Occupational Risk Factors for Burnout Syndrome Among Healthcare Professionals: A Global Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Registration and Protocol
2.2. Eligibility Criteria
2.3. Information Sources
2.4. Search Strategy
2.5. Selection Process
2.6. Data Collection Process
2.7. Data Items
2.8. Study Risk of Bias Assessment
2.9. Effect Measures
2.10. Synthesis Methods
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias in Studies
4. Results of Individual Studies
5. Results of Syntheses
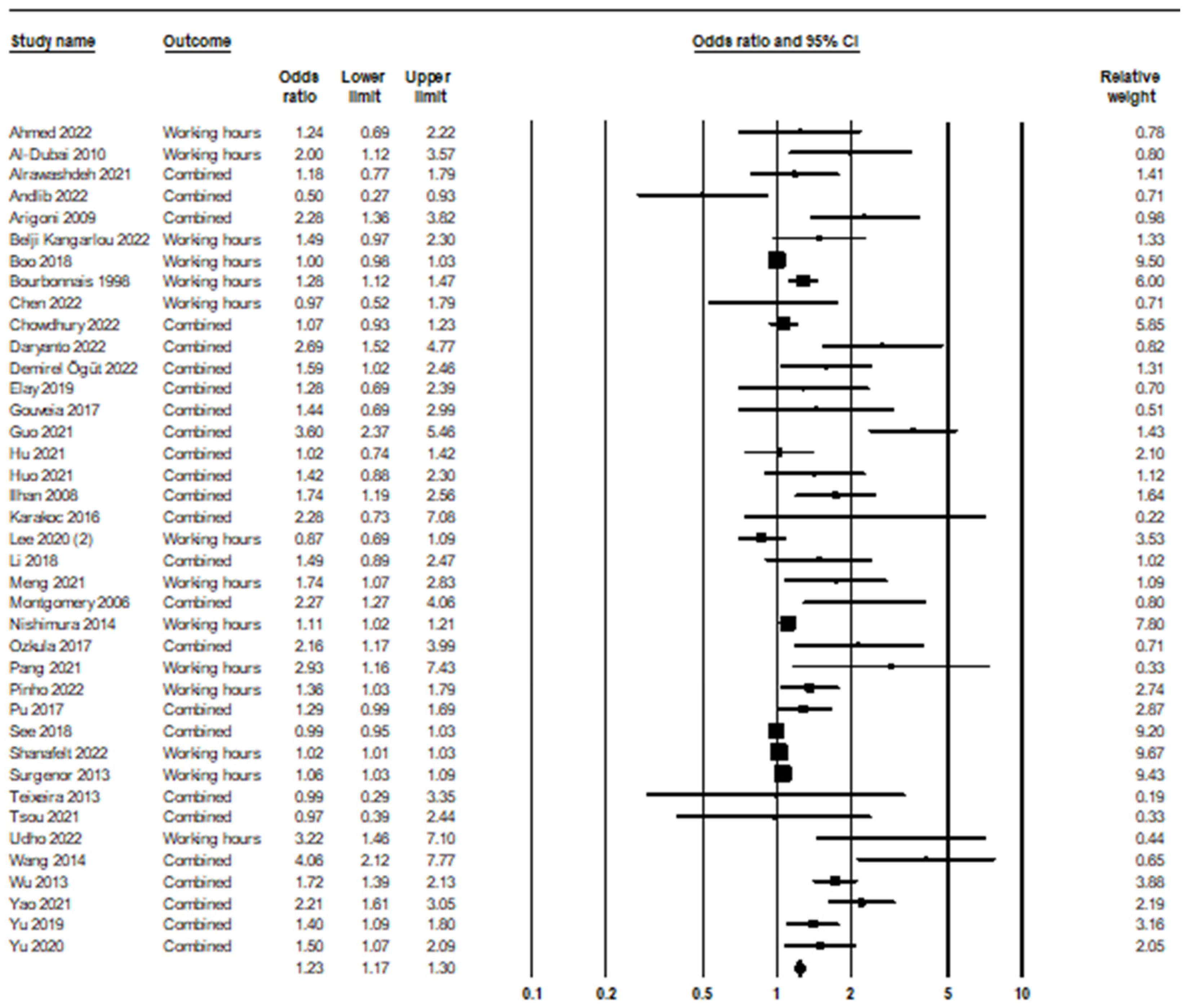
5.1. Long Working Hours and Burnout Syndrome
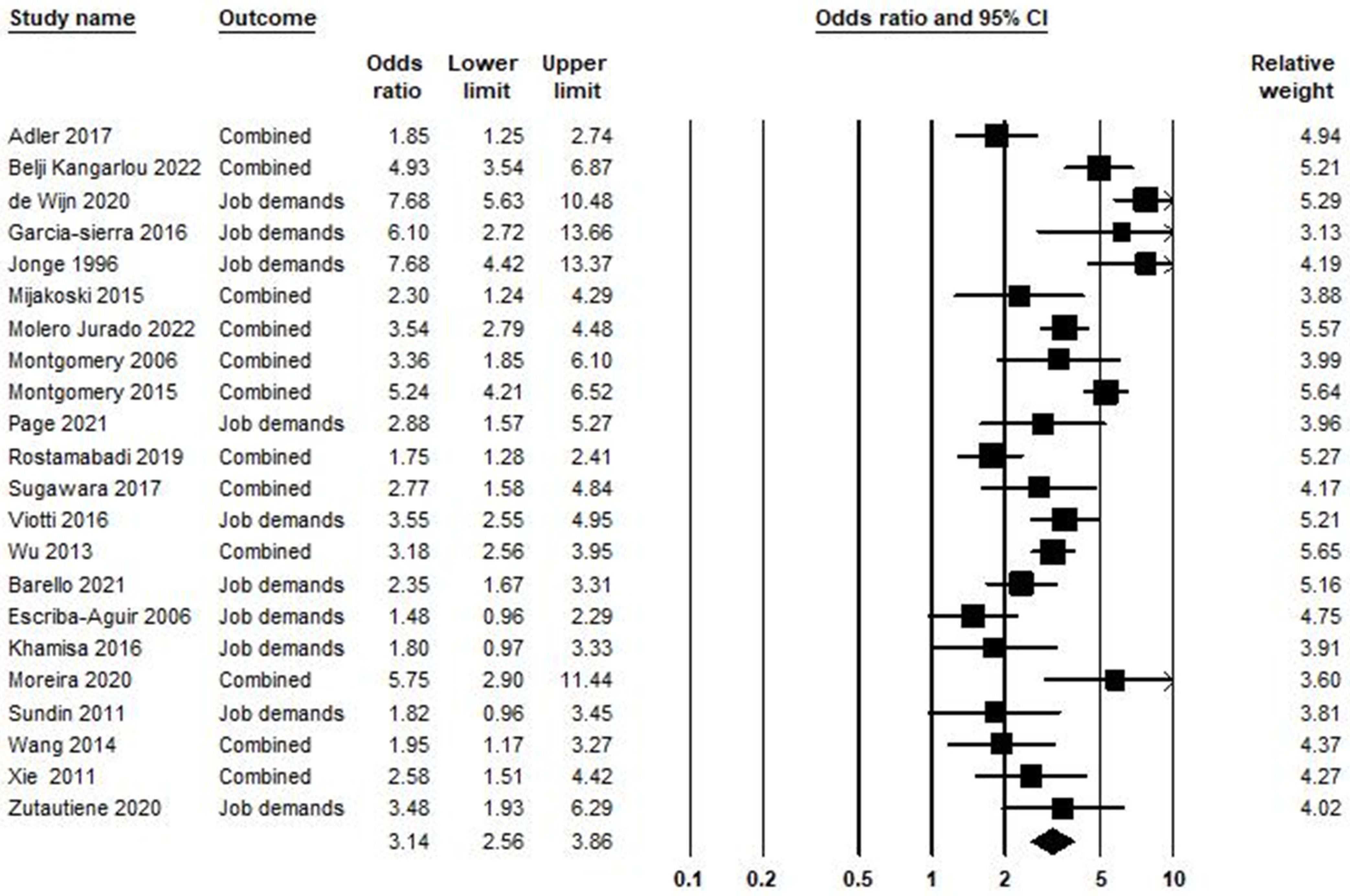
5.2. Job Demand and Burnout Syndrome
5.3. Workload and Burnout Syndrome
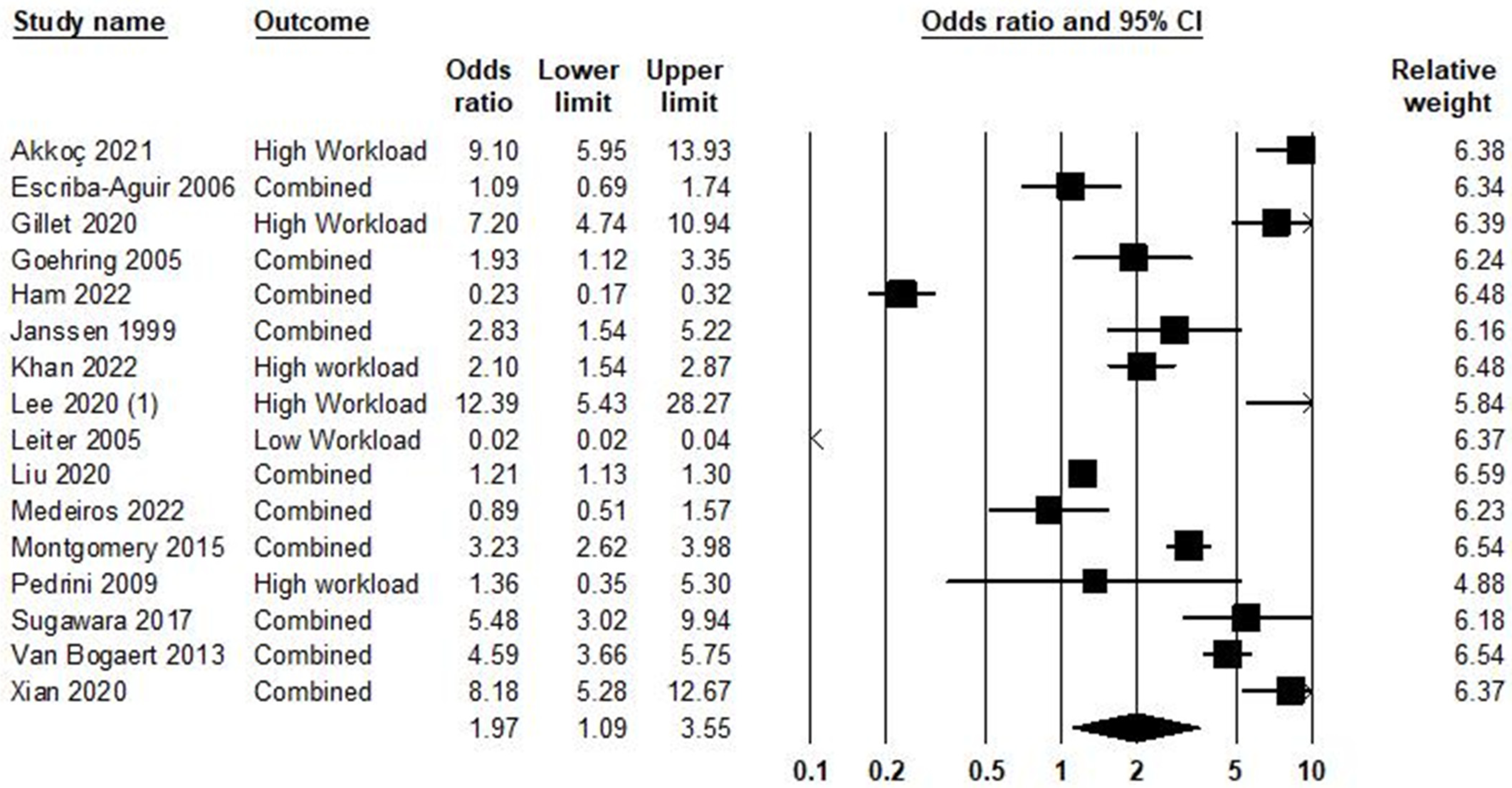
5.4. Job Stress and Burnout Syndrome
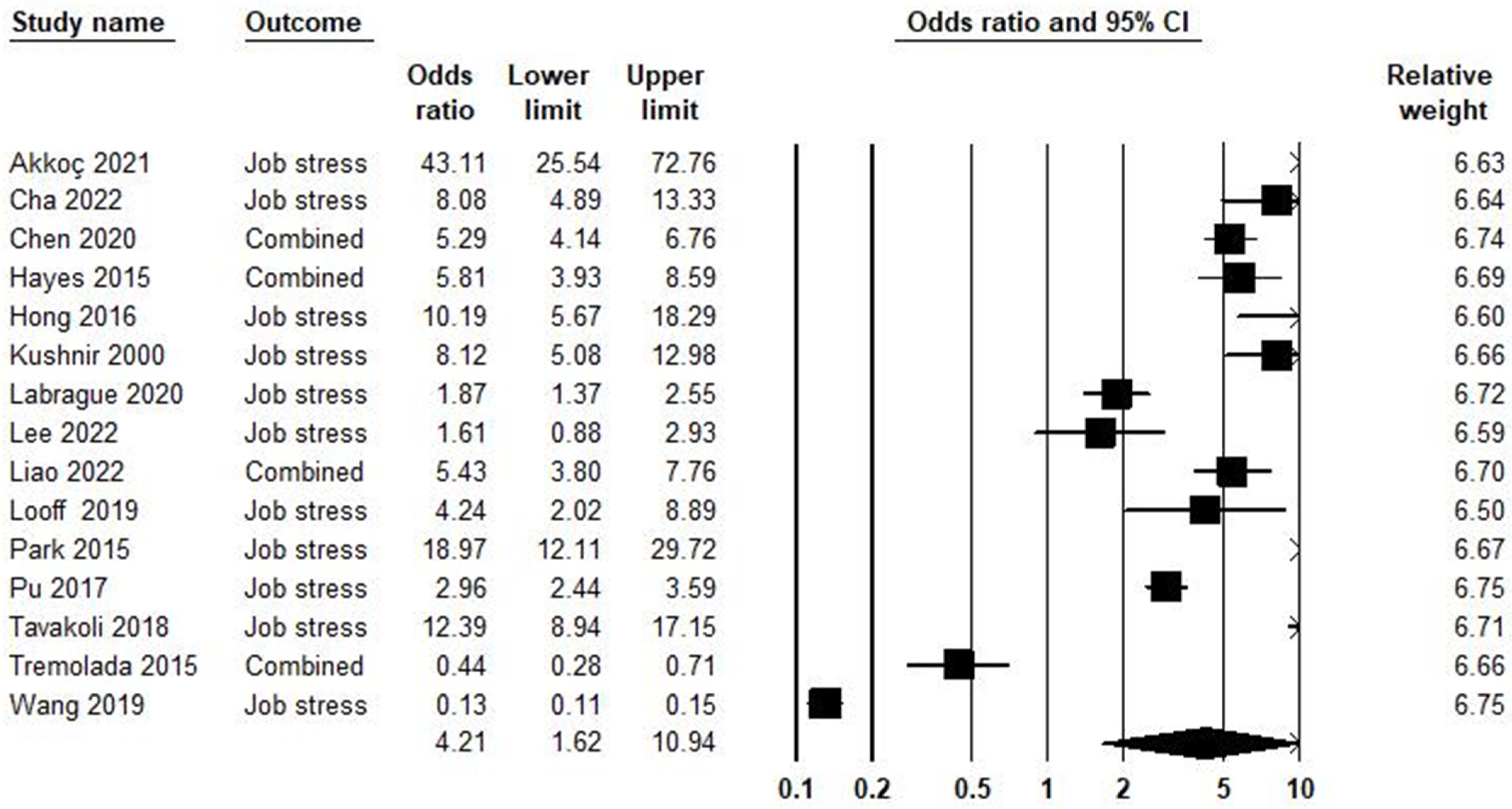
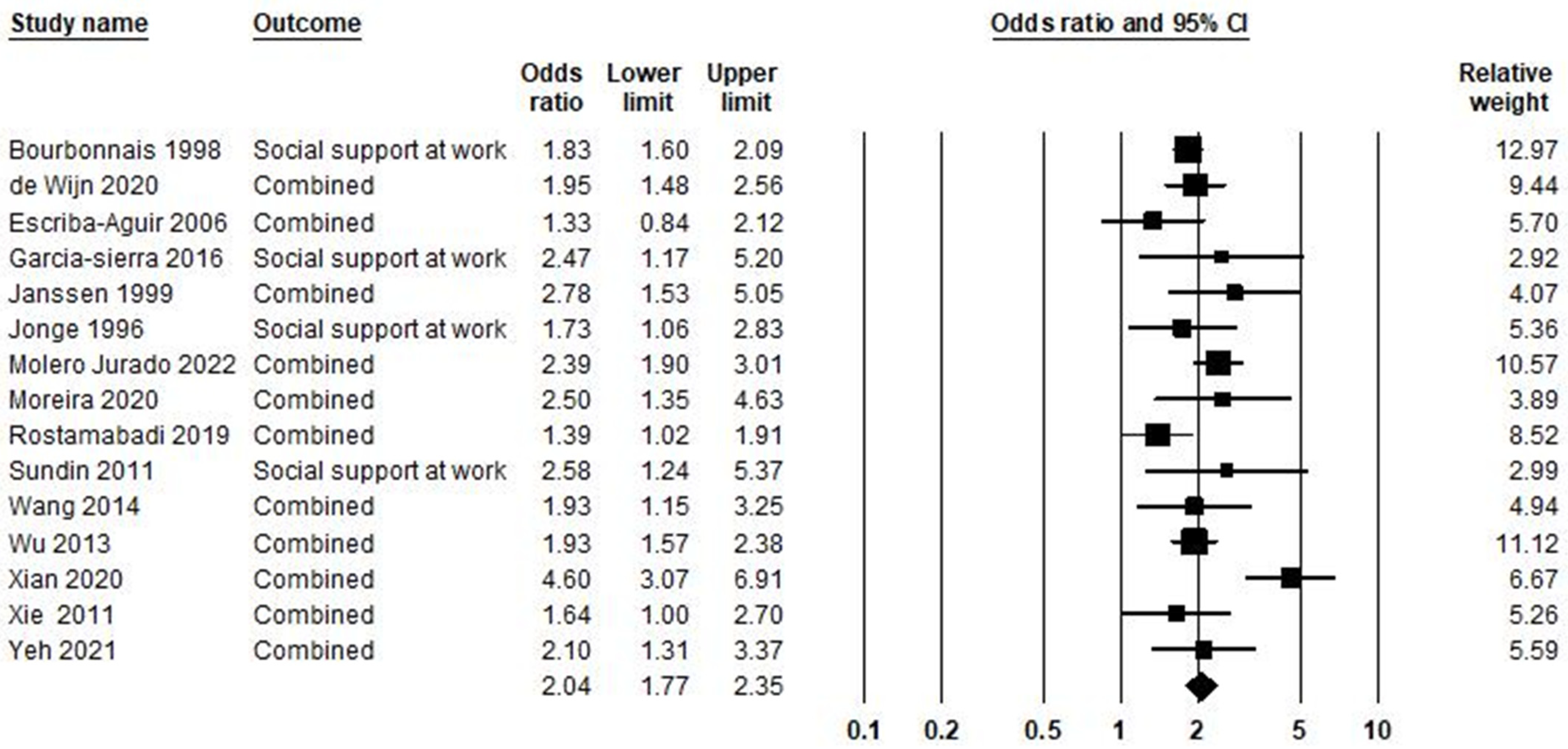
5.5. Low Social Support at Work and Burnout Syndrome
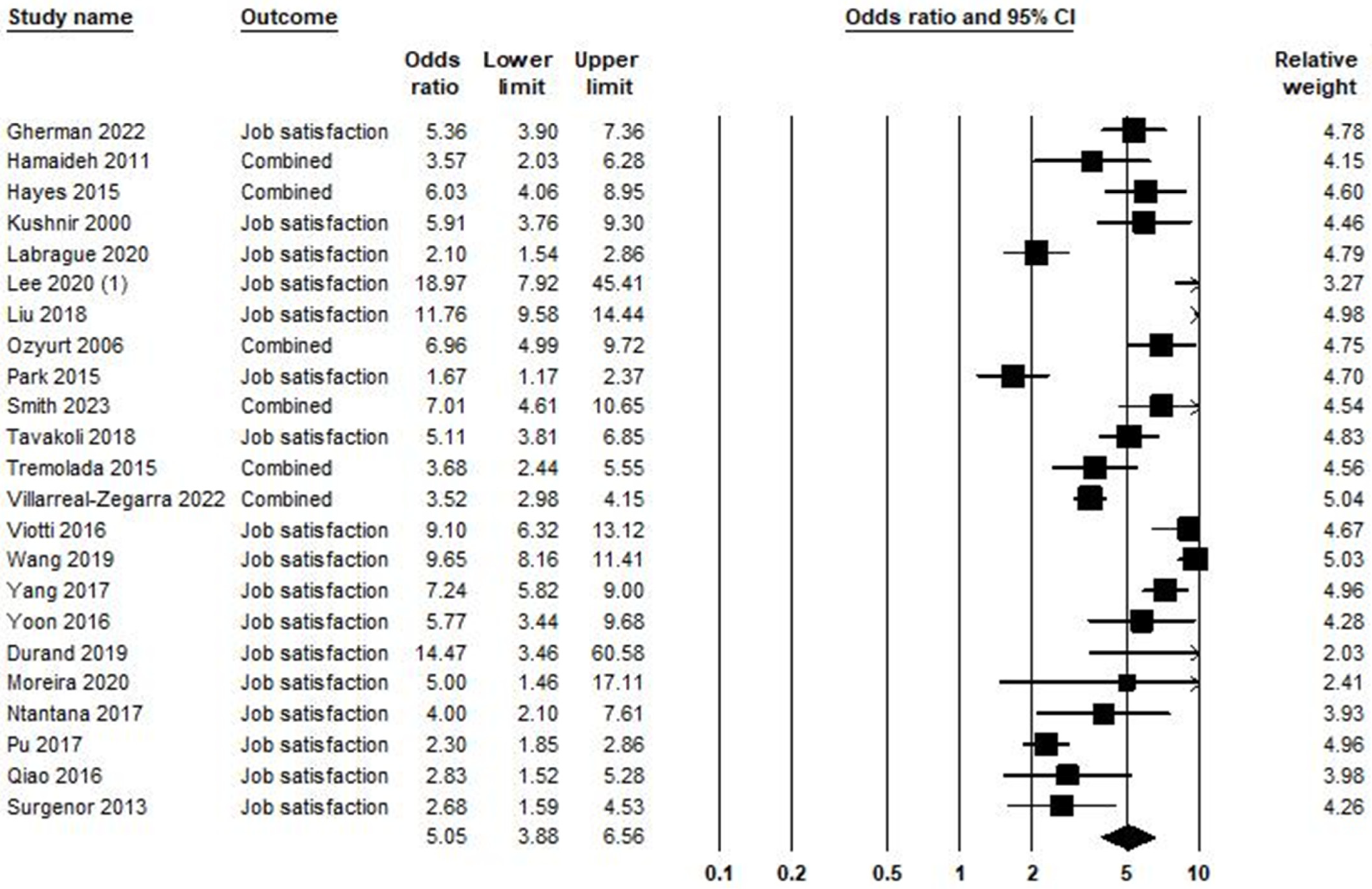
5.6. Low Job Satisfaction and Burnout Syndrome
5.7. Job Control and Burnout Syndrome
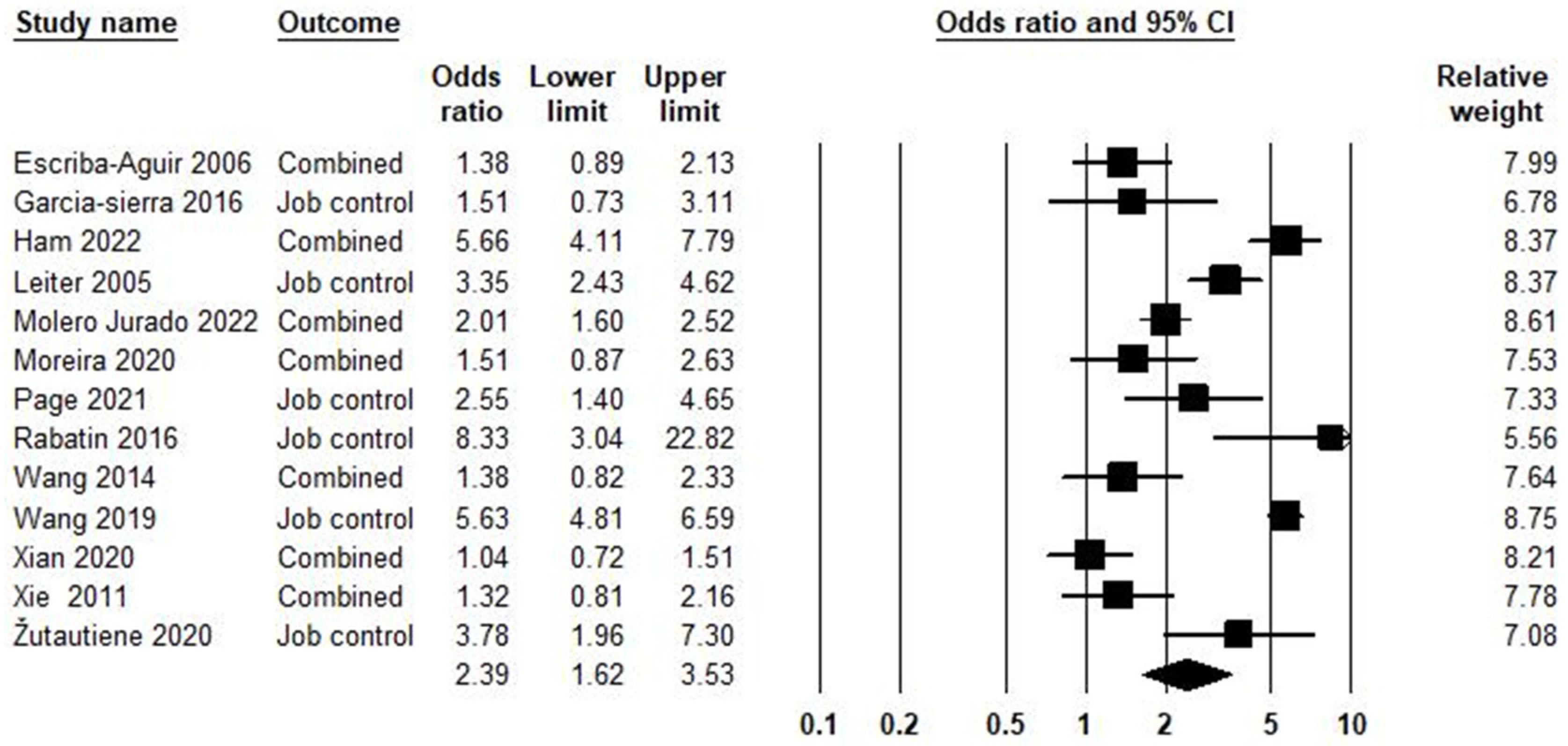
5.8. Work–Life Imbalance and Burnout Syndrome
5.9. Effort–Reward Imbalance, Other Stressors, and Burnout Syndrome
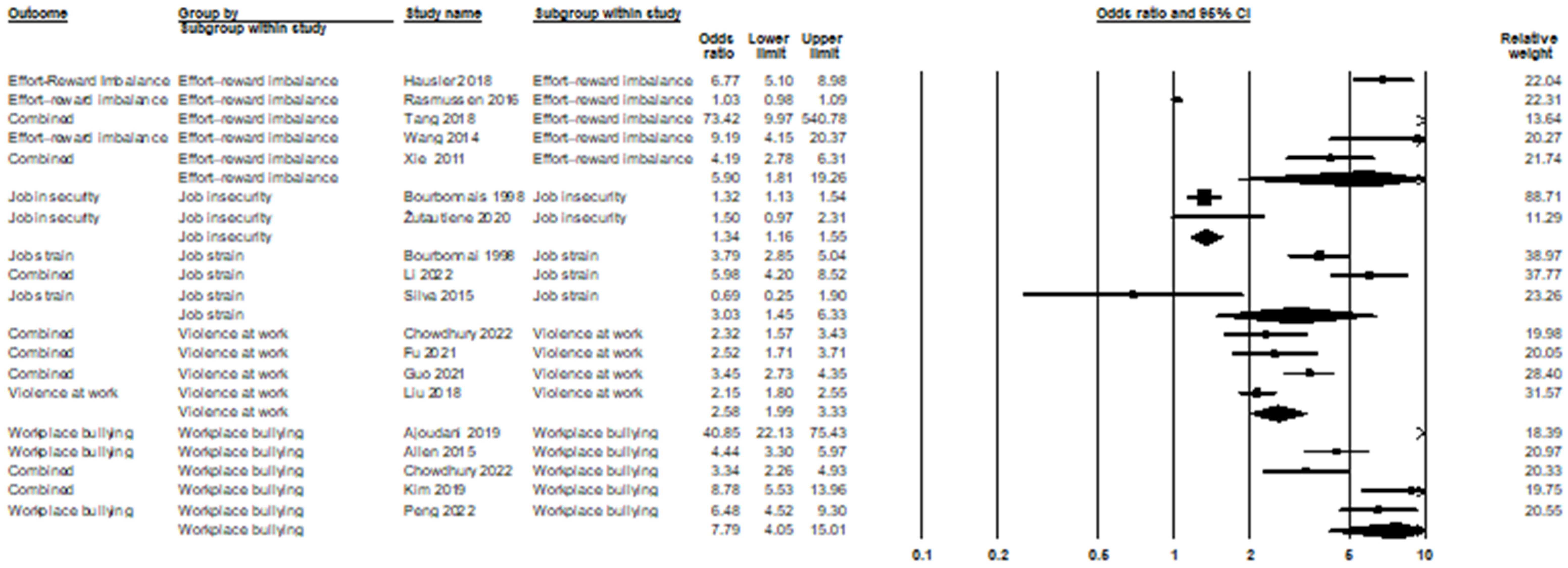
5.10. Publication Bias and Heterogeneity
6. Discussion
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organazation. Burn-Out an “Occupational Phenomenon”: International Classification of Diseases. 2019. Available online: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases (accessed on 11 August 2024).
- Maslach, C.; Jackson, S.; Leiter, M. The Maslach Burnout Inventory Manual. In Evaluating Stress: A Book of Resources; The Scarecrow Press: Lanham, MD, USA, 1997; Volume 3, pp. 191–218. [Google Scholar]
- Yazici, M.U.; Teksam, O.; Agin, H.; Erkek, N.; Arslankoylu, A.E.; Akca, H.; Esen, F.; Derinoz, O.; Yener, N.; Kilinc, M.A.; et al. The Burden of Burnout Syndrome in Pediatric Intensive Care Unit and Pediatric Emergency Department: A Multicenter Evaluation. Pediatr. Emerg. Care 2021, 37, e955–e961. [Google Scholar] [CrossRef] [PubMed]
- Al-Haddad, A.; Al-Omar, F.; Al-Khaleel, A.; Al-Khalaf, A. Prevalence of burnout syndrome and its related risk factors among physicians working in primary health care centers of the Ministry of Health, Al Ahsa region, Saudi Arabia, 2018–2019. J. Fam. Med. Prim. Care 2020, 9, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Rotenstein, L.S.; Torre, M.; Ramos, M.A.; Rosales, R.C.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA 2018, 320, 1131–1150. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shah, M.K.; Gandrakota, N.; Cimiotti, J.P.; Ghose, N.; Moore, M.; Ali, M.K. Prevalence of and Factors Associated With Nurse Burnout in the US. JAMA Netw. Open 2021, 4, e2036469. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kansoun, Z.; Boyer, L.; Hodgkinson, M.; Villes, V.; Lançon, C.; Fond, G. Burnout in French physicians: A systematic review and meta-analysis. J. Affect. Disord. 2019, 246, 132–147. [Google Scholar] [CrossRef] [PubMed]
- E, C. Doctor Burnout, Stress and Depression: Not an Easy Fix. U.S News & World Repor 2016. Available online: http://health.usnews.com/health-news/patient-advice/articles/2016-04-12/doctor-burnout-stress-and-depression-not-an-easy-fix (accessed on 11 August 2024).
- Lovell, L.P.; Atherley, A.E.N.; Watson, H.R.; King, R.D. An exploration of burnout and resilience among emergency physicians at three teaching hospitals in the English-speaking Caribbean: A cross-sectional survey. Lancet Reg. Health Am. 2022, 15, 100357. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Woo, T.; Ho, R.; Tang, A.; Tam, W. Global prevalence of burnout symptoms among nurses: A systematic review and meta-analysis. J. Psychiatr. Res. 2020, 123, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Ulbrichtova, R.; Svihrova, V.; Tatarkova, M.; Svihra, J., Jr.; Novak, M.; Hudeckova, H. Prevalence of Burnout Syndrome in COVID-19 and Non-COVID-19 Units in University Hospital: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 12664. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fortuna, F.; Gonzalez, D.; Fritzler, A.; Ibar, C.; Nenda, G.; D’Isa, E.; Otero, P.; Jamardo, J.; Calvo, M.; Funez, F.; et al. Burnout components, perceived stress and hair cortisol in healthcare professionals during the second wave of COVID 19 pandemic. Sci Rep. 2024, 14, 28828. [Google Scholar] [CrossRef]
- Jalili, M.; Niroomand, M.; Hadavand, F.; Zeinali, K.; Fotouhi, A. Burnout among healthcare professionals during COVID-19 pandemic: A cross-sectional study. Int. Arch. Occup. Environ. Health 2021, 94, 1345–1352. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ferry, A.V.; Wereski, R.; Strachan, F.E.; Mills, N.L. Predictors of UK healthcare worker burnout during the COVID-19 pandemic. QJM 2021, 114, 374–380. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhou, A.Y.; Panagioti, M.; Esmail, A.; Agius, R.; Van Tongeren, M.; Bower, P. Factors Associated With Burnout and Stress in Trainee Physicians: A Systematic Review and Meta-analysis. JAMA Netw. Open 2020, 3, e2013761. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Taranu, S.M.; Ilie, A.C.; Turcu, A.M.; Stefaniu, R.; Sandu, I.A.; Pislaru, A.I.; Alexa, I.D.; Sandu, C.A.; Rotaru, T.S.; Alexa-Stratulat, T. Factors Associated with Burnout in Healthcare Professionals. Int. J. Environ. Res. Public Health. 2022, 19, 14701. [Google Scholar] [CrossRef] [PubMed]
- Mazzetti, G.; Çetin, M.; Guglielmi, D.; Simbula, S. Resilience and the Dynamics of Job Demands: A Diary Study on Interactions in Healthcare Professionals During the COVID-19 Pandemic. J. Adv. Nurs. 2024. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Urquiza, J.L.; Vargas, C.; De la Fuente, E.I.; Fernández-Castillo, R.; Cañadas-De la Fuente, G.A. Age as a risk factor for burnout syndrome in nursing professionals: A meta-analytic study. Res. Nurs. Health 2017, 40, 99–110. [Google Scholar] [CrossRef]
- Canadas-De la Fuente, G.A.; Vargas, C.; San Luis, C.; Garcia, I.; Canadas, G.R.; De la Fuente, E.I. Risk factors and prevalence of burnout syndrome in the nursing profession. Int. J. Nurs. Stud. 2015, 52, 240–249. [Google Scholar] [CrossRef] [PubMed]
- Bridgeman, P.J.; Bridgeman, M.B.; Barone, J. Burnout syndrome among healthcare professionals. Am. J. Health Syst. Pharm. 2018, 75, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Vargas, C.; Cañadas, G.A.; Aguayo, R.; Fernández, R.; de la Fuente, E.I. Which occupational risk factors are associated with burnout in nursing? A meta-analytic study. Int. J. Clin. Health Psychol. 2014, 14, 28–38. [Google Scholar] [CrossRef]
- López-López, I.M.; Gómez-Urquiza, J.L.; Cañadas, G.R.; De la Fuente, E.I.; Albendín-García, L.; Cañadas-De la Fuente, G.A. Prevalence of burnout in mental health nurses and related factors: A systematic review and meta-analysis. Int. J. Ment. Health Nurs. 2019, 28, 1032–1041. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Urquiza, J.L.; Aneas-López, A.B.; Fuente-Solana, E.I.; Albendín-García, L.; Díaz-Rodríguez, L.; Fuente, G.A. Prevalence, Risk Factors, and Levels of Burnout Among Oncology Nurses: A Systematic Review. Oncol. Nurs. Forum 2016, 43, E104–E120. [Google Scholar] [CrossRef] [PubMed]
- Membrive-Jiménez, M.J.; Pradas-Hernández, L.; Suleiman-Martos, N.; Vargas-Román, K.; Cañadas-De la Fuente, G.A.; Gomez-Urquiza, J.L.; De la Fuente-Solana, E.I. Burnout in Nursing Managers: A Systematic Review and Meta-Analysis of Related Factors, Levels and Prevalence. Int. J. Environ. Res. Public Health 2020, 17, 3983. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Boutou, A.; Pitsiou, G.; Sourla, E.; Kioumis, I. Burnout syndrome among emergency medicine physicians: An update on its prevalence and risk factors. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 9058–9065. [Google Scholar] [CrossRef] [PubMed]
- Adriaenssens, J.; De Gucht, V.; Maes, S. Determinants and prevalence of burnout in emergency nurses: A systematic review of 25 years of research. Int. J. Nurs. Stud. 2015, 52, 649–661. [Google Scholar] [CrossRef] [PubMed]
- Molina-Praena, J.; Ramirez-Baena, L.; Gómez-Urquiza, J.L.; Cañadas, G.R.; De la Fuente, E.I.; Cañadas-De la Fuente, G.A. Levels of Burnout and Risk Factors in Medical Area Nurses: A Meta-Analytic Study. Int. J. Environ. Res. Public Health 2018, 15, 2800. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Group, P.-P. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.; Stiles, C.R.; Hagen, N.A.; Biondo, P.D.; Cummings, G.G. Assessment of study quality for systematic reviews: A comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: Methodological research. J. Eval. Clin. Pract. 2012, 18, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Thomas, H. Quality assessment tool for quantitative studies. In Effective Public Health Practice Project; McMaster University: Toronto, ON, Canada, 2003. [Google Scholar]
- Borenstein, M.; Hedges, L.; Higgins, J.; Rothstein, H.J.E. Comprehensive Meta-Analysis, version 3.3. 070; Biostatistics: Newark, NJ, USA, 2014; 97p. [Google Scholar]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Ioannidis, J.P.; Patsopoulos, N.A.; Evangelou, E. Uncertainty in heterogeneity estimates in meta-analyses. BMJ 2007, 335, 914–916. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1110. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P. Cochrane Handbook for Systematic Reviews of Interventions. 2019. Available online: http://www.cochrane-handbook.org (accessed on 11 August 2024).
- Sterne, J.A.; Sutton, A.J.; Ioannidis, J.P.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rucker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F.; Hawulte, B.; Yuya, M.; Birhanu, S.; Oljira, L. Prevalence of burnout and associated factors among health professionals working in public health facilities of Dire Dawa city administration, Eastern Ethiopia. Front. Public Health 2022, 10, 836654. [Google Scholar] [CrossRef]
- Al-Dubai, S.A.; Rampal, K.G. Prevalence and associated factors of burnout among doctors in Yemen. J. Occup. Health 2010, 52, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Alrawashdeh, H.M.; Al-Tammemi, A.a.B.; Alzawahreh, M.K.; Al-Tamimi, A.; Elkholy, M.; Al Sarireh, F.; Abusamak, M.; Elehamer, N.M.K.; Malkawi, A.; Al-Dolat, W. Occupational burnout and job satisfaction among physicians in times of COVID-19 crisis: A convergent parallel mixed-method study. BMC Public Health 2021, 21, 811. [Google Scholar] [CrossRef]
- Andlib, S.; Inayat, S.; Azhar, K.; Aziz, F. Burnout and psychological distress among Pakistani nurses providing care to COVID-19 patients: A cross-sectional study. Int. Nurs. Rev. 2022, 69, 529–537. [Google Scholar] [CrossRef]
- Arigoni, F.; Bovier, P.A.; Mermillod, B.; Waltz, P.; Sappino, A.-P. Prevalence of burnout among Swiss cancer clinicians, paediatricians and general practitioners: Who are most at risk? Support. Care Cancer 2009, 17, 75–81. [Google Scholar] [CrossRef]
- Boo, Y.L.; Liam, C.C.K.; Lim, S.Y.; Look, M.; Tan, M.H.; Ching, S.M.; Wan, J.L.; Chin, P.; Hoo, F. Stress and burnout syndrome in health-care providers treating dengue infection: A cross-sectional study. Med. J. Malays. 2018, 73, 371–375. [Google Scholar]
- Bourbonnais, R.; Comeau, M.; Vezina, M.; Dion, G. Job strain, psychological distress, and burnout in nurses. Am. J. Ind. Med. 1998, 34, 20–28. [Google Scholar] [CrossRef]
- CChen, Y.J.; Lin, K.P. Association among work characteristics, role transition, and job burnout in nurse practitioners in Taiwan. INQUIRY J. Health Care Organ. Provis. Financ. 2022, 59, 00469580221081403. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, S.R.; Kabir, H.; Chowdhury, M.R.; Hossain, A. Workplace bullying and violence on burnout among Bangladeshi registered nurses: A survey following a year of the COVID-19 pandemic. Int. J. Public Health 2022, 67, 1604769. [Google Scholar] [CrossRef] [PubMed]
- Daryanto, B.; Putri, F.R.; Kurniawan, J.; Ilmawan, M.; Fajar, J.K. The Prevalence and the Associated Sociodemographic-Occupational Factors of Professional Burnout Among Health Professionals During COVID-19 Pandemic in Malang, Indonesia: A Cross-Sectional Study. Front. Public Health 2022, 10, 894946. [Google Scholar] [CrossRef] [PubMed]
- Demirel Öğüt, N.; Öğüt, Ç.; Eşme, P. The role of online consultation requests to personal social media accounts and instant messaging services of dermatologists in occupational burnout: An emerging problem. J. Cosmet. Dermatol. 2022, 21, 2542–2549. [Google Scholar] [CrossRef]
- Elay, G.; Bahar, I.; Demirkiran, H.; Oksüz, H. Severe burnout among critical care workers in Turkey. Saudi Med. J. 2019, 40, 943. [Google Scholar] [CrossRef]
- Gouveia, P.A.d.C.; Ribeiro, M.H.C.; Aschoff, C.A.d.M.; Gomes, D.P.; Silva, N.A.F.d.; Cavalcanti, H.A.F. Factors associated with burnout syndrome in medical residents of a university hospital. Rev. Assoc. Médica Bras. 2017, 63, 504–511. [Google Scholar] [CrossRef]
- Guo, Y.; Hu, S.; Liang, F. The prevalence and stressors of job burnout among medical staff in Liaoning, China: A cross-section study. BMC Public Health 2021, 21, 777. [Google Scholar] [CrossRef]
- Hu, Z.; Wang, H.; Xie, J.; Zhang, J.; Li, H.; Liu, S.; Li, Q.; Yang, Y.; Huang, Y. Burnout in ICU doctors and nurses in mainland China-A national cross-sectional study. J. Crit. Care 2021, 62, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Huo, L.; Zhou, Y.; Li, S.; Ning, Y.; Zeng, L.; Liu, Z.; Qian, W.; Yang, J.; Zhou, X.; Liu, T.; et al. Burnout and Its Relationship With Depressive Symptoms in Medical Staff During the COVID-19 Epidemic in China. Front. Psychol. 2021, 12, 616369. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- İlhan, M.N.; Durukan, E.; Taner, E.; Maral, I.; Bumin, M.A. Burnout and its correlates among nursing staff: Questionnaire survey. J. Adv. Nurs. 2008, 61, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Karakoc, A.; Yilmaz, M.; Alcalar, N.; Esen, B.; Kayabasi, H.; Sit, D. Burnout Syndrome Among Hemodialysis and Peritoneal Dialysis Nurses. Iran J. Kidney Dis. 2016, 10, 395–404. [Google Scholar] [PubMed]
- Lee, Y.G.; Maeng, C.H.; Kim, D.Y.; Kim, B.S. Perspectives on Professional Burnout and Occupational Stress among Medical Oncologists: A Cross-sectional Survey by Korean Society for Medical Oncology (KSMO). Cancer Res. Treat. 2020, 52, 1002–1009. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, H.; Zuo, M.; Gelb, A.W.; Zhang, B.; Zhao, X.; Yao, D.; Xia, D.; Huang, Y. Chinese anesthesiologists have high burnout and low job satisfaction: A cross-sectional survey. Anesth. Analg. 2018, 126, 1004–1012. [Google Scholar] [CrossRef] [PubMed]
- Meng, H.; Bai, S.; Cao, Q. Risk factors of role stress and professional burnout among nurse anesthetists: A multicenter cross-sectional study. Jpn. J. Nurs. Sci. 2021, 18, e12413. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, A.J.; Panagopolou, E.; Benos, A. Work–family interference as a mediator between job demands and job burnout among doctors. Stress Health J. Int. Soc. Investig. Stress 2006, 22, 203–212. [Google Scholar] [CrossRef]
- Nishimura, K.; Nakamura, F.; Takegami, M.; Fukuhara, S.; Nakagawara, J.; Ogasawara, K.; Ono, J.; Shiokawa, Y.; Miyachi, S.; Nagata, I. Cross-sectional survey of workload and burnout among Japanese physicians working in stroke care: The nationwide survey of acute stroke care capacity for proper designation of comprehensive stroke center in Japan (J-ASPECT) study. Circ. Cardiovasc. Qual. Outcomes 2014, 7, 414–422. [Google Scholar] [CrossRef]
- Ozkula, G.; Durukan, E. Burnout syndrome among physicians: The role of socio-demographic characteristics. Dusunen Adam J. Psychiatry Neurol. Sci. 2017, 30, 136. [Google Scholar] [CrossRef]
- Pang, Y.; He, Y.; Chen, Z.; Han, X.; Leng, J.; Tang, L. The perceptions of burnout and related influencing factors in Chinese physicians and nurses working in a cancer hospital. Psycho Oncol. 2021, 30, 1525–1534. [Google Scholar] [CrossRef]
- Pinho, R.d.N.L.; Costa, T.F.; Silva, N.M.; Barros-Areal, A.F.; Salles, A.d.M.; Oliveira, A.P.R.A.; Rassi, C.H.R.E.; Gomes, C.M.; Silva, D.L.M.d.; Oliveira, F.A.R.d. High prevalence of burnout syndrome among medical and nonmedical residents during the COVID-19 pandemic. PLoS ONE 2022, 17, e0267530. [Google Scholar] [CrossRef]
- Pu, J.; Zhou, X.; Zhu, D.; Zhong, X.; Yang, L.; Wang, H.; Zhang, Y.; Fan, S.; Liu, L.; Xie, P. Gender differences in psychological morbidity, burnout, job stress and job satisfaction among Chinese neurologists: A national cross-sectional study. Psychol. Health Med. 2017, 22, 680–692. [Google Scholar] [CrossRef]
- See, K.C.; Zhao, M.Y.; Nakataki, E.; Chittawatanarat, K.; Fang, W.-F.; Faruq, M.O.; Wahjuprajitno, B.; Arabi, Y.M.; Wong, W.T.; Divatia, J.V. Professional burnout among physicians and nurses in Asian intensive care units: A multinational survey. Intensive Care Med. 2018, 44, 2079–2090. [Google Scholar] [CrossRef] [PubMed]
- Surgenor, L.J.; Spearing, R.L.; Horn, J.; Beautrais, A.L.; Mulder, R.T.; Chen, P. Burnout in hospital-based medical consultants in the New Zealand public health system. N. Z. Med. J. 2009, 122, 11–18. [Google Scholar] [PubMed]
- Teixeira, C.; Ribeiro, O.; Fonseca, A.M.; Carvalho, A.S. Burnout in intensive care units—A consideration of the possible prevalence and frequency of new risk factors: A descriptive correlational multicentre study. BMC Anesthesiol. 2013, 13, 38. [Google Scholar] [CrossRef] [PubMed]
- Tsou, M.-T.; Pai, T.-P.; Chiang, T.-M.; Huang, W.-H.; Lin, H.-M.; Lee, S.-C. Burnout and metabolic syndrome among different departments of medical center nurses in Taiwan-Cross-sectional study and biomarker research. J. Occup. Health 2021, 63, e12188. [Google Scholar] [CrossRef]
- Udho, S.; Kabunga, A. Burnout and Associated Factors among Hospital-Based Nurses in Northern Uganda: A Cross-Sectional Survey. BioMed Res. Int. 2022, 2022, 8231564. [Google Scholar] [CrossRef]
- Wang, Z.; Xie, Z.; Dai, J.; Zhang, L.; Huang, Y.; Chen, B. Physician burnout and its associated factors: A cross-sectional study in Shanghai. J. Occup. Health 2014, 56, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Liu, L.; Wang, Y.; Gao, F.; Zhao, X.; Wang, L. Factors associated with burnout among Chinese hospital doctors: A cross-sectional study. BMC Public Health 2013, 13, 786. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yao, H.; Wang, P.; Tang, Y.L.; Liu, Y.; Liu, T.; Liu, H.; Chen, Y.; Jiang, F.; Zhu, J. Burnout and job satisfaction of psychiatrists in China: A nationwide survey. BMC Psychiatry 2021, 21, 593. [Google Scholar] [CrossRef]
- Yu, J.; Gao, J.; Chen, J.; Sun, Y. Academic versus non-academic neurosurgeons in China: A national cross-sectional study on workload, burnout and engagement. BMJ Open 2019, 9, e028309. [Google Scholar] [CrossRef]
- Yu, J.; Zou, F.; Sun, Y. Job satisfaction, engagement, and burnout in the population of orthopedic surgeon and neurosurgeon trainees in mainland China. Neurosurg. Focus 2020, 48, E3. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; West, C.P.; Dyrbye, L.N.; Trockel, M.; Tutty, M.; Wang, H.; Carlasare, L.E.; Sinsky, C. Changes in Burnout and Satisfaction With Work-Life Integration in Physicians During the First 2 Years of the COVID-19 Pandemic. Mayo Clin. Proc. 2022, 97, 2248–2258. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Adler, A.B.; Adrian, A.L.; Hemphill, M.; Scaro, N.H.; Sipos, M.L.; Thomas, J.L. Professional stress and burnout in US military medical personnel deployed to Afghanistan. Mil. Med. 2017, 182, e1669–e1676. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Caruso, R.; Palamenghi, L.; Nania, T.; Dellafiore, F.; Bonetti, L.; Silenzi, A.; Marotta, C.; Graffigna, G. Factors associated with emotional exhaustion in healthcare professionals involved in the COVID-19 pandemic: An application of the job demands-resources model. Int. Arch. Occup. Environ. Health 2021, 94, 1751–1761. [Google Scholar] [CrossRef] [PubMed]
- Belji Kangarlou, M.; Fatemi, F.; Paknazar, F.; Dehdashti, A. Occupational Burnout symptoms and its relationship with workload and fear of the SARS-CoV-2 pandemic among hospital nurses. Front. Public Health 2022, 971, 852629. [Google Scholar] [CrossRef]
- de Wijn, A.N.; van der Doef, M.P. Patient-related stressful situations and stress-related outcomes in emergency nurses: A cross-sectional study on the role of work factors and recovery during leisure time. Int. J. Nurs. Stud. 2020, 107, 103579. [Google Scholar] [CrossRef] [PubMed]
- Escribà-Agüir, V.; Martín-Baena, D.; Pérez-Hoyos, S. Psychosocial work environment and burnout among emergency medical and nursing staff. Int. Arch. Occup. Environ. Health 2006, 80, 127–133. [Google Scholar] [CrossRef]
- García-Sierra, R.; Fernández-Castro, J.; Martínez-Zaragoza, F. Relationship between job demand and burnout in nurses: Does it depend on work engagement? J. Nurs. Manag. 2016, 24, 780–788. [Google Scholar] [CrossRef]
- Jonge, J.D.; Janseen, P.P.M.; Van Breukelen, G.J.P. Testing the demand-control-support model among health-care professionals: A structural equation model. Work. Stress 1996, 10, 209–224. [Google Scholar] [CrossRef]
- Khamisa, N.; Peltzer, K.; Ilic, D.; Oldenburg, B. Work related stress, burnout, job satisfaction and general health of nurses: A follow-up study. Int. J. Nurs. Pract. 2016, 22, 538–545. [Google Scholar] [CrossRef] [PubMed]
- Mijakoski, D.; Karadzinska-Bislimovska, J.; Basarovska, V.; Montgomery, A.; Panagopoulou, E.; Stoleski, S.; Minov, J. Burnout, engagement, and organizational culture: Differences between physicians and nurses. Open Access Maced. J. Med. Sci. 2015, 3, 506. [Google Scholar] [CrossRef]
- Molero Jurado, M.d.M.; Martos Martínez, Á.; Pérez-Fuentes, M.d.C.; Castiñeira López, H.; Gázquez Linares, J.J. Job strain and burnout in Spanish nurses during the COVID-19: Resilience as a protective factor in a cross-sectional study. Hum. Resour. Health 2022, 20, 79. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, A.; Spânu, F.; Băban, A.; Panagopoulou, E. Job demands, burnout, and engagement among nurses: A multi-level analysis of ORCAB data investigating the moderating effect of teamwork. Burn. Res. 2015, 2, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Moreira, A.S.; Lucca, S.R.d. Psychosocial factors and Burnout Syndrome among mental health professionals. Rev. Lat. Am. Enferm. 2020, 28, e3336. [Google Scholar] [CrossRef] [PubMed]
- Page, K.; Graves, N. A cross sectional study of organizational factors and their impact on job satisfaction and emotional burnout in a group of Australian nurses: Infection control practitioners. BMC Health Serv. Res. 2021, 21, 441. [Google Scholar] [CrossRef]
- Rostamabadi, A.; Shouroki, F.K.; Jalilian, H.; Choobineh, A.; Azmoon, H.; Shakerian, M. The relationship between work-related psychosocial factors and burnout among Iranian nurses: Job Demand-Control-Support model. La Med. Lav. 2019, 110, 312. [Google Scholar]
- Sugawara, N.; Danjo, K.; Furukori, H.; Sato, Y.; Tomita, T.; Fujii, A.; Nakagami, T.; Kitaoka, K.; Yasui-Furukori, N. Work–family conflict as a mediator between occupational stress and psychological health among mental health nurses in Japan. Neuropsychiatr. Dis. Treat. 2017, 13, 779–784. [Google Scholar] [CrossRef]
- Sundin, L.; Hochwälder, J.; Lisspers, J. A longitudinal examination of generic and occupational specific job demands, and work-related social support associated with burnout among nurses in Sweden. Work 2011, 38, 389–4000. [Google Scholar] [CrossRef]
- Viotti, S.; Converso, D. Relationship between job demands and psychological outcomes among nurses: Does skill discretion matter? Int. J. Occup. Med. Environ. Health 2016, 29, 439–460. [Google Scholar] [CrossRef] [PubMed]
- Xie, Z.; Wang, A.; Chen, B. Nurse burnout and its association with occupational stress in a cross-sectional study in Shanghai. J. Adv. Nurs. 2011, 67, 1537–1546. [Google Scholar] [CrossRef] [PubMed]
- Žutautienė, R.; Radišauskas, R.; Kaliniene, G.; Ustinaviciene, R. The prevalence of burnout and its associations with psychosocial work environment among Kaunas region (Lithuania) hospitals’ physicians. Int. J. Environ. Res. Public Health 2020, 17, 3739. [Google Scholar] [CrossRef]
- Akkoç, İ.; Okun, O.; Türe, A. The effect of role-related stressors on nurses’ burnout syndrome: The mediating role of work-related stress. Perspect. Psychiatr. Care 2021, 57, 583–596. [Google Scholar] [CrossRef] [PubMed]
- Gillet, N.; Huyghebaert-Zouaghi, T.; Réveillère, C.; Colombat, P.; Fouquereau, E. The effects of job demands on nurses’ burnout and presenteeism through sleep quality and relaxation. J. Clin. Nurs. 2020, 29, 583–592. [Google Scholar] [CrossRef] [PubMed]
- Goehring, C.; Gallacchi, M.B.; Kunzi, B.; Bovier, P. Psychosocial and professional characteristics of bournout in Swiss primary care practitioners: A cross-sectional survey. Swiss Med. Wkly. 2005, 135, 101–108. [Google Scholar] [PubMed]
- Ham, E.; Seto, M.C.; Rodrigues, N.C.; Hilton, N.Z. Workplace stressors and PTSD among psychiatric workers: The mediating role of burnout. Int. J. Ment. Health Nurs. 2022, 31, 1151–1163. [Google Scholar] [CrossRef]
- Janssen, P.P.M.; Schaufelioe, W.B.; Houkes, I. Work-related and individual determinants of the three burnout dimensions. Work. Stress 1999, 13, 74–86. [Google Scholar] [CrossRef]
- Khan, Y.; Bruyneel, A.; Smith, P. Determinants of the risk of burnout among nurses during the first wave of the COVID-19 pandemic in Belgium: A cross-sectional study. J. Nurs. Manag. 2022, 30, 1125–1135. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Leiter, M.P. Perception of risk: An organizational model of occupational risk, burnout, and physical symptoms. Anxiety Stress Coping 2005, 18, 131–144. [Google Scholar] [CrossRef]
- Liu, Y.; Lu, L.; Wang, W.-X.; Liu, S.; Chen, H.-R.; Gao, X.; Huang, M.-Y.; Liu, Y.-N.; Ren, Y.-M.; Wang, C.-C. Job burnout and occupational stressors among Chinese healthcare professionals at county-level health alliances. Int. J. Environ. Res. Public Health 2020, 17, 1848. [Google Scholar] [CrossRef]
- Medeiros, A.I.C.d.; Mesquita, R.B.d.; Macêdo, F.d.S.; Matos, A.G.d.C.; Pereira, E.D. Prevalence of burnout among healthcare workers in six public referral hospitals in northeastern Brazil during the COVID-19 pandemic: A cross-sectional study. Sao Paulo Med. J. 2022, 140, 553–558. [Google Scholar] [CrossRef]
- Pedrini, L.; Magni, L.R.; Giovannini, C.; Panetta, V.; Zacchi, V.; Rossi, G.; Placentino, A. Burnout in nonhospital psychiatric residential facilities. Psychiatr. Serv. 2009, 60, 1547–1551. [Google Scholar] [CrossRef]
- Van Bogaert, P.; Kowalski, C.; Weeks, S.M.; Clarke, S.P. The relationship between nurse practice environment, nurse work characteristics, burnout and job outcome and quality of nursing care: A cross-sectional survey. Int. J. Nurs. Stud. 2013, 50, 1667–1677. [Google Scholar] [CrossRef] [PubMed]
- Xian, M.; Zhai, H.; Xiong, Y.; Han, Y. The role of work resources between job demands and burnout in male nurses. J. Clin. Nurs. 2020, 29, 535–544. [Google Scholar] [CrossRef] [PubMed]
- Cha, Y.J.; Lee, K.-S.; Cho, J.H.; Choi, I.S.; Lee, D. Effect of job stress on burnout among nurses responding to COVID-19: The mediating effect of resilience. Int. J. Environ. Res. Public Health 2022, 19, 5409. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Li, J.; Cao, B.; Wang, F.; Luo, L.; Xu, J. Mediating effects of self-efficacy, coping, burnout, and social support between job stress and mental health among young Chinese nurses. J. Adv. Nurs. 2020, 76, 163–173. [Google Scholar] [CrossRef] [PubMed]
- de Looff, P.; Didden, R.; Embregts, P.; Nijman, H. Burnout symptoms in forensic mental health nurses: Results from a longitudinal study. Int. J. Ment. Health Nurs. 2019, 28, 306–317. [Google Scholar] [CrossRef] [PubMed]
- Hayes, B.; Douglas, C.; Bonner, A. Work environment, job satisfaction, stress and burnout among haemodialysis nurses. J. Nurs. Manag. 2015, 23, 588–598. [Google Scholar] [CrossRef] [PubMed]
- Hong, E.; Lee, Y.S. The mediating effect of emotional intelligence between emotional labour, job stress, burnout and nurses’ turnover intention. Int. J. Nurs. Pract. 2016, 22, 625–632. [Google Scholar] [CrossRef] [PubMed]
- Kushnir, T.; Cohen, A.H.; Kitai, E. Continuing medical education and primary physicians’ job stress, burnout and dissatisfaction. Med. Educ. 2000, 34, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L.J.; De Los Santos, J.A.A.; Falguera, C.C.; Nwafor, C.E.; Galabay, J.R.; Rosales, R.A.; Firmo, C.N. Predictors of nurses’ turnover intention at one and five years’ time. Int. Nurs. Rev. 2020, 67, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.Y.; Kim, K.-j.; Ko, S.; Song, E.K. Communication competence and resilience are modifiable factors for burnout of operating room nurses in South Korea. BMC Nurs. 2022, 21, 203. [Google Scholar] [CrossRef]
- Liao, H.; Liang, R.; He, H.; Huang, Y.; Liu, M. Work stress, burnout, occupational commitment, and social support among Chinese pediatric nurses: A moderated mediation model. J. Pediatr. Nurs. 2022, 67, e16–e23. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-A.; Ahn, S.-H. Relation of compassionate competence to burnout, job stress, turnover intention, job satisfaction and organizational commitment for oncology nurses in Korea. Asian Pac. J. Cancer Prev. 2015, 16, 5463–5469. [Google Scholar] [CrossRef] [PubMed]
- Tavakoli, N.; Shaker, S.H.; Soltani, S.; Abbasi, M.; Amini, M.; Tahmasebi, A.; Kasnavieh, S.M.H. Job burnout, stress, and satisfaction among emergency nursing staff after health system transformation plan in Iran. Emergency 2018, 6, e41. [Google Scholar] [PubMed]
- Tremolada, M.; Schiavo, S.; Tison, T.; Sormano, E.; De Silvestro, G.; Marson, P.; Pierelli, L. Stress, burnout, and job satisfaction in 470 health professionals in 98 apheresis units in Italy: A SIdEM collaborative study. J. Clin. Apher. 2015, 30, 297–304. [Google Scholar] [CrossRef]
- Wang, Q.Q.; Lv, W.J.; Qian, R.L.; Zhang, Y.H. Job burnout and quality of working life among Chinese nurses: A cross-sectional study. J. Nurs. Manag. 2019, 27, 1835–1844. [Google Scholar] [CrossRef] [PubMed]
- Yeh, T.F.; Chang, Y.C.; Hsu, Y.H.; Huang, L.L.; Yang, C.C. Causes of nursing staff burnout: Exploring the effects of emotional exhaustion, work–family conflict, and supervisor support. Jpn. J. Nurs. Sci. 2021, 18, e12392. [Google Scholar] [CrossRef]
- Durand, A.-C.; Bompard, C.; Sportiello, J.; Michelet, P.; Gentile, S. Stress and burnout among professionals working in the emergency department in a French university hospital: Prevalence and associated factors. Work 2019, 63, 57–67. [Google Scholar] [CrossRef]
- Gherman, M.A.; Arhiri, L.; Holman, A.C.; Soponaru, C. The Moral Impact of the COVID-19 Pandemic on Nurses’ Burnout, Work Satisfaction and Adaptive Work Performance: The Role of Autobiographical Memories of Potentially Morally Injurious Events and Basic Psychological Needs. Int. J. Environ. Res. Public Health 2022, 19, 7645. [Google Scholar] [CrossRef]
- Hamaideh, S.H. Burnout, social support, and job satisfaction among Jordanian mental health nurses. Issues Ment. Health Nurs. 2011, 32, 234–242. [Google Scholar] [CrossRef]
- Ntantana, A.; Matamis, D.; Savvidou, S.; Giannakou, M.; Gouva, M.; Nakos, G.; Koulouras, V. Burnout and job satisfaction of intensive care personnel and the relationship with personality and religious traits: An observational, multicenter, cross-sectional study. Intensive Crit. Care Nurs. 2017, 41, 11–17. [Google Scholar] [CrossRef]
- Ozyurt, A.; Hayran, O.; Sur, H. Predictors of burnout and job satisfaction among Turkish physicians. J. Assoc. Physicians 2006, 99, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Qiao, Z.; Chen, L.; Chen, M.; Guan, X.; Wang, L.; Jiao, Y.; Yang, J.; Tang, Q.; Yang, X.; Qiu, X. Prevalence and factors associated with occupational burnout among HIV/AIDS healthcare workers in China: A cross-sectional study. BMC Public Health 2016, 16, 335. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.; Lapkin, S.; Halcomb, E.; Sim, J. Job satisfaction among small rural hospital nurses: A cross-sectional study. J. Nurs. Scholarsh. 2023, 55, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Villarreal-Zegarra, D.; Lázaro-Illatopa, W.I.; Castillo-Blanco, R.; Cabieses, B.; Blukacz, A.; Bellido-Boza, L.; Mezones-Holguin, E. Relationship between job satisfaction, burnout syndrome and depressive symptoms in physicians: A cross-sectional study based on the employment demand-control model using structural equation modelling. BMJ Open 2022, 12, e057888. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yang, S.; Liu, D.; Liu, H.; Zhang, J.; Duan, Z. Relationship of work-family conflict, self-reported social support and job satisfaction to burnout syndrome among medical workers in southwest China: A cross-sectional study. PLoS ONE 2017, 12, e0171679. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yoon, H.S.; Sok, S.R. Experiences of violence, burnout and job satisfaction in Korean nurses in the emergency medical centre setting. Int. J. Nurs. Pract. 2016, 22, 596–604. [Google Scholar] [CrossRef]
- Perrewé, P.L.; Ganster, D.C. New Developments in Theoretical and Conceptual Approaches to Job Stress; Emerald Group Publishing Limited: Bingley, UK, 2010. [Google Scholar]
- Gribben, L.; Semple, C.J. Factors contributing to burnout and work-life balance in adult oncology nursing: An integrative review. Eur. J. Oncol. Nurs. 2021, 50, 101887. [Google Scholar] [CrossRef]
- Rabatin, J.; Williams, E.; Baier Manwell, L.; Schwartz, M.D.; Brown, R.L.; Linzer, M. Predictors and outcomes of burnout in primary care physicians. J. Prim. Care Community Health 2016, 7, 41–43. [Google Scholar] [CrossRef]
- Leineweber, C.; Westerlund, H.; Chungkham, H.S.; Lindqvist, R.; Runesdotter, S.; Tishelman, C. Nurses’ practice environment and work-family conflict in relation to burn out: A multilevel modelling approach. PLoS ONE 2014, 9, e96991. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Min, D. Effects of resilience, burnout, and work-related physical pain on work-life balance of registered nurses in South Korean nursing homes: A cross-sectional study. Medicine 2022, 101, e29889. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, Y.; Chang, Y.; Fu, J.; Wang, L. Work-family conflict and burnout among Chinese female nurses: The mediating effect of psychological capital. BMC Public Health 2012, 12, 915. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Häusler, N.; Bopp, M.; Hämmig, O. Effort–Reward Imbalance, Work–Privacy Conflict, and Burnout Among Hospital Employees. J. Occup. Environ. Med. 2018, 60, e183–e187. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, V.; Turnell, A.; Butow, P.; Juraskova, I.; Kirsten, L.; Wiener, L.; Patenaude, A.; Hoekstra-Weebers, J.; Grassi, L.; Committee, I.R. Burnout among psychosocial oncologists: An application and extension of the effort–reward imbalance model. Psycho-Oncology 2016, 25, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Zhang, L.; Li, X.; Lu, Q. Moderated role of social support in the relationship between job strain, burnout, and organizational commitment among operating room nurses: A cross-sectional study. Int. J. Environ. Res. Public Health 2022, 19, 10813. [Google Scholar] [CrossRef]
- Silva, J.L.L.d.; Soares, R.d.S.; Costa, F.d.S.; Ramos, D.d.S.; Lima, F.B.; Teixeira, L.R. Psychosocial factors and prevalence of burnout syndrome among nursing workers in intensive care units. Rev. Bras. Ter. Intensiv. 2015, 27, 125–133. [Google Scholar] [CrossRef]
- Fu, C.; Wang, G.; Shi, X.; Ren, Y.; Cao, F. The association between fear of future workplace violence and burnout among nurses in China: A cross-sectional study. J. Affect. Disord. 2021, 293, 29–35. [Google Scholar] [CrossRef]
- Liu, W.; Zhao, S.; Shi, L.; Zhang, Z.; Liu, X.; Li, L.I.; Duan, X.; Li, G.; Lou, F.; Jia, X. Workplace violence, job satisfaction, burnout, perceived organisational support and their effects on turnover intention among Chinese nurses in tertiary hospitals: A cross-sectional study. BMJ Open 2018, 8, e019525. [Google Scholar] [CrossRef]
- Ajoudani, F.; Baghaei, R.; Lotfi, M. Moral distress and burnout in Iranian nurses: The mediating effect of workplace bullying. Nurs. Ethics 2019, 26, 1834–1847. [Google Scholar] [CrossRef]
- Allen, B.C.; Holland, P.; Reynolds, R. The effect of bullying on burnout in nurses: The moderating role of psychological detachment. J. Adv. Nurs. 2015, 71, 381–390. [Google Scholar] [CrossRef]
- Kim, Y.; Lee, E.; Lee, H. Association between workplace bullying and burnout, professional quality of life, and turnover intention among clinical nurses. PLoS ONE 2019, 14, e0226506. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Saiki, M.; Matthews, T.A.; Kawakami, N.; Robbins, W.; Li, J. Formulations of Job Strain and Psychological Distress: A Four-year Longitudinal Study in Japan. Saf. Health Work 2024, 15, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Peng, J.; Luo, H.; Ma, Q.; Zhong, Y.; Yang, X.; Huang, Y.; Sun, X.; Wang, X.; He, J.; Song, Y. Association between workplace bullying and nurses’ professional quality of life: The mediating role of resilience. J. Nurs. Manag. 2022, 30, 1549–1558. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, S.E.; MacPhee, M.; Dahinten, V.S. Factors related to perioperative nurses’ job satisfaction and intention to leave. Jpn. J. Nurs. Sci. 2020, 17, e12263. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wang, J.; He, L.; Hu, Y.; Li, C.; Xie, Y.; Wang, N.; Luo, A.; Lu, Z. Turnover intention and influential factors among primary healthcare workers in Guangdong province, China: A cross-sectional study. BMJ Open. 2024, 14, e084859. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pepper, S.N.; Farrell, E.T.; Dawson, R.M.; Wirth, M.D. The Relationship Between Work Engagement, Depression, Anxiety, and COVID-19 Anxiety in Physician Assistant Students. Psychol. Rep. 2024, 332941241300968. [Google Scholar] [CrossRef] [PubMed]
- Khamisa, N.; Peltzer, K.; Oldenburg, B. Burnout in relation to specific contributing factors and health outcomes among nurses: A systematic review. Int. J. Environ. Res. Public Health 2013, 10, 2214–2240. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Cr, F. Compassion fatigue as secondary traumatic stress disorder-An overview. In Compassion Fatigue; Routledge: London, UK, 1995; pp. 1–20. [Google Scholar]
- Bride, B.E.; Robinson, M.M.; Yegidis, B.; Figley, C.R. Development and Validation of the Secondary Traumatic Stress Scale. Res. Soc. Work. Pract. 2004, 14, 27–35. [Google Scholar] [CrossRef]
- Dominguez-Gomez, E.; Rutledge, D.N. Prevalence of secondary traumatic stress among emergency nurses. J. Emerg. Nurs. 2009, 35, 199–204, quiz 73–94. [Google Scholar] [CrossRef] [PubMed]
- Ong, Y.T.; Sinnathamby, A.; Tan, J.H.; Ravindran, N.; Lim, S.X.; Hiew, A.W.H.; Ng, S.Y.; Ong, S.Y.K.; Krishna, L.K.R. Towards a Clinically Relevant Appreciation of the Cost of Caring: A Study of Palliative Care Physicians in Malaysia. Am. J. Hosp. Palliat. Care. 2024, 10499091241298281, Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Miljeteig, I.; Førde, R.; Rø, K.I.; Bååthe, F.; Bringedal, B.H. Moral distress among physicians in Norway: A longitudinal study. BMJ Open. 2024, 14, e080380. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Galbany-Estragués, P.; Millán-Martínez, P. Escasez de enfermeras en España: Del caso global a la situación particular. Informe SESPAS 2024 [Shortage of nurses in Spain: From the global case to particular situation. SESPAS Report 2024]. Gac Sanit. 2024, 38, 102376, Spanish. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Noseworthy, J.H. Executive Leadership and Physician Well-being: Nine Organizational Strategies to Promote Engagement and Reduce Burnout. Mayo Clin. Proc. 2017, 92, 129–146. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; Dyrbye, L.N.; West, C.P.; Sinsky, C.A. Potential Impact of Burnout on the US Physician Workforce. Mayo Clin. Proc. 2016, 91, 1667–1668. [Google Scholar] [CrossRef]
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry 2016, 15, 103–111. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Niedhammer, I.; Malard, L.; Chastang, J.F. Occupational factors and subsequent major depressive and generalized anxiety disorders in the prospective French national SIP study. BMC Public Health 2015, 15, 200. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wedegaertner, F.; Arnhold-Kerri, S.; Sittaro, N.A.; Bleich, S.; Geyer, S.; Lee, W.E. Depression- and anxiety-related sick leave and the risk of permanent disability and mortality in the working population in Germany: A cohort study. BMC Public Health 2013, 13, 145. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yates, M.; Samuel, V. Burnout in oncologists and associated factors: A systematic literature review and meta-analysis. Eur. J. Cancer Care 2019, 28, e13094. [Google Scholar] [CrossRef] [PubMed]
- Oenning, N.S.X.; Ziegelmann, P.K.; Goulart, B.N.G.; Niedhammer, I. Occupational factors associated with major depressive disorder: A Brazilian population-based study. J. Affect. Disord. 2018, 240, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Bonde, J.P. Psychosocial factors at work and risk of depression: A systematic review of the epidemiological evidence. Occup. Environ. Med. 2008, 65, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Santa Maria, A.; Wörfel, F.; Wolter, C.; Gusy, B.; Rotter, M.; Stark, S.; Kleiber, D.; Renneberg, B. The Role of Job Demands and Job Resources in the Development of Emotional Exhaustion, Depression, and Anxiety Among Police Officers. Police Q. 2017, 21, 109–134. [Google Scholar] [CrossRef]
- Zare, H.; Meyerson, N.S.; Nwankwo, C.A.; Thorpe, R.J., Jr. How Income and Income Inequality Drive Depressive Symptoms in U.S. Adults, Does Sex Matter: 2005-2016. Int. J. Environ. Res. Public Health 2022, 19, 6227. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Woo, J.M.; Kim, W.; Hwang, T.Y.; Frick, K.D.; Choi, B.H.; Seo, Y.J.; Kang, E.H.; Kim, S.J.; Ham, B.J.; Lee, J.S.; et al. Impact of depression on work productivity and its improvement after outpatient treatment with antidepressants. Value Health 2011, 14, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Amer, S.; Elotla, S.F.; Ameen, A.E.; Shah, J.; Fouad, A.M. Occupational Burnout and Productivity Loss: A Cross-Sectional Study Among Academic University Staff. Front. Public Health 2022, 10, 861674. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Melamed, S.; Kushnir, T.; Shirom, A. Burnout and risk factors for cardiovascular diseases. Behav. Med. 1992, 18, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Alameri, F.; Aldaheri, N.; Almesmari, S.; Basaloum, M.; Albeshr, N.A.; Simsekler, M.C.E.; Ugwuoke, N.V.; Dalkilinc, M.; Al Qubaisi, M.; Campos, L.A.; et al. Burnout and Cardiovascular Risk in Healthcare Professionals During the COVID-19 Pandemic. Front. Psychiatry 2022, 13, 867233. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- De Guillebon, E.; He, C.; Akhtar, S.; Pietrzak, R.H.; Ripp, J.; Peccoralo, L. Association of Psychological Safety with Burnout and Intent to Leave Among Physician Faculty in New York City. J. Gen. Intern. Med. 2024. epub ahead of print. [Google Scholar] [CrossRef]
- Musio, M.E.; Russo, M.; Barbieri, M.; Moro, A.; Zanini, M.; Sasso, L.; Bagnasco, A.; Catania, G. Influencing Factors of Nurses’ Well-Being in Critical Care During Pandemic Era: A Systematic Review. Public Health Nurs. 2024. epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Dean, W.; Talbot, S.; Dean, A. Reframing Clinician Distress: Moral Injury Not Burnout. Fed. Pract. 2019, 36, 400–440. [Google Scholar] [PubMed] [PubMed Central]
- Maslach, C.; Schaufeli, W.B.; Leiter, M.P. Job Burnout. Annu. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef] [PubMed]
- Thomas, L.R.; Ripp, J.A.; West, C.P. Charter on physician well-being. JAMA 2018, 319, 1541–1542. [Google Scholar] [CrossRef] [PubMed]
- Motluk, A. Do doctors experiencing burnout make more errors? CMAJ 2018, 190, E1216–E1217. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Menon, N.K.; Shanafelt, T.D.; Sinsky, C.A.; Linzer, M.; Carlasare, L.; Brady, K.J.S.; Stillman, M.J.; Trockel, M.T. Association of Physician Burnout with Suicidal Ideation and Medical Errors. JAMA Netw. Open 2020, 3, e2028780. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amiri, S.; Mahmood, N.; Mustafa, H.; Javaid, S.F.; Khan, M.A. Occupational Risk Factors for Burnout Syndrome Among Healthcare Professionals: A Global Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2024, 21, 1583. https://doi.org/10.3390/ijerph21121583
Amiri S, Mahmood N, Mustafa H, Javaid SF, Khan MA. Occupational Risk Factors for Burnout Syndrome Among Healthcare Professionals: A Global Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2024; 21(12):1583. https://doi.org/10.3390/ijerph21121583
Chicago/Turabian StyleAmiri, Sohrab, Nailah Mahmood, Halla Mustafa, Syed Fahad Javaid, and Moien AB Khan. 2024. "Occupational Risk Factors for Burnout Syndrome Among Healthcare Professionals: A Global Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 21, no. 12: 1583. https://doi.org/10.3390/ijerph21121583
APA StyleAmiri, S., Mahmood, N., Mustafa, H., Javaid, S. F., & Khan, M. A. (2024). Occupational Risk Factors for Burnout Syndrome Among Healthcare Professionals: A Global Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 21(12), 1583. https://doi.org/10.3390/ijerph21121583