Improving the Health and Environmental Health Literacy of Professionals: Evaluating the Effect of a Virtual Intervention on Phthalate Environmental Health Literacy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participant Recruitment
2.2. Participant Questionnaires
2.3. Online Educational Intervention
2.4. Data Analyses
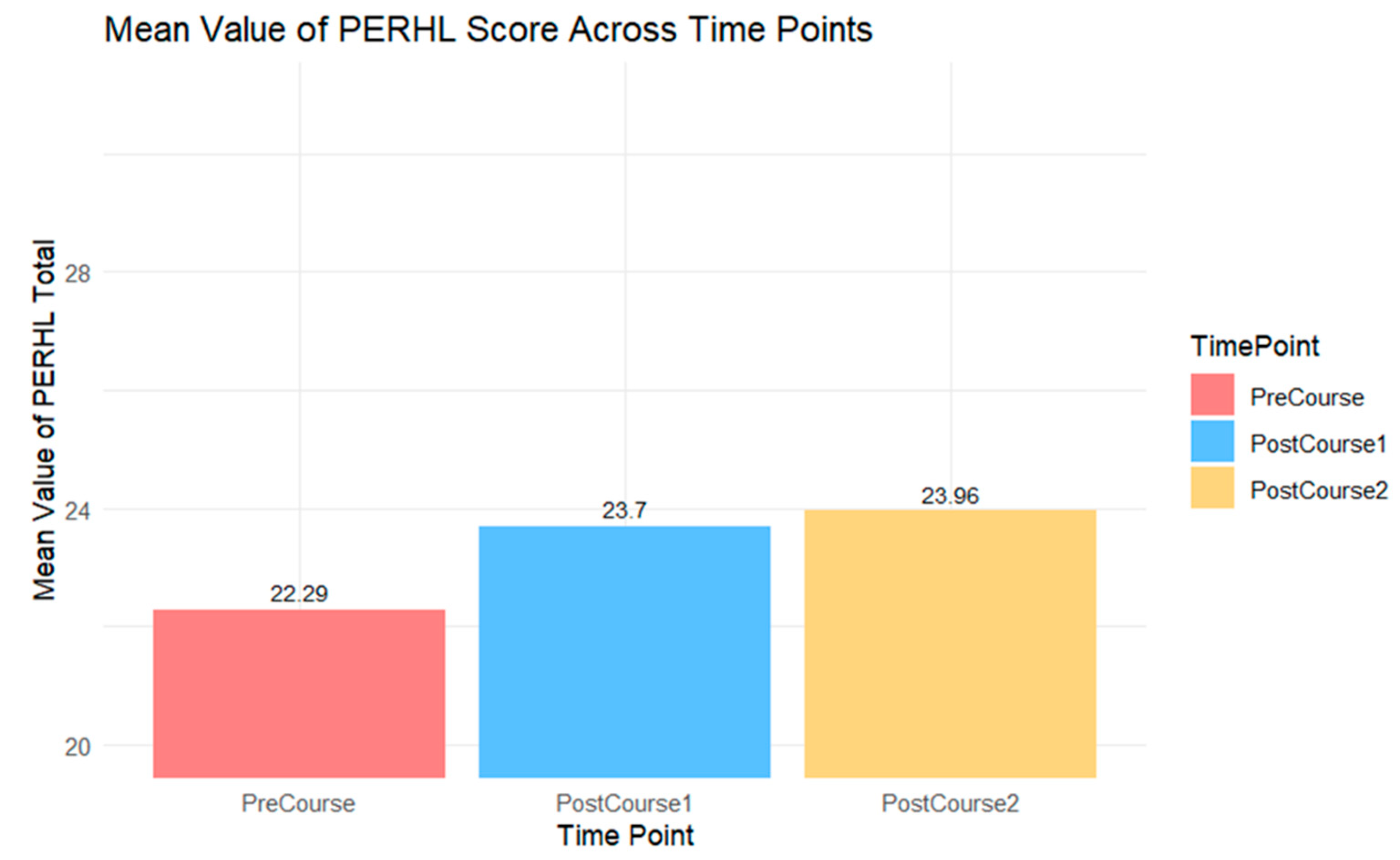
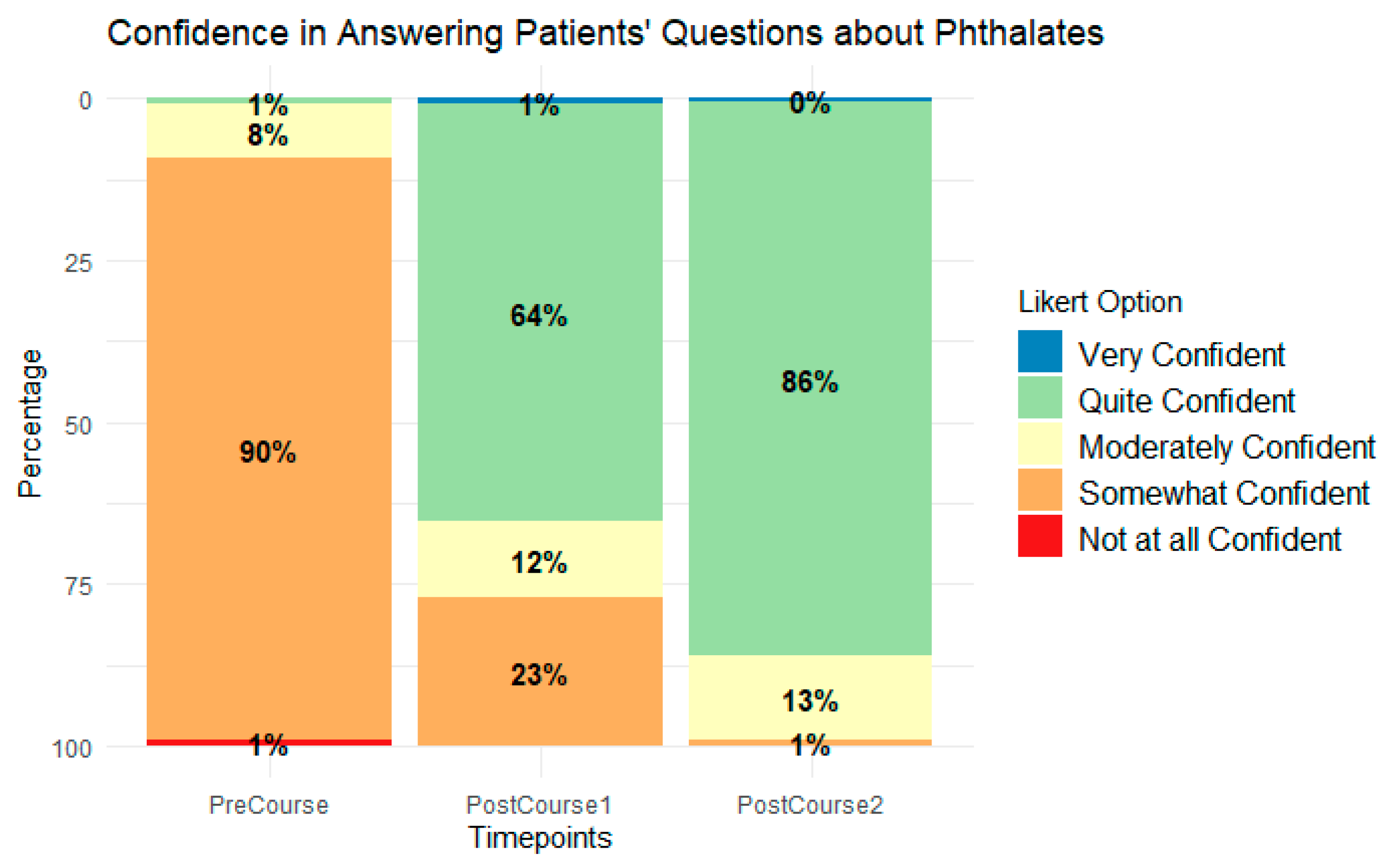
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- ACOG Committee Opinion. Reducing Prenatal Exposure to Toxic Environmental Agents. 2021. Available online: https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2021/07/reducing-prenatal-exposure-to-toxic-environmental-agents (accessed on 30 September 2021).
- Philippat, C.; Bennett, D.; Calafat, A.M.; Picciotto, I.H. Exposure to select phthalates and phenols through use of personal care products among Californian adults and their children. Environ. Res. 2016, 140, 369–376. [Google Scholar] [CrossRef]
- Pagoni, A.; Arvaniti, O.S.; Kalantzi, O.I. Exposure to Phthalates from Personal Care Products: Urinary Levels and Predictors of Exposure; Environmental Research; Academic Press Inc.: Cambridge, MA, USA, 2022; Volume 212. [Google Scholar]
- Fruh, V.; Preston, E.V.; Quinn, M.R.; Hacker, M.R.; Wylie, B.J.; O’Brien, K.; Hauser, R.; James-Todd, T.; Mahalingaiah, S. Urinary phthalate metabolite concentrations and personal care product use during pregnancy—Results of a pilot study. Sci. Total Environ. 2022, 835, 155439. [Google Scholar] [CrossRef] [PubMed]
- Hauser, R.; Calafat, A.M. Phthalates and human health. Occup. Environ. Med. 2005, 11, 806–818. [Google Scholar] [CrossRef] [PubMed]
- Meeker, J.D.; Sathyanarayana, S.; Swan, S.H. Phthalates and other additives in plastics: Human exposure and associated health outcomes. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 2009, 364, 2097–2113. [Google Scholar] [CrossRef]
- Zhang, Y.; Mustieles, V.; Yland, J.; Braun, J.M.; Williams, P.L.; Attaman, J.A.; Ford, J.B.; Calafat, A.M.; Hauser, R.; Messerlian, C. Association of Parental Preconception Exposure to Phthalates and Phthalate Substitutes with Preterm Birth. JAMA Netw. Open 2020, 3, e202159. [Google Scholar] [CrossRef]
- Lucaccioni, L.; Trevisani, V.; Passini, E.; Righi, B.; Plessi, C.; Predieri, B.; Iughetti, L. Perinatal Exposure to Phthalates: From Endocrine to Neurodevelopment Effects. Int. J. Mol. Sci. 2021, 22, 4063. [Google Scholar] [CrossRef]
- Yang, T.C.; Jovanovic, N.; Chong, F.; Worcester, M.; Sakhi, A.K.; Thomsen, C.; Garlantézec, R.; Chevrier, C.; Jensen, G.; Cingotti, N.; et al. Interventions to Reduce Exposure to Synthetic Phenols and Phthalates from Dietary Intake and Personal Care Products: A Scoping Review. Curr. Environ. Health Rep. 2023, 10, 184–214. [Google Scholar] [CrossRef]
- Stotland, N.E.; Sutton, P.; Trowbridge, J.; Atchley, D.S.; Conry, J.; Trasande, L.; Gerbert, B.; Charlesworth, A.; Woodruff, T.J. Counseling Patients on Preventing Prenatal Environmental Exposures—A Mixed-Methods Study of Obstetricians. PLoS ONE 2014, 9, e98771. [Google Scholar] [CrossRef]
- Tinney, V.A.; Paulson, J.A.; Bathgate, S.L.; Larsen, J.W. Medical education for obstetricians and gynecologists should incorporate environmental health. Am. J. Obs. Gynecol. 2015, 212, 163–166.e1. [Google Scholar] [CrossRef]
- Mariana, M.; Castelo-Branco, M.; Soares, A.M.; Cairrao, E. Phthalates’ exposure leads to an increasing concern on cardiovascular health. J. Hazard. Mater. 2023, 457, 131680. [Google Scholar] [CrossRef]
- United States Environmental Protection Agency. Phthalates. 2011. Available online: https://www.epa.gov/sites/default/files/2015-06/documents/ace3phthalatesreviewpackage3-02-11.pdf (accessed on 9 September 2024).
- Freire, C.; Castiello, F.; Babarro, I.; Anguita-Ruiz, A.; Casas, M.; Vrijheid, M.; Sarzo, B.; Beneito, A.; Kadawathagedara, M.; Philippat, C.; et al. Association of prenatal exposure to phthalates and synthetic phenols with pubertal development in three European cohorts. Int. J. Hyg. Environ. Health 2024, 261, 114418. [Google Scholar] [CrossRef] [PubMed]
- Mouatsou, C.; Margetaki, K.; Kampouri, M.; Psoma, S.; Roumeliotaki, T.; Vafeiadi, M.; Chatzi, L.; Kogevinas, M.; Koutra, K. Prenatal exposure to phthalates and childrens mental health trajectorie_Rhea cohort, Greece. Eur. J. Public Health 2024, 34, iii769–iii770. [Google Scholar] [CrossRef]
- Zheng, Y.; Hua, L.; Zhang, Z.; Zhu, L.; Zhu, H.; Sun, H.; Zhao, H. Current Phthalate Exposure Risks of Rural Population in the Northwest China: Evidence from an Internal Exposure Study. Environ. Health 2024, 2, 586–595. [Google Scholar] [CrossRef] [PubMed]
- Marie, C.; Vendittelli, F.; Sauvant-Rochat, M.P. Obstetrical outcomes and biomarkers to assess exposure to phthalates: A review. Environ. Int. 2015, 83, 116–136. [Google Scholar] [CrossRef]
- Adibi, J.J.; Perera, F.P.; Jedrychowski, W.; Camann, D.E.; Barr, D.; Jacek, R.; Whyatt, R.M. Prenatal exposures to Phthalates among women in New York and Krakow, Poland. Environ. Health Perspect. 2003, 111, 1719–1722. [Google Scholar] [CrossRef]
- Wang, L.; Duan, W.; Zhao, Y.; Sun, G.; Lin, Y.; Gao, Y. The exposure levels of phthalates in pregnant women and impact factors of fetal malformation. Hum. Exp. Toxicol. 2021, 40 (Suppl. 12), S622–S631. [Google Scholar] [CrossRef]
- Wu, H.; Kupsco, A.; Just, A.; Calafat, A.M.; Oken, E.; Braun, J.M.; Sanders, A.P.; Mercado-Garcia, A.; Cantoral, A.; Pantic, I.; et al. Maternal Phthalates Exposure and Blood Pressure during and after Pregnancy in the PROGRESS Study. Environ. Health Perspect. 2021, 129, 127007. [Google Scholar] [CrossRef]
- Petroff, R.L.; Padmanabhan, V.; Dolinoy, D.C.; Watkins, D.J.; Ciarelli, J.; Haggerty, D.; Ruden, D.M.; Goodrich, J.M. Prenatal Exposures to Common Phthalates and Prevalent Phthalate Alternatives and Infant DNA Methylation at Birth. Front. Genet. 2022, 13, 793278. [Google Scholar] [CrossRef]
- Cathey, A.L.; Watkins, D.; Rosario, Z.Y.; Vélez, C.; Alshawabkeh, A.N.; Cordero, J.F.; Meeker, J.D. Associations of phthalates and phthalate replacements with CRH and other hormones among pregnant women in Puerto Rico. J. Endocr. Soc. 2019, 3, 1127–1149. [Google Scholar] [CrossRef]
- Shin, H.M.; Dhar, U.; Calafat, A.M.; Nguyen, V.; Schmidt, R.J.; Hertz-Picciotto, I. Temporal Trends of Exposure to Phthalates and Phthalate Alternatives in California Pregnant Women during 2007–2013: Comparison with Other Populations. Environ. Sci. Technol. 2020, 54, 13157–13166. [Google Scholar] [CrossRef]
- Vernet, C.; Pin, I.; Giorgis-Allemand, L.; Philippat, C.; Benmerad, M.; Quentin, J.; Calafat, A.M.; Ye, X.; Annesi-Maesano, I.; Siroux, V.; et al. In Utero Exposure to Select Phenols and Phthalates and Respiratory Health in Five-Year-Old Boys: A Prospective Study. Environ. Health Perspect. 2017, 125, 097006. [Google Scholar] [CrossRef] [PubMed]
- James-Todd, T.M.; Meeker, J.D.; Huang, T.; Hauser, R.; Ferguson, K.K.; Rich-Edwards, J.W.; McElrath, T.F.; Seely, E.W. Pregnancy urinary phthalate metabolite concentrations and gestational diabetes risk factors. Environ. Int. 2016, 96, 118–126. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, K.K.; McElrath, T.F.; Meeker, J.D. Environmental phthalate exposure and preterm birth. JAMA Pediatr. 2014, 168, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, K.K.; Rosen, E.M.; Rosario, Z.; Feric, Z.; Calafat, A.M.; McElrath, T.F.; Vélez Vega, C.; Cordero, J.F.; Alshawabkeh, A.; Meeker, J.D. Environmental phthalate exposure and preterm birth in the PROTECT birth cohort. Environ. Int. 2019, 132, 105099. [Google Scholar] [CrossRef]
- Cathey, A.L.; Watkins, D.J.; Rosario, Z.Y.; Vélez, C.; Mukherjee, B.; Alshawabkeh, A.N.; Cordero, J.F.; Meeker, J.D. Biomarkers of Exposure to Phthalate Mixtures and Adverse Birth Outcomes in a Puerto Rico Birth Cohort. Environ. Health Perspect. 2022, 130, 37009. [Google Scholar] [CrossRef]
- Welch, B.M.; Keil, A.P.; Buckley, J.P.; Calafat, A.M.; Christenbury, K.E.; Engel, S.M.; O’Brien, K.M.; Rosen, E.M.; James-Todd, T.; Zota, A.R.; et al. Associations Between Prenatal Urinary Biomarkers of Phthalate Exposure and Preterm Birth: A Pooled Study of 16 US Cohorts. JAMA Pediatr. 2022, 27709, 895–905. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software partners. J. Biomed. Inf. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Tomsho, K.S.; Quinn, M.R.; Adamkiewicz, G.; James-Todd, T. Development of a Phthalate Environmental Reproductive Health Literacy (PERHL) Scale. Environ. Health Perspect. 2024, 132, 47013. [Google Scholar] [CrossRef]
- Chan, M.; Mita, C.; Bellavia, A.; Parker, M.; James-Todd, T. Racial/Ethnic Disparities in Pregnancy and Prenatal Exposure to Endocrine-Disrupting Chemicals Commonly Used in Personal Care Products. Curr. Environ. Health Rep. 2021, 8, 98–112. [Google Scholar] [CrossRef]
- James-Todd, T.; Senie, R.; Terry, M.B. Racial/ethnic differences in hormonally-active hair product use: A plausible risk factor for health disparities. J. Immigr. Minor. Health 2012, 14, 506–511. [Google Scholar] [CrossRef]
- Huang, T.; Saxena, A.R.; Isganaitis, E.; James-Todd, T. Gender and racial/ethnic differences in the associations of urinary phthalate metabolites with markers of diabetes risk: National health and nutrition examination survey 2001–2008. Environ. Health 2014, 13, 6. [Google Scholar] [CrossRef] [PubMed]
- James-Todd, T.M.; Chiu, Y.H.; Zota, A.R. Racial/Ethnic Disparities in Environmental Endocrine Disrupting Chemicals and Women’s Reproductive Health Outcomes: Epidemiological Examples Across the Life Course. Curr. Epidemiol. Rep. 2016, 3, 161–180. [Google Scholar] [CrossRef] [PubMed]
- James-Todd, T.; Terry, M.B.; Rich-Edwards, J.; Deierlein, A.; Senie, R. Childhood Hair Product Use and Earlier Age at Menarche in a Racially Diverse Study Population: A Pilot Study. Ann. Epidemiol. 2011, 21, 461–465. [Google Scholar] [CrossRef] [PubMed]
- Gaston, S.A.; James-Todd, T.; Harmon, Q.; Taylor, K.W.; Baird, D.; Jackson, C.L. Chemical/straightening and other hair product usage during childhood, adolescence, and adulthood among African-American women: Potential implications for health. J. Expo. Sci. Environ. Epidemiol. 2020, 30, 86–96. [Google Scholar] [CrossRef]
- Welch, B.M.; Keil, A.P.; Buckley, J.P.; Engel, S.M.; James-Todd, T.; Zota, A.R.; Alshawabkeh, A.N.; Barrett, E.S.; Bloom, M.S.; Bush, N.R.; et al. Racial and ethnic disparities in phthalate exposure and preterm birth: A pooled study of 16 US cohorts. Environ. Health Perspect. 2023, 131, 127015. [Google Scholar] [CrossRef]
- Deslauriers, L.; McCarty, L.S.; Miller, K.; Callaghan, K.; Kestin, G. Measuring actual learning versus feeling of learning in response to being actively engaged in the classroom. Proc. Natl. Acad. Sci. USA 2019, 116, 19251–19257. [Google Scholar] [CrossRef]
- EmVision. EmVision Productions. 2023. Available online: https://www.em.vision/ (accessed on 5 February 2024).
- McCue, K.; DeNicola, N. Environmental Exposures in Reproductive Health. Obstet. Gynecol. Clin. N. Am. 2019, 46, 455–468. [Google Scholar] [CrossRef]
- Singh, S.; Li, S.S. Epigenetic Effects of Environmental Chemicals Bisphenol A and Phthalates. Int. J. Mol. Sci. 2012, 13, 10143–10153. [Google Scholar] [CrossRef]
- Gehle, K.S.; Crawford, J.L.; Hatcher, M.T. Integrating environmental health into medical education. Am. J. Prev. Med. 2011, 41 (Suppl. 3), S296–S301. [Google Scholar] [CrossRef]
- Trasande, L.; Newman, N.; Long, L.; Howe, G.; Kerwin, B.J.; Martin, R.J.; Gahagan, S.A.; Weil, W.B. Translating knowledge about environmental health to practitioners: Are we doing enough? Mt. Sinai J. Med. 2010, 77, 114–123. [Google Scholar] [CrossRef]
- McCurdy, L.E.; Roberts, J.; Rogers, B.; Love, R.; Etzel, R.; Paulson, J.; Witherspoon, N.O.; Dearry, A. Incorporating environmental health into pediatric medical and nursing education. Environ. Health Perspect. 2004, 112, 1755–1760. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pope, A.M.; Rall, D.P. Environmental Medicine: Integrating a Missing Element into Medical Education; National Academy Press: Washington, DC, USA, 1995; 975p. [Google Scholar]
- Rosas, L.G.; Trujillo, C.; Camacho, J.; Madrigal, D.; Bradman, A.; Eskenazi, B. Acceptability of health information technology aimed at environmental health education in a prenatal clinic. Patient Educ. Couns. 2014, 97, 244–247. [Google Scholar] [CrossRef] [PubMed]
- Rogers, B.; McCurdy, L.E.; Slavin, K.; Grubb, K.; Roberts, J.R. Children’s Environmental Health Faculty Champions Initiative: A successful model for integrating environmental health into pediatric health care. Environ. Health Perspect. 2009, 117, 850–855. [Google Scholar] [CrossRef]
- Gee, G.C.; Payne-Sturges, D.C. Environmental Health Disparities: A Framework Integrating Psychosocial and Environmental Concepts. Environ. Health Perspect. 2004, 112, 1645–1653. [Google Scholar] [CrossRef]
- Ruiz, D.; Becerra, M.; Jagai, J.S.; Ard, K.; Sargis, R.M. Disparities in environmental exposures to endocrine-disrupting chemicals and diabetes risk in vulnerable populations. Diabetes Care 2018, 41, 193–205. [Google Scholar] [CrossRef]
- Zota, A.R.; Shamasunder, B. The environmental injustice of beauty: Framing chemical exposures from beauty products as a health disparities concern. Am. J. Obs. Gynecol. 2017, 217, e1–e418. [Google Scholar] [CrossRef]
- Chan, M.; Parikh, S.; Shyr, D.; Shamasunder, B.; Adamkiewicz, G.; James-Todd, T. Evaluating Neighborhood-Level Differences in Hair Product Safety by Environmental Working Group Ratings among Retailers in Boston, Massachusetts. Environ. Health Perspect. 2023, 131, 97002. [Google Scholar] [CrossRef]
- Kobrosly, R.W.; Parlett, L.E.; Stahlhut, R.W.; Barrett, E.S.; Swan, S.H. Socioeconomic factors and phthalate metabolite concentrations among United States women of reproductive age. Environ. Res. 2012, 115, 11–17. [Google Scholar] [CrossRef]
- Preston, E.V.; Chan, M.; Nozhenko, K.; Bellavia, A.; Grenon, M.C.; Cantonwine, D.E.; McElrath, T.F.; James-Todd, T. Socioeconomic and racial/ethnic differences in use of endocrine-disrupting chemical-associated personal care product categories among pregnant women. Environ. Res. 2021, 198, 111212. [Google Scholar] [CrossRef]


| Characteristics | All (n = 203) |
|---|---|
| Median [Min, Max] or n (%) | |
| Age at Enrollment (years) | 33.0 [27.0, 41.0] |
| Race | |
| Black/African American | 41 (20.2%) |
| East Asian | 29 (14.3%) |
| Mexican/Mexican American | 1 (0.5%) |
| Native Hawaiian/PI | 6 (3.0%) |
| Puerto Rican | 1 (0.5%) |
| South Asian | 29 (14.3%) |
| White | 96 (47.3%) |
| Occupational Title | |
| Doctor of Medicine (MD) | 46 (22.7%) |
| Doctor of Osteopathic Medicine (DO) | 1 (0.5%) |
| Nurse Practitioner (NP) | 101 (49.8%) |
| Physician Assistant (PA-C) | 55 (27.1%) |
| Other | 46 (22.7%) |
| Years Employed in Position Relevant to Reproductive Health | |
| 1−5 years | 98 (48.3%) |
| 5−10 years | 96 (47.3%) |
| 10−15 years | 9 (4.4%) |
| Previous Experience with Environmental Health | |
| No | 201 (99.0%) |
| No Response | 2 (1.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tomsho, K.S.; Quinn, M.R.; Wang, Z.; Preston, E.V.; Adamkiewicz, G.; Joseph, N.T.; Wylie, B.J.; James-Todd, T. Improving the Health and Environmental Health Literacy of Professionals: Evaluating the Effect of a Virtual Intervention on Phthalate Environmental Health Literacy. Int. J. Environ. Res. Public Health 2024, 21, 1571. https://doi.org/10.3390/ijerph21121571
Tomsho KS, Quinn MR, Wang Z, Preston EV, Adamkiewicz G, Joseph NT, Wylie BJ, James-Todd T. Improving the Health and Environmental Health Literacy of Professionals: Evaluating the Effect of a Virtual Intervention on Phthalate Environmental Health Literacy. International Journal of Environmental Research and Public Health. 2024; 21(12):1571. https://doi.org/10.3390/ijerph21121571
Chicago/Turabian StyleTomsho, Kathryn S., Marlee R. Quinn, Zifan Wang, Emma V. Preston, Gary Adamkiewicz, Naima T. Joseph, Blair J. Wylie, and Tamarra James-Todd. 2024. "Improving the Health and Environmental Health Literacy of Professionals: Evaluating the Effect of a Virtual Intervention on Phthalate Environmental Health Literacy" International Journal of Environmental Research and Public Health 21, no. 12: 1571. https://doi.org/10.3390/ijerph21121571
APA StyleTomsho, K. S., Quinn, M. R., Wang, Z., Preston, E. V., Adamkiewicz, G., Joseph, N. T., Wylie, B. J., & James-Todd, T. (2024). Improving the Health and Environmental Health Literacy of Professionals: Evaluating the Effect of a Virtual Intervention on Phthalate Environmental Health Literacy. International Journal of Environmental Research and Public Health, 21(12), 1571. https://doi.org/10.3390/ijerph21121571







