Associations Between Walking in the Third Trimester of Pregnancy and Maternal Mental Health During the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. Walking Levels
2.2.2. Prenatal Maternal Mental Health Symptoms
2.2.3. Covariates
2.3. Statistical Analysis
3. Results
3.1. Descriptive Statistics
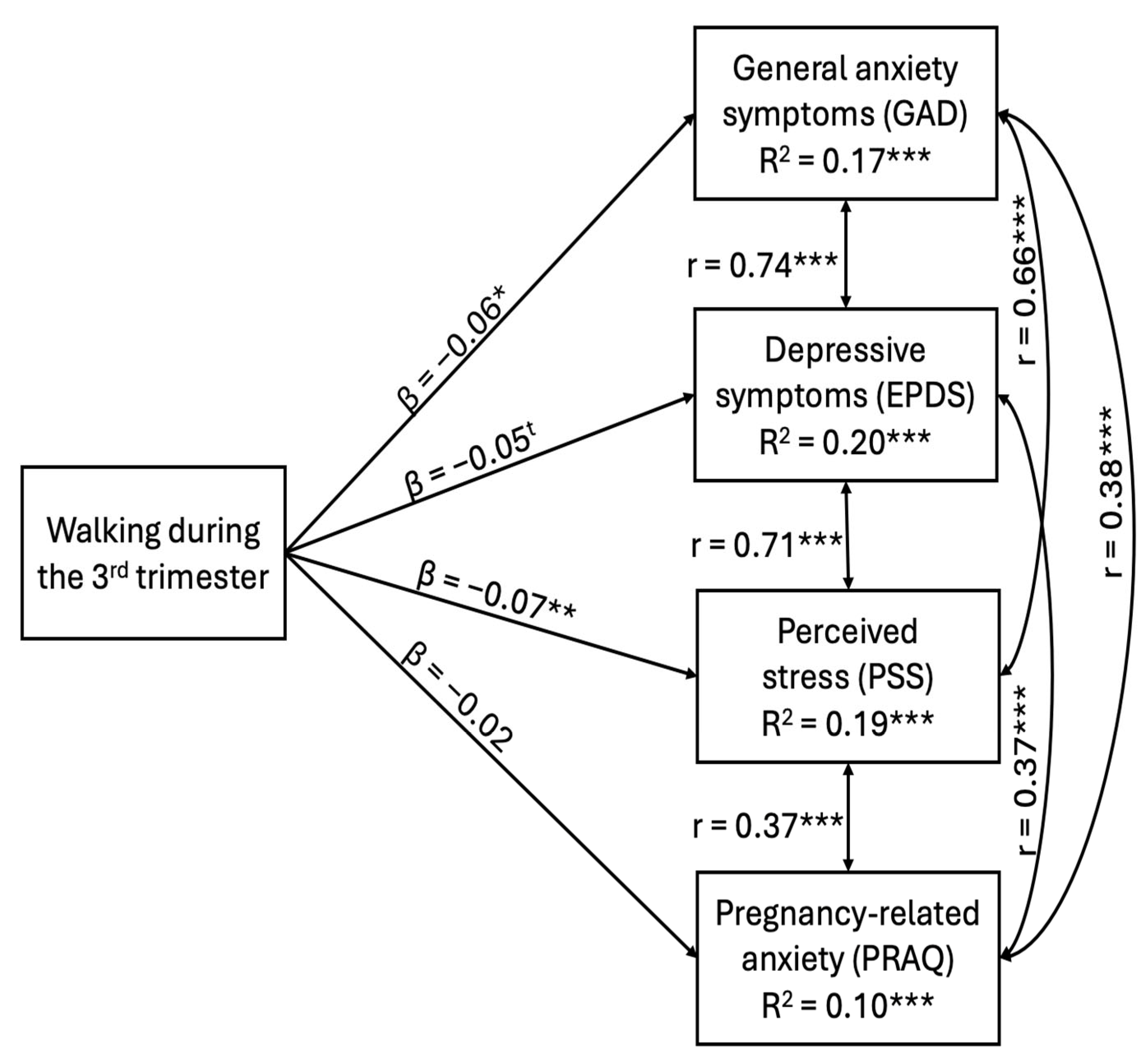
3.2. Associations Between Walking Levels and Maternal Mental Health Symptoms
3.3. Factors Associated with Walking Levels
4. Discussion
4.1. Associations Between Walking Levels and Maternal Mental Health
4.2. Factors Associated with Walking Levels During the Third Trimester
4.3. Strengths, Limitations and Research Perspectives
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cook, J.L.; Shea, A.K.; St-André, M. Perinatal Mental Illness: We Need to Act Now. Together. J. Obstet. Gynaecol. Can. 2023, 45, 4–5. [Google Scholar] [CrossRef]
- Schwab, M.; Rakers, F. Long-Term Effects of Prenatal Maternal Stress and Mental Health. In Developmental Origins of Health and Disease; Godfrey, K.M., Poston, L., Hanson, M.A., Gluckman, P.D., Eds.; Cambridge University Press: Cambridge, UK, 2022; pp. 46–55. [Google Scholar] [CrossRef]
- Howard, L.M.; Khalifeh, H. Perinatal Mental Health: A Review of Progress and Challenges. World Psychiatry 2020, 19, 313–327. [Google Scholar] [CrossRef]
- Gelaye, B.; Rondon, M.; Araya, R.; Williams, M.A. Epidemiology of Maternal Depression, Risk Factors, and Child Outcomes in Low-Income and Middle-Income Countries. Lancet Psychiatry 2016, 3, 973–982. [Google Scholar] [CrossRef]
- Delanerolle, G.; McCauley, M.; Hirsch, M.; Zeng, Y.; Cong, X.; Cavalini, H.; Sajid, S.; Shetty, A.; Rathod, S.; Shi, J.Q.; et al. The Prevalence of Mental Ill-Health in Women during Pregnancy and after Childbirth during the Covid-19 Pandemic: A Systematic Review and Meta-Analysis. BMC Pregnancy Childbirth 2023, 23, 76. [Google Scholar] [CrossRef] [PubMed]
- Tomfohr-Madsen, L.M.; Racine, N.; Giesbrecht, G.F.; Lebel, C.; Madigan, S. Depression and Anxiety in Pregnancy during COVID-19: A Rapid Review and Meta-Analysis. Psychiatry Res. 2021, 300, 113912. [Google Scholar] [CrossRef] [PubMed]
- Berthelot, N.; Lemieux, R.; Garon-Bissonnette, J.; Drouin-Maziade, C.; Martel, É.; Maziade, M. Uptrend in Distress and Psychiatric Symptomatology in Pregnant Women during the Coronavirus Disease 2019 Pandemic. Acta Obstet. Gynecol. Scand. 2020, 99, 848–855. [Google Scholar] [CrossRef] [PubMed]
- Lebel, C.; MacKinnon, A.; Bagshawe, M.; Tomfohr-Madsen, L.; Giesbrecht, G. Elevated Depression and Anxiety Symptoms among Pregnant Individuals during the COVID-19 Pandemic. J. Affect. Disord. 2020, 277, 5–13. [Google Scholar] [CrossRef]
- Zhang, C.X.W.; Okeke, J.C.; Levitan, R.D.; Murphy, K.E.; Foshay, K.; Lye, S.J.; Knight, J.A.; Matthews, S.G. Evaluating Depression and Anxiety throughout Pregnancy and after Birth: Impact of the COVID-19 Pandemic. Am. J. Obstet. Gynecol. MFM 2022, 4, 100605. [Google Scholar] [CrossRef]
- Coussons-Read, M.E. Effects of Prenatal Stress on Pregnancy and Human Development: Mechanisms and Pathways. Obstet. Med. 2013, 6, 52–57. [Google Scholar] [CrossRef]
- Huizink, A.C.; Delforterie, M.J.; Scheinin, N.M.; Tolvanen, M.; Karlsson, L.; Karlsson, H. Adaption of Pregnancy Anxiety Questionnaire–Revised for All Pregnant Women Regardless of Parity: PRAQ-R2. Arch. Womens Ment. Health 2016, 19, 125–132. [Google Scholar] [CrossRef]
- Reck, C.; Zimmer, K.; Dubber, S.; Zipser, B.; Schlehe, B.; Gawlik, S. The Influence of General Anxiety and Childbirth-Specific Anxiety on Birth Outcome. Arch. Womens Ment. Health 2013, 16, 363–369. [Google Scholar] [CrossRef]
- Van Den Bergh, B.R.H.; Van Den Heuvel, M.I.; Lahti, M.; Braeken, M.; De Rooij, S.R.; Entringer, S.; Hoyer, D.; Roseboom, T.; Räikkönen, K.; King, S.; et al. Prenatal Developmental Origins of Behavior and Mental Health: The Influence of Maternal Stress in Pregnancy. Neurosci. Biobehav. Rev. 2020, 117, 26–64. [Google Scholar] [CrossRef]
- Tripathy, P. A Public Health Approach to Perinatal Mental Health: Improving Health and Wellbeing of Mothers and Babies. J. Gynecol. Obstet. Hum. Reprod. 2020, 49, 101747. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Perinatal Mental Health. Available online: https://www.who.int/teams/mental-health-and-substance-use/promotion-prevention/maternal-mental-health (accessed on 30 September 2025).
- Cai, C.; Busch, S.; Wang, R.; Sivak, A.; Davenport, M.H. Physical Activity before and during Pregnancy and Maternal Mental Health: A Systematic Review and Meta-Analysis of Observational Studies. J. Affect. Disord. 2022, 309, 393–403. [Google Scholar] [CrossRef]
- Davenport, M.H.; McCurdy, A.P.; Mottola, M.F.; Skow, R.J.; Meah, V.L.; Poitras, V.J.; Jaramillo Garcia, A.; Gray, C.E.; Barrowman, N.; Riske, L.; et al. Impact of Prenatal Exercise on Both Prenatal and Postnatal Anxiety and Depressive Symptoms: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2018, 52, 1376–1385. [Google Scholar] [CrossRef]
- Davenport, M.H.; Meyer, S.; Meah, V.L.; Strynadka, M.C.; Khurana, R. Moms Are Not OK: COVID-19 and Maternal Mental Health. Front. Glob. Womens Health 2020, 1, 1. [Google Scholar] [CrossRef]
- Davenport, M.H.; Ruchat, S.-M.; Poitras, V.J.; Garcia, A.J.; Gray, C.E.; Barrowman, N.; Skow, R.J.; Meah, V.L.; Riske, L.; Sobierajski, F.; et al. Prenatal Exercise for the Prevention of Gestational Diabetes Mellitus and Hypertensive Disorders of Pregnancy: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2018, 52, 1367–1375. [Google Scholar] [CrossRef]
- Silva-Jose, C.; Sánchez-Polán, M.; Barakat, R.; Gil-Ares, J.; Refoyo, I. Level of Physical Activity in Pregnant Populations from Different Geographic Regions: A Systematic Review. J. Clin. Med. 2022, 11, 4638. [Google Scholar] [CrossRef]
- Srugo, S.A.; Fernandes da Silva, D.; Menard, L.M.; Shukla, N.; Lang, J.J. Recent Patterns of Physical Activity and Sedentary Behaviour Among Pregnant Adults in Canada. J. Obstet. Gynaecol. Can. 2023, 45, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, S.L.; Surita, F.G.; Godoy, A.C.; Kasawara, K.T.; Morais, S.S. Physical Activity Patterns and Factors Related to Exercise during Pregnancy: A Cross Sectional Study. PLoS ONE 2015, 10, e0128953. [Google Scholar] [CrossRef]
- Santos-Rocha, R. Exercise and Physical Activity During Pregnancy and Postpartum: Evidence-Based Guidelines; Springer International Publishing AG: Cham, Switzerland, 2022. [Google Scholar]
- Connolly, C.P.; Conger, S.A.; Montoye, A.H.K.; Marshall, M.R.; Schlaff, R.A.; Badon, S.E.; Pivarnik, J.M. Walking for Health during Pregnancy: A Literature Review and Considerations for Future Research. J. Sport Health Sci. 2019, 8, 401–411. [Google Scholar] [CrossRef]
- Battle, C.L.; Schofield, C.A.; Kraines, M.A.; Abrantes, A.M. Acceptability, Feasibility, and Preliminary Efficacy of a Prenatal Walking Program for Depressed Pregnant Women. J. Affect. Disord. Rep. 2023, 12, 100513. [Google Scholar] [CrossRef]
- Petrovic, D.; Perovic, M.; Lazovic, B.; Pantic, I. Association between Walking, Dysphoric Mood and Anxiety in Late Pregnancy: A Cross-Sectional Study. Psychiatry Res. 2016, 246, 360–363. [Google Scholar] [CrossRef]
- Atkinson, L.; De Vivo, M.; Hayes, L.; Hesketh, K.R.; Mills, H.; Newham, J.J.; Olander, E.K.; Smith, D.M. Encouraging Physical Activity during and after Pregnancy in the COVID-19 Era, and Beyond. Int. J. Environ. Res. Public. Health 2020, 17, 7304. [Google Scholar] [CrossRef]
- Harrison, A.L.; Taylor, N.F.; Shields, N.; Frawley, H.C. Attitudes, Barriers and Enablers to Physical Activity in Pregnant Women: A Systematic Review. J. Physiother. 2018, 64, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Boden, M.; Zimmerman, L.; Azevedo, K.J.; Ruzek, J.I.; Gala, S.; Abdel Magid, H.S.; Cohen, N.; Walser, R.; Mahtani, N.D.; Hoggatt, K.J.; et al. Addressing the Mental Health Impact of COVID-19 through Population Health. Clin. Psychol. Rev. 2021, 85, 102006. [Google Scholar] [CrossRef]
- Environmental Protection Agency (EPA). National Walkability Index: Methodology and User Guide; 2021, United States. Available online: https://www.epa.gov/sites/default/files/2021-06/documents/national_walkability_index_methodology_and_user_guide_june2021.pdf (accessed on 6 June 2025).
- Conway, K.S.; Menclova, A.K. You’ll Never Walk Alone—The Effects of Walkability on Pregnancy Behaviors and Outcomes. Econ. Hum. Biol. 2023, 50, 101269. [Google Scholar] [CrossRef] [PubMed]
- Institut National de Santé Publique du Québec. Ligne du temps COVID-19 au Québec|INSPQ. Available online: https://www.inspq.qc.ca/covid-19/donnees/ligne-du-temps (accessed on 29 January 2025).
- Cohen, T.; Plourde, H.; Koski, K. Use of the Pregnancy Physical Activity Questionnaire (PPAQ) to Identify Behaviors Associated With Appropriate Gestational Weight Gain During Pregnancy. J. Phys. Act. Health 2013, 10, 1000–1007. [Google Scholar] [CrossRef]
- Chasan-Taber, L.; Park, S.; Marcotte, R.T.; Staudenmayer, J.; Strath, S.; Freedson, P. Update and Novel Validation of a Pregnancy Physical Activity Questionnaire. Am. J. Epidemiol. 2023, 192, 1743–1753. [Google Scholar] [CrossRef] [PubMed]
- Chasan-Taber, L.; Schmidt, M.D.; Roberts, D.E.; Hosmer, D.; Markenson, G.; Freedson, P.S. Development and Validation of a Pregnancy Physical Activity Questionnaire. Med. Sci. Sports Exerc. 2004, 36, 1750–1760, Erratum in Med. Sci. Sports Exerc. 2011, 43, 195. [Google Scholar] [CrossRef]
- Chandonnet, N.; Saey, D.; Alméras, N.; Marc, I. French Pregnancy Physical Activity Questionnaire Compared with an Accelerometer Cut Point to Classify Physical Activity among Pregnant Obese Women. PLoS ONE 2012, 7, e38818. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Haskell, W.L.; Herrmann, S.D.; Meckes, N.; Bassett, D.R.J.; Tudor-Locke, C.; Greer, J.L.; Vezina, J.; Whitt-Glover, M.C.; Leon, A.S. 2011 Compendium of Physical Activities: A Second Update of Codes and MET Values. Med. Sci. Sports Exerc. 2011, 43, 1575. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of Postnatal Depression. Development of the 10-Item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry J. Ment. Sci. 1987, 150, 782–786. [Google Scholar] [CrossRef] [PubMed]
- Levis, B.; Negeri, Z.; Sun, Y.; Benedetti, A.; Thombs, B.D. Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for Screening to Detect Major Depression among Pregnant and Postpartum Women: Systematic Review and Meta-Analysis of Individual Participant Data. BMJ 2020, 371, m4022. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Langille, C.; Andreou, P.; Piccinini-Vallis, H. The Prevalence of Pregnancy-Specific Perinatal Anxiety in Nova Scotia. Matern. Child Health J. 2023, 27, 1127–1132. [Google Scholar] [CrossRef]
- Cohen, S. Perceived Stress in a Probability Sample of the United States. In The Social Psychology of Health; The Claremont Symposium on Applied Social Psychology; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1988; pp. 31–67. [Google Scholar]
- State of New Hampshire Employee Assistance Program, Perceived Stress Scale Score Cut off; State of New Hampshire Employee Assistance Program: Manchester, NH, USA, 1983.
- Bert, F.; Ferrara, M.; Boietti, E.; Langiano, E.; Savatteri, A.; Scattaglia, M.; Lo Moro, G.; Leombruni, P.; De Vito, E.; Siliquini, R. Depression, Suicidal Ideation and Perceived Stress in Italian Humanities Students: A Cross-Sectional Study. Psychol. Rep. 2022, 125, 256–279. [Google Scholar] [CrossRef]
- Desrosiers, H.; Boivin, M.; Saysset, V. “Conjugal Life of the Parents, Part II—Spousal/Partner Support—What Do the Mothers Think?” In Longitudinal Study of Child Development in Québec (ÉLDEQ 1998-2002). Inst. Stat. Qué. 2000, 1, 37–58. [Google Scholar]
- Statistics Canada. 2021 Census—Boundary File [Data Set]; Statistics Canada: Ottawa, ON, USA, 2023. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 29.0; IBM Corp.: Armonk, NY, USA, 2023.
- Muthén, L.k.; Muthén, B.O. Mplus, Version 8.11; Muthén & Muthén: Los Angeles, CA, USA, 2024.
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988. [Google Scholar] [CrossRef]
- Chan, C.W.H.; Au Yeung, E.; Law, B.M.H. Effectiveness of Physical Activity Interventions on Pregnancy-Related Outcomes among Pregnant Women: A Systematic Review. Int. J. Environ. Res. Public. Health 2019, 16, 1840. [Google Scholar] [CrossRef]
- Mottola, M.F.; Davenport, M.H.; Ruchat, S.-M.; Davies, G.A.; Poitras, V.J.; Gray, C.E.; Garcia, A.J.; Barrowman, N.; Adamo, K.B.; Duggan, M.; et al. 2019 Canadian Guideline for Physical Activity throughout Pregnancy. Br. J. Sports Med. 2018, 52, 1339–1346. [Google Scholar] [CrossRef]
- Ewing, R.; Cervero, R. Travel and the Built Environment: A Meta-Analysis. J. Am. Plann. Assoc. 2010, 76, 265–294. [Google Scholar] [CrossRef]
- Stewart, O.T.; Vernez Moudon, A.; Saelens, B.E.; Lee, C.; Kang, B.; Doescher, M.P. Comparing Associations Between the Built Environment and Walking in Rural Small Towns and a Large Metropolitan Area. Environ. Behav. 2016, 48, 13–36. [Google Scholar] [CrossRef]
- Joiner, A.; McFarlane, C.; Rella, L.; Uriarte-Ruiz, M. Problematising Density: COVID-19, the Crowd, and Urban Life. Soc. Cult. Geogr. 2024, 25, 181–198. [Google Scholar] [CrossRef]
- Bu, F.; Mak, H.W.; Steptoe, A.; Wheeler, B.W.; Fancourt, D. Urban Greenspace and Anxiety Symptoms during the COVID-19 Pandemic: A 20-Month Follow up of 19,848 Participants in England. Health Place 2022, 77, 102897. [Google Scholar] [CrossRef] [PubMed]
- Badon, S.E.; Iturralde, E.; Nkemere, L.; Nance, N.; Avalos, L.A. Perceived Barriers and Motivators for Physical Activity in Women with Perinatal Depression. J. Phys. Act. Health 2021, 18, 801–810. [Google Scholar] [CrossRef] [PubMed]
| Variables | n | N |
|---|---|---|
| Mother’s age (years) | 1059 | |
| 18 to 27 | 232 (21.9%) | |
| 28 to 35 | 682 (64.4%) | |
| 36 to 45 | 145 (13.7%) | |
| Ethnicity | 1068 | |
| White | 1027 (96.2%) | |
| Black | 11 (1%) | |
| Asian | 11 (1%) | |
| Latin American | 12 (1.1%) | |
| Other | 7 (0.7%) | |
| Education | 1055 | |
| High school diploma or less | 60 (5.5%) | |
| Postsecondary diplomas (non-university) | 306 (28.2%) | |
| University diploma | 689 (65.3%) | |
| Family income (CAD$) | 1046 | |
| 49,999 or less | 99 (9.5%) | |
| 50,000 to 79,999 | 163 (15.6%) | |
| 80,000 to 99,999 | 183 (17.5%) | |
| 100,000 to 149,999 | 426 (40.7%) | |
| 150,000 and more | 175 (16.7%) | |
| First pregnancy | 1080 | |
| Yes | 592 (54.8%) | |
| No | 488 (45.2%) | |
| Pregnancy complications | 1086 | |
| No | 834 (76.8%) | |
| Yes | 252 (23.2%) | |
| Number of children at home | 1080 | |
| 0 | 653 (60.5%) | |
| 1 | 297 (27.5%) | |
| 2 | 98 (9.1%) | |
| 3 or more | 32 (2.9%) | |
| Living with a partner | 1052 | |
| Yes | 1009 (95.9%) | |
| No | 43 (4.1%) | |
| Density (number of people per km2) | 1065 | |
| 400 or less (rural region) | 541 (49.8%) | |
| 401 and more (urban region) | 524 (48.3%) | |
| COVID-19 waves at completion | 1086 | |
| Second wave (23 August 2020–20 March 2021) | 59 (5.4%) | |
| Third wave (21 March–17 July 2021) | 63 (5.8%) | |
| Fourth wave (18 July–4 December 2021) | 221 (20.3%) | |
| Fifth wave (5 December 2021–12 March 2022) | 299 (27.5%) | |
| Sixth wave (13 March–28 May 2022) | 207 (19.1%) | |
| Seventh wave (29 May 2022 onward) | 237 (21.8%) | |
| Season during completion | 1086 | |
| Winter | 344 (31.7%) | |
| Spring | 296 (27.3%) | |
| Summer | 222 (20.4%) | |
| Fall | 224 (20.6%) |
| Variables | N | Mean | SD | Min. | Max. |
|---|---|---|---|---|---|
| Maternal well-being indices | |||||
| Generalized anxiety symptoms | 1074 | 5.18 | 4.50 | 0 | 21 |
| Perceived stress symptoms | 1077 | 20.31 | 3.99 | 0 | 33 |
| Depressive symptoms | 1080 | 7.64 | 5.36 | 0 | 28 |
| Pregnancy-related anxiety symptoms | 1082 | 23.85 | 7.50 | 10 | 50 |
| Walking levels (METs-H/week) | |||||
| Slow walking | 1086 | 4.12 | 3.35 | 0 | 9.60 |
| Uphill walking | 1086 | 2.37 | 4.66 | 0 | 19.50 |
| Total walking score | 1086 | 6.50 | 6.75 | 0 | 29.10 |
| Variables | Generalized Anxiety | Depression | Perceived Stress | Pregnancy-Related Anxiety |
|---|---|---|---|---|
| β | β | β | β | |
| Model 1 | ||||
| Walking | −0.11 *** | −0.11 *** | −0.13 *** | −0.00 |
| R2 | 0.01 * | 0.01 | 0.02 * | 0.00 |
| Model 2 | ||||
| Walking | −0.06 * | −0.05 | −0.07 ** | −0.02 |
| Summer | −0.10 | −0.10 * | −0.04 | −0.10 |
| Fall | −0.09 | −0.07 | −0.03 | −0.03 |
| Spring | −0.14 * | −0.11 * | −0.08 | −0.13 * |
| Wave 2 of COVID-19 | −0.06 | −0.03 | −0.03 | −0.05 |
| Wave 3 of COVID-19 | 0.04 | 0.05 | 0.05 | −0.00 |
| Wave 4 of COVID-19 | −0.05 | −0.04 | −0.06 | −0.08 * |
| Wave 5 of COVID-19 | −0.03 | 0.01 | −0.01 | −0.13 * |
| Pregnancy complications | 0.19 *** | 0.16 *** | 0.17 *** | 0.13 *** |
| First pregnancy | 0.04 | 0.04 | 0.07 * | −0.24 *** |
| University diploma | −0.19 ** | −0.23 ** | −0.08 | −0.05 |
| Postsecondary diplomas (non-university) | −0.11 | −0.10 | 0.01 | −0.04 |
| Mother’s age | −0.13 *** | −0.05 | −0.07 * | −0.02 |
| Partner support | −0.27 *** | −0.34 *** | −0.33 *** | −0.18 *** |
| Population density | 0.08 * | 0.04 | 0.05 | 0.05 |
| R2 | 0.17 *** | 0.20 *** | 0.19 *** | 0.10 *** |
| Variables | β | p |
|---|---|---|
| Wave 3 of COVID-19 | −0.07 | 0.123 |
| Wave 4 of COVID-19 | −0.19 ** | 0.003 |
| Wave 5 of COVID-19 | −0.22 ** | 0.002 |
| Wave 6–7 of COVID-19 | −0.17 * | 0.028 |
| Pregnancy complications | −0.06 * | 0.039 |
| Mother’s age | 0.06 | 0.051 |
| Number of children | −0.16 *** | <0.001 |
| Partner support | 0.06 * | 0.044 |
| Population density | 0.09 ** | 0.005 |
| COVID-19 concerns | −0.03 | 0.412 |
| University diploma | 0.13* | 0.019 |
| Postsecondary diplomas (non-university) | 0.07 | 0.216 |
| R2 | 0.08 *** | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brun, A.; Ruchat, S.-M.; Chaput-Langlois, S.; Booij, L.; Giac, R.; Séguin, K.; Bernier, A.; Morisset, A.-S.; Boucoiran, I.; Vaillancourt, C.; et al. Associations Between Walking in the Third Trimester of Pregnancy and Maternal Mental Health During the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2025, 22, 1538. https://doi.org/10.3390/ijerph22101538
Brun A, Ruchat S-M, Chaput-Langlois S, Booij L, Giac R, Séguin K, Bernier A, Morisset A-S, Boucoiran I, Vaillancourt C, et al. Associations Between Walking in the Third Trimester of Pregnancy and Maternal Mental Health During the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2025; 22(10):1538. https://doi.org/10.3390/ijerph22101538
Chicago/Turabian StyleBrun, Angélique, Stephanie-May Ruchat, Sophie Chaput-Langlois, Linda Booij, Raphaëlle Giac, Katherine Séguin, Andréanne Bernier, Anne-Sophie Morisset, Isabelle Boucoiran, Cathy Vaillancourt, and et al. 2025. "Associations Between Walking in the Third Trimester of Pregnancy and Maternal Mental Health During the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 22, no. 10: 1538. https://doi.org/10.3390/ijerph22101538
APA StyleBrun, A., Ruchat, S.-M., Chaput-Langlois, S., Booij, L., Giac, R., Séguin, K., Bernier, A., Morisset, A.-S., Boucoiran, I., Vaillancourt, C., Lippé, S., & Herba, C. M. (2025). Associations Between Walking in the Third Trimester of Pregnancy and Maternal Mental Health During the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 22(10), 1538. https://doi.org/10.3390/ijerph22101538







