Being Cynical Is Bad for Your Wellbeing: A Structural Equation Model of the Relationship Between Cynicism and Mental Health in First Responders in South Africa
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instruments
2.3. Ethics
2.4. Data Analyses
- Chi-squared (χ2), which should be non-significant; however, this would indicate a perfect fit [60].
- Relative chi-squared (χ2/df); a value ≤3 indicates good fit.
- Comparative fit index (CFI), which should be ≥0.90 [59].
- Root mean square error of approximation (RMSEA), which should be ≤0.08.
- Standardized root mean square residual (SRMR), which should be ≤0.08.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Šmigelskas, K.; Joffė, R.; Jonynienė, J.; Julkunen, J.; Kauhanen, J. High levels of cynical distrust partly predict premature mortality in middle-aged to ageing men. J. Behav. Med. 2017, 40, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Kachel, T.; Huber, A.; Strecker, C.; Höge, T.; Höfer, S. Development of Cynicism in Medical Students: Exploring the Role of Signature Character Strengths and Well-Being. Front. Psychol. 2020, 11, 328. [Google Scholar] [CrossRef] [PubMed]
- Turner, J.H.; Valentine, S.R. Cynicism as a fundamental dimension of moral decision-making: A scale development. J. Bus. Ethics 2001, 34, 123–136. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. Maslach Burnout Inventory Manual; Consulting Psychologists Press: Palo Alto, CA, USA, 1996. [Google Scholar]
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry 2016, 15, 103–111. [Google Scholar] [CrossRef]
- Shalaby, R.; Oluwasina, F.; Eboreime, E.; El Gindi, H.; Agyapong, B.; Hrabok, M.; Dhanoa, S.; Kim, E.; Nwachukwu, I.; Abba-Aji, A.; et al. Burnout among Residents: Prevalence and Predictors of Depersonalization, Emotional Exhaustion and Professional Unfulfillment among Resident Doctors in Canada. Int. J. Environ. Res. Public Health 2023, 20, 3677. [Google Scholar] [CrossRef]
- Dangel, T.J.; Webb, J.R.; Hirsch, J.K. Forgiveness and Suicidal Behavior: Cynicism and Psychache as Serial Mediators. J. Psychol. 2018, 152, 77–95. [Google Scholar] [CrossRef]
- Abraham, R. Organizational cynicism: Bases and consequences. Genet. Soc. Gen. Psychol. Monogr. 2000, 126, 269–292. [Google Scholar]
- Atalay, M.O.; Aydemir, P.; Acuner, T. The Influence of Emotional Exhaustion on Organizational Cynicism: The Sequential Mediating Effect of Organizational Identification and Trust in Organization. SAGE Open 2022, 12, 215824402210933. [Google Scholar] [CrossRef]
- Pedrosa, J.; Sousa, L.; Valentim, O.; Antunes, V. Organizational culture and nurse’s turnover: A systematic literature review. Int. J. Healthc. Manag. 2021, 14, 1542–1550. [Google Scholar] [CrossRef]
- Elsaied, M. Exploitative leadership and organizational cynicism: The mediating role of emotional exhaustion. Leadersh. Organ. Dev. J. 2022, 43, 25–38. [Google Scholar] [CrossRef]
- Petitta, L.; Ghezzi, V. Remote, Disconnected, or Detached? Examining the Effects of Psychological Disconnectedness and Cynicism on Employee Performance, Wellbeing, and Work-Family Interface. Int. J. Environ. Res. Public Health 2023, 20, 6318. [Google Scholar] [CrossRef] [PubMed]
- Sims, M.; Glover, L.S.M.; Gebreab, S.Y.; Spruill, T.M. Cumulative psychosocial factors are associated with cardiovascular disease risk factors and management among African Americans in the Jackson Heart Study. BMC Public Health 2020, 20, 566. [Google Scholar] [CrossRef] [PubMed]
- Suchy-Dicey, A.; Eyituoyo, H.; O’Leary, M.; Cole, S.A.; Traore, A.; Verney, S.; Howard, B.; Manson, S.; Buchwald, D.; Whitney, P. Psychological and social support associations with mortality and cardiovascular disease in middle-aged American Indians: The Strong Heart Study. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 1421–1433. [Google Scholar] [CrossRef] [PubMed]
- Arbisi, P.A.; Polusny, M.A.; Rusch, L.; Thuras, P.; Erbes, C.R. Does Cynicism Play a Role in Failure to Obtain Needed Care? Mental Health Service Utilization Among Returning U.S. National Guard Soldiers. Psychol. Assess. 2013, 25, 991–996. [Google Scholar] [CrossRef] [PubMed]
- Benincasa, V.; Passannante, M.; Pierrini, F.; Carpinelli, L.; Moccia, G.; Marinaci, T.; Capunzo, M.; Pironti, C.; Genovese, A.; Savarese, G.; et al. Burnout and Psychological Vulnerability in First Responders: Monitoring Depersonalization and Phobic Anxiety during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 2794. [Google Scholar] [CrossRef] [PubMed]
- Tselebis, A.; Sikaras, C.; Milionis, C.; Sideri, E.P.; Fytsilis, K.; Papageorgiou, S.M.; Ilias, I.; Pachi, A. A Moderated Mediation Model of the Influence of Cynical Distrust, Medical Mistrust, and Anger on Vaccination Hesitancy in Nursing Staff. Eur. J. Investig. Health Psychol. Educ. 2023, 13, 2373–2387. [Google Scholar] [CrossRef]
- Bakioğlu, F.; Kiraz, Z. Burnout and wellbeing of teacher candidates: The mediator role of cynicism. An. Psicol. 2019, 35, 521–528. [Google Scholar] [CrossRef]
- Richardsen, A.M.; Burke, R.J.; Martinussen, M. Work and Health Outcomes Among Police Officers: The Mediating Role of Police Cynicism and Engagement. Int. J. Stress Manag. 2006, 13, 555–574. [Google Scholar] [CrossRef]
- Kocoglu, M. Cynicism as a mediator of relations between job stress and work alienation: A study from a developing country—Turkey. Glob. Bus. Manag. Res. 2014, 6, 24–36. [Google Scholar]
- Wylie-Rosett, J.; Aragaki, A.K.; Cochrane, B.; Perri, M.G.; Rosal, M.C.; Rapp, S.R. Cynicism: Incident diabetes and worsening of metabolic syndrome in postmenopausal women. Diabetes Metab Synd 2010, 4, 187–189. [Google Scholar] [CrossRef]
- Ntatamala, I.; Adams, S. The correlates of post-traumatic stress disorder in ambulance personnel and barriers faced in accessing care for work-related stress. Int. J. Environ. Res. Public Health 2022, 19, 2046. [Google Scholar] [CrossRef]
- Fjeldheim, C.B.; Nöthling, J.; Pretorius, K.; Basson, M.; Ganasen, K.; Heneke, R.; Cloete, K.J.; Seedat, S. Trauma exposure, posttraumatic stress disorder and the effect of explanatory variables in paramedic trainees. BMC Emerg. Med. 2014, 14, 11. [Google Scholar] [CrossRef] [PubMed]
- Schuurman, N.; Cinnamon, J.; Walker, B.B.; Fawcett, V.; Nicol, A.; Hameed, S.M.; Matzopoulos, R. Intentional injury and violence in Cape Town, South Africa: An epidemiological analysis of trauma admissions data. Glob. Health Act. 2015, 8, 27016. [Google Scholar] [CrossRef] [PubMed]
- Ponder, W.N.; Walters, K.; Simons, J.S.; Simons, R.M.; Jetelina, K.K.; Carbajal, J. Network analysis of distress, suicidality, and resilience in a treatment seeking sample of first responders. J. Affect. Disord. 2023, 320, 742–750. [Google Scholar] [CrossRef]
- Masson, F.; Moodley, J. Secondary Traumatic Stress: The Experiences of Social Workers in the South African Police Service. Practice 2020, 32, 169–189. [Google Scholar] [CrossRef]
- Smith, A.J.; Weisenbach, S.L.; Jones, R.T.; Ferreira, R.J.; Bride, B.E. Cynicism Among Veterans Who Struggle to Adapt to Life After Combat: Towards an Understanding of Adaptive Functions and Maladaptive Consequences. Traumatology 2018, 24, 17–26. [Google Scholar] [CrossRef]
- Huang, G.; Chu, H.; Chen, R.; Liu, D.; Banda, K.J.; O’Brien, A.P.; Jen, H.-J.; Chiang, K.-J.; Chiou, J.-F.; Chou, K.-R. Prevalence of depression, anxiety, and stress among first responders for medical emergencies during COVID-19 pandemic: A meta-analysis. J. Glob. Health 2022, 12, 05028. [Google Scholar] [CrossRef]
- Vujanovic, A.A.; Lebeaut, A.; Leonard, S. Exploring the impact of the COVID-19 pandemic on the mental health of first responders. Cogn. Behav. Ther. 2021, 50, 320–335. [Google Scholar] [CrossRef]
- Hegarty, S.; Lamb, D.; Stevelink, S.A.M.; Bhundia, R.; Raine, R.; Doherty, M.J.; Scott, H.R.; Marie Rafferty, A.; Williamson, V.; Dorrington, S.; et al. ‘It hurts your heart’: Frontline healthcare worker experiences of moral injury during the COVID-19 pandemic. Eur. J. Psychotraumatol. 2022, 13, 2128028. [Google Scholar] [CrossRef]
- Harper, S.; Karypidou, A. Moral Suffering in Frontline Social Care Workers: A Study of Moral Injury and Moral Distress. Eur. J. Ment. Health 2024, 19, e0021. [Google Scholar] [CrossRef]
- Williamson, V.; Murphy, D.; Greenberg, N. COVID-19 and experiences of moral injury in front-line key workers. Occup. Med. 2020, 70, 317–319. [Google Scholar] [CrossRef] [PubMed]
- Stogner, J.; Miller, B.L.; McLean, K. Police Stress, Mental Health, and Resiliency during the COVID-19 Pandemic. Am. J. Crim. Justice 2020, 45, 718–730. [Google Scholar] [CrossRef] [PubMed]
- Syed, S.; Ashwick, R.; Schlosser, M.; Jones, R.; Rowe, S.; Billings, J. Global prevalence and risk factors for mental health problems in police personnel: A systematic review and meta-analysis. Occup. Environ. Med. 2020, 77, 737–747. [Google Scholar] [CrossRef]
- Purba, A.; Demou, E. The relationship between organisational stressors and mental wellbeing within police officers: A systematic review. BMC Public Health 2019, 19, 1286. [Google Scholar] [CrossRef]
- Bezabh, Y.H.; Abebe, S.M.; Fanta, T.; Tadese, A.; Tulu, M. Prevalence and associated factors of post-traumatic stress disorder among emergency responders of Addis Ababa Fire and Emergency Control and Prevention Service Authority, Ethiopia: Institution-based, cross-sectional study. BMJ Open 2018, 8, e020705. [Google Scholar] [CrossRef]
- Barnett, C.; Anum, A.; Acquah, B.; Dzokoto, V. Do police experience trauma during routine work? An analysis of work-related potentially traumatic events and expressed trauma in a sample of Ghanaian police officers. Police Pract. Res. 2022, 23, 80–94. [Google Scholar] [CrossRef]
- O’Neil, J.W.; Kruger, L. Mindset as a resilience resource and perceived wellness of first responders in a South African context. JAMBA 2022, 14, 1312. [Google Scholar] [CrossRef]
- Ward, C.L.; Lombard, C.J.; Gwebushe, N. Critical incident exposure in South African emergency services personnel: Prevalence and associated mental health issues. Emerg. Med. J. 2006, 23, 226–231. [Google Scholar] [CrossRef]
- Kadhum, M.; Ayinde, O.O.; Wilkes, C.; Chumakov, E.; Dahanayake, D.; Ashrafi, A.; Kafle, B.; Lili, R.; Farrell, S.; Bhugra, D.; et al. Wellbeing, burnout and substance use amongst medical students: A summary of results from nine countries. Int. J. Soc. Psychiatry 2022, 68, 1218–1222. [Google Scholar] [CrossRef]
- Liang, L.; Hu, Y.; Fei, J.; Yuan, T.; Gao, R.; Yue, J.; Song, Q.; Zhao, X.; Mei, S. Association between burnout and post-traumatic stress disorder among frontline nurse during COVID-19 pandemic: A moderated mediation analysis. J. Clin. Nurs. 2024, 33, 1076–1083. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. The Job Demands-Resources model: State of the art. J. Managerial Psychol. 2007, 22, 309–328. [Google Scholar] [CrossRef]
- Wei, X.; Wang, R.; MacDonald, E. Exploring the Relations between Student Cynicism and Student Burnout. Psychological reports 2015, 117, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Tayfur, O.; Bayhan Karapinar, P.; Metin Camgoz, S.; Glazer, S. The Mediating Effects of Emotional Exhaustion Cynicism and Learned Helplessness on Organizational Justice-Turnover Intentions Linkage. Int. J. Stress Manag. 2013, 20, 193–221. [Google Scholar] [CrossRef]
- Prajogo, W.; Wijaya, N.H.S.; Kusumawati, H. The Relationship of Organisational Cynicism, Emotional Exhaustion, Creative Work Involvement and InRole Performance. Int. J. Innov. Creat. Chang. 2020, 12, 201–214. [Google Scholar]
- Bang, H.; Reio, T.G. Examining the role of cynicism in the relationships between burnout and employee behavior. Rev. Psicol. Trab. Organ. 2017, 33, 217–227. [Google Scholar] [CrossRef]
- Chalder, T.; Berelowitz, G.; Pawlikowska, T.; Watts, L.; Wessely, S.; Wright, D.; Wallace, E.P. Development of a fatigue scale. J. Psychosom. Res. 1993, 37, 147–153. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Coetzee, B.; Loades, M.E.; Du Toit, S.; Read, R.; Kagee, A. Fatigue among South African adolescents living with HIV: Is the Chalder Fatigue Questionnaire a suitable measure and how common is fatigue? Vulnerable Child. Youth Stud. 2018, 13, 305–316. [Google Scholar] [CrossRef]
- Makhubela, M.; Khumalo, I.P. Psychometric evaluation of the PHQ-9 in university students: Factorial validity and measurement equivalence across three African countries. Curr. Psychol. 2023, 42, 18061–18069. [Google Scholar] [CrossRef]
- Smith Fawzi, M.C.; Ngakongwa, F.; Liu, Y.; Rutayuga, T.; Siril, H.; Somba, M.; Kaaya, S.F. Validating the Patient Health Questionnaire-9 (PHQ-9) for screening of depression in Tanzania. Neurol. Psychiatry Brain Res. 2019, 31, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Obadeji, A.; Oluwole, L.O.; Dada, M.U.; Ajiboye, A.S.; Kumolalo, B.F.; Solomon, O.A. Assessment of Depression in a Primary Care Setting in Nigeria using the PHQ-9. J. Family Med. Prim. Care 2015, 4, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Kigozi, G. Construct validity and reliability of the generalised anxiety disorder-7 scale in a sample of tuberculosis patients in the Free State Province, South Africa. S. Afr. J. Infect. Dis. 2021, 36, e1–e6. [Google Scholar] [CrossRef] [PubMed]
- Tadi, N.F.; Pillay, K.; Ejoke, U.P.; Khumalo, I.P. Sex Differences in Depression and Anxiety Symptoms: Measurement Invariance, Prevalence, and Symptom Heterogeneity Among University Students in South Africa. Front. Psychol. 2022, 13, 873292. [Google Scholar] [CrossRef]
- van Wijk, C.H.; Martin, J.H.; Maree, D.J.F. Clinical validation of brief mental health scales for use in South African occupational healthcare. SA J. Ind. Psychol. 2021, 47, e1–e17. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis; Prentice Hall: Englewood Cliffs, NJ, USA, 2010. [Google Scholar]
- Illinois State University SPSS Descriptive Statistics. Available online: https://coursefinder.illinoisstate.edu/psy/138/ (accessed on 8 August 2024).
- Vu, L.G.; Le, L.K.; Dam, A.V.T.; Nguyen, S.H.; Vu, T.T.M.; Trinh, T.T.H.; Do, A.L.; Do, N.M.; Le, T.H.; Latkin, C.; et al. Factor Structures of Patient Health Questionnaire-9 Instruments in Exploring Depressive Symptoms of Suburban Population. Front. Psychiatry 2022, 13, 838747. [Google Scholar] [CrossRef]
- Jöreskog, K.G.; Olsson, U.H.; Wallentin, F.Y. Confirmatory factor analysis (CFA). In Multivariate Analysis with LISREL; Jöreskog, K.G., Olsson, U.H., Wallentin, F.Y., Eds.; Springer: New York, NY, USA, 2016; pp. 283–339. [Google Scholar]
- DeVon, H.A.; Block, M.E.; Moyle-Wright, P.; Ernst, D.M.; Hayden, S.J.; Lazzara, D.J.; Savoy, S.M.; Kostas-Polston, E. A psychometric toolbox for testing validity and reliability. J. Nurs. Scholarsh. 2007, 39, 155–164. [Google Scholar] [CrossRef]
- Lazarus, R.S. Stress and Emotion: A New Synthesis; Springer Publishing Company: New York, NY, USA, 2006. [Google Scholar]
- Beck, A.T.; Emery, G.; Greenberg, R.L. Anxiety Disorders and Phobias: A Cognitive Perspective; Basic Books: New York, NY, USA, 1985. [Google Scholar]
- Manuel, F.-A.; Gustavo Alexis Calderón-De la, C.; Sergio, D.-L. Reduction of Burnout Syndrome in Health Workers through a Cognitive-Behavioural Model-Based Program: A Pilot Study. Psychol. Top. 2022, 31, 585–603. [Google Scholar]
- Ghasemi, F.; Herman, K.C.; Reinke, W.M. A cognitive-behavioral approach to teacher burnout: A randomized controlled trial of a group therapy program. Anxiety Stress Coping 2023, 36, 533–541. [Google Scholar] [CrossRef]
- Riepenhausen, A.; Wackerhagen, C.; Reppmann, Z.C.; Deter, H.-C.; Kalisch, R.; Veer, I.M.; Walter, H. Positive cognitive reappraisal in stress resilience, mental health, and well-being: A comprehensive systematic review. Emot. Rev. 2022, 14, 310–331. [Google Scholar] [CrossRef]
- Caldwell, J.A.; Caldwell, J.L.; Thompson, L.A.; Lieberman, H.R. Fatigue and its management in the workplace. Neurosci. Biobehav. Rev. 2019, 96, 272–289. [Google Scholar] [CrossRef] [PubMed]
- Gotaas, M.E.; Stiles, T.C.; Bjørngaard, J.H.; Borchgrevink, P.C.; Fors, E.A. Cognitive Behavioral Therapy Improves Physical Function and Fatigue in Mild and Moderate Chronic Fatigue Syndrome: A Consecutive Randomized Controlled Trial of Standard and Short Interventions. Front. Psychiatry 2021, 12, 580924. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Cai, J.; Sawhney, R.; Jiang, S.; Buys, N.; Sun, J. The Effectiveness of Cognitive-Behavioral Therapy in Helping People on Sick Leave to Return to Work: A Systematic Review and Meta-analysis. J. Occup. Rehabil. 2024, 34, 4–36. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Tang, L.; Ye, Z.; Zou, P.; Shao, J.; Wu, M.; Zhang, Q.; Qiao, G.; Mu, S. The role of social support and emotional exhaustion in the association between work-family conflict and anxiety symptoms among female medical staff: A moderated mediation model. BMC Psychiatry 2020, 20, 266–269. [Google Scholar] [CrossRef]
- Xu, S.; Ouyang, X.; Shi, X.; Li, Y.; Chen, D.; Lai, Y.; Fan, F. Emotional exhaustion and sleep-related worry as serial mediators between sleep disturbance and depressive symptoms in student nurses: A longitudinal analysis. J. Psychosom. Res. 2020, 129, 109870. [Google Scholar] [CrossRef]
- Santa Maria, A.; Wörfel, F.; Wolter, C.; Gusy, B.; Rotter, M.; Stark, S.; Kleiber, D.; Renneberg, B. The Role of Job Demands and Job Resources in the Development of Emotional Exhaustion, Depression, and Anxiety Among Police Officers. Police Q. 2018, 21, 109–134. [Google Scholar] [CrossRef]

| Variable | Category | n | % | Mean | SD |
|---|---|---|---|---|---|
| Gender | Male | 236 | 56% | ||
| Female | 193 | 45% | |||
| Relationship status | Single | 151 | 35.2% | ||
| Married | 221 | 51.5% | |||
| Divorced/Separated/Widowed | 57 | 13.3% | |||
| Work setting | Urban | 396 | 92.3% | ||
| Peri-urban | 11 | 2.6% | |||
| Rural | 22 | 5.1% | |||
| Age | 39.0 | 9.9 | |||
| Length of service | 13.2 | 9.7 |
| Variable/Scale | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. Cynicism | — | |||
| 2. Depression | 0.21 ** | — | ||
| 3. Anxiety | 0.22 ** | 0.73 ** | — | |
| 4. Fatigue | 0.21 ** | 0.49 ** | 0.50 ** | — |
| Mean | 52.46 | 9.51 | 7.73 | 14.40 |
| SD | 10.16 | 6.42 | 5.86 | 6.80 |
| Skewness | −0.62 | 0.37 | 0.38 | 0.12 |
| Kurtosis | 0.84 | −0.49 | −0.81 | −0.25 |
| α | 0.88 | 0.89 | 0.92 | 0.89 |
| ω | 0.87 | 0.89 | 0.92 | 0.89 |
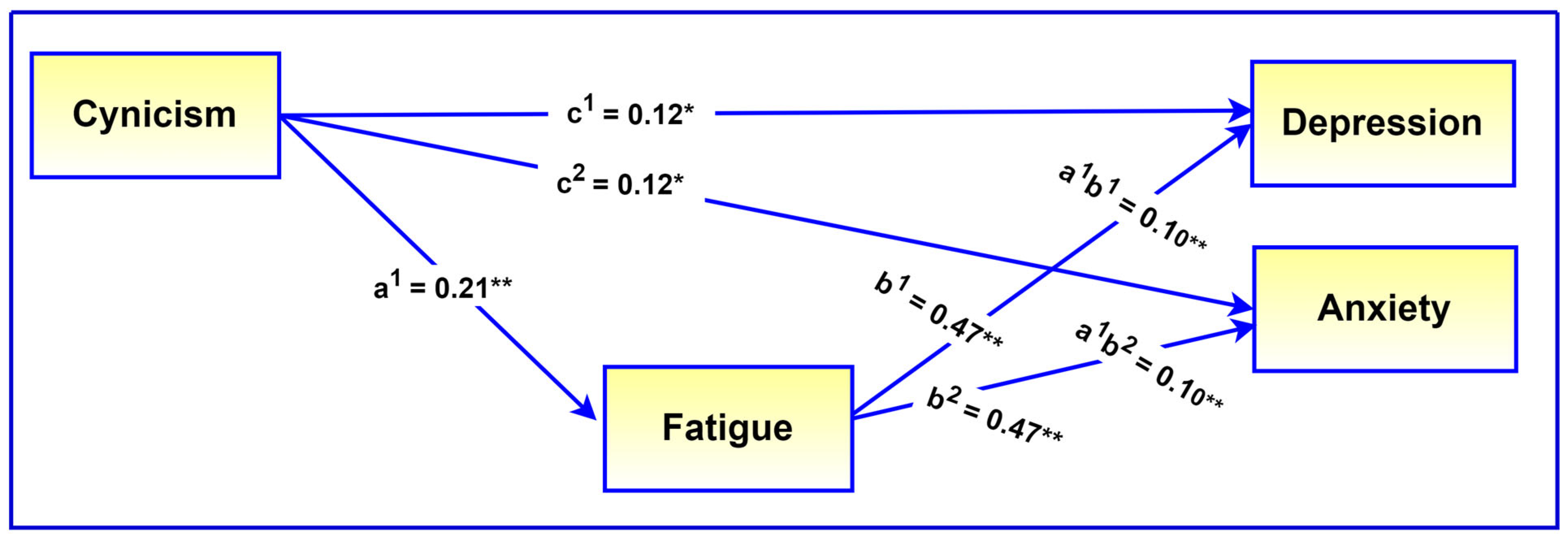
| Effects | B | SE | 95% CI | β | p |
|---|---|---|---|---|---|
| Direct effects | |||||
| Cynicism → Depression | 0.08 | 0.03 | [0.02, 0.13] | 0.12 | 0.005 |
| Cynicism → Anxiety | 0.07 | 0.03 | [0.02, 0.12] | 0.12 | 0.004 |
| Fatigue → Depression | 0.44 | 0.04 | [0.37, 0.51] | 0.47 | <0.001 |
| Fatigue → Anxiety | 0.41 | 0.04 | [0.34, 0.47] | 0.47 | <0.001 |
| Indirect effects | |||||
| Cynicism → Fatigue → Depression | 0.06 | 0.02 | [0.04, 0.09] | 0.10 | <0.001 |
| Cynicism → Fatigue → Depression | 0.06 | 0.02 | [0.04, 0.08] | 0.10 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Padmanabhanunni, A.; Pretorius, T.B. Being Cynical Is Bad for Your Wellbeing: A Structural Equation Model of the Relationship Between Cynicism and Mental Health in First Responders in South Africa. Int. J. Environ. Res. Public Health 2024, 21, 1684. https://doi.org/10.3390/ijerph21121684
Padmanabhanunni A, Pretorius TB. Being Cynical Is Bad for Your Wellbeing: A Structural Equation Model of the Relationship Between Cynicism and Mental Health in First Responders in South Africa. International Journal of Environmental Research and Public Health. 2024; 21(12):1684. https://doi.org/10.3390/ijerph21121684
Chicago/Turabian StylePadmanabhanunni, Anita, and Tyrone B. Pretorius. 2024. "Being Cynical Is Bad for Your Wellbeing: A Structural Equation Model of the Relationship Between Cynicism and Mental Health in First Responders in South Africa" International Journal of Environmental Research and Public Health 21, no. 12: 1684. https://doi.org/10.3390/ijerph21121684
APA StylePadmanabhanunni, A., & Pretorius, T. B. (2024). Being Cynical Is Bad for Your Wellbeing: A Structural Equation Model of the Relationship Between Cynicism and Mental Health in First Responders in South Africa. International Journal of Environmental Research and Public Health, 21(12), 1684. https://doi.org/10.3390/ijerph21121684






