Molecular Surveillance of Artemisinin-Resistant Plasmodium falciparum Parasites in Mining Areas of the Roraima Indigenous Territory in Brazil
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. World Malaria Report 2022; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Brazil. Ministry of Health. Data for Citizens from the Sivep-Malaria, Sinan and E-SUS-VS Data Sources, for Notifications in Brazil from 2007 to 2023. Available online: https://public.tableau.com/app/profile/mal.ria.brasil/viz/Dadosparacidado_201925_03_2020/Incio (accessed on 13 April 2024).
- Brazil Ministry of Health. Health Surveillance Secretariat. In Epidemiological Bulletin—Malaria 2021; Ministry of Health: Brasília, Brazil, 2022. [Google Scholar]
- World Health Organization. Global Technical Strategy For Malaria 2016–2030; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Eliminate Malaria Brazil: National Malaria Elimination Plan; Brazil, Ministry of Health, Health Surveillance Secretariat, Department of Immunization and Communicable Diseases: Brasília, Brazil, 2022; 60p.
- World Health Organization. Artemisinin Resistance and Artemisinin-Based Combination Therapy Efficacy; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Payne, D. Spread of chloroquine resistance in Plasmodium falciparum. Parasitol. Today 1987, 3, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Cortese, J.F.; Caraballo, A.; Contreras, C.E.; Plowe, C.V. Origin and dissemination of Plasmodium falciparum drug-resistance mutations in South America. J. Infect. Dis. 2002, 186, 999–1006. [Google Scholar] [CrossRef] [PubMed]
- Griffing, S.M.; Mixson-Hayden, T.; Sridaran, S.; Alam, M.T.; McCollum, A.M.; Cabezas, C. South American Plasmodium falciparum after the malaria eradication era: Clonal population expansion and survival of the fittest hybrids. PLoS ONE 2011, 6, e23486. [Google Scholar] [CrossRef] [PubMed]
- Sridaran, S.; Rodriguez, B.; Soto, A.M.; Macedo De Oliveira, A.; Udhayakumar, V. Molecular analysis of chloroquine and sulfadoxine-pyrimethamine resistance-associated alleles in Plasmodium falciparum isolates from Nicaragua. Am. J. Trop. Med. Hyg. 2014, 90, 840–845. [Google Scholar] [CrossRef]
- Pelleau, S.; Moss, E.L.; Dhingra, S.K.; Volney, B.; Casteras, J.; Gabryszewski, S.J. Adaptive evolution of malaria parasites in French Guiana: Reversal of chloroquine resistance by acquisition of a mutation in pfcrt. Proc. Natl. Acad. Sci. USA 2015, 112, 11672–11677. [Google Scholar] [CrossRef] [PubMed]
- Cerutti, C., Jr.; Durlacher, R.R.; de Alencar, F.E.; Segurado, A.A.; Pang, L.W. In vivo efficacy of mefloquine for the treatment of Falciparum malaria in Brazil. J. Infect. Dis. 1999, 180, 2077–2080. [Google Scholar] [CrossRef]
- Tchekounou, C.; Zida, A.; Zongo, C.; Soulama, I.; Sawadogo, P.M.; Guiguemde, K.T. Antimalarial drugs resistance genes of Plasmodium falciparum: A review. Ann. Parasitol. 2022, 68, 215–225. [Google Scholar] [PubMed]
- Newton, P.N.; Dondorp, A.; Green, M.; Mayxay, M.; White, N.J. Counterfeit artesunate antimalarials in southeast Asia. Lancet 2003, 362, 169. [Google Scholar] [CrossRef]
- Ouji, M.; Augereau, J.M.; Paloque, L.; Benoit-Vical, F. Plasmodium falciparum resistance to artemisinin-based combination therapies: A sword of Damocles in the path toward malaria elimination. Parasite 2018, 25, 24. [Google Scholar] [CrossRef]
- Lapouble, O.M.M.; Santelli, A.C.F.S.; Muniz-Junqueira, M.I. Epidemiological situation of malaria in the Brazilian Amazon region, 2003 to 2012. Rev. Panam. Salud Publica 2015, 38, 4. [Google Scholar]
- Ward, K.E.; Fidock, D.A.; Bridgford, J.L. Plasmodium falciparum resistance to artemisinin-based combination therapies. Curr. Opin. Microbiol. 2022, 69, 102193. [Google Scholar] [CrossRef] [PubMed]
- Straimer, J.; Gnädig, N.F.; Witkowski, B.; Amaratunga, C.; Duru, V.; Ramadani, A.P. Drug resistance. K13-propeller mutations confer artemisinin resistance in Plasmodium falciparum clinical isolates. Science 2015, 347, 428–431. [Google Scholar]
- Yeung, S.; Van Damme, W.; Socheat, D.; White, N.J.; Mills, A. Access to artemisinin combination therapy for malaria in remote areas of Cambodia. Malar. J. 2008, 7, 96. [Google Scholar] [CrossRef] [PubMed]
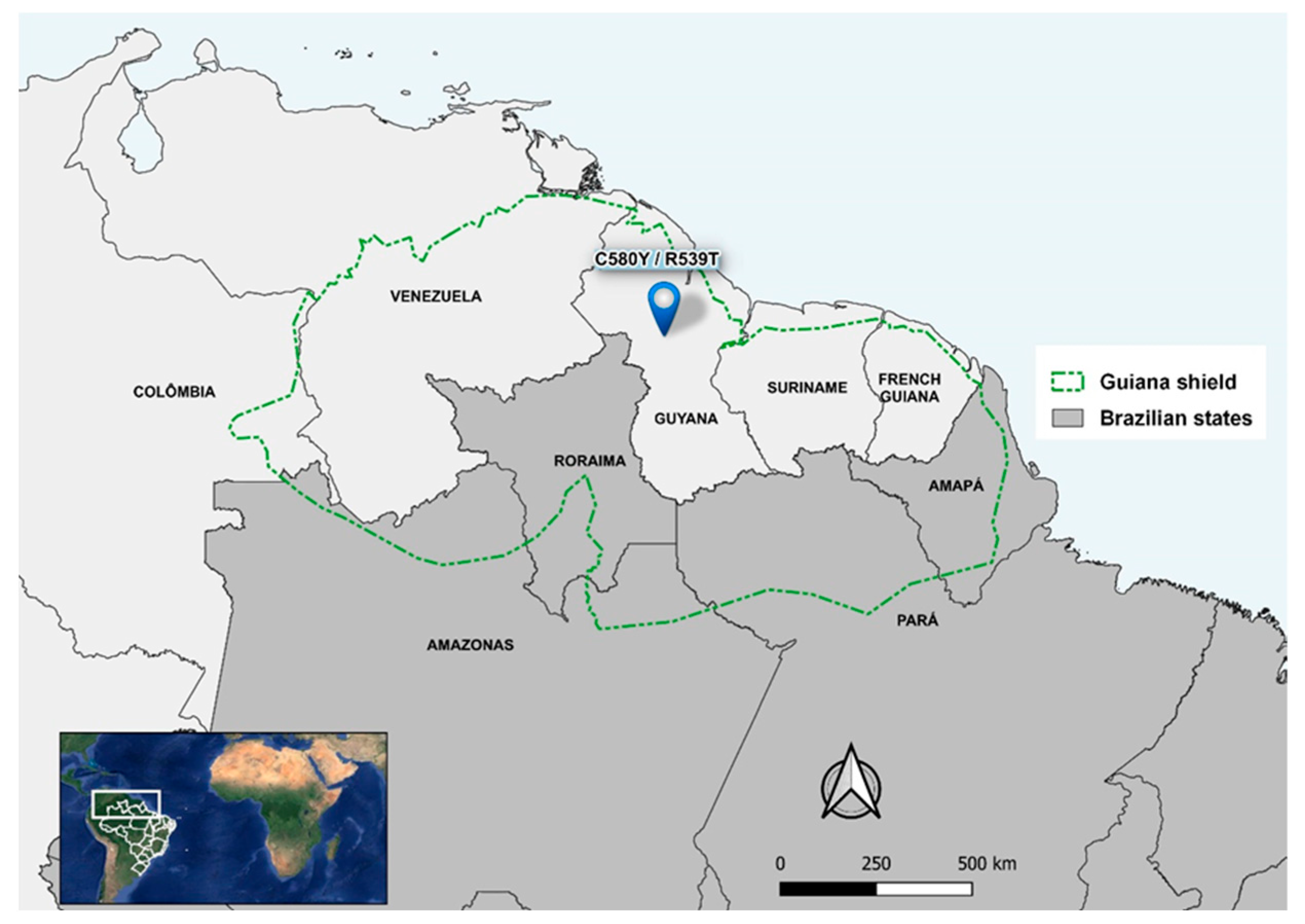
- Chenet, S.M.; Okoth, S.A.; Huber, C.S.; Chandrabose, J.; Lucchi, N.W.; Talundzic, E.; Krishnalall, K.; Ceron, N.; Musset, L.; de Oliveira, A.M.; et al. Independent Emergence of the Plasmodium falciparum Kelch Propeller Domain Mutant Allele C580Y in Guyana. J. Infect. Dis. 2016, 213, 1472–1475. [Google Scholar] [CrossRef] [PubMed]
- Heemskerk, M.; Duijves, C. Small-scale gold mining and conflict in Suriname. In Small-Scale Gold Mining in the Transboundary Areas of Brazil, Suriname and French Guiana; Social and Environmental Issues; United Nations Development Programme: Report Paramaribo, Suriname, 2011; pp. 85–101. [Google Scholar]
- Douine, M.; Musset, L.; Corlin, F.; Pelleau, S.; Pasquier, J.; Mutricy, L. Prevalence of Plasmodium spp. in illegal gold miners in French Guiana in 2015: A hidden but critical malaria reservoir. Malar. J. 2016, 15, 315. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, L.C.; Singh, P.; Monteiro, W.M.; Magris, M.; Cox, H.; Lazrek, Y. Kelch13 mutations in Plasmodium falciparum and risk of spreading in Amazon basin countries. J. Antimicrob. Chemother. 2021, 76, 2854–2862. [Google Scholar] [CrossRef] [PubMed]
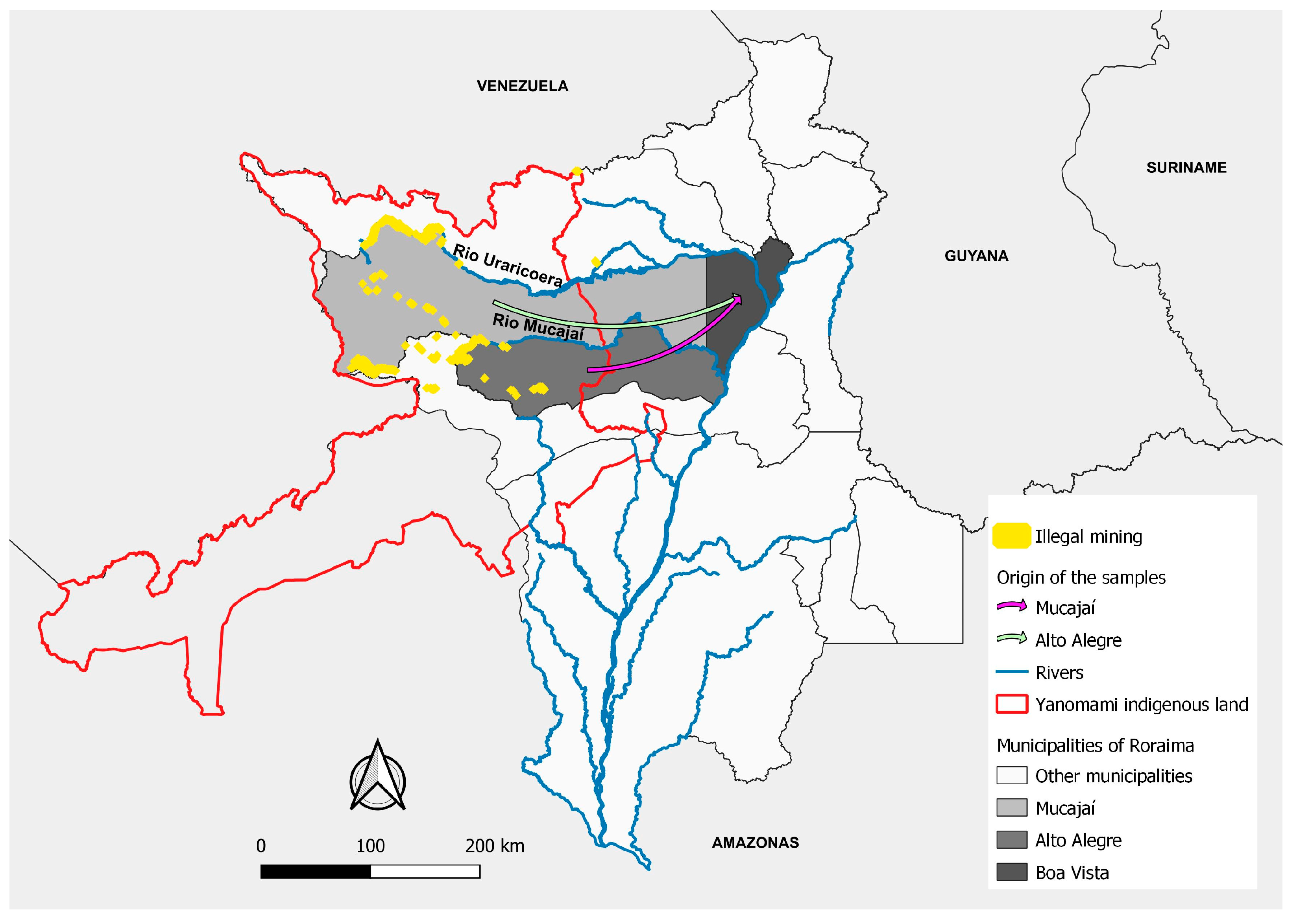
- De Aguiar Barros, J.; Granja, F.; Pequeno, P.; Marchesini, P.; Ferreira da Cruz, M.F. Gold miners augment malaria transmission in indigenous territories of Roraima state, Brazil. Malar. J. 2022, 21, 358. [Google Scholar] [CrossRef] [PubMed]
- Recht, J.; Siqueira, A.M.; Monteiro, W.M.; Herrera, S.M.; Herrera, S.; Lacerda, M.V.G. Malaria in Brazil, Colombia, Peru and Venezuela: Current challenges in malaria control and elimination. Malar. J. 2017, 16, 273. [Google Scholar] [CrossRef] [PubMed]
- Yanomami, H.A.; Wnasseduume, A. Amazonia; Hutukara Associação Yanomami & Associação Wanasseduume Ye’kwana: Boa Vista, Roraima, Brazil, 2021; 52p. [Google Scholar]
- Nacher, M.; Guérin, P.J.; Demar-Pierre, M.; Djossou, F.; Nosten, F.; Carme, B. Made in Europe: Will artemisinin resistance emerge in French Guiana? Malar. J. 2013, 12, 152. [Google Scholar] [CrossRef]
- Yan, S.D.; Orkis, J.; Khan Sohail, S.; Davis, T.; Storey, J.D. Digging for care-seeking behaviour among gold miners in the Guyana hinterland: A qualitative doer non-doer analysis of social and behavioural motivations for malaria testing and treatment. Malar. J. 2020, 19, 235. [Google Scholar] [CrossRef]
- Mvumbi, D.M.; Kayembe, J.M.; Situakibanza, H.; Bobanga, T.L.; Nsibu, C.N.; Mvumbi, G.L. Falciparum malaria molecular drug resistance in the Democratic Republic of Congo: A systematic review. Malar. J. 2015, 14, 354. [Google Scholar] [CrossRef]
- Costa, G.L.; Amaral, L.C.; Fontes, C.J.F.; Carvalho, L.H.; de Brito, C.F.A.; de Sousa, T.N. Assessment of copy number variation in genes related to drug resistance in Plasmodium vivax and Plasmodium falciparum isolates from the Brazilian Amazon and a systematic review of the literature. Malar. J. 2017, 16, 152. [Google Scholar] [CrossRef]
- Pan American Health Organization. Manual de Referencia Para la Vigilancia, El Seguimiento y La Evaluación de La Malaria; Pan American Health Organization: Washington, DC, USA, 2018. [Google Scholar]
- Pacheco, M.A.; Forero-Peña, D.A.; Schneider, K.A.; Chavero, M.; Gamardo, A.; Figuera, L.; Kadakia, E.R.; Grillet, M.; Oliveira-Ferreira, J.; Escalante, A. Malaria in Venezuela: Changes in the complexity of infection reflects the increment in transmission intensity. Malar. J. 2020, 19, 176. [Google Scholar] [CrossRef] [PubMed]
- de Sales, H.J.; Oliveira, I.A.D.; Galdino, L.K.A. Production of urban space in Boa Vista, RR: From planning to “disordered” expansion. Terra Livre 2022, 1, 6. [Google Scholar]
- Barros, F.S.M.; Horório, N.A. Man biting rate seasonal variation of malaria vectors in Roraima, Brazil. Memórias Do Inst. Oswaldo Cruz 2007, 102, 299–302. [Google Scholar] [CrossRef] [PubMed]
- Ariey, F.; Witkowski, B.; Amaratunga, C.; Beghain, J.; Langlois, A.C.; Khim, N.; Kim, S. A molecular marker of artemisinin-resistant Plasmodium falciparum malaria. Nature. 2014, 505, 50–55. [Google Scholar] [CrossRef] [PubMed]
- MapBiomas Project—Collection 7.0 of the 2021 Annual Series of Land Use and Coverage Maps of Brazil. Available online: https://brasil.mapbiomas.org/colecoes-mapbiomas/. (accessed on 1 September 2023).
- IBGE—Brazilian Institute of Geography and Statistics. Vectors of Geopolitical Limits, of Indigenous Lands. Available online: https://www.ibge.gov.br/geociencias/downloads-geociencias.html (accessed on 1 September 2023).
- De-Aguiar-Barros, J.; Silva, D.S.; Citó, A.C.; Peterka, C.; Ferreira-da-Cruz, M.F. A snapshot of a representative Brazilian state of illegal mining in indigenous areas during the era of malaria elimination. CSP 2024, in press. [Google Scholar]
- Murta, F.L.G.; Marques, L.L.G.; Santos, A.P.C.; Batista, T.S.B.; Mendes, M.O.; Silva, E.D. Perceptions about malaria among Brazilian gold miners in an Amazonian border area: Perspectives for malaria elimination strategies. Malar. J. 2021, 20, 286. [Google Scholar] [CrossRef]
- Rosenthal, P.J.; Asua, V.; Conrad, M.D. Emergence, transmission dynamics and mechanisms of artemisinin partial resistance in malaria parasites in Africa. Nat. Rev. Microbiol. 2024, 6, 373–384. [Google Scholar] [CrossRef] [PubMed]
- Inoue, J.; Jovel, I.; Morris, U.; Aydin-Schmidt, B.; Islam, A.; Segurado, A.C. Absence of Plasmodium falciparum K13 Propeller Domain Polymorphisms among Field Isolates Collected from the Brazilian Amazon Basin between 1984 and 2011. Am. J. Trop. Med. Hyg. 2018, 99, 1504–1507. [Google Scholar] [CrossRef]
- Mathieu, L.C.; Cox, H.; Early, A.M.; Mok, S.; Lazrek, Y.; Paquet, J.C.; Ade, M.P.; Lucchi, N.W.; Grant, Q.; Udhayakumar, V.; et al. Local emergence in Amazonia of Plasmodium falciparum k13 C580Y mutants associated with in vitro artemisinin resistance. eLife 2020, 9, e51015. [Google Scholar] [CrossRef]
- Hassett, M.R.; Roepe, P.D. Origin and Spread of Evolving Artemisinin-Resistant Plasmodium falciparum Malarial Parasites in Southeast Asia. Am. J. Trop. Med. Hyg. 2019, 101, 1204–1211. [Google Scholar] [CrossRef]
- Huang, F.; Yan, H.; Xue, J.B.; Cui, Y.W.; Zhou, S.S.; Xia, Z.G.; Abeyasinghe, R.; Ringwald, P.; Zhou, X.N. Molecular surveillance of pfcrt, pfmdr1 and pfk13-propeller mutations in Plasmodium falciparum isolates imported from Africa to China. Malar. J. 2021, 20, 73. [Google Scholar] [CrossRef] [PubMed]
- Stokes, B.H.; Dhingra, S.K.; Rubiano, K.; Mok, S.; Straimer, J.; Gnädig, N.F.; Deni, I.; Schindler, K.A.; Bath, J.R.; Ward, K.E.; et al. Plasmodium falciparum K13 mutations in Africa and Asia impact artemisinin resistance and parasite fitness. eLife 2021, 10, e66277. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, A.B.B.; de Abreu-Fernandes, R.; Neto, Z.; Jandondo, D.; Almeida-de-Oliveira, N.K.; de Lavigne Mello, A.R.; Morais, J.; Daniel-Ribeiro, C.T.; Menard, D.; Ferreira-da-Cruz, M.F. Pfkelch13 Plasmodium falciparum Mutations in Huambo, Angola. Pathogens 2022, 11, 554. [Google Scholar] [CrossRef]
- Lucchi, N.W.; Abdallah, R.; Louzada, J.; Udhayakumar, V.; Oliveira-Ferreira, J. Molecular Surveillance for Polymorphisms Associated with Artemisinin-Based Combination Therapy Resistance in Plasmodium falciparum Isolates Collected in the State of Roraima, Brazil. Am. J. Trop. Med. Hyg. 2020, 102, 310–312. [Google Scholar] [CrossRef] [PubMed]
- Gomes, L.R.; Lavigne, A.; Peterka, C.L.; Brasil, P.; Ménard, D.; Daniel-Ribeiro, C.T.; Ferreira-da-Cruz, M.F. Absence of K13 Polymorphism in Plasmodium falciparum from Brazilian Areas Where the Parasite Is Endemic. Antimicrob. Agents Chemother. 2018, 62, e00354-18. [Google Scholar] [CrossRef]
- Itoh, M.; Negreiros do Valle, S.; Farias, S.; Holanda de Souza, T.M.; Rachid Viana, G.M.; Lucchi, N. Efficacy of Artemether-Lumefantrine for Uncomplicated Plasmodium falciparum Malaria in Cruzeiro do Sul, Brazil, 2016. Am. J. Trop. Med. Hyg. 2018, 98, 88–94. [Google Scholar] [CrossRef]
- WWARN K13 Genotype-Phenotype Study Group. Association of mutations in the Plasmodium falciparum Kelch13 gene (Pf3D7_1343700) with parasite clearance rates after artemisinin-based treatments-a WWARN individual patient data meta-analysis. BMC Med. 2019, 17, 1. [Google Scholar]
- Olivera, M.J.; Guerra, A.P.; Cortes, L.J.; Horth, R.Z.; Padilla, J.; Novoa, J.; Ade, M.P.; Ljolje, D.; Lucchi, N.W.; Marquiño, W.; et al. Artemether-Lumefantrine Efficacy for the Treatment of Uncomplicated Plasmodium falciparum Malaria in Choco, Colombia after 8 Years as First-Line Treatment. Am. J. Trop. Med. Hyg. 2020, 102, 1056–1063. [Google Scholar] [CrossRef]
- Owoloye, A.; Olufemi, M.; Idowu, E.T.; Oyebola, K.M. Prevalence of potential mediators of artemisinin resistance in African isolates of Plasmodium falciparum. Malar. J. 2021, 20, 451. [Google Scholar] [CrossRef] [PubMed]
- Paloque, L.; Coppée, R.; Stokes, B.H.; Gnädig, N.F.; Niaré, K.; Augereau, J.M.; Fidock, D.A.; Clain, J.; Benoit-Vical, F. Mutation in the Plasmodium falciparum BTB/POZ Domain of K13 Protein Confers Artemisinin Resistance. Antimicrob. Agents Chemother. 2022, 66, e0132021. [Google Scholar] [CrossRef] [PubMed]
- Ullah, I.; Farringer, M.A.; Burkhard, A.Y.; Hathaway, E.; Willett, B.C.; Khushu, M. Artemisinin resistance mutations in Pfcoronin impede hemoglobin uptake. bioRxiv 2023, arXiv:bioRxiv:2023.12.22.572193. [Google Scholar]
- Demas, A.R.; Sharma, A.I.; Wong, W.; Early, A.M.; Redmond, S.; Bopp, S.; Neafsey, D.E.; Volkman, S.K.; Hartl, D.L.; Wirth, D.F. Mutations in Plasmodium falciparum actin-binding protein coronin confer reduced artemisinin susceptibility. Proc. Natl. Acad. Sci. USA 2018, 115, 12799–12804. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Aguiar-Barros, J.; Granja, F.; de Abreu-Fernandes, R.; de Queiroz, L.T.; da Silva e Silva, D.; Citó, A.C.; Mocelin, N.K.A.-d.-O.; Daniel-Ribeiro, C.T.; Ferreira-da-Cruz, M.d.F. Molecular Surveillance of Artemisinin-Resistant Plasmodium falciparum Parasites in Mining Areas of the Roraima Indigenous Territory in Brazil. Int. J. Environ. Res. Public Health 2024, 21, 679. https://doi.org/10.3390/ijerph21060679
de Aguiar-Barros J, Granja F, de Abreu-Fernandes R, de Queiroz LT, da Silva e Silva D, Citó AC, Mocelin NKA-d-O, Daniel-Ribeiro CT, Ferreira-da-Cruz MdF. Molecular Surveillance of Artemisinin-Resistant Plasmodium falciparum Parasites in Mining Areas of the Roraima Indigenous Territory in Brazil. International Journal of Environmental Research and Public Health. 2024; 21(6):679. https://doi.org/10.3390/ijerph21060679
Chicago/Turabian Stylede Aguiar-Barros, Jacqueline, Fabiana Granja, Rebecca de Abreu-Fernandes, Lucas Tavares de Queiroz, Daniel da Silva e Silva, Arthur Camurça Citó, Natália Ketrin Almeida-de-Oliveira Mocelin, Cláudio Tadeu Daniel-Ribeiro, and Maria de Fátima Ferreira-da-Cruz. 2024. "Molecular Surveillance of Artemisinin-Resistant Plasmodium falciparum Parasites in Mining Areas of the Roraima Indigenous Territory in Brazil" International Journal of Environmental Research and Public Health 21, no. 6: 679. https://doi.org/10.3390/ijerph21060679
APA Stylede Aguiar-Barros, J., Granja, F., de Abreu-Fernandes, R., de Queiroz, L. T., da Silva e Silva, D., Citó, A. C., Mocelin, N. K. A.-d.-O., Daniel-Ribeiro, C. T., & Ferreira-da-Cruz, M. d. F. (2024). Molecular Surveillance of Artemisinin-Resistant Plasmodium falciparum Parasites in Mining Areas of the Roraima Indigenous Territory in Brazil. International Journal of Environmental Research and Public Health, 21(6), 679. https://doi.org/10.3390/ijerph21060679







