Visualizing Parcel-Level Lead Risk Using an Exterior Housing-Based Index
Abstract
1. Introduction
2. Methods
2.1. Data Sources
2.2. The Exterior Lead Risk Index
2.3. Statistical Methods
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- LeBlanc, T.T.; Svendsen, E.R.; Allwood, P. Ubiquitous Lead—A Challenge for the Future of Public Health. Am. J. Public Health 2022, 112, S628. [Google Scholar] [CrossRef]
- McFarland, M.J.; Hauer, M.E.; Reuben, A. Half of US population exposed to adverse lead levels in early childhood. Proc. Natl. Acad. Sci. USA 2022, 119, e2118631119. [Google Scholar] [CrossRef]
- Patterson, C.C. An Alternative Perspective—Lead Pollution in the Human Environment: Origin, Extent, and Significance. In Lead in the Human Environment: A Report; National Research Council (U.S.), Ed.; National Academy of Sciences: Washington, DC, USA, 1980; pp. 265–350. [Google Scholar]
- Rosner, D.; Markowitz, G. Building the World That Kills Us: The Politics of Lead, Science, and Polluted Homes, 1970 to 2000. J. Urban. Hist. 2016, 42, 323–345. [Google Scholar] [CrossRef]
- Needleman, H. Lead poisoning. Annu. Rev. Med. 2004, 55, 209–222. [Google Scholar] [CrossRef]
- Needleman, H. Childhood lead poisoning: The promise and abandonment of primary prevention. Am. J. Public Health 1998, 88, 1871–1877. [Google Scholar] [CrossRef]
- Lanphear, B.P. Low-level toxicity of chemicals: No acceptable levels? PLoS Biol. 2017, 15, e2003066. [Google Scholar] [CrossRef]
- Jones, D.J. Primary prevention and health outcomes: Treatment of residential lead-based paint hazards and the prevalence of childhood lead poisoning. J. Urban. Econ. 2012, 71, 151–164. [Google Scholar] [CrossRef]
- Jacobs, D.E.; Clickner, R.P.; Zhou, J.Y.; Viet, S.M.; Marker, D.A.; Rogers, J.W.; Zeldin, D.C.; Broene, P.; Friedman, W. The Prevalence of Lead-Based Paint Hazards in, U.S. Housing. Environ. Health Perspect. 2002, 110, A599–A606. [Google Scholar] [CrossRef] [PubMed]
- Hanna-Attisha, M.; LaChance, J.; Sadler, R.C.; Champney Schnepp, A. Elevated Blood Lead Levels in Children Associated With the Flint Drinking Water Crisis: A Spatial Analysis of Risk and Public Health Response. Am. J. Public Health 2016, 106, 283–290. [Google Scholar] [CrossRef]
- Brown, M.J.; Raymond, J.; Homa, D.; Kennedy, C.; Sinks, T. Association between children’s blood lead levels, lead service lines, and water disinfection, Washington, DC, 1998–2006. Environ. Res. 2011, 111, 67–74. [Google Scholar] [CrossRef]
- Mielke, H.W.; Laidlaw, M.A.S.; Gonzales, C. Lead (Pb) legacy from vehicle traffic in eight California urbanized areas: Continuing influence of lead dust on children’s health. Sci. Total Environ. 2010, 408, 3965–3975. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Zhang, H. Accumulation of Heavy Metals in Roadside Soil in Urban Area and the Related Impacting Factors. Int. J. Environ. Res. Public Health 2018, 15, 1064. [Google Scholar] [CrossRef]
- McClintock, N. A critical physical geography of urban soil contamination. Geoforum 2015, 65, 69–85. [Google Scholar] [CrossRef]
- Moody, H.A.; Darden, J.T.; Pigozzi BWm Grady, S.C. The Relationship of Neighborhood Socioeconomic Differences and Racial Residential Segregation to Childhood Blood Lead Levels in Metropolitan Detroit. J. Urban. Health 2016, 93, 820–839. [Google Scholar] [CrossRef]
- Subcommittee on Economic and Consumer Policy, Committee on Oversight and Reform. Baby Foods Are Tainted with Dangerous Levels of Arsenic, Lead, Cadmium, and Mercury; U.S. House of Representatives: Washington, DC, USA, 2021. Available online: https://oversightdemocrats.house.gov/sites/evo-subsites/democrats-oversight.house.gov/files/2021-02-04%20ECP%20Baby%20Food%20Staff%20Report.pdf (accessed on 19 December 2024).
- Nigg, J.T.; Nikolas, M.; Mark Knottnerus, G.; Cavanagh, K.; Friderici, K. Confirmation and extension of association of blood lead with attention-deficit/hyperactivity disorder (ADHD) and ADHD symptom domains at population-typical exposure levels: ADHD and blood lead. J. Child. Psychol. Psychiatry 2010, 51, 58–65. [Google Scholar] [CrossRef]
- Aizer, A.; Currie, J. Lead and Juvenile Delinquency: New Evidence from Linked Birth, School and Juvenile Detention Records. Published online May 2017. Available online: https://www.nber.org/papers/w23392 (accessed on 26 August 2021).
- Reuben, A.; Caspi, A.; Belsky, D.W.; Broadbent, J.; Harrington, H.; Sugden, K.; Houts, R.M.; Ramrakha, S.; Poulton, R.; Moffitt, T.E. Association of Childhood Blood Lead Levels with Cognitive Function and Socioeconomic Status at Age 38 Years and with IQ Change and Socioeconomic Mobility Between Childhood and Adulthood. JAMA 2017, 317, 1244. [Google Scholar] [CrossRef]
- Sanders, T.; Liu, Y.; Buchner, V.; Tchounwou, P.B. Neurotoxic Effects and Biomarkers of Lead Exposure: A review. Rev. Environ. Health 2009, 24, 15–45. [Google Scholar] [CrossRef]
- Kim, R.; Rotnitzky, A.; Sparrow, D.; Weiss, S.T.; Wagner, C.; Hu, H. A Longitudinal Study of Low-Level Lead Exposure and Impairment of Renal Function: The Normative Aging Study. JAMA 1996, 275, 1177–1181. [Google Scholar] [CrossRef] [PubMed]
- Ronis, M.J.J.; Gandy, J.; Badger, T. Endocrine mechanisms underlying reproductive toxicity in the developing rat chronically exposed to dietary lead. J. Toxicol. Environ. Health A 1998, 54, 77–99. [Google Scholar] [CrossRef]
- Vaziri, N.D. Mechanisms of lead-induced hypertension and cardiovascular disease. Am. J. Physiol. Heart Circ. Physiol. 2008, 295, H454–H465. [Google Scholar] [CrossRef]
- Grandjean, P.; Landrigan, P.J. Neurobehavioural effects of developmental toxicity. Lancet Neurol. 2014, 13, 330–338. [Google Scholar] [CrossRef] [PubMed]
- White, B.M.; Bonilha, H.S.; Ellis, C. Racial/Ethnic Differences in Childhood Blood Lead Levels Among Children <72 Months of Age in the United States: A Systematic Review of the Literature. J. Racial Ethn. Health Disparities 2016, 3, 145–153. [Google Scholar] [CrossRef]
- Egan, K.B.; Cornwell, C.R.; Courtney, J.G.; Ettinger, A.S. Blood Lead Levels in U.S. Children Ages 1–11 Years, 1976–2016. Environ. Health Perspect. 2021, 129, 037003. [Google Scholar] [CrossRef]
- Bailey, A.J.; Sargent, J.D.; Blake, M.K. A tale of Two Counties: Childhood Lead Poisoning, Industrialization, and Abatement in New England. Econ Geogr. 1998, 74, 96–111. [Google Scholar]
- Hauptman, M.; Niles, J.K.; Gudin, J.; Kaufman, H.W. Individual- and Community-Level Factors Associated With Detectable and Elevated Blood Lead Levels in US Children: Results From a National Clinical Laboratory. JAMA Pediatr. 2021, 175, 1252–1260. [Google Scholar] [CrossRef]
- Hauptman, M.; Rogers, M.L.; Scarpaci, M.; Morin, B.; Vivier, P.M. Neighborhood disparities and the burden of lead poisoning. Pediatr. Res. 2023, 94, 826–836. [Google Scholar] [CrossRef] [PubMed]
- Zartarian, V.; Poulakos, A.; Garrison, V.H.; Spalt, N.; Tornero-Velez, R.; Xue, J.; Egan, K.; Courtney, J. Lead Data Mapping to Prioritize US Locations for Whole-of-Government Exposure Prevention Efforts: State of the Science, Federal Collaborations, and Remaining Challenges. Am. J. Public Health 2022, 112, S658–S669. [Google Scholar] [CrossRef]
- U.S. Environmental Protection Agency. EJScreen: Environmental Justice Screening and Mapping Tool. 3 September 2014. Available online: https://www.epa.gov/ejscreen (accessed on 14 June 2024).
- Garrison, V.E.H.; Ashley, P.J. Identifying Jurisdictions at Risk of Containing Housing Units With Deteriorated Paint: Results and Targeting Implications for the US Department of Housing and Urban Development. J. Public Health Manag. Pract. 2020; Publish Ahead of Print. [Google Scholar] [CrossRef]
- Schultz, B.D.; Morara, M.; Buxton, B.E.; Weintraub, M. Predicting Blood-Lead Levels Among U.S. Children at the Census Tract Level. Environ. Justice 2017, 10, 129–136. [Google Scholar] [CrossRef]
- Romer Present, P.S.; Berg, K.; Snow, M.; Richardson, K. Detecting New Sources of Childhood Environmental Lead Exposure Using a Statistical Surveillance System, 2015–2019. Am. J. Public Health 2022, 112, S715–S722. [Google Scholar] [CrossRef] [PubMed]
- Xue, J.; Zartarian, V.; Tornero-Velez, R.; Stanek, L.W.; Poulakos, A.; Walts, A.; Triantafillou, K.; Suero, M.; Grokhowsky, N. A Generalizable Evaluated Approach, Applying Advanced Geospatial Statistical Methods, to Identify High Lead Exposure Locations at Census Tract Scale: Michigan Case Study. Environ. Health Perspect. 2022, 130, 077004. [Google Scholar] [CrossRef]
- Ettinger, A.S. Invited Perspective: Identifying Childhood Lead Exposure Hotspots for Action. Environ. Health Perspect. 2022, 130, 071301. [Google Scholar] [CrossRef]
- Jacobs, D.E.; Wilson, J.; Dixon, S.L.; Smith, J.; Evens, A. The Relationship of Housing and Population Health: A 30-Year Retrospective Analysis. Environ. Health Perspect. 2009, 117, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Dixon, S.; Wilson, J.; Kawecki, C.; Green, R.; Phoenix, J.; Galke, W.; Clark, S.; Breysse, J. Selecting a Lead Hazard Control Strategy Based on Dust Lead Loading Housing Condition:, I. Methods and Results. J. Occup. Environ. Hyg. 2008, 5, 530–539. [Google Scholar] [CrossRef] [PubMed]
- Weitzman, M.; Baten, A.; Rosenthal, D.G.; Hoshino, R.; Tohn, E.; Jacobs, D.E. Housing and Child Health. Curr. Probl. Pediatr. Adolesc. Health Care 2013, 43, 187–224. [Google Scholar] [CrossRef] [PubMed]
- Office of the Surgeon General, United States Public Health Service; National Center for Environmental Health. The Surgeon General’s Call to Action to Promote Healthy Homes; U.S. Department of Health and Human Services: Washington, DC, USA, 2009.
- Braveman, P.; Gottlieb, L. The Social Determinants of Health: It’s Time to Consider the Causes of the Causes. Public. Health Rep. 2014, 129 (Suppl. S2), 19–31. [Google Scholar] [CrossRef] [PubMed]
- Markowitz, G.E.; Rosner, D. Lead Wars: The Politics of Science and the Fate of America’s Children; University of California Press: Oakland, CA, USA, 2014. [Google Scholar]
- Robinson, W. Ecological Correlations and the Behavior of Individuals. Int. J. Epidemiol. 2009, 38, 337–341. [Google Scholar] [CrossRef]
- Manson, S.M.; Sander, H.A.; Ghosh, D.; Oakes, J.M.; Orfield, J.M.W.; Craig, W.J.; Luce, J.T.F.; Myott, E.; Sun, S. Parcel Data for Research and Policy. Geogr. Compass 2009, 3, 698–726. [Google Scholar] [CrossRef]
- Wilson, B.; Wilson, N.; Martin, S. Using GIS to Advance Social Economics Research: Geocoding, Aggregation, and Spatial Thinking. Forum. Soc. Econ. 2019, 50, 480–504. [Google Scholar] [CrossRef]
- President’s Task Force on Environmental Health Risks and Safety Risks to Children. 2018. Available online: https://www.epa.gov/sites/default/files/2018-12/documents/fedactionplan_lead_final.pdf (accessed on 19 September 2023).
- Breysse, P.N.; Cascio, W.E.; Geller, A.M.; Choiniere, C.J.; Ammon, M. Targeting Coordinated Federal Efforts to Address Persistent Hazardous Exposures to Lead. Am. J. Public Health 2022, 112, S640–S646. [Google Scholar] [CrossRef]
- Wilson, N.J.; Friedman, E.; Kennedy, K.; Manolakos, P.T.; Reierson, L.; Roberts, A.; Simon, S. Using exterior housing conditions to predict elevated pediatric blood lead levels. Environ. Res. 2023, 218, 114944. [Google Scholar] [CrossRef]
- Ruckart, P.Z.; Jones, R.L.; Courtney, J.G.; LeBlanc, T.T.; Jackson, W.; Karwowski, M.P.; Cheng, P.-Y.; Allwood, P.; Svendsen, E.R.; Breysse, P.N. Update of the Blood Lead Reference Value—United States, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1509–1512. [Google Scholar] [CrossRef] [PubMed]
- Dignam, T.; Kaufmann, R.B.; LeStourgeon, L.; Brown, M.J. Control of Lead Sources in the United States, 1970–2017: Public Health Progress and Current Challenges to Eliminating Lead Exposure. J. Public Health Manag. Pract. 2019, 25, S13–S22. [Google Scholar] [CrossRef]
- Lanphear, B.P.; Hornung, R.; Khoury, J.; Yolton, K.; Baghurst, P.; Bellinger, D.C.; Canfield, R.L.; Dietrich, K.N.; Bornschein, R.; Greene, T.; et al. Low-Level Environmental Lead Exposure and Children’s Intellectual Function: An International Pooled Analysis. Environ. Health Perspect. 2005, 113, 894–899. [Google Scholar] [CrossRef] [PubMed]
- Clark, S.; Galke, W.; Succop, P.; Grote, J.; McLaine, P.; Wilson, J.; Dixon, S.; Menrath, W.; Roda, S.; Chen, M.; et al. Effects of HUD-supported lead hazard control interventions in housing on children’s blood lead. Environ. Res. 2011, 111, 301–311. [Google Scholar] [CrossRef]
- Wilson, N.J.; Bowles, D. A Parcel Level Housing Conditions Survey in Academic and Civil Context. SAGE Open 2024, 14, 21582440241257674. [Google Scholar] [CrossRef]
- Kennedy, K. Housing and Health: Making the Connection Using Geographic Information Systems; Practicum Report; University of Missouri-Kansas City: Kansas City, MO, USA, 2011. [Google Scholar]
- Šimić, I.; Lovrić, M.; Godec, R.; Kröll, M.; Bešlić, I. Applying machine learning methods to better understand, model and estimate mass concentrations of traffic-related pollutants at a typical street canyon. Environ. Pollut. 2020, 263, 114587. [Google Scholar] [CrossRef]
- Goin, D.E.; Rudolph, K.E.; Ahern, J. Predictors of firearm violence in urban communities: A machine-learning approach. Health Place. 2018, 51, 61–67. [Google Scholar] [CrossRef]
- Tibshirani, R. Regression Shrinkage and Selection Via the Lasso. J. R. Stat. Soc. Ser. B Methodol. 1996, 58, 267–288. [Google Scholar] [CrossRef]
- Breysse, P.; Farr, N.; Galke, W.; Lanphear, B.; Morley, R.; Bergofsky, L. The Relationship between Housing and Health: Children at Risk. Environ. Health Perspect. 2004, 112, 1583–1588. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences, Engineering, and Medicine. Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health; National Academies Press: Washington, DC, USA, 2019; p. 25467. [Google Scholar] [CrossRef]
- Zartarian, V.G.; Xue, J.; Poulakos, A.G.; Tornero-Velez, R.; Stanek, L.W.; Snyder, E.; Garrison, V.H.; Egan, K.; Courtney, J.G. A U.S. Lead Exposure Hotspots Analysis. Environ. Sci. Technol. 2024, 58, 3311–3321. [Google Scholar] [CrossRef] [PubMed]
- Baek, M.; Outrich, M.B.; Barnett, K.S.; Reece, J. Neighborhood-Level Lead Paint Hazard for Children under 6: A Tool for Proactive and Equitable Intervention. Int. J. Environ. Res. Public Health 2021, 18, 2471. [Google Scholar] [CrossRef] [PubMed]
- Kwan, M.P. The Uncertain Geographic Context Problem. Ann. Am. Assoc. Geogr. 2012, 102, 958–968. [Google Scholar] [CrossRef]
- American Healthy Homes Survey II. U.S. Department of Housing and Urban Development Office of Lead Hazard Control and Healthy Homes. 2021. Available online: https://www.hud.gov/sites/dfiles/HH/documents/AHHS%20II_Lead_Findings_Report_Final_29oct21.pdf (accessed on 19 December 2024).
- Akkus, C.; Ozdenerol, E. Exploring Childhood Lead Exposure through GIS: A Review of the Recent Literature. Int. J. Environ. Res. Public Health 2014, 11, 6314–6334. [Google Scholar] [CrossRef] [PubMed]
- Miranda, M.L.; Dolinoy, D.C.; Overstreet, M.A. Mapping for Prevention: GIS Models for Directing Childhood Lead Poisoning Prevention Programs. Environ. Health Perspect. 2002, 110, 947–953. [Google Scholar] [CrossRef] [PubMed]
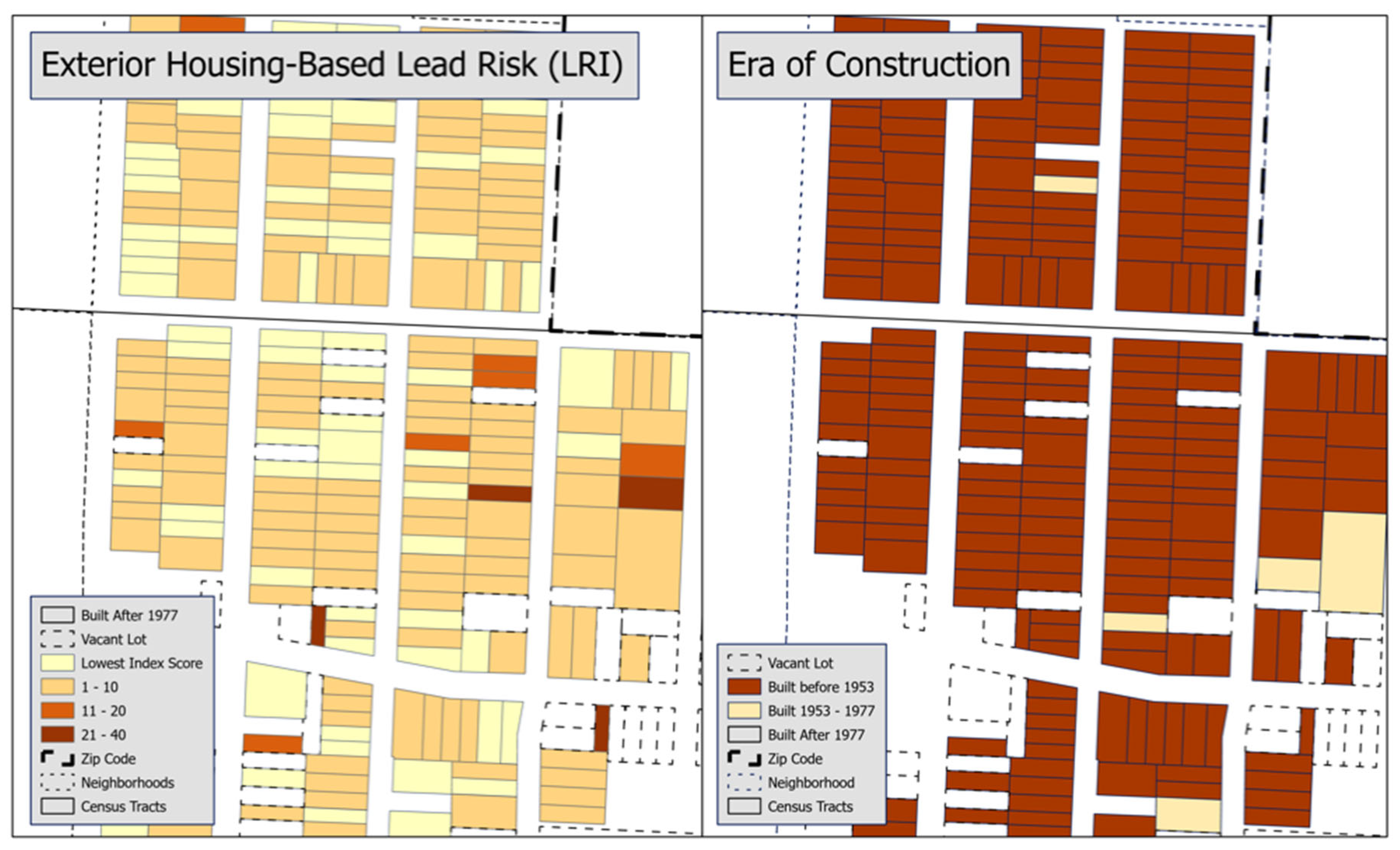
| Era of Home Construction | Value | Condition of Housing Category | Value |
|---|---|---|---|
| 1978 or later | 0 | Excellent or Good | 0 |
| 1953–1977 | 1 | Substandard | 1 |
| 1952 or before | 2 | Seriously Deteriorated | 2 |
| Severely Deteriorated | 3 | ||
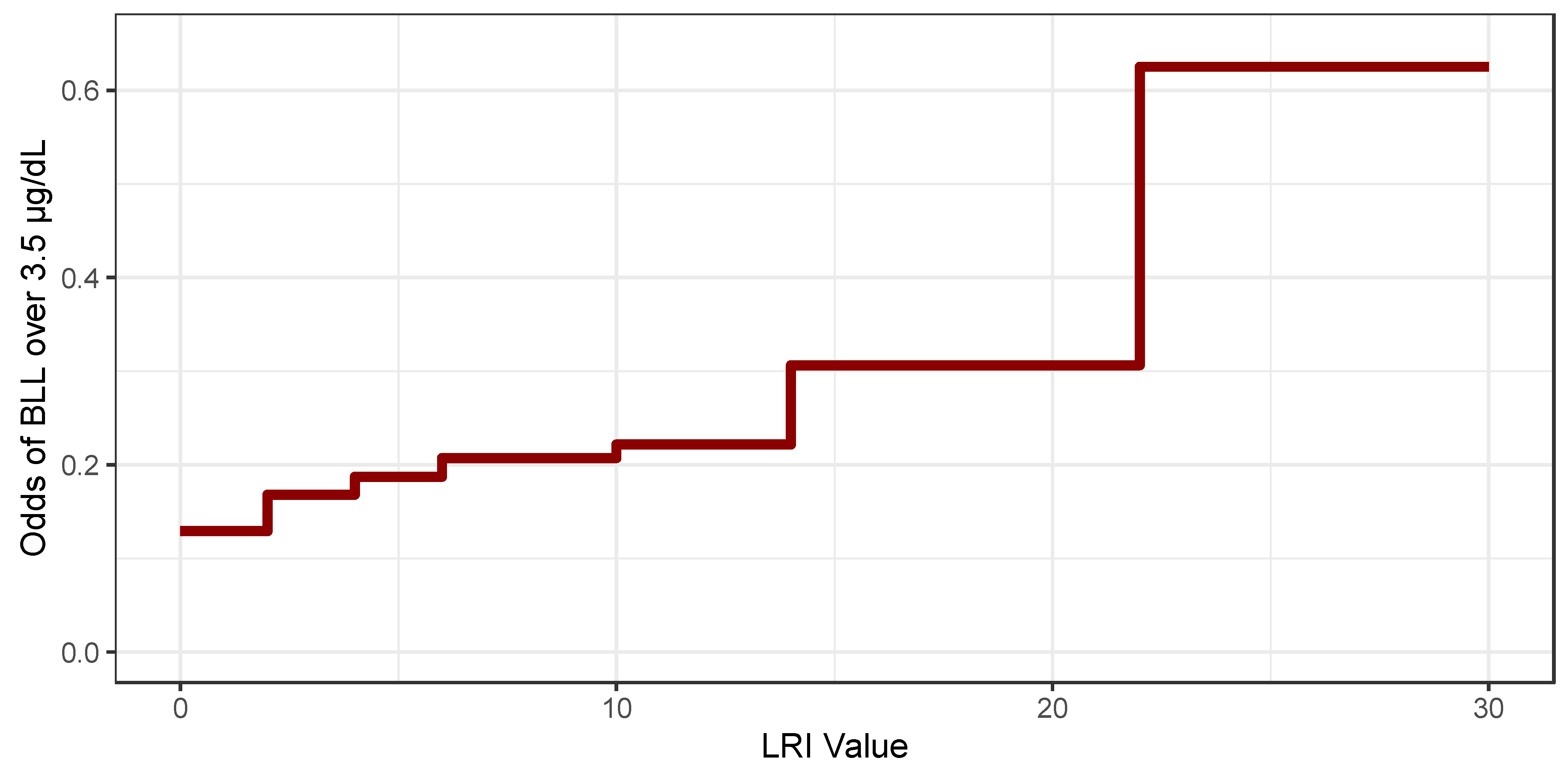
| Variable | Observations | Lasso Coefficient Estimate | Variable | Observations | Lasso Coefficient Estimate |
|---|---|---|---|---|---|
| (Intercept) | −1.909 | ||||
| LRI Contrasts | Child-focused Variables | ||||
| LRI 1 | 368 | · | Test Before 2005 | 1983 | 1.52 |
| LRI 2 | 1399 | 0.3109 | 18–36 months | 1709 | 0.4067 |
| LRI 3 | 36 | · | 37–72 months | 2987 | · |
| LRI 4 | 899 | 0.1289 | Public Walks Contrasts | ||
| LRI 5 | 21 | · | Ordinal Rating 2 | 2162 | · |
| LRI 6 | 548 | 0.127 | Ordinal Rating 3 | 1082 | · |
| LRI 8 | 488 | · | Ordinal Rating 4 | 359 | · |
| LRI 9 | 2 | · | Ordinal Rating 5 | 512 | · |
| LRI 10 | 205 | 0.0859 | Curbs Contrasts | ||
| LRI 12 | 88 | · | Ordinal Rating 2 | 2545 | · |
| LRI 14 | 60 | 0.4393 | Ordinal Rating 3 | 1006 | · |
| LRI 16 | 48 | · | Ordinal Rating 4 | 699 | · |
| LRI 18 | 16 | · | Ordinal Rating 5 | 358 | · |
| LRI 20 | 8 | · | Streetlights Contrast | ||
| LRI 22 | 7 | 1.3288 | Ordinal Rating 2 | 300 | · |
| LRI 24 | 1 | · | Ordinal Rating 3 | 21 | · |
| LRI 26 | 1 | · | Ordinal Rating 4 | 2 | · |
| LRI 30 | 1 | · | Ordinal Rating 5 | 4 | · |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilson, N.J.; Allenbrand, R.; Friedman, E.; Kennedy, K.; Roberts, A.; Simon, S. Visualizing Parcel-Level Lead Risk Using an Exterior Housing-Based Index. Int. J. Environ. Res. Public Health 2025, 22, 16. https://doi.org/10.3390/ijerph22010016
Wilson NJ, Allenbrand R, Friedman E, Kennedy K, Roberts A, Simon S. Visualizing Parcel-Level Lead Risk Using an Exterior Housing-Based Index. International Journal of Environmental Research and Public Health. 2025; 22(1):16. https://doi.org/10.3390/ijerph22010016
Chicago/Turabian StyleWilson, Neal J., Ryan Allenbrand, Elizabeth Friedman, Kevin Kennedy, Amy Roberts, and Stephen Simon. 2025. "Visualizing Parcel-Level Lead Risk Using an Exterior Housing-Based Index" International Journal of Environmental Research and Public Health 22, no. 1: 16. https://doi.org/10.3390/ijerph22010016
APA StyleWilson, N. J., Allenbrand, R., Friedman, E., Kennedy, K., Roberts, A., & Simon, S. (2025). Visualizing Parcel-Level Lead Risk Using an Exterior Housing-Based Index. International Journal of Environmental Research and Public Health, 22(1), 16. https://doi.org/10.3390/ijerph22010016






