Impact of Face-to-Face and Online Mindfulness-Based Public Health Interventions on Health-Related Quality of Life in Older People: A Comparative Study
Abstract
1. Introduction
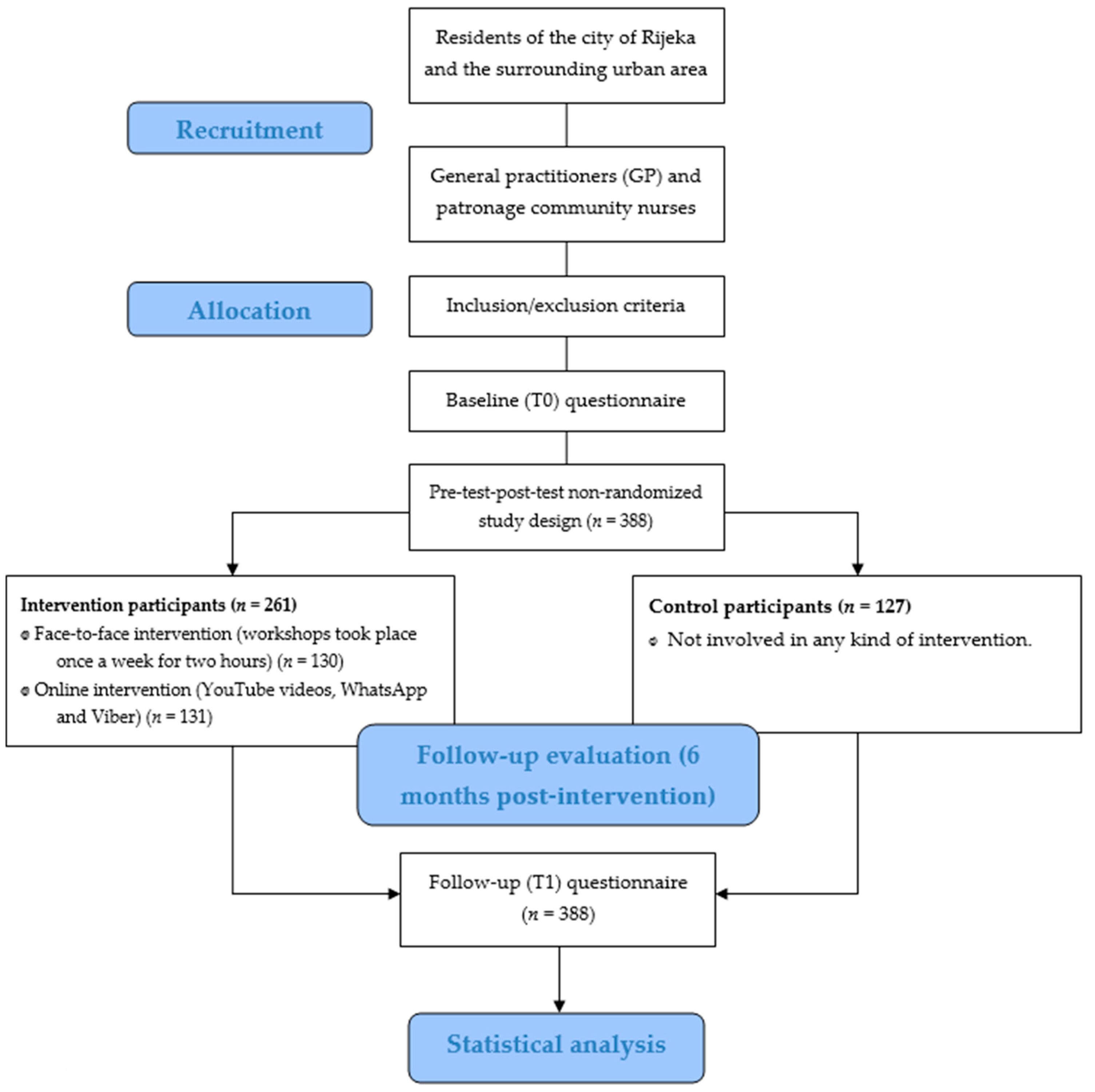
2. Materials and Methods
2.1. Participants
2.2. Inclusion/Exclusion Criteria
2.3. Intervention Procedures
2.4. Outcome Measures
2.5. Statistical Analysis
2.6. Ethical Considerations
3. Results
4. Discussion
Limitation of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HRQoL | Health-related quality of life |
| QoL | Quality of life |
| SF-12 | 12-Item Short-Form Health Survey |
| EQ-5D-5L | EuroQol-5 Dimensions-5 Level Questionnaire |
| GDP | Gross domestic product |
| HDI | Human Development Index |
| OECD | Organization for Economic Co-operation and Development |
| NCDs | Non-communicable chronic diseases |
| COPD | Chronic obstructive pulmonary disease |
| MBSR | Mindfulness-Based Stress Reduction |
| GROW | Goal, Reality, Options, and Will |
| CDSMP | Chronic Disease Self-Management Program |
| GPs | General practitioners |
| DSM-IV | Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition |
| SMART | Specific, Measurable, Achievable, Relevant and Time-bound |
| COVID-19 | Coronavirus disease 2019 |
| SEFAC | Social Engagement Framework for Addressing the Chronic Disease Challenge |
| QALY | Quality-Adjusted Life Year |
| EQ-VAS | EQ visual Analog scale |
| T0 | Baseline measurement |
| T1 | Six months post-intervention |
| IBM | International Business Machines Corporation |
| NY | New York |
| USA | United States of America |
| ANOVA | Analysis of variance |
| LSD | Least Significant Difference |
| EU | European Union |
| GDPR | General Data Protection Regulation |
| ISRCTN | International Standard Randomized Controlled Trial Number |
| WHO | World Health Organization |
| RCT | Randomized controlled trial |
| MBCT | Mindfulness-Based Cognitive Therapy |
| MBIs | Mindfulness-based interventions |
References
- World Health Organization. Programme on Mental Health: WHOQOL User Manual, 2012 Revision. Available online: https://apps.who.int/iris/handle/10665/77932 (accessed on 23 April 2025).
- Grabowska, K.; Antczak, R.; Zwierzchowski, J.; Panek, T. Individual Quality of Life and The Environment—Towards a Concept of Livable Areas for Persons with Disabilities in Poland. BMC Public Health 2021, 21, 740. [Google Scholar] [CrossRef]
- Stiglitz, J.E.; Sen, A.; Fitoussi, J.P. Report by the Commission on the Measurement of Economic Performance and Social Progress. Available online: https://ec.europa.eu/eurostat/documents/8131721/8131772/Stiglitz-Sen-Fitoussi-Commission-report.pdf (accessed on 23 April 2025).
- United Nations Development Programme. Human Development Index (HDI). Available online: https://hdr.undp.org/data-center/human-development-index#/indicies/HDI (accessed on 24 April 2025).
- Sustainable Development Solutions Network. The World Happiness Report. Available online: https://worldhappiness.report/about/ (accessed on 24 April 2025).
- Organisation for Economic Co-operation and Development. Better Life Index. Available online: https://www.oecdbetterlifeindex.org/#/11111111111 (accessed on 24 April 2025).
- National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. Health-Related Quality of Life (HRQOL). Available online: https://archive.cdc.gov/#/details?url=https://www.cdc.gov/hrqol/index.htm (accessed on 25 April 2025).
- Lo Buono, V.; Corallo, F.; Bramanti, P.; Marino, S. Coping Strategies and Health-Related Quality of Life After Stroke. J. Health Psychol. 2017, 22, 16–28. [Google Scholar] [CrossRef] [PubMed]
- Dominick, K.L.; Ahern, F.M.; Gold, C.H.; Heller, D.A. Relationship of Health-Related Quality of Life to Health Care Utilization and Mortality among Older Adults. Aging Clin. Exp. Res. 2002, 14, 499–508. [Google Scholar] [CrossRef]
- DeSalvo, K.B.; Bloser, N.; Reynolds, K.; He, J.; Muntner, P. Mortality Prediction with a Single General Self-Rated Health Question. A Meta-Analysis. J. Gen. Intern. Med. 2006, 21, 267–275. [Google Scholar] [CrossRef]
- Marquez, D.X.; Aguiñaga, S.; Vásquez, P.M.; Conroy, D.E.; Erickson, K.I.; Hillman, C.; Stillman, C.M.; Ballard, R.M.; Sheppard, B.B.; Petruzzello, S.J.; et al. A Systematic Review of Physical Activity and Quality of Life and Well-Being. Transl. Behav. Med. 2020, 10, 1098–1109. [Google Scholar] [CrossRef]
- Otones, P.; García, E.; Sanz, T.; Pedraz, A. A Physical Activity Program Versus Usual Care in The Management of Quality of Life for Pre-Frail Older Adults with Chronic Pain: Randomized Controlled Trial. BMC Geriatr. 2020, 20, 396. [Google Scholar] [CrossRef]
- Dale, H.; Brassington, L.; King, K. The Impact of Healthy Lifestyle Interventions on Mental Health and Wellbeing: A Systematic Review. Ment. Health. Rev. J. 2014, 19, 1–26. [Google Scholar] [CrossRef]
- Cheng, W.L.; Chang, C.C.; Griffiths, M.D.; Yen, C.F.; Liu, J.H.; Su, J.A.; Lin, C.Y.; Pakpour, A.H. Quality of Life and Care Burden among Family Caregivers of People with Severe Mental Illness: Mediating Effects of Self-Esteem and Psychological Distress. BMC Psychiatry 2022, 22, 672. [Google Scholar] [CrossRef] [PubMed]
- Chollou, K.M.; Shirzadi, S.; Pourrazavi, S.; Babazadeh, T.; Ranjbaran, S. The Role of Perceived Social Support on Quality of Life in People with Cardiovascular Diseases. Ethiop. J. Health. Sci. 2022, 32, 1019–1026. [Google Scholar] [CrossRef]
- Chiesa, A.; Serretti, A. Mindfulness-Based stress Reduction for Stress Management in Healthy People: A Review and Meta-Analysis. J. Altern. Complement. Med. 2009, 15, 593–600. [Google Scholar] [CrossRef]
- Reibel, D.K.; Greeson, J.M.; Brainhard, G.C.; Rosenzweig, S. Mindfulness-Based Stress Reduction and Health-Related Quality of Life in A Heterogeneous Patient Population. Gen. Hosp. Psychiatry 2001, 23, 183–192. [Google Scholar] [CrossRef]
- Carlson, L.E.; Speca, M.; Patel, K.D.; Goodey, E. Mindfulness-Based Stress Reduction in Relation to Quality of Life, Mood, Symptoms of Stress, and Immune Parameters in Breast and Prostate Cancer Outpatients. Psychosom. Med. 2003, 65, 571–581. [Google Scholar] [CrossRef]
- Lorig, K.R.; Ritter, P.L.; Laurent, D.D.; Plant, K. Internet-Based Chronic Disease Self-Management: A Randomized Trial. Med. Care. 2006, 44, 964–971. [Google Scholar] [CrossRef]
- Glasgow, R.E.; Kurz, D.; King, D.; Dickman, J.M.; Faber, A.J.; Halterman, E.; Woolley, T.; Toobert, D.J.; Strycker, L.A.; Estabrooks, P.A.; et al. Twelve-Month Outcomes of an Internet-Based Diabetes Self-Management Support Program. Patient Educ. Couns. 2012, 87, 81–92. [Google Scholar] [CrossRef]
- Jaglal, S.B.; Haroun, V.A.; Salbach, N.M.; Hawker, G.; Voth, J.; Lou, W.; Kontos, P.; Cameron, J.E.; Cockerill, R.; Bereket, T. Increasing Access to Chronic Disease Self-Management Programs in Rural and Remote Communities Using Telehealth. Telemed. J. E Health 2013, 19, 467–473. [Google Scholar] [CrossRef]
- Buyl, R.; Beogo, I.; Fobelets, M.; Deletroz, C.; Van Landuyt, P.; Dequanter, S.; Gorus, E.; Bourbonnais, A.; Giguère, A.; Lechasseur, K.; et al. E-Health Interventions for Healthy Aging: A Systematic Review. Syst. Rev. 2020, 9, 128. [Google Scholar] [CrossRef]
- Nguyen, H.Q.; Donesky-Cuenco, D.; Wolpin, S.; Reinke, L.F.; Benditt, J.O.; Paul, S.M.; Carrieri-Kohlman, V. Randomized Controlled Trial of an Internet-Based Versus Face-to-Face Dyspnea Self-Management Program for Patients with Chronic Obstructive Pulmonary Disease: Pilot Study. J. Med. Internet Res. 2008, 10, e9. [Google Scholar] [CrossRef]
- Bourne, S.; DeVos, R.; North, M.; Chauhan, A.; Green, B.; Brown, T.; Cornelius, V.; Wilkinson, T. Online Versus Face-to-Face Pulmonary Rehabilitation for Patients with Chronic Obstructive Pulmonary Disease: Randomised Controlled Trial. BMJ Open 2017, 7, e014580. [Google Scholar] [CrossRef] [PubMed]
- Hwang, R.; Bruning, J.; Morris, N.R.; Mandrusiak, A.; Russell, T. Home-Based Telerehabilitation Is Not Inferior to a Centre-Based Program in Patients with Chronic Heart Failure: A Randomised Trial. J. Physiother 2017, 63, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J. Mindfulness-Based Interventions in Context: Past, Present, and Future. Clin. Psychol. 2003, 10, 144–156. [Google Scholar] [CrossRef]
- Bishop, S.R.; Lau, M.; Shapiro, S.; Carlson, L.; Anderson, N.D.; Carmody, J.; Segal, Z.V.; Abbey, S.; Speca, M.; Velting, D.; et al. Mindfulness: A Proposed Operational Definition. Clin. Psychol. 2004, 11, 230–234. [Google Scholar] [CrossRef]
- Lardone, A.; Liparoti, M.; Sorrentino, P.; Rucco, R.; Jacini, F.; Polverino, A.; Minino, R.; Pesoli, M.; Baselice, F.; Sorriso; et al. Mindfulness Meditation Is Related to Long-Lasting Changes in Hippocampal Functional Topology During Resting State: A Magnetoencephalography Study. Neural. Plast. 2018, 2018, 5340717. [Google Scholar] [CrossRef]
- Khoury, B.; Sharma, M.; Rush, S.E.; Fournier, C. Mindfulness-Based Stress Reduction for Healthy Individuals: A Meta-Analysis. J. Psychosom. Res. 2015, 78, 519–528. [Google Scholar] [CrossRef]
- Marino, F.; Failla, C.; Carrozza, C.; Ciminata, M.; Chilà, P.; Minutoli, R.; Genovese, S.; Puglisi, A.; Arnao, A.A.; Tartarisco, G.; et al. Mindfulness-Based Interventions for Physical and Psychological Wellbeing in Cardiovascular Diseases: A Systematic Review and Meta-Analysis. Brain. Sci. 2021, 11, 727. [Google Scholar] [CrossRef]
- Marciniak, R.; Šumec, R.; Vyhnálek, M.; Bendíčková, K.; Lázničková, P.; Forte, G.; Jeleník, A.; Římalová, V.; Frič, J.; Hort, J.; et al. The Effect of Mindfulness-Based Stress Reduction (MBSR) on Depression, Cognition, and Immunity in Mild Cognitive Impairment: A Pilot Feasibility Study. Clin. Interv. Aging 2020, 15, 365–381. [Google Scholar] [CrossRef]
- Grossman, P.; Niemann, L.; Schmidt, S.; Walach, H. Mindfulness-Based Stress Reduction and Health Benefits. A Meta-Analysis. J. Psychosom. Res. 2004, 57, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Compen, F.; Bisseling, E.; Schellekens, M.; Donders, R.; Carlson, L.; van der Lee, M.; Speckens, A. Face-to-Face and Internet-Based Mindfulness-Based Cognitive Therapy Compared with Treatment as Usual in Reducing Psychological Distress in Patients with Cancer: A Multicenter Randomized Controlled Trial. J. Clin. Oncol. 2018, 36, 2413–2421. [Google Scholar] [CrossRef] [PubMed]
- Burgess, D.J.; Calvert, C.; Hagel Campbell, E.M.; Allen, K.D.; Bangerter, A.; Behrens, K.; Branson, M.; Bronfort, G.; Cross, L.J.S.; Evans, R.; et al. Telehealth Mindfulness-Based Interventions for Chronic Pain: The LAMP Randomized Clinical Trial. JAMA Intern. Med. 2024, 184, 1163–1173. [Google Scholar] [CrossRef]
- Day, M.A.; Ciol, M.A.; Mendoza, M.E.; Borckardt, J.; Ehde, D.M.; Newman, A.K.; Chan, J.F.; Drever, S.A.; Friedly, J.L.; Burns, J.; et al. The Effects of Telehealth-Delivered Mindfulness Meditation, Cognitive Therapy, and Behavioral Activation for Chronic Low Back Pain: A Randomized Clinical Trial. BMC Med. 2024, 22, 156. [Google Scholar] [CrossRef]
- Herbert, M.S.; Afari, N.; Liu, L.; Heppner, P.; Rutledge, T.; Williams, K.; Eraly, S.; VanBuskirk, K.; Nguyen, C.; Bondi, M.; et al. Telehealth Versus In-Person Acceptance and Commitment Therapy for Chronic Pain: A Randomized Noninferiority Trial. J. Pain 2017, 18, 200–211. [Google Scholar] [CrossRef]
- Whitmore, J. Coaching for Performance: Growing Human Potential and Purpose—The Principles and Practice of Coaching and Leadership, 4th ed.; Nicholas Brealey Publishing: London, UK, 2009. [Google Scholar]
- Tan, S.S.; Pisano, M.M.; Boone, A.L.; Baker, G.; Pers, Y.M.; Pilotto, A.; Valsecchi, V.; Zora, S.; Zhang, X.; Fierloos, I.; et al. Evaluation Design of EFFICHRONIC: The Chronic Disease Self-Management Programme (CDSMP) Intervention for Citizens with a Low Socioeconomic Position. Int. J. Environ. Res. Public Health 2019, 16, 1883. [Google Scholar] [CrossRef]
- Mindfulness Association. Mindfulness Based Living Course (MBLC). Available online: https://www.mindfulnessassociation.net/mindfulness-courses/8-week-mblc/ (accessed on 29 April 2025).
- Handley, M.A.; Lyles, C.R.; McCulloch, C.; Cattamanchi, A. Selecting and Improving Quasi-Experimental Designs in Effectiveness and Implementation Research. Annu. Rev. Public Health 2018, 39, 5–25. [Google Scholar] [CrossRef]
- Dweck, C.S.; Yeager, D.S. Mindsets: A View from Two Eras. Perspect. Psychol. Sci. 2019, 14, 481–496. [Google Scholar] [CrossRef]
- Bailey, R.R. Goal Setting and Action Planning for Health Behavior Change. Am. J. Lifestyle. Med. 2017, 13, 615–618. [Google Scholar] [CrossRef]
- Juraga, D.; Rukavina, T.; Bilajac, L.; Marinović Glavić, M.; Roviš, D.; Raat, H.; Vasiljev, V. Comparison of Conventional (Face-To-Face) and Online Approach in Mindfulness-Based Chronic Disease Self-Management Interventions for Older Adults. J. Public Health Res. 2022, 11, 2779. [Google Scholar] [CrossRef]
- Leong, S.M.; Lei, W.I.; Chan, U.W. The Six-Month and One-Year Outcome of a Chronic Disease Self-Management Program Among Older Adults in Macao: A Quasi-Experimental Study. SAGE Open Nurs. 2020, 6, 2377960820958231. [Google Scholar] [CrossRef] [PubMed]
- Gallegos, A.M.; Moynihan, J.; Pigeon, W.R. A Secondary Analysis of Sleep Quality Changes in Older Adults From a Randomized Trial of an MBSR Program. J. Appl. Gerontol. 2018, 37, 1327–1343. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Tan, S.S.; Fierloos, I.; Zanutto, O.; Alhambra-Borrás, T.; Vasiljev, V.; Bennett, S.; Rentoumis, T.; Buranello, A.; Macchione, S.; et al. Evaluation Design of the Social Engagement Framework for Addressing the Chronic-Disease-Challenge (SEFAC): A Mindfulness-Based Intervention to Promote the Self-Management of Chronic Conditions and a Healthy Lifestyle. BMC Public Health 2019, 19, 664. [Google Scholar] [CrossRef] [PubMed]
- Terwee, C.B.; Bot, S.D.; de Boer, M.R.; van der Windt, D.A.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C. Quality Criteria Were Proposed for Measurement Properties of Health Status Questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef]
- Pyo, E.; Weber, M.B.; Sivaram, J.; Staimez, L.R.; Mohan, V.; Anjana, R.M.; Haardörfer, R.; Ranjani, H. Construct Validity of the 12-Item Short Form Health Survey (SF-12) Version 2 and the Impact of Lifestyle Modifications on the Health-Related Quality of Life Among Indian Adults with Prediabetes: Results from the D-CLIP Trial. Qual. Life Res. 2024, 33, 1593–1603. [Google Scholar] [CrossRef]
- Feng, Y.S.; Kohlmann, T.; Janssen, M.F.; Buchholz, I. Psychometric Properties of the EQ-5D-5L: A Systematic Review of the Literature. Qual. Life Res. 2021, 30, 647–673. [Google Scholar] [CrossRef] [PubMed]
- Des Jarlais, D.C.; Lyles, C.; Crepaz, N.; TREND Group. Improving the Reporting Quality of Nonrandomized Evaluations of Behavioral and Public Health Interventions: The TREND Statement. Am. J. Public Health 2004, 94, 361–366. [Google Scholar] [CrossRef]
- Alsubaie, M.; Abbott, R.; Dunn, B.; Dickens, C.; Keil, T.F.; Henley, W.; Kuyken, W. Mechanisms of Action in Mindfulness-Based Cognitive Therapy (MBCT) and Mindfulness-Based Stress Reduction (MBSR) in People with Physical and/or Psychological Conditions: A Systematic Review. Clin. Psychol. Rev. 2017, 55, 74–91. [Google Scholar] [CrossRef]
- Hoge, E.A.; Acabchuk, R.L.; Kimmel, H.; Moitra, E.; Britton, W.B.; Dumais, T.; Ferrer, R.A.; Lazar, S.W.; Vago, D.; Lipsky, J.; et al. Emotion-Related Constructs Engaged by Mindfulness-Based Interventions: A Systematic Review and Meta-Analysis. Mindfulness 2021, 12, 1041–1062. [Google Scholar] [CrossRef]
- Grecucci, A.; Pappaianni, E.; Siugzdaite, R.; Theuninck, A.; Job, R. Mindful Emotion Regulation: Exploring the Neurocognitive Mechanisms behind Mindfulness. Biomed. Res. Int. 2015, 2015, 670724. [Google Scholar] [CrossRef]
- Sommers-Spijkerman, M.; Austin, J.; Bohlmeijer, E.; Pots, W. New Evidence in the Booming Field of Online Mindfulness: An Updated Meta-analysis of Randomized Controlled Trials. JMIR Ment. Health 2021, 8, e28168. [Google Scholar] [CrossRef]
- Spijkerman, M.P.; Pots, W.T.; Bohlmeijer, E.T. Effectiveness of Online Mindfulness-Based Interventions in Improving Mental Health: A Review and Meta-Analysis of Randomised Controlled Trials. Clin. Psychol. Rev. 2016, 45, 102–114. [Google Scholar] [CrossRef]
- König, H.H.; Neumann-Böhme, S.; Sabat, I.; Schreyögg, J.; Torbica, A.; van Exel, J.; Barros, P.P.; Stargardt, T.; Hajek, A. Health-Related Quality of Life in Seven European Countries Throughout the Course of the COVID-19 Pandemic: Evidence from the European COVID Survey (ECOS). Qual. Life. Res. 2023, 32, 1631–1644. [Google Scholar] [CrossRef]
- World Health Organization. COVID-19 Pandemic Triggers 25% Increase in Prevalence of Anxiety and Depression Worldwide. Available online: https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide (accessed on 10 October 2025).
- Muppavarapu, K.; Saeed, S.A.; Jones, K.; Hurd, O.; Haley, V. Study of Impact of Telehealth Use on Clinic “No Show” Rates at an Academic Practice. Psychiatr. Q. 2022, 93, 689–699. [Google Scholar] [CrossRef] [PubMed]
- Ojinnaka, C.O.; Johnstun, L.; Dunnigan, A.; Nordstrom, L.; Yuh, S. Telemedicine Reduces Missed Appointments but Disparities Persist. Am. J. Prev. Med. 2024, 67, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Choi, N.G.; DiNitto, D.M.; Marti, C.N. Older Adults’ Frequency of Going Outside during the COVID-19 Pandemic: Associations with Physical Distancing, Health Status, and Fall Risk Factors. J. Appl. Gerontol. 2023, 42, 324–335. [Google Scholar] [CrossRef]
- Manchia, M.; Gathier, A.W.; Yapici-Eser, H.; Schmidt, M.V.; de Quervain, D.; van Amelsvoort, T.; Bisson, J.I.; Cryan, J.F.; Howes, O.D.; Pinto, L.; et al. The Impact of the Prolonged COVID-19 Pandemic on Stress Resilience and Mental Health: A Critical Review Across Waves. Eur. Neuropsychopharmacol. 2022, 55, 22–83. [Google Scholar] [CrossRef]
- Hatef, E.; Wilson, R.F.; Zhang, A.; Hannum, S.M.; Kharrazi, H.; Davis, S.A.; Foroughmand, I.; Weiner, J.P.; Robinson, K.A. Effectiveness of Telehealth Versus In-Person Care During the COVID-19 Pandemic: A Systematic Review. NPJ Digit. Med. 2024, 7, 157. [Google Scholar] [CrossRef]
- Badh, G.; Knowles, T. Acoustic and Perceptual Impact of Face Masks on Speech: A Scoping Review. PLoS ONE 2023, 18, e0285009. [Google Scholar] [CrossRef]
- Jacobsen, P.; Choksi, T.; Sawyer, K.; Maximen, C.; Harding, E.; Richardson, M. Home Practice in Mindfulness-Based Interventions for Psychosis Groups: A Systematic Review and Qualitative Study. BMC Psychol. 2022, 10, 9. [Google Scholar] [CrossRef]
- Witarto, B.S.; Visuddho, V.; Witarto, A.P.; Bestari, D.; Sawitri, B.; Melapi, T.A.S.; Wungu, C.D.K. Effectiveness of Online Mindfulness-Based Interventions in Improving Mental Health During the COVID-19 Pandemic: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. PLoS ONE 2022, 17, e0274177. [Google Scholar] [CrossRef]
- Amro, T.M.; Arcos González, P.; Montero Viñuales, E.; Castro Delgado, R. Impact of COVID-19 Pandemic on Stress and Burnout Levels amongst Emergency Medical Technicians: A Cross-Sectional Study in Spain. Ann. Med. 2022, 54, 3007–3016. [Google Scholar] [CrossRef]
- Karimi, S.; Derakhshan, M.; Tondro, A. Evaluation of the Relationship between Stress and Severity of COVID-19 Symptoms and Sleep Quality in COVID-19 Patients. Maedica 2022, 17, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Monnig, M.A.; Clark, S.E.; Avila, J.C.; Sokolovsky, A.W.; Treloar Padovano, H.; Goodyear, K.; Aston, E.R.; Haass-Koffler, C.L.; Tidey, J.W.; Ahluwalia, J.S.; et al. COVID-19-Related Stressors and Clinical Mental Health Symptoms in a Northeast US Sample. Int. J. Environ. Res. Public Health 2023, 20, 1367. [Google Scholar] [CrossRef] [PubMed]
- Grasaas, E.; Skarstein, S.; Mikkelsen, H.T.; Småstuen, M.C.; Rohde, G.; Helseth, S.; Haraldstad, K. The Relationship Between Stress and Health-Related Quality of Life and the Mediating Role of Self-Efficacy in Norwegian Adolescents: A Cross-Sectional Study. Health Qual. Life Outcomes 2022, 20, 162. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.; Honan, C.; Skromanis, S.; Sanderson, B.; Matthews, A.J. Psychological Outcomes and Mechanisms of Mindfulness-Based Training for Generalised Anxiety Disorder: A Systematic Review and Meta-Analysis. Curr. Psychol. 2023, 43, 5318–5340. [Google Scholar] [CrossRef] [PubMed]
- Mohsen, S.; El-Masry, R.; Ali, O.F.; Abdel-Hady, D. Quality of Life During COVID-19 Pandemic: A Community-Based Study in Dakahlia Governorate, Egypt. Glob. Health. Res. Policy 2022, 7, 15. [Google Scholar] [CrossRef]
- Arab-Zozani, M.; Hashemi, F.; Safari, H.; Yousefi, M.; Ameri, H. Health-Related Quality of Life and its Associated Factors in COVID-19 Patients. Osong Public Health Res. Perspect. 2020, 11, 296–302. [Google Scholar] [CrossRef]
- Pierce, M.; Hope, H.; Ford, T.; Hatch, S.; Hotopf, M.; John, A.; Kontopantelis, E.; Webb, R.; Wessely, S.; McManus, S.; et al. Mental Health Before and During the COVID-19 Pandemic: A Longitudinal Probability Sample Survey of the UK Population. Lancet Psychiatry 2020, 7, 883–892. [Google Scholar] [CrossRef]
- Niedzwiedz, C.L.; Green, M.J.; Benzeval, M.; Campbell, D.; Craig, P.; Demou, E.; Leyland, A.; Pearce, A.; Thomson, R.; Whitley, E.; et al. Mental Health and Health Behaviours Before and During the Initial Phase of the COVID-19 Lockdown: Longitudinal Analyses of the UK Household Longitudinal Study. J. Epidemiol. Community Health 2021, 75, 224–231. [Google Scholar] [CrossRef]
- Santomauro, D.F.; Mantilla Herrera, A.M.; Shadid, J.; Zheng, P.; Ashbaugh, C.; Pigott, D.M.; Abbafati, C.; Adolph, C.; Amlag, J.O.; Aravkin, A.Y.; et al. COVID-19 Mental Disorders Collaborators. Global Prevalence and Burden of Depressive and Anxiety Disorders in 204 Countries and Territories in 2020 Due to the COVID-19 Pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef] [PubMed]
- van Ballegooijen, H.; Goossens, L.; Bruin, R.H.; Michels, R.; Krol, M. Concerns, Quality of Life, Access to Care and Productivity of the General Population During the First 8 Weeks of the Coronavirus Lockdown in Belgium and the Netherlands. BMC Health Serv. Res. 2021, 21, 227. [Google Scholar] [CrossRef] [PubMed]



| Face-to-Face Intervention (n = 130) n (%) | Online Intervention (n = 131) n (%) | Control Group (n = 127) n (%) | Total (n = 388) n (%) | p | |
|---|---|---|---|---|---|
| Age (y) () | 71.9 | 71.5 | 72.1 | 71.8 | 0.664 |
| Sex | |||||
| Women Men | 116 (89.2) | 104 (79.4) | 83 (65.4) | 303 (78.1) | <0.001 |
| 14 (10.8) | 27 (20.6) | 44 (34.6) | 85 (21.9) | ||
| Marital status | |||||
| Single Partnership Widow(er) | 16 (12.3) | 21 (16.0) | 13 (10.2) | 50 (12.9) | |
| 65 (50.0) 49 (37.7) | 75 (57.3) 35 (26.7) | 92 (72.4) 22 (17.3) | 232 (59.8) 106 (27.3) | 0.027 | |
| Household composition | |||||
| Living alone Living with others | 48 (36.9) | 42 (32.1) | 22 (17.3) | 112 (28.9) | |
| 82 (63.1) | 89 (67.9) | 105 (82.7) | 276 (71.1) | 0.002 | |
| Educational level | |||||
| Primary or less Secondary Tertiary or higher | 24 (18.5) | 4 (3.1) | 8 (6.3) | 36 (9.3) | |
| 64 (49.2) 42 (32.3) | 75 (57.2) 52 (39.7) | 84 (66.1) 35 (27.6) | 223 (57.5) 129 (33.2) | 0.018 | |
| Household income | |||||
| Decile 1 + 2 (<239–345€) Decile 3 + 4 (346–597€) Decile 5 + 6 (598–889€) Decile 7 + 8 (890–1287€) Decile 9 + 10 (1288–>1606€) | 24 (18.5) | 13 (9.9) | 10 (7.9) | 47 (12.1) | 0.080 |
| 50 (38.5) | 35 (26.7) | 55 (43.3) | 140 (36.1) | ||
| 26 (20.0) | 59 (45.0) | 39 (30.7) | 124 (32.0) | ||
| 20 (15.4) 10 (7.7) | 17 (13.0) 7 (5.3) | 19 (15.0) 4 (3.1) | 56 (14.4) 21 (5.4) |
| Sum of Squares | df | Mean Square | F | p | η2 | |
|---|---|---|---|---|---|---|
| SF-12—Physical dimension | 371.562 | 1 | 371.562 | 11.794 | <0.001 | 0.030 |
| Group: face-to-face, online, control | 812.892 | 2 | 406.446 | 2.862 | 0.058 | 0.015 |
| SF-12—Physical dimension x Group: face-to-face, online, control | 549.607 | 2 | 274.803 | 8.723 | <0.001 | 0.043 |
| Error (SF-12—Physical dimension) | 12,128.678 | 385 | 31.503 | |||
| Error (Group: face-to-face, online, control) | 54,683.601 | 385 | 142.035 |
| Participants per Intervention | SF-12—Physical Dimension (T0) (SD) | SF-12—Physical Dimension (T1) (SD) | MD | SE | p | 95% Confidence Interval for Difference | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| Face-to-face (n = 130) | 44.0 (8.8) | 45.0 (8.6) | −1.014 | 0.696 | 0.146 | −2.382 | 0.355 |
| Online (n = 131) | 43.3 (9.8) | 46.9 (9.6) | −3.605 | 0.694 | <0.001 | −4.969 | −2.242 |
| Control (n = 127) | 42.9 (9.7) | 42.4 (9.3) | 0.467 | 0.704 | 0.508 | −0.918 | 1.852 |
| Sum of Squares | df | Mean Square | F | p | η2 | |
|---|---|---|---|---|---|---|
| SF-12—Mental dimension | 7.615 | 1 | 7.615 | 0.181 | 0.670 | 0.000 |
| Group: face-to-face, online, control | 645.765 | 2 | 322.883 | 2.779 | 0.063 | 0.014 |
| SF-12—Mental dimension x Group: face-to-face, online, control | 523.541 | 2 | 261.771 | 6.233 | 0.002 | 0.031 |
| Error (SF-12—Mental dimension) | 16,170.276 | 385 | 42.001 | |||
| Error (Group: face-to-face, online, control) | 44,735.846 | 385 | 116.197 |
| Participants per Intervention | SF-12—Mental Dimension (T0) (SD) | SF-12—Mental Dimension (T1) (SD) | MD | SE | p | 95% Confidence Interval for Difference | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| Face-to-face (n = 130) | 47.8 (8.8) | 48.9 (8.6) | −1.156 | 0.804 | 0.151 | −2.737 | 0.424 |
| Online (n = 131) | 46.1 (10.1) | 47.7 (9.6) | −1.561 | 0.801 | 0.052 | −3.136 | 0.013 |
| Control (n = 127) | 47.2 (9.4) | 45.1 (9.3) | 2.123 | 0.813 | 0.009 | 0.524 | 3.722 |
| Sum of Squares | df | Mean Square | F | p | η2 | |
|---|---|---|---|---|---|---|
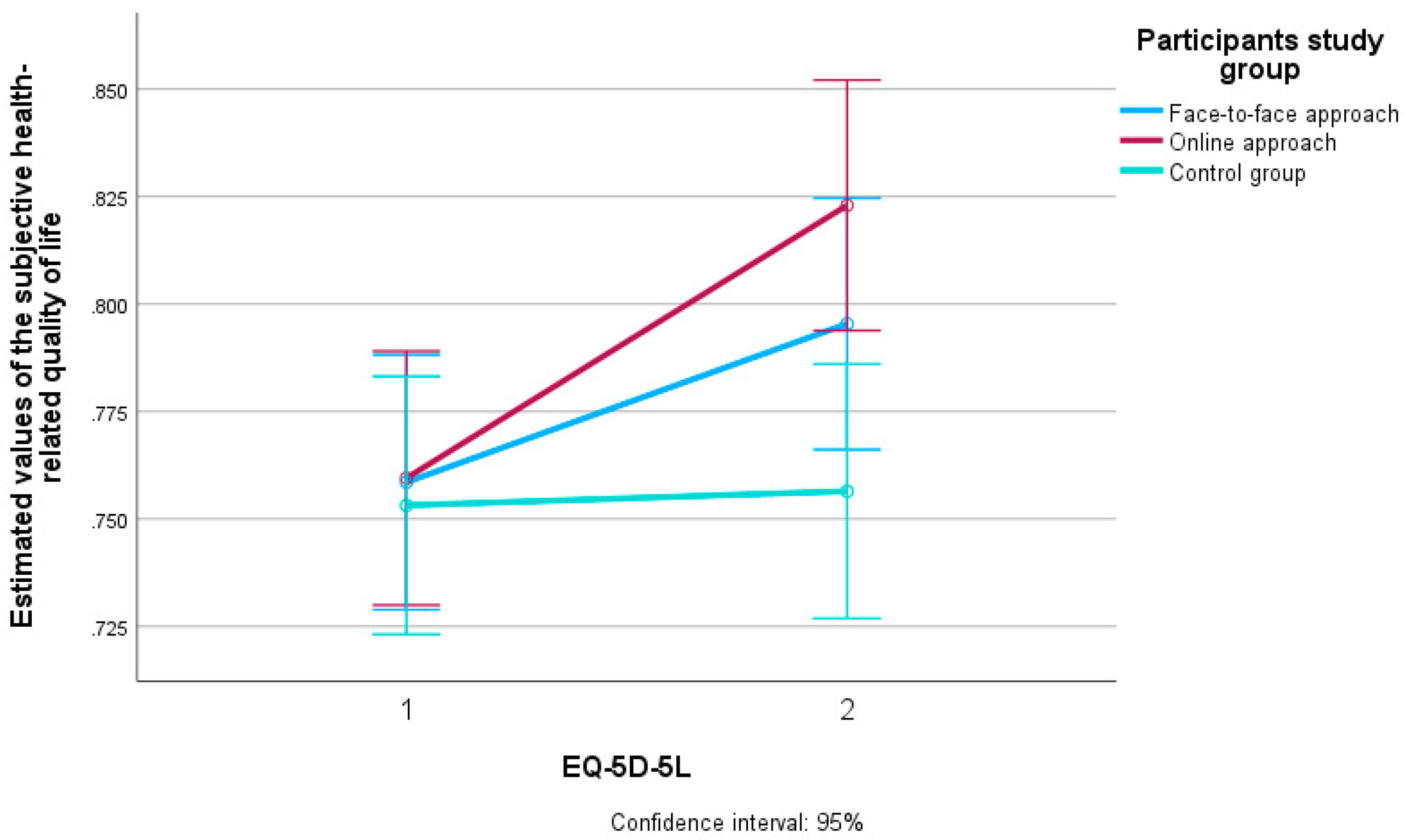
| EQ-5D-5L | 0.231 | 1 | 0.231 | 19.648 | <0.001 | 0.049 |
| Group: face-to-face, online, control | 0.173 | 2 | 0.087 | 1.862 | 0.157 | 0.010 |
| EQ-5D-5L x Group: face-to-face, online, control | 0.117 | 2 | 0.059 | 4.977 | 0.007 | 0.025 |
| Error (EQ-5D-5L) | 4.533 | 385 | 0.012 | |||
| Error (Group: face-to-face, online, control) | 17.937 | 385 | 0.047 |
| Participants per Intervention | EQ-5D-5L (T0) (SD) | EQ-5D-5L (T1) (SD) | MD | SE | p | 95% Confidence Interval for Difference | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| Face-to-face (n = 130) | 0.76 (0.15) | 0.80 (0.16) | −0.037 | 0.013 | 0.006 | −0.063 | −0.010 |
| Online (n = 131) | 0.76 (0.17) | 0.82 (0.16) | −0.063 | 0.013 | <0.001 | −0.090 | −0.037 |
| Control (n = 127) | 0.75 (0.19) | 0.76 (0.19) | −0.003 | 0.014 | 0.810 | −0.030 | 0.023 |
| Sum of Squares | df | Mean Square | F | p | η2 | |
|---|---|---|---|---|---|---|
| EQ-VAS | 2246.703 | 1 | 2246.703 | 19.120 | <0.001 | 0.047 |
| Group: face-to-face, online, control | 3054.450 | 2 | 1527.225 | 3.467 | 0.032 | 0.018 |
| EQ-VAS x Group: face-to-face, online, control | 3464.734 | 2 | 1732.367 | 14.743 | <0.001 | 0.071 |
| Error (EQ-VAS) | 45,240.436 | 385 | 117.508 | |||
| Error (Group: face-to-face, online, control) | 169,609.612 | 385 | 440.544 |
| Participants per Intervention | EQ-VAS (T0) (SD) | EQ-VAS (T1) (SD) | MD | SE | p | 95% Confidence Interval for Difference | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| Face-to-face (n = 130) | 69.4 (15.8) | 75.1 (16.9) | −5.731 | 1.345 | <0.001 | −8.374 | −3.087 |
| Online (n = 131) | 70.1 (17.1) | 77.2 (14.9) | −7.031 | 1.339 | <0.001 | −9.664 | −4.397 |
| Control (n = 127) | 70.2 (17.6) | 67.6 (17.9) | 2.551 | 1.360 | 0.061 | −0.123 | 5.226 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Juraga, D.; Rukavina, T.; Glavić, M.M.; Roviš, D.; Racz, A.; Bilajac, L.; Antonić, M.; Raat, H.; Vasiljev, V. Impact of Face-to-Face and Online Mindfulness-Based Public Health Interventions on Health-Related Quality of Life in Older People: A Comparative Study. Int. J. Environ. Res. Public Health 2025, 22, 1588. https://doi.org/10.3390/ijerph22101588
Juraga D, Rukavina T, Glavić MM, Roviš D, Racz A, Bilajac L, Antonić M, Raat H, Vasiljev V. Impact of Face-to-Face and Online Mindfulness-Based Public Health Interventions on Health-Related Quality of Life in Older People: A Comparative Study. International Journal of Environmental Research and Public Health. 2025; 22(10):1588. https://doi.org/10.3390/ijerph22101588
Chicago/Turabian StyleJuraga, Denis, Tomislav Rukavina, Mihaela Marinović Glavić, Darko Roviš, Aleksandar Racz, Lovorka Bilajac, Maša Antonić, Hein Raat, and Vanja Vasiljev. 2025. "Impact of Face-to-Face and Online Mindfulness-Based Public Health Interventions on Health-Related Quality of Life in Older People: A Comparative Study" International Journal of Environmental Research and Public Health 22, no. 10: 1588. https://doi.org/10.3390/ijerph22101588
APA StyleJuraga, D., Rukavina, T., Glavić, M. M., Roviš, D., Racz, A., Bilajac, L., Antonić, M., Raat, H., & Vasiljev, V. (2025). Impact of Face-to-Face and Online Mindfulness-Based Public Health Interventions on Health-Related Quality of Life in Older People: A Comparative Study. International Journal of Environmental Research and Public Health, 22(10), 1588. https://doi.org/10.3390/ijerph22101588








