Bayesian Network Modeling of Environmental, Social, and Behavioral Determinants of Cardiovascular Disease Risk
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Database and Sample Size
2.2.1. Measurement of Key Variables
Cardiovascular Biomarkers (Outcome Variables)
Health Predictors
Environmental Exposure Biomarkers
Lifestyle, Socioeconomic and Demographic Covariates
2.3. Inclusion and Exclusion Criteria
2.4. Statistical Techniques
2.4.1. Descriptive Statistics
2.4.2. Spearman Correlation Analysis
2.4.3. Bayesian Network Model
- Structure of a Bayesian Network
- B represents the Bayesian Network.
- G is a Directed Acyclic Graph (DAG), where nodes (X1, X2, …, Xn) represent random variables, and directed edges between them signify dependencies.
- Θ are the set parameters that define the conditional probability distributions governing these variables.
- Mathematical Representation of a Bayesian Network
3. Results
3.1. Descriptive Analysis of Cardiovascular and Metabolic Health Indicators
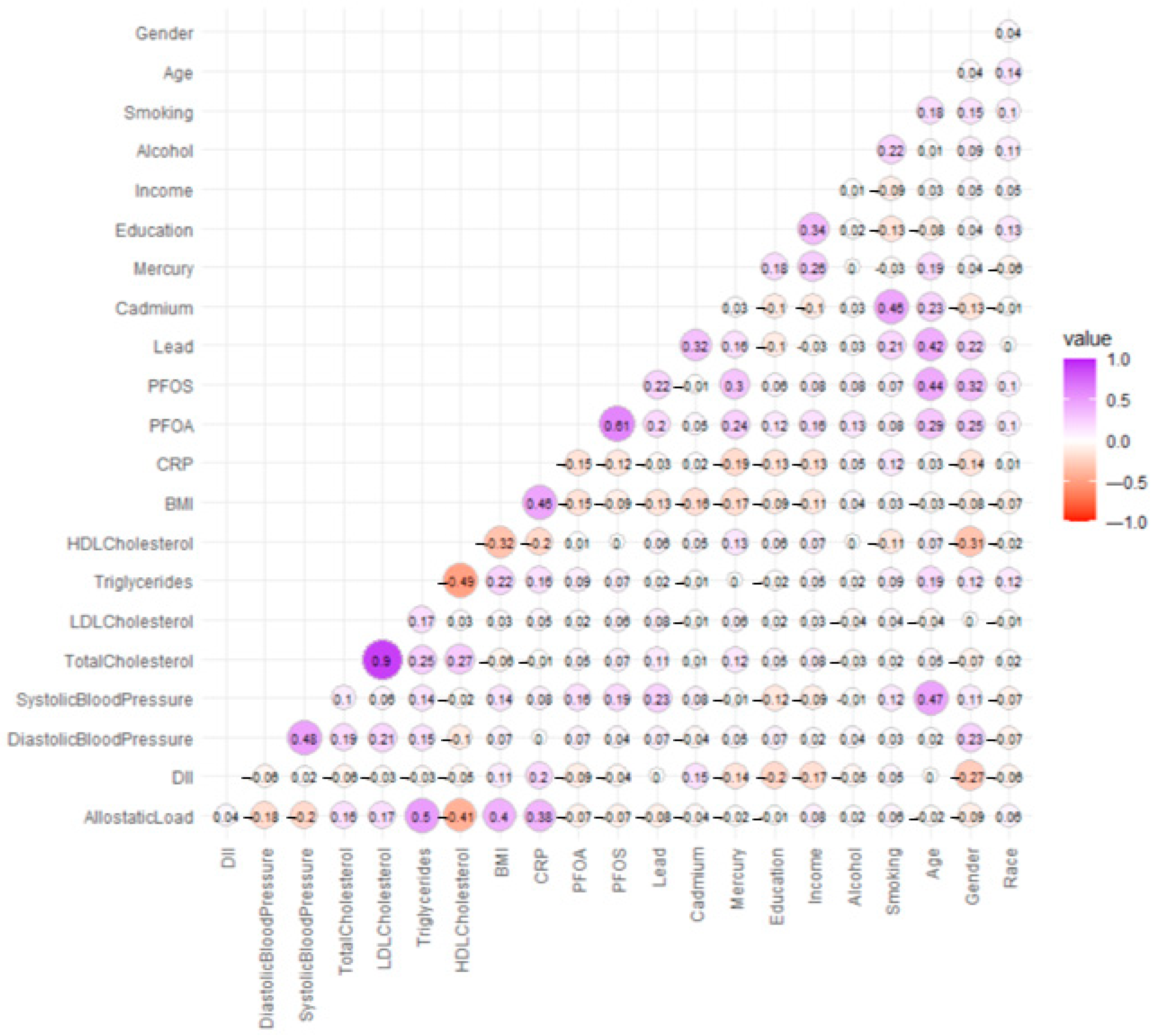
3.2. Spearman Correlation Results
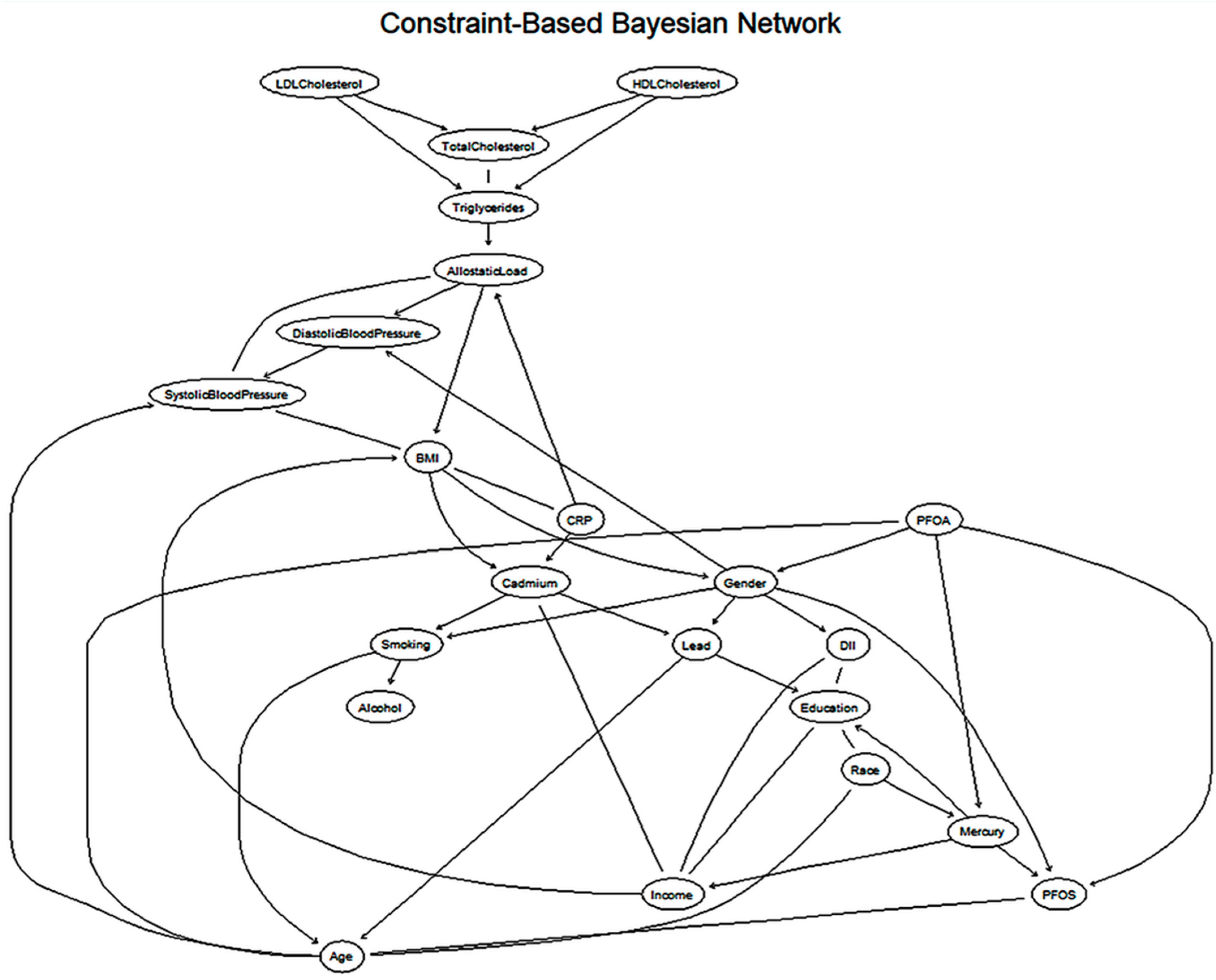
3.3. Bayesian Network Learning Using the Grow-Shrink Algorithm
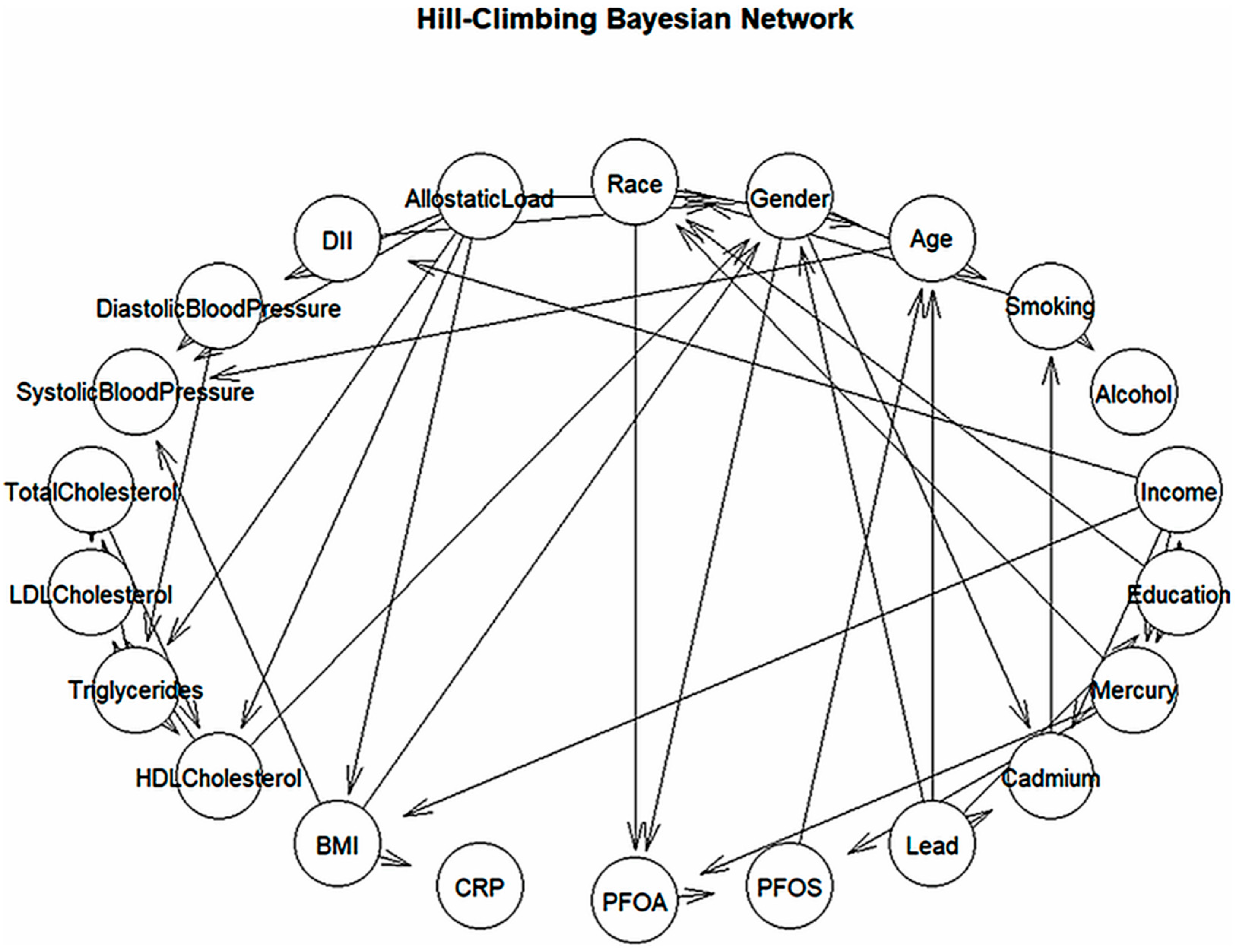
3.4. Bayesian Network Learning Using the Hill-Climbing Algorithm
3.5. Cardiovascular Network Structure from Grow-Shrink Bayesian Model
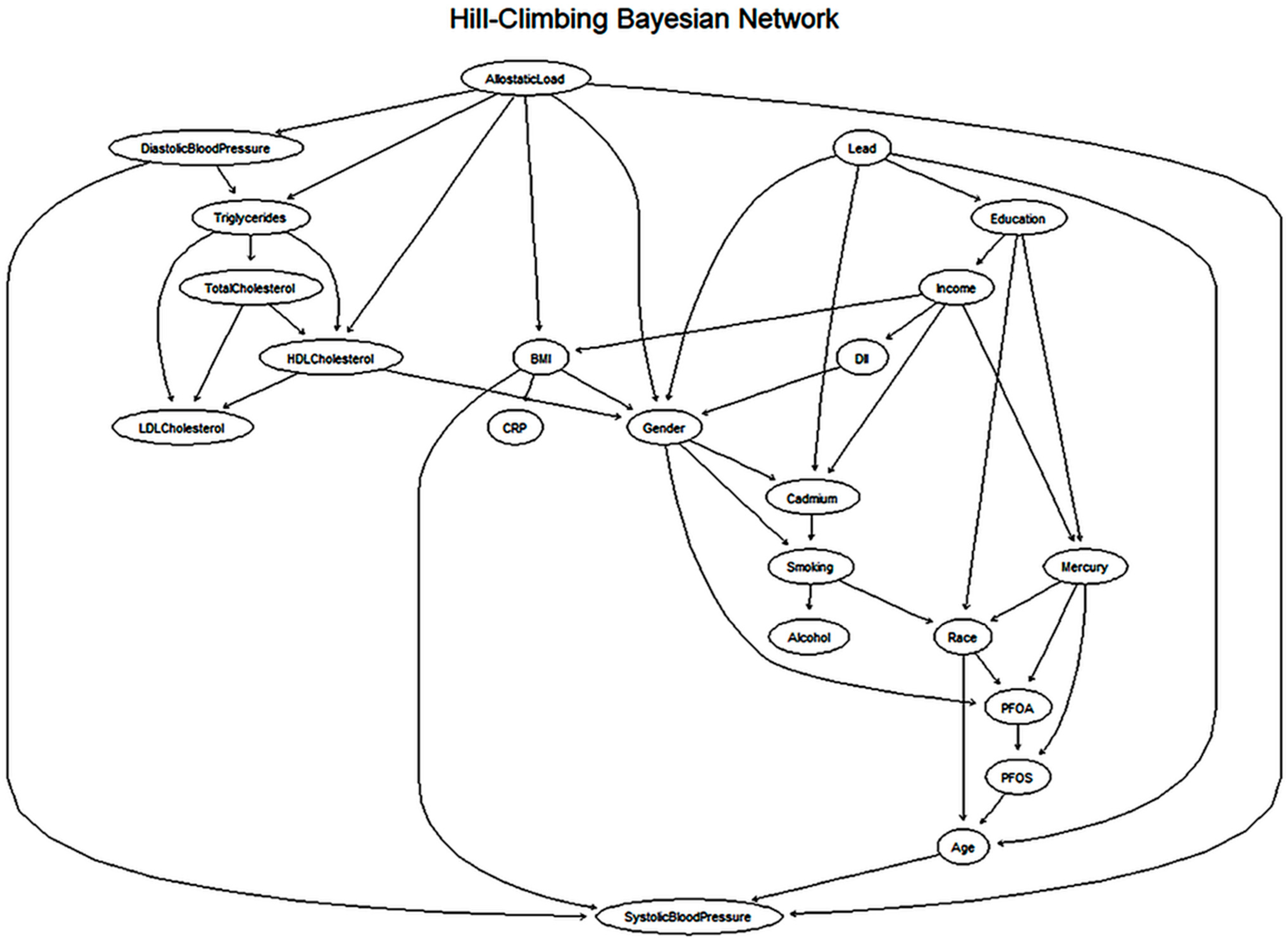
3.6. Cardiovascular Network Structure from Hill-Climbing Bayesian Model
3.7. Hierarchical Visualization of Constraint-Based Cardiovascular Network
3.8. Hierarchical Visualization of Score-Based Cardiovascular Network
4. Discussion
4.1. Overview of Key Findings
4.2. Interpretation of Descriptive and Correlational Results
4.3. Network Analysis Insights
4.3.1. Constraint-Based (Grow-Shrink) Network
4.3.2. Score-Based (Hill-Climbing) Network
4.3.3. Strengths of the Network Analysis
4.4. Comparing Algorithms and Network Structures
4.5. Social and Environmental Determinants of Health
4.6. Public Health and Policy Implications
4.7. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N. Heart disease and stroke statistics—2021 update: A report from the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef]
- Roth, G.A.; Forouzanfar, M.H.; Moran, A.E.; Barber, R.; Nguyen, G.; Feigin, V.L.; Naghavi, M.; Mensah, G.A.; Murray, C.J.L. Demographic and Epidemiologic Drivers of Global Cardiovascular Mortality. N. Engl. J. Med. 2015, 372, 1333–1341. [Google Scholar] [CrossRef]
- Global Burden of Cardiovascular Diseases Collaboration; Roth, G.A.; Johnson, C.O.; Abate, K.H.; Abd-Allah, F.; Ahmed, M.; Alam, K.; Alam, T.; Alvis-Guzman, N.; Ansari, H.; et al. The Burden of Cardiovascular Diseases Among US States, 1990–2016. JAMA Cardiol. 2018, 3, 375–389. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, S.; Hawken, S.; Ôunpuu, S.; Dans, T.; Avezum, A.; Lanas, F.; McQueen, M.; Budaj, A.; Pais, P.; Varigos, J. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet 2004, 364, 937–952. [Google Scholar] [CrossRef] [PubMed]
- Houston, M.C. The role of mercury and cadmium heavy metals in vascular disease, hypertension, coronary heart disease, and myocardial infarction. Altern. Ther. Health Med. 2007, 13, S128–S133. [Google Scholar]
- Lamas, G.A.; Bhatnagar, A.; Jones, M.R.; Mann, K.K.; Nasir, K.; Tellez-Plaza, M.; Ujueta, F.; Navas-Acien, A.; American Heart Association Council on Epidemiology and Prevention; Council on Cardiovascular and Stroke Nursing; et al. Prevention Contaminant metals as cardiovascular risk factors: A scientific statement from the American Heart Association. J. Am. Heart Assoc. 2023, 12, e029852. [Google Scholar] [CrossRef] [PubMed]
- Ozarde, Y.; Purandare, D.; Deshmukh, S.; Gadhave, R. Heavy metals and cardiovascular health: Uncovering links and health challenges. J. Trace Elem. Med. Biol. 2025, 89, 127648. [Google Scholar] [CrossRef]
- Tellez-Plaza, M.; Navas-Acien, A.; Crainiceanu, C.M.; Guallar, E. Cadmium exposure and hypertension in the 1999–2004 National Health and Nutrition Examination Survey (NHANES). Environ. Health Perspect. 2008, 116, 51–56. [Google Scholar] [CrossRef]
- Pan, Z.; Gong, T.; Liang, P. Heavy metal exposure and cardiovascular disease. Circ. Res. 2024, 134, 1160–1178. [Google Scholar] [CrossRef]
- Steenland, K.; Fletcher, T.; Savitz, D.A. Epidemiologic evidence on the health effects of perfluorooctanoic acid (PFOA). Environ. Health Perspect. 2010, 118, 1100–1108. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Appel, L.J.; Van Horn, L. Components of a cardioprotective diet: New insights. Circulation 2011, 123, 2870–2891. [Google Scholar] [CrossRef]
- Münzel, T.; Daiber, A. Environmental stressors and their impact on health and disease with focus on oxidative stress. Antioxid. Redox Signal. 2018, 28, 735–740. [Google Scholar] [CrossRef]
- McEwen, B.S. Protective and damaging effects of stress mediators. N. Engl. J. Med. 1998, 338, 171–179. [Google Scholar] [CrossRef]
- Guidi, J.; Lucente, M.; Sonino, N.; Fava, G.A. Allostatic load and its impact on health: A systematic review. Psychother. Psychosom. 2020, 90, 11–27. [Google Scholar] [CrossRef] [PubMed]
- Havranek, E.P.; Mujahid, M.S.; Barr, D.A.; Blair, I.V.; Cohen, M.S.; Cruz-Flores, S.; Davey-Smith, G.; Dennison-Himmelfarb, C.R.; Lauer, M.S.; Lockwood, D.W. Social determinants of risk and outcomes for cardiovascular disease: A scientific statement from the American Heart Association. Circulation 2015, 132, 873–898. [Google Scholar] [CrossRef]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef]
- Braveman, P.; Gottlieb, L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 2014, 129, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Schulz, A.J.; Mentz, G.; Lachance, L.; Johnson, J.; Gaines, C.; Israel, B.A. Associations between socioeconomic status and allostatic load: Effects of neighborhood poverty and tests of mediating pathways. Am. J. Public Health 2012, 102, 1706–1714. [Google Scholar] [CrossRef]
- Kyrimi, E.; McLachlan, S.; Dube, K.; Neves, M.R.; Fahmi, A.; Fenton, N. A comprehensive scoping review of Bayesian networks in healthcare: Past, present and future. Artif. Intell. Med. 2021, 117, 102108. [Google Scholar] [CrossRef] [PubMed]
- Ordovás, J.M.; Rios-Insua, D.; Santos-Lozano, A.; Lucia, A.; Torres, A.; Kosgodagan, A.; Camacho, J.M. A Bayesian network model for predicting cardiovascular risk. Comput. Methods Programs Biomed. 2023, 231, 107405. [Google Scholar] [CrossRef]
- Chen, G.; O’Malley, A.J. Bayesian hierarchical network autocorrelation models for estimating direct and indirect effects of peer hospitals on outcomes of hospitalized patients. Appl. Netw. Sci. 2024, 9, 24. [Google Scholar] [CrossRef]
- Flores, M.J.; Nicholson, A.E.; Brunskill, A.; Korb, K.B.; Mascaro, S. Incorporating expert knowledge when learning Bayesian network structure: A medical case study. Artif. Intell. Med. 2011, 53, 181–204. [Google Scholar] [CrossRef]
- Arora, P.; Boyne, D.; Slater, J.J.; Gupta, A.; Brenner, D.R.; Druzdzel, M.J. Bayesian networks for risk prediction using real-world data: A tool for precision medicine. Value Health 2019, 22, 439–445. [Google Scholar] [CrossRef]
- Albert, M.A.; Glynn, R.J.; Buring, J.; Ridker, P.M. Impact of traditional and novel risk factors on the relationship between socioeconomic status and incident cardiovascular events. Circulation 2006, 114, 2619–2626. [Google Scholar] [CrossRef] [PubMed]
- Al-Kindi, S.G.; Brook, R.D.; Biswal, S.; Rajagopalan, S. Environmental determinants of cardiovascular disease: Lessons learned from air pollution. Nat. Rev. Cardiol. 2020, 17, 656–672. [Google Scholar] [CrossRef] [PubMed]
- Zabinski, J. Advancing Environmental Human Health Risk Assessment Through Bayesian Network Analysis. Ph.D. Thesis, The University of North Carolina at Chapel Hill, Chapel Hill, NC, USA, 2017. [Google Scholar] [CrossRef]
- Psaltopoulou, T.; Hatzis, G.; Papageorgiou, N.; Androulakis, E.; Briasoulis, A.; Tousoulis, D. Socioeconomic status and risk factors for cardiovascular disease: Impact of dietary mediators. Hell. J. Cardiol. 2017, 58, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Marmot, M. The role of psychobiological pathways in socio-economic inequalities in cardiovascular disease risk. Eur. Heart J. 2002, 23, 13–25. [Google Scholar] [CrossRef]
- Kershaw, K.N.; Mezuk, B.; Abdou, C.M.; Rafferty, J.A.; Jackson, J.S. Socioeconomic position, health behaviors, and C-reactive protein: A moderated-mediation analysis. Health Psychol. 2010, 29, 307. [Google Scholar] [CrossRef]
- Javed, Z.; Haisum Maqsood, M.; Yahya, T.; Amin, Z.; Acquah, I.; Valero-Elizondo, J.; Andrieni, J.; Dubey, P.; Jackson, R.K.; Daffin, M.A. Race, racism, and cardiovascular health: Applying a social determinants of health framework to racial/ethnic disparities in cardiovascular disease. Circ. Cardiovasc. Qual. Outcomes 2022, 15, e007917. [Google Scholar] [CrossRef] [PubMed]
- Powell-Wiley, T.M.; Baumer, Y.; Baah, F.O.; Baez, A.S.; Farmer, N.; Mahlobo, C.T.; Pita, M.A.; Potharaju, K.A.; Tamura, K.; Wallen, G.R. Social determinants of cardiovascular disease. Circ. Res. 2022, 130, 782–799. [Google Scholar] [CrossRef]
- Baek, S.-U.; Yoon, J.-H. Systemic Inflammation Across Metabolic Obesity Phenotypes: A Cross-Sectional Study of Korean Adults Using High-Sensitivity C-Reactive Protein as a Biomarker. Int. J. Mol. Sci. 2024, 25, 11540. [Google Scholar] [CrossRef]
- Wilson, P.W.; Grundy, S.M. The metabolic syndrome: Practical guide to origins and treatment: Part I. Circulation 2003, 108, 1422–1424. [Google Scholar] [CrossRef]
- Girona, J.; Amigó, N.; Ibarretxe, D.; Plana, N.; Rodríguez-Borjabad, C.; Heras, M.; Ferré, R.; Gil, M.; Correig, X.; Masana, L. HDL triglycerides: A new marker of metabolic and cardiovascular risk. Int. J. Mol. Sci. 2019, 20, 3151. [Google Scholar] [CrossRef]
- Mourad, B.H.; El-Sherif, G.H. Exploring the Link Between the Serum/Blood Levels of Heavy Metals (Pb, As, Cd, and Cu) and 2 Novel Biomarkers of Cardiovascular Stress (Growth Differentiation Factor 15 and Soluble Suppression of Tumorigenicity 2) in Copper Smelter Workers. J. Occup. Environ. Med. 2022, 64, 976–984. [Google Scholar] [CrossRef] [PubMed]
- Navas-Acien, A.; Guallar, E.; Silbergeld, E.K.; Rothenberg, S.J. Lead exposure and cardiovascular disease—A systematic review. Environ. Health Perspect. 2007, 115, 472–482. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, P.; Lemieux, I.; Després, J.P. Obesity, inflammation, and cardiovascular risk. Clin. Pharmacol. Ther. 2010, 87, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Kivimäki, M.; Bartolomucci, A.; Kawachi, I. The multiple roles of life stress in metabolic disorders. Nat. Rev. Endocrinol. 2023, 19, 10–27. [Google Scholar] [CrossRef]
- Shim, J.-S.; Song, B.M.; Lee, J.H.; Lee, S.W.; Park, J.H.; Choi, D.P.; Lee, M.H.; Ha, K.H.; Kim, D.J.; Park, S. Cardiovascular and Metabolic Diseases Etiology Research Center (CMERC) cohort: Study protocol and results of the first 3 years of enrollment. Epidemiol. Health 2017, 39, e2017016. [Google Scholar] [CrossRef]
- Peters, J.L.; Fabian, M.P.; Levy, J.I. Combined impact of lead, cadmium, polychlorinated biphenyls and non-chemical risk factors on blood pressure in NHANES. Environ. Res. 2014, 132, 93–99. [Google Scholar] [CrossRef]
- O’Neil, A.; Shivappa, N.; Jacka, F.N.; Kotowicz, M.A.; Kibbey, K.; Hebert, J.R.; Pasco, J.A. Pro-inflammatory dietary intake as a risk factor for CVD in men: A 5-year longitudinal study. Br. J. Nutr. 2015, 114, 2074–2082. [Google Scholar] [CrossRef]
- Waddell, T.H. Applying Bayesian-networks to Model Multi-Organ Pathologies. Ph.D. Thesis, University of Oxford, Oxford, UK, 2023. [Google Scholar] [CrossRef]
- Xu, S.; Thompson, W.; Kerr, J.; Godbole, S.; Sears, D.D.; Patterson, R.; Natarajan, L. Modeling interrelationships between health behaviors in overweight breast cancer survivors: Applying Bayesian networks. PLoS ONE 2018, 13, e0202923. [Google Scholar] [CrossRef] [PubMed]
- Gasse, M.; Aussem, A.; Elghazel, H. A hybrid algorithm for Bayesian network structure learning with application to multi-label learning. Expert Syst. Appl. 2014, 41, 6755–6772. [Google Scholar] [CrossRef]
- Pudrovska, T. Early-life socioeconomic status and mortality at three life course stages: An increasing within-cohort inequality. J. Health Soc. Behav. 2014, 55, 181–195. [Google Scholar] [CrossRef]
- Phelan, J.C.; Link, B.G.; Diez-Roux, A.; Kawachi, I.; Levin, B. “Fundamental causes” of social inequalities in mortality: A test of the theory. J. Health Soc. Behav. 2004, 45, 265–285. [Google Scholar] [CrossRef] [PubMed]
- Crimmins, E.M.; Kim, J.K.; Seeman, T.E. Poverty and biological risk: The earlier “aging” of the poor. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2009, 64, 286–292. [Google Scholar] [CrossRef]
- Colombo, D.; Maathuis, M.H. Order-independent constraint-based causal structure learning. J. Mach. Learn. Res. 2014, 15, 3741–3782. [Google Scholar] [CrossRef]
- Aussem, A.; Tchernof, A.; de Morais, S.R.; Rome, S. Analysis of lifestyle and metabolic predictors of visceral obesity with Bayesian Networks. BMC Bioinform. 2010, 11, 487. [Google Scholar] [CrossRef]
- Xie, J.; Liu, Y.; Zeng, X.; Zhang, W.; Mei, Z. A Bayesian network model for predicting type 2 diabetes risk based on electronic health records. Mod. Phys. Lett. B 2017, 31, 1740055. [Google Scholar] [CrossRef]
- Schulz, A.; Northridge, M.E. Social determinants of health: Implications for environmental health promotion. Health Educ. Behav. 2004, 31, 455–471. [Google Scholar] [CrossRef]
- Suglia, S.F.; Appleton, A.A.; Bleil, M.E.; Campo, R.A.; Dube, S.R.; Fagundes, C.P.; Heard-Garris, N.J.; Johnson, S.B.; Slopen, N.; Stoney, C.M. Timing, duration, and differential susceptibility to early life adversities and cardiovascular disease risk across the lifespan: Implications for future research. Prev. Med. 2021, 153, 106736. [Google Scholar] [CrossRef]
- Jilani, M.H.; Javed, Z.; Yahya, T.; Valero-Elizondo, J.; Khan, S.U.; Kash, B.; Blankstein, R.; Virani, S.S.; Blaha, M.J.; Dubey, P.; et al. Social determinants of health and cardiovascular disease: Current state and future directions towards healthcare equity. Curr. Atheroscler. Rep. 2021, 23, 55. [Google Scholar] [CrossRef] [PubMed]
- Homa, D.M.; Neff, L.J.; King, B.A.; Caraballo, R.S.; Bunnell, R.E.; Babb, S.D.; Garrett, B.E.; Sosnoff, C.S.; Wang, L.; Control, C.f.D.; et al. Vital signs: Disparities in nonsmokers’ exposure to secondhand smoke—United States, 1999–2012. MMWR Morb Mortal Weekly Rep. 2015, 64, 103–108. [Google Scholar]
- Raghuveer, G.; White, D.A.; Hayman, L.L.; Woo, J.G.; Villafane, J.; Celermajer, D.; Ward, K.D.; De Ferranti, S.D.; Zachariah, J. Cardiovascular consequences of childhood secondhand tobacco smoke exposure: Prevailing evidence, burden, and racial and socioeconomic disparities: A scientific statement from the American Heart Association. Circulation 2016, 134, e336–e359. [Google Scholar] [CrossRef]
- Rodin, A.S.; Gogoshin, G.; Litvinenko, A.; Boerwinkle, E. Exploring genetic epidemiology data with Bayesian networks. In Handbook of Statistics; Elsevier: Amsterdam, The Netherlands, 2012; Volume 28, pp. 479–510. [Google Scholar] [CrossRef]
- Hartmann, M. Modelling Risk Factors for Aetiologically Complex Diseases with BAYESIAN Networks. Ph.D. Thesis, Queen Mary University of London, London, UK, 2023. [Google Scholar]
- Dolcini, J.; Landi, R.; Ponzio, E.; Picchini, L.; Luciani, A.; Formenti, L.; Svegliati Baroni, S.; Gabrielli, A.; D’Errico, M.M.; Barbadoro, P. Association between TNF-α, cortisol levels, and exposure to PM10 and PM2.5: A pilot study. Environ. Sci. Eur. 2024, 36, 141. [Google Scholar] [CrossRef]

| Variable Type | Variables | Description |
|---|---|---|
| Outcome Variables | Diastolic Blood Pressure, Systolic Blood Pressure, Total Cholesterol, LDL Cholesterol, Triglycerides, HDL Cholesterol | Key cardiovascular health indicators |
| Health Predictors | Allostatic Load, Dietary Inflammatory Index (DII), body mass index (BMI), C-reactive protein (CRP) | Measures of stress, inflammation, and metabolic health |
| Environmental Predictors | PFOA, PFOS, Lead, Cadmium, Mercury | Exposure to toxic substances |
| Lifestyle Predictors | Alcohol, Smoking | Behavioral risk factors |
| Socioeconomic Predictors | Education, Income | Social determinants of health |
| Demographic Predictors | Age, Gender, Race |
| Variable | 25th Percentile | Median | Mean | 75th Percentile |
|---|---|---|---|---|
| Allostatic Load | 3.00 | 3.00 | 3.59 | 5.00 |
| DII (Dietary Inflammation Index) | 0.35 | 1.64 | 1.49 | 2.74 |
| Diastolic Blood Pressure | 64.67 | 72.67 | 72.67 | 79.33 |
| Systolic Blood Pressure | 112.67 | 123.33 | 125.96 | 136.67 |
| Total Cholesterol | 155.00 | 182.00 | 185.10 | 209.00 |
| LDL Cholesterol | 85.00 | 106.00 | 109.90 | 129.00 |
| Triglycerides | 59.00 | 89.00 | 104.40 | 130.00 |
| HDL Cholesterol | 42.00 | 51.00 | 54.39 | 62.00 |
| BMI | 24.50 | 28.20 | 29.81 | 34.00 |
| CRP | 0.80 | 1.79 | 4.43 | 6.09 |
| Parameter | Value | Explanation |
|---|---|---|
| Nodes | 22 | Number of variables (e.g., BMI, Blood Pressure, etc.) in the model |
| Total arcs | 44 | Total number of edges (connections) in the network |
| Directed Arcs | 32 | Edges with a defined direction, suggesting potential causal influence |
| Undirected Arcs | 12 | Edges with no assigned direction, indicating potential association only |
| Average Markov Blanket Size | 5.00 | Average number of variables in each node’s Markov blanket |
| Average Neighborhood Size | 4.00 | Average number of adjacent (connected) nodes per variable |
| Average Branching Factor | 1.45 | Average number of outgoing edges per node |
| Conditional Independence Test | Pearson’s Correlation | Statistical test used to check if two variables are related |
| Alpha Threshold | 0.05 | Significance level used in independence testing |
| Tests Used in Procedure | 3917 | Total number of statistical tests conducted during network structure learning |
| Parameter | Value | Explanation |
|---|---|---|
| Nodes | 22 | Total number of variables included in the network |
| Total Arcs | 44 | Number of edges (relationships) identified between variables |
| Directed Arcs | 44 | All arcs have assigned direction, indicating potential causal influence |
| Undirected Arcs | 0 | No undirected arcs present in the final model |
| Average Markov Blanket Size | 6.09 | Average number of variables in each node’s Markov blanket |
| Average Neighborhood Size | 4.00 | Average number of directly connected neighbors per variable |
| Average Branching Factor | 2.00 | Average number of outgoing arcs per node |
| Scoring Function | Bayesian Gaussian (BGe) | Scoring metric used to evaluate model fit |
| Imaginary Sample Size (Normal) | 1 | Prior parameter controlling strength of the normal component |
| Imaginary Sample Size (Wishart) | 4 | Prior parameter for the Wishart distribution in the BGe score |
| Test used in procedure | 1281 | Total number of model comparisons evaluated during structure learning |
| Optimized | True | Indicates the algorithm successfully identified a high-scoring network model |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nyavor, H.; Obeng-Gyasi, E. Bayesian Network Modeling of Environmental, Social, and Behavioral Determinants of Cardiovascular Disease Risk. Int. J. Environ. Res. Public Health 2025, 22, 1551. https://doi.org/10.3390/ijerph22101551
Nyavor H, Obeng-Gyasi E. Bayesian Network Modeling of Environmental, Social, and Behavioral Determinants of Cardiovascular Disease Risk. International Journal of Environmental Research and Public Health. 2025; 22(10):1551. https://doi.org/10.3390/ijerph22101551
Chicago/Turabian StyleNyavor, Hope, and Emmanuel Obeng-Gyasi. 2025. "Bayesian Network Modeling of Environmental, Social, and Behavioral Determinants of Cardiovascular Disease Risk" International Journal of Environmental Research and Public Health 22, no. 10: 1551. https://doi.org/10.3390/ijerph22101551
APA StyleNyavor, H., & Obeng-Gyasi, E. (2025). Bayesian Network Modeling of Environmental, Social, and Behavioral Determinants of Cardiovascular Disease Risk. International Journal of Environmental Research and Public Health, 22(10), 1551. https://doi.org/10.3390/ijerph22101551







