlm.nih.gov/pubmed/26744700 (accessed on 15 May 2025). [PubMed]
- Mattke, S.; Liu, H.; Caloyeras, J.; Huang, C.Y.; Van Busum, K.R.; Khodyakov, D.; Shier, V. Workplace Wellness Programs Study: Final Report. Rand Health Q. 2013, 3, 7. Available online: http://www.ncbi.nlm.nih.gov/pubmed/4945172 (accessed on 15 May 2025). [PubMed]
- World Health Organization. Healthy Diet—Fact Sheet. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/healthy-diet (accessed on 12 October 2024).
- World Health Organization. Physical Activity—Fact Sheet. 2024. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 12 October 2024).
- World Health Organization. Noncommunicable Diseases: Factsheet. 2024. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 2 August 2025).
- Rojanasarot, S.; Bhattacharyya, S.K.; Edwards, N. Productivity loss and productivity loss costs to United States employers due to priority conditions: A systematic review. J. Med. Econ. 2023, 26, 262–270. [Google Scholar] [CrossRef]
- Virtanen, M.; Lallukka, T.; Elovainio, M.; Steptoe, A.; Kivimäki, M. Effectiveness of workplace interventions for health promotion. Lancet Public Health 2025, 10, e512–e530. [Google Scholar] [CrossRef] [PubMed]
- Rachmah, Q.; Martiana, T.; Mulyono, M.; Paskarini, I.; Dwiyanti, E.; Widajati, N.; Ernawati, M.; Ardyanto, Y.D.; Tualeka, A.R.; Haqi, D.N.; et al. The Effectiveness of Nutrition and Health Intervention in Workplace Setting: A Systematic Review. J. Public Health Res. 2022, 11, 2312. [Google Scholar] [CrossRef] [PubMed]
- Baicker, K.; Cutler, D.; Song, Z. Workplace Wellness Programs Can Generate Savings. Health Aff. 2010, 29, 304–311. [Google Scholar] [CrossRef]
- Mohammad, A.; Silva Paulo, M.; Al Hosani, S.; Al Jabri, O.; Al Yafei, Z.; Datta, S.; Koornneef, E. Health and Wellness Characteristics of Employees Enrolled in a Workplace Wellness Study in the United Arab Emirates: A Descriptive Analysis of a Pilot Study. Cureus 2024, 16, e62294. [Google Scholar] [CrossRef]
- Magkos, F.; Fraterrigo, G.; Yoshino, J.; Luecking, C.; Kirbach, K.; Kelly, S.C.; de Las Fuentes, L.; He, S.; Okunade, A.L.; Patterson, B.W.; et al. Effects of Moderate and Subsequent Progressive Weight Loss on Metabolic Function and Adipose Tissue Biology in Humans with Obesity. Cell Metab. 2016, 23, 591–601. [Google Scholar] [CrossRef]
- Qiu, Y.; Fernández-García, B.; Lehmann, H.I.; Li, G.; Kroemer, G.; López-Otín, C.; Xiao, J. Exercise sustains the hallmarks of health. J. Sport Health Sci. 2023, 12, 8–35. [Google Scholar] [CrossRef]
- Flegal, K.M.; Kit, B.K.; Orpana, H.; Graubard, B.I. Association of All-Cause Mortality with Overweight and Obesity Using Standard Body Mass Index Categories: A Systematic Review and Meta-analysis. JAMA 2013, 309, 71–82. [Google Scholar] [CrossRef]
- American Diabetes Association. Understanding Blood Glucose and Exercise. 2018. Available online: https://diabetes.org/health-wellness/fitness/blood-glucose-and-exercise (accessed on 24 October 2024).
- Ji, S.; Dong, C.; Chen, R.; Shen, C.; Xiao, J.; Gu, Y.J.; Gao, J.L. Effects of Variability in Glycemic Indices on Longevity in Chinese Centenarians. Front. Nutr. 2022, 9, 955101. [Google Scholar] [CrossRef]
- Zgutka, K.; Tkacz, M.; Tomasiak, P.; Tarnowski, M. A Role for Advanced Glycation End Products in Molecular Ageing. Int. J. Mol. Sci. 2023, 24, 9881. [Google Scholar] [CrossRef]
- US Centers for Disease Control and Prevention (CDC). How People with Type 2 Diabetes Can Live Longer. 2024. Available online: https://www.cdc.gov/diabetes/data-research/research/treatment-goals.html (accessed on 18 August 2024).
- Murata, S.; Ebeling, M.; Meyer, A.C.; Schmidt-Mende, K.; Hammar, N.; Modig, K. Blood biomarker profiles and exceptional longevity: Comparison of centenarians and non-centenarians in a 35-year follow-up of the Swedish AMORIS cohort. GeroScience 2023, 46, 1693–1702. [Google Scholar] [CrossRef]
- Johnson, A.A.; Stolzing, A. The role of lipid metabolism in aging, lifespan regulation, and age-related disease. Aging Cell. 2019, 18, 13048. [Google Scholar] [CrossRef]
- Parthasarathy, V.; Frazier, D.T.; Bettcher, B.M.; Jastrzab, L.; Chao, L.; Reed, B.; Mungas, D.; Weiner, M.; DeCarli, C.; Chui, H.; et al. Triglycerides are negatively correlated with cognitive function in nondemented aging adults. Neuropsychology 2017, 31, 682–688. [Google Scholar] [CrossRef] [PubMed]
- Arai, Y.; Martin-Ruiz, C.M.; Takayama, M.; Abe, Y.; Takebayashi, T.; Koyasu, S.; Suematsu, M.; Hirose, N.; von Zglinicki, T. Inflammation, But Not Telomere Length, Predicts Successful Ageing at Extreme Old Age: A Longitudinal Study of Semi-supercentenarians. EBioMedicine 2015, 2, 1549–1558. [Google Scholar] [CrossRef]
- Coe, C.L.; Miyamoto, Y.; Love, G.D.; Karasawa, M.; Kawakami, N.; Kitayama, S.; Ryff, C.D. Cultural and life style practices associated with low inflammatory physiology in Japanese adults. Brain Behav. Immun. 2020, 90, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Fujii, H.; Doi, H.; Ko, T.; Fukuma, T.; Kadono, T.; Asaeda, K.; Kobayashi, R.; Nakano, T.; Doi, T.; Nakatsugawa, Y.; et al. Frequently abnormal serum gamma-glutamyl transferase activity is associated with future development of fatty liver: A retrospective cohort study. BMC Gastroenterol. 2020, 20, 217. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Ferguson, T.; Deev, A.; Deev, A.; Maher, C.A. Evaluation of the “15 Minute Challenge”: A Workplace Health and Wellbeing Program. Healthcare 2024, 12, 1255. [Google Scholar] [CrossRef]
- Cuntz, U.; Quadflieg, N.; Voderholzer, U. Health Risk and Underweight. Nutrients 2023, 15, 3262. [Google Scholar] [CrossRef] [PubMed]

| Full Cohort | Complete | Dropouts | p Complete vs. Dropouts | |
|---|---|---|---|---|
| N | 2300 | 1688 | 612 | |
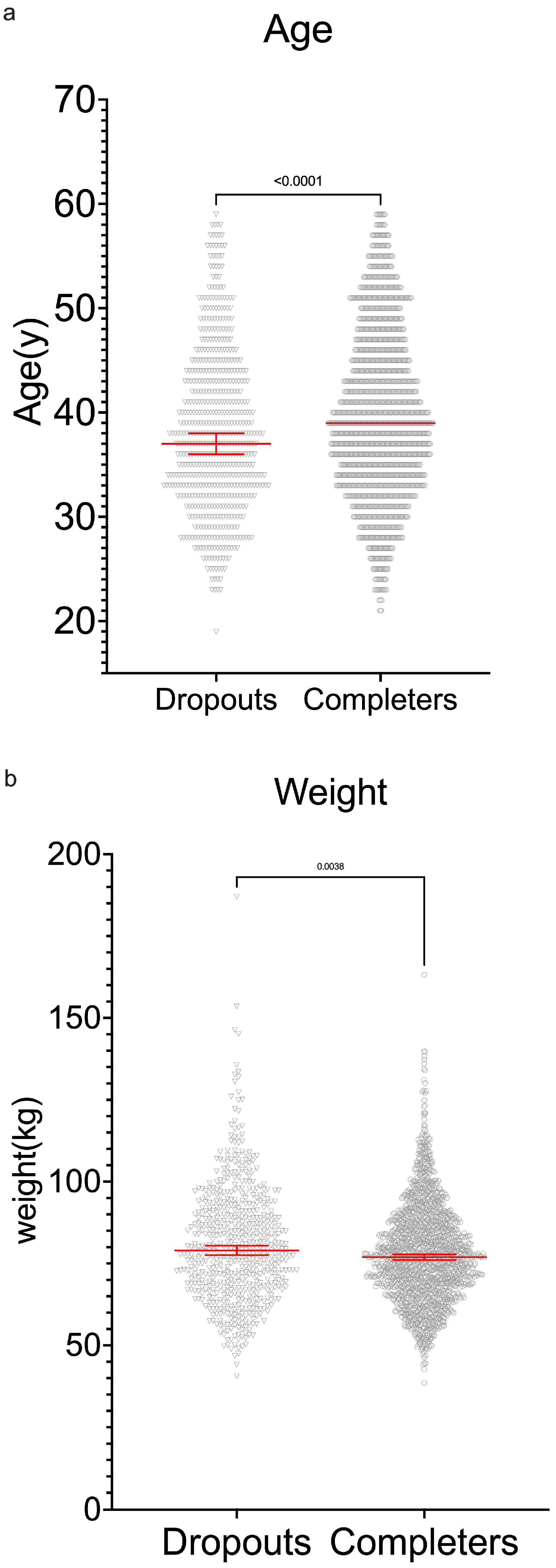
| Age (Y) (MED [IQR]) | 39 [33–45] | 39 [34–45] | 37 [32–43] | <0.0001 |
| Weight (kg) (MED [IQR]) | 77.5 [68.0–88] | 77.0 [68.0–87.2] | 79.1 [68.3–91.1] | <0.0001 |
| Male/Female Ratio | 2:1 | 2.2:1 | 1.7:1 | <0.0001 |
| Height (cm) (MED [IQR]) | 169 [162–175] | 169 [162–175] | 169 [162–175] | not significant |
| BMI (kg/m2) | 27.0 [24.5–30.1] | 26.8 [24.4–29.9] | 27.2 [25.0–30.8] | <0.001 |
| UAE National/Emirati (%) | 17.4 | 9.7 | 46 | |
| Non-Smoker/Smoker Ratio | 4.4:1 | 5.2:1 | 3.1:1 |
| Group | Abbr. | n | % |
|---|---|---|---|
| Total | 1688 | ||
| OVERWEIGHT-OVERWEIGHT | OW_OW | 651 | 38.6 |
| NORMALWEIGHT-NORMALWEIGHT | NW_NW | 499 | 29.6 |
| OBESE-OBESE | OB_OB | 342 | 20.3 |
| OVERWEIGHT-NORMALWEIGHT | OW_NW | 78 | 4.6 |
| OBESE-OVERWEIGHT | OB_OW | 57 | 3.4 |
| NORMALWEIGHT-OVERWEIGHT | NW_OW | 26 | 1.5 |
| OVERWEIGHT-OBESE | OW_OB | 22 | 1.3 |
| UNDERWEIGHT-UNDERWEIGHT | UW_UW | 6 | 0.4 |
| NORMALWEIGHT-UNDERWEIGHT | NW_UW | 3 | 0.2 |
| OBESE-NORMALWEIGHT | OB_NW | 2 | 0.1 |
| UNDERWEIGHT-NORMALWEIGHT | UW_NW | 2 | 0.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Hassani, G.; Koornneef, E.; Al Harbi, M.; Hussein, S.E.D.; Al Neyadi, G.; Al Hammadi, O.; Ghoneim, Y.; Abdrabo, M.; Holt, S.G. Benefits of an Innovative 90-Day Longevity Workplace Program on Health in the United Arab Emirates (UAE). Int. J. Environ. Res. Public Health 2025, 22, 1594. https://doi.org/10.3390/ijerph22101594
Al Hassani G, Koornneef E, Al Harbi M, Hussein SED, Al Neyadi G, Al Hammadi O, Ghoneim Y, Abdrabo M, Holt SG. Benefits of an Innovative 90-Day Longevity Workplace Program on Health in the United Arab Emirates (UAE). International Journal of Environmental Research and Public Health. 2025; 22(10):1594. https://doi.org/10.3390/ijerph22101594
Chicago/Turabian StyleAl Hassani, Ghanem, Erik Koornneef, Mariam Al Harbi, Salah El Din Hussein, Ghuwaya Al Neyadi, Omar Al Hammadi, Yasser Ghoneim, Mostafa Abdrabo, and Stephen G. Holt. 2025. "Benefits of an Innovative 90-Day Longevity Workplace Program on Health in the United Arab Emirates (UAE)" International Journal of Environmental Research and Public Health 22, no. 10: 1594. https://doi.org/10.3390/ijerph22101594
APA StyleAl Hassani, G., Koornneef, E., Al Harbi, M., Hussein, S. E. D., Al Neyadi, G., Al Hammadi, O., Ghoneim, Y., Abdrabo, M., & Holt, S. G. (2025). Benefits of an Innovative 90-Day Longevity Workplace Program on Health in the United Arab Emirates (UAE). International Journal of Environmental Research and Public Health, 22(10), 1594. https://doi.org/10.3390/ijerph22101594







