Bushfires and Mothers’ Mental Health in Pregnancy and Recent Post-Partum
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Bushfire and Smoke Exposures
2.3. COVID-19 Exposure
2.4. Pregnancy
2.5. Mental Health and Wellbeing Measures
2.6. Covariates
2.7. Statistical Analysis
3. Results
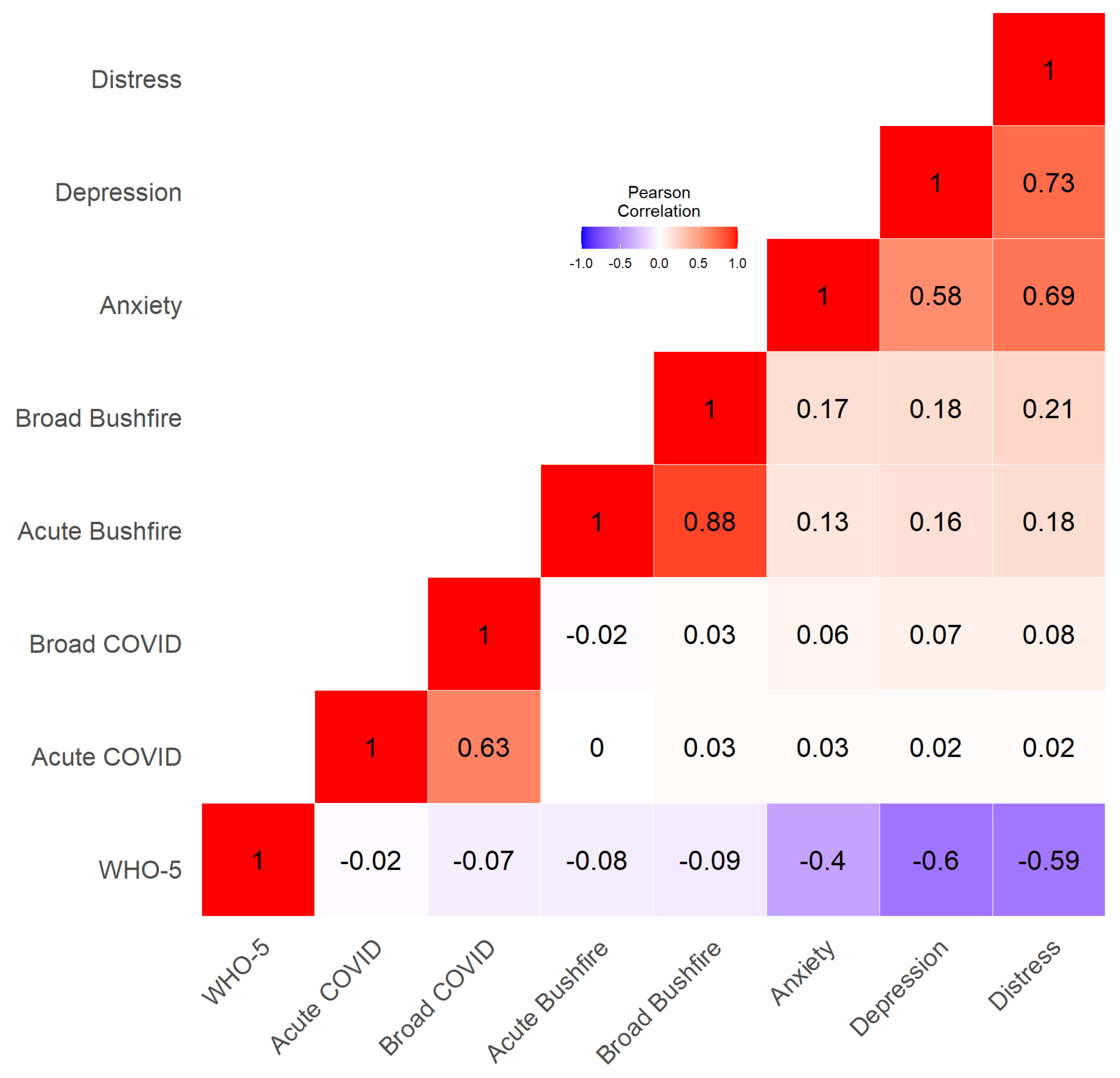
3.1. Mental Health
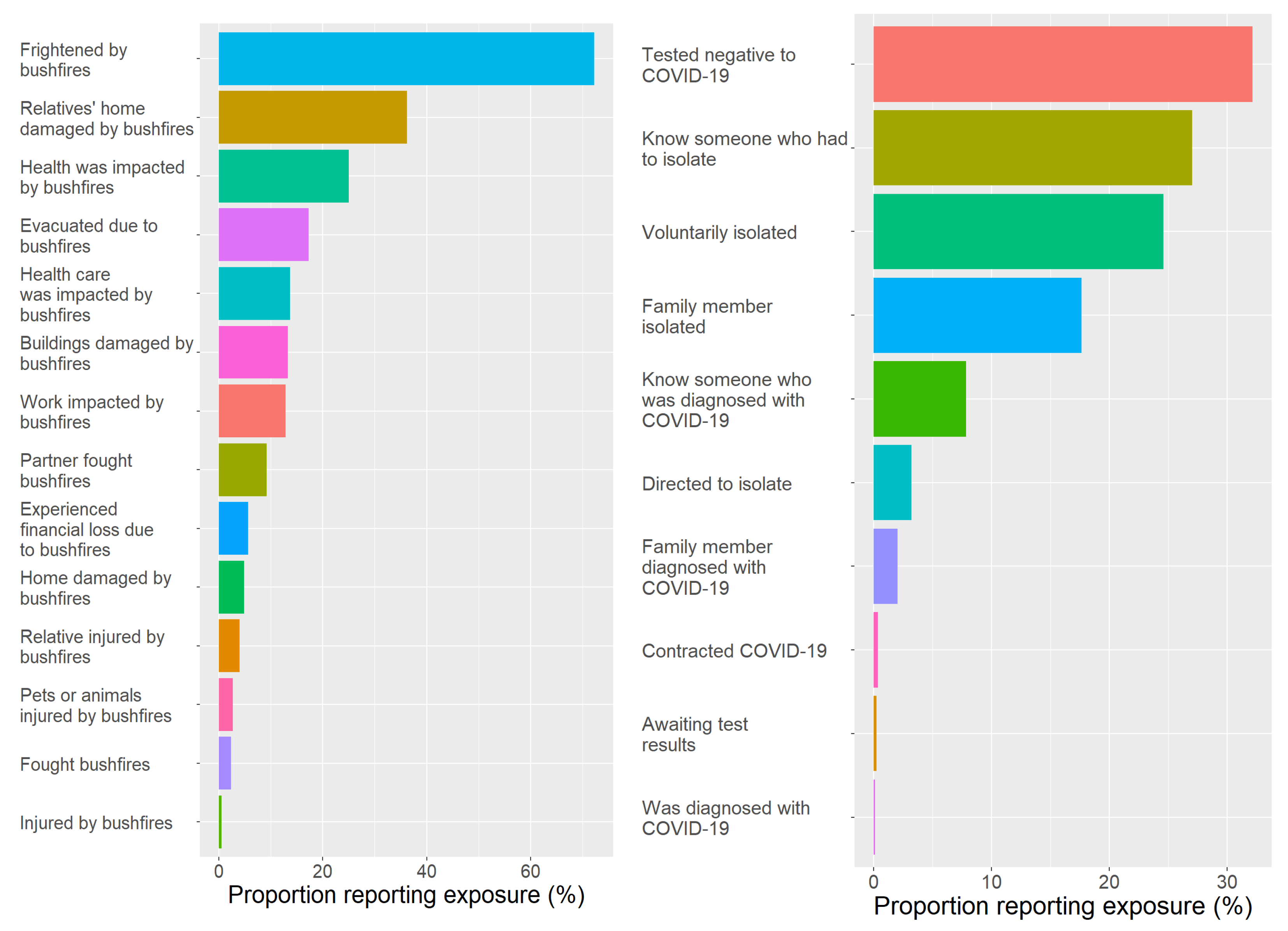
3.2. Bushfire and Smoke Exposure
3.3. COVID-19 Exposure
3.4. Bushfire and Smoke Exposure and Mental Health
3.5. COVID-19 and Mental Health
3.6. Sensitivity Analyses
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Intergovernmental Panel on Climate Change. The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report; Intergovernmental Panel on Climate Change: Geneva, Switzerland, 2021; Available online: https://www.ipcc.ch/report/ar6/wg1/ (accessed on 16 November 2023).
- Mendenhall, E.; Kohrt, B.A.; Logie, C.H.; Tsai, A.C. Syndemics and clinical science. Nat. Med. 2022, 28, 1359–1362. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.C.; Pereira, G.; Uhl, S.A.; Bravo, M.A.; Bell, M.L. A systematic review of the physical health impacts from non-occupational exposure to wildfire smoke. Environ. Res. 2015, 136, 120–132. [Google Scholar] [CrossRef] [PubMed]
- Reid, C.E.; Brauer, M.; Johnston, F.H.; Jerrett, M.; Balmes, J.R.; Elliott, C.T. Critical Review of Health Impacts of Wildfire Smoke Exposure. Environ. Health Perspect. 2016, 124, 1334–1343. [Google Scholar] [CrossRef] [PubMed]
- Sohail, H.; Kollanus, V.; Tiittanen, P.; Schneider, A.; Lanki, T. Heat, Heatwaves and Cardiorespiratory Hospital Admissions in Helsinki, Finland. Int. J. Environ. Res. Public. Health 2020, 17, 7892. [Google Scholar] [CrossRef] [PubMed]
- Alves, L. Surge of respiratory illnesses in children due to fires in Brazil’s Amazon region. Lancet Respir. Med. 2020, 8, 21–22. [Google Scholar] [CrossRef] [PubMed]
- Borchers Arriagada, N.; Palmer, A.J.; Bowman, D.M.; Morgan, G.G.; Jalaludin, B.B.; Johnston, F.H. Unprecedented smoke-related health burden associated with the 2019-20 bushfires in eastern Australia. Med. J. Aust. 2020, 213, 282–283. [Google Scholar] [CrossRef]
- Johnston, F.H.; Henderson, S.B.; Chen, Y.; Randerson, J.T.; Marlier, M.; DeFries, R.S.; Kinney, P.; Bowman, D.M.J.S.; Brauer, M. Estimated Global Mortality Attributable to Smoke from Landscape Fires. Environ. Health Perspect. 2012, 120, 695–701. [Google Scholar] [CrossRef] [PubMed]
- Shaposhnikov, D.; Revich, B.; Bellander, T.; Bedada, G.B.; Bottai, M.; Kharkova, T.; Kvasha, E.; Lezina, E.; Lind, T.; Semutnikova, E.; et al. Mortality related to air pollution with the moscow heat wave and wildfire of 2010. Epidemiology 2014, 25, 359–364. [Google Scholar] [CrossRef]
- Makwana, N. Disaster and its impact on mental health: A narrative review. J. Fam. Med. Prim. Care 2019, 8, 3090–3095. [Google Scholar] [CrossRef]
- Bansal, A.; Cherbuin, N.; Davis, D.L.; Peek, M.J.; Wingett, A.; Christensen, B.K.; Carlisle, H.; Broom, M.; Schoenaker, D.A.J.M.; Dahlstrom, J.E.; et al. Heatwaves and wildfires suffocate our healthy start to life: Time to assess impact and take action. Lancet Planet. Health 2023, 7, e718–e725. [Google Scholar] [CrossRef]
- Woody, C.A.; Ferrari, A.J.; Siskind, D.J.; Whiteford, H.A.; Harris, M.G. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J. Affect. Disord. 2017, 219, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Al-abri, K.; Edge, D.; Armitage, C.J. Prevalence and correlates of perinatal depression. Soc. Psychiatry Psychiatr. Epidemiol. 2023, 58, 1581–1590. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.; Bansal, A.; Schoenaker, D.A.J.M.; Cherbuin, N.; Peek, M.J.; Davis, D.L. Birth outcomes, health and healthcare needs of childbearing women following wildfire disasters: An integrative state of the science review. Environ. Health Perspect. 2022, 130, 86001. [Google Scholar] [CrossRef] [PubMed]
- Holstius, D.M.; Reid, C.E.; Jesdale, B.M.; Morello-Frosch, R. Birth weight following pregnancy during the 2003 Southern California wildfires. Environ. Health Perspect. 2012, 120, 1340–1345. [Google Scholar] [CrossRef] [PubMed]
- da Silva, A.M.C.; Moi, G.P.; Mattos, I.E.; Hacon, S.D. Low birth weight at term and the presence of fine particulate matter and carbon monoxide in the Brazilian Amazon: A population-based retrospective cohort study. BMC Pregnancy Childbirth 2014, 14, 309. [Google Scholar] [CrossRef]
- Abdo, M.; Ward, I.; O’Dell, K.; Ford, B.; Pierce, J.R.; Fischer, E.V.; Crooks, J.L. Impact of Wildfire Smoke on Adverse Pregnancy Outcomes in Colorado, 2007–2015. Int. J. Environ. Res. Public Health 2019, 16, 3720. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, M.H.; Behie, A.M. Effects of wildfire disaster exposure on male birth weight in an Australian population. Evol. Med. Public Health 2015, 2015, 344–354. [Google Scholar] [CrossRef]
- Chersich, M.F.; Pham, M.D.; Areal, A.; Haghighi, M.M.; Manyuchi, A.; Swift, C.P.; Wernecke, B.; Robinson, M.; Hetem, R.; Boeckmann, M.; et al. Associations between high temperatures in pregnancy and risk of preterm birth, low birth weight, and stillbirths: Systematic review and meta-analysis. BMJ 2020, 371, m3811. [Google Scholar] [CrossRef]
- Kuehn, L.; McCormick, S. Heat Exposure and Maternal Health in the Face of Climate Change. Int. J. Environ. Res. Public Health 2017, 14, 853. [Google Scholar] [CrossRef]
- Melody, S.M.; Ford, J.; Wills, K.; Venn, A.; Johnston, F.H. Maternal exposure to fine particulate matter from a coal mine fire and birth outcomes in Victoria, Australia. Environ. Int. 2019, 127, 233–242. [Google Scholar] [CrossRef]
- King, S.; Laplante, D.P. The effects of prenatal maternal stress on children’s cognitive development: Project Ice Storm. Stress 2005, 8, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Harville, E.; Xiong, X.; Buekens, P. Disasters and perinatal health: A systematic review. Obs. Gynecol. Surv. 2010, 65, 713–728. [Google Scholar] [CrossRef] [PubMed]
- Simcock, G.; Cobham, V.E.; Laplante, D.P.; Elgbeili, G.; Gruber, R.; Kildea, S.; King, S. A cross-lagged panel analysis of children’s sleep, attention, and mood in a prenatally stressed cohort: The QF2011 Queensland flood study. J. Affect. Disord. 2019, 255, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.; Chen, G.; He, P.; Zhang, L.; Zheng, X. Risk of cognitive impairment in children after maternal exposure to the 1998 Yangtze River flood during pregnancy: Analysis of data from China’s second National Sample Survey on Disability. Lancet Planet. Health 2020, 4, e522–e529. [Google Scholar] [CrossRef] [PubMed]
- Beaglehole, B.; Mulder, R.T.; Frampton, C.M.; Boden, J.M.; Newton-Howes, G.; Bell, C.J. Psychological distress and psychiatric disorder after natural disasters: Systematic review and meta-analysis. Br. J. Psychiatry 2018, 213, 716–722. [Google Scholar] [CrossRef] [PubMed]
- Newnham, E.A.; Mergelsberg, E.L.P.; Chen, Y.; Kim, Y.; Gibbs, L.; Dzidic, P.L.; Ishida DaSilva, M.; Chan, E.Y.Y.; Shimomura, K.; Narita, Z.; et al. Long term mental health trajectories after disasters and pandemics: A multilingual systematic review of prevalence, risk and protective factors. Clin. Psychol. Rev. 2022, 97, 102203. [Google Scholar] [CrossRef] [PubMed]
- Tang, B.; Liu, X.; Liu, Y.; Xue, C.; Zhang, L. A meta-analysis of risk factors for depression in adults and children after natural disasters. BMC Public Health 2014, 14, 623. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Meteorology. Hottest, Driest Year on Record Led to Extreme Bushfire Season. Available online: https://media.bom.gov.au/social/blog/2304/hottest-driest-year-on-record-led-to-extreme-bushfire-season/ (accessed on 16 November 2023).
- Vardoulakis, S.; Jalaludin, B.; Morgan, G.G.; Hanigan, I.C.; Johnston, F.H. Bushfire smoke: Urgent need for a national health protection strategy. Med. J. Aust. 2020, 212, 349–353.e341. [Google Scholar] [CrossRef]
- Australian Capital Territory Health Directorate. Air Quality in the ACT. Available online: https://health.act.gov.au/about-our-health-system/population-health/environmental-monitoring/monitoring-and-regulating-air (accessed on 16 November 2023).
- Rodney, R.M.; Swaminathan, A.; Calear, A.L.; Christensen, B.K.; Lal, A.; Lane, J.; Leviston, Z.; Reynolds, J.; Trevenar, S.; Vardoulakis, S.; et al. Physical and Mental Health Effects of Bushfire and Smoke in the Australian Capital Territory 2019-20. Front. Public Health 2021, 9, 682402. [Google Scholar] [CrossRef]
- Zhou, X.; Josey, K.; Kamareddine, L.; Caine, M.C.; Liu, T.; Mickley, L.J.; Cooper, M.; Dominici, F. Excess of COVID-19 cases and deaths due to fine particulate matter exposure during the 2020 wildfires in the United States. Sci. Adv. 2021, 7, eabi8789. [Google Scholar] [CrossRef]
- Bansal, A.; Cherbuin, N.; Leach, L.; Simmons, R.A.; Nolan, C.J. Wildfires and COVID-19: Syndemic impact on maternal and child health. Trends Endocrinol. Metab. 2023, 34, 779–782. [Google Scholar] [CrossRef] [PubMed]
- Roseboom, T.J.; Ozanne, S.E.; Godfrey, K.M.; Isasi, C.R.; Itoh, H.; Simmons, R.; Bansal, A.; Barker, M.; Plosch, T.; Sloboda, D.M.; et al. Unheard, unseen and unprotected: DOHaD council’s call for action to protect the younger generation from the long-term effects of COVID-19. J. Dev. Orig. Health Dis. 2021, 12, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Wenham, C.; Smith, J.; Davies, S.E.; Feng, H.; Grépin, K.A.; Harman, S.; Herten-Crabb, A.; Morgan, R. Women are most affected by pandemics—Lessons from past outbreaks. Nature 2020, 583, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Calear, A.L.; McCallum, S.; Morse, A.R.; Banfield, M.; Gulliver, A.; Cherbuin, N.; Farrer, L.M.; Murray, K.; Rodney Harris, R.M.; Batterham, P.J. Psychosocial impacts of home-schooling on parents and caregivers during the COVID-19 pandemic. BMC Public Health 2022, 22, 119. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Epidemiology 2007, 18, 805–835. [Google Scholar] [CrossRef] [PubMed]
- Dawel, A.; Shou, Y.; Smithson, M.; Cherbuin, N.; Banfield, M.; Calear, A.L.; Farrer, L.M.; Gray, D.; Gulliver, A.; Housen, T.; et al. The Effect of COVID-19 on Mental Health and Wellbeing in a Representative Sample of Australian Adults. Front. Psychiatry 2020, 11, 579985. [Google Scholar] [CrossRef] [PubMed]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Brown, T.A.; Chorpita, B.F.; Korotitsch, W.; Barlow, D.H. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behav. Res. Ther. 1997, 35, 79–89. [Google Scholar] [CrossRef]
- Antony, M.M.; Bieling, P.J.; Cox, B.J.; Enns, M.W.; Swinson, R.P. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol. Assess. 1998, 10, 176. [Google Scholar] [CrossRef]
- Ng, F.; Trauer, T.; Dodd, S.; Callaly, T.; Campbell, S.; Berk, M. The validity of the 21-item version of the Depression Anxiety Stress Scales as a routine clinical outcome measure. Acta Neuropsychiatr. 2007, 19, 304–310. [Google Scholar] [CrossRef]
- Lee, J.; Lee, E.H.; Moon, S.H. Systematic review of the measurement properties of the Depression Anxiety Stress Scales-21 by applying updated COSMIN methodology. Qual. Life Res. 2019, 28, 2325–2339. [Google Scholar] [CrossRef] [PubMed]
- Moya, E.; Larson, L.M.; Stewart, R.C.; Fisher, J.; Mwangi, M.N.; Phiri, K.S. Reliability and validity of depression anxiety stress scale (DASS)-21 in screening for common mental disorders among postpartum women in Malawi. BMC Psychiatry 2022, 22, 352. [Google Scholar] [CrossRef] [PubMed]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E., Jr. SF-36 health survey update. Spine 2000, 25, 3130–3139. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Employee Earnings and Hours Survey; Australian Bureau of Statistics: Canberra, Australia, 2021. [Google Scholar]
- Australian Bureau of Statistics. Education and Work Survey; Australian Bureau of Statistics: Canberra, Australia, 2022. [Google Scholar]
- Bryson, H.; Perlen, S.; Price, A.; Mensah, F.; Gold, L.; Dakin, P.; Goldfeld, S. Patterns of maternal depression, anxiety, and stress symptoms from pregnancy to 5 years postpartum in an Australian cohort experiencing adversity. Arch. Women’s Ment. Health 2021, 24, 987–997. [Google Scholar] [CrossRef] [PubMed]
- Crawford, J.; Cayley, C.; Lovibond, P.F.; Wilson, P.H.; Hartley, C. Percentile Norms and Accompanying Interval Estimates from an Australian General Adult Population Sample for Self-Report Mood Scales (BAI, BDI, CRSD, CES-D, DASS, DASS-21, STAI-X, STAI-Y, SRDS, and SRAS). Aust. Psychol. 2011, 46, 3–14. [Google Scholar] [CrossRef]
- Neria, Y.; Sullivan, G.M. Understanding the Mental Health Effects of Indirect Exposure to Mass Trauma Through the Media. JAMA 2011, 306, 1374–1375. [Google Scholar] [CrossRef]
- Takubo, Y.; Tsujino, N.; Aikawa, Y.; Fukiya, K.; Iwai, M.; Uchino, T.; Ito, M.; Akiba, Y.; Mizuno, M.; Nemoto, T. Psychological impacts of the COVID-19 pandemic on one-month postpartum mothers in a metropolitan area of Japan. BMC Pregnancy Childbirth 2021, 21, 845. [Google Scholar] [CrossRef]
- Wang, Z.; Liu, J.; Shuai, H.; Cai, Z.; Fu, X.; Liu, Y.; Xiao, X.; Zhang, W.; Krabbendam, E.; Liu, S.; et al. Mapping global prevalence of depression among postpartum women. Transl. Psychiatry 2021, 11, 543. [Google Scholar] [CrossRef]
- Murray, L.; Fearon, P.; Cooper, P. Postnatal Depression, Mother–Infant Interactions, and Child Development. In Identifying Perinatal Depression and Anxiety; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2015; pp. 139–164. [Google Scholar] [CrossRef]
- Walker, A.L.; Peters, P.H.; de Rooij, S.R.; Henrichs, J.; Witteveen, A.B.; Verhoeven, C.J.M.; Vrijkotte, T.G.M.; de Jonge, A. The Long-Term Impact of Maternal Anxiety and Depression Postpartum and in Early Childhood on Child and Paternal Mental Health at 11–12 Years Follow-Up. Front. Psychiatry 2020, 11, 562237. [Google Scholar] [CrossRef]
- Yang, K.; Wu, J.; Chen, X. Risk factors of perinatal depression in women: A systematic review and meta-analysis. BMC Psychiatry 2022, 22, 63. [Google Scholar] [CrossRef]
- Sousa, G.M.d.; Tavares, V.D.d.O.; de Meiroz Grilo, M.L.P.; Coelho, M.L.G.; Lima-Araújo, G.L.d.; Schuch, F.B.; Galvão-Coelho, N.L. Mental Health in COVID-19 Pandemic: A Meta-Review of Prevalence Meta-Analyses. Front. Psychol. 2021, 12, 703838. [Google Scholar] [CrossRef]
- Ahmad, M.; Vismara, L. The Psychological Impact of COVID-19 Pandemic on Women’s Mental Health during Pregnancy: A Rapid Evidence Review. Int. J. Environ. Res. Public Health 2021, 18, 7112. [Google Scholar] [CrossRef]
- Maharlouei, N.; Keshavarz, P.; Salemi, N.; Lankarani, K.B. Depression and anxiety among pregnant mothers in the initial stage of the Coronavirus Disease (COVID-19) pandemic in the southwest of Iran. Reprod. Health 2021, 18, 111. [Google Scholar] [CrossRef]
- Batterham, P.J.; Calear, A.L.; McCallum, S.M.; Morse, A.R.; Banfield, M.; Farrer, L.M.; Gulliver, A.; Cherbuin, N.; Rodney Harris, R.M.; Shou, Y.; et al. Trajectories of depression and anxiety symptoms during the COVID-19 pandemic in a representative Australian adult cohort. Med. J. Aust. 2021, 214, 462–468. [Google Scholar] [CrossRef] [PubMed]
| Survey Questions | ||
|---|---|---|
| Broad Bushfire Exposure | Acute Bushfire Exposure | “Were you evacuated from your home or workplace because of the threat of fire?” |
| “Were you personally involved in fighting bushfires threatening your own home or neighbourhood?” | ||
| “Were your own home, possessions or workplace damaged or destroyed?” | ||
| “Was your partner/spouse personally involved in fighting bushfires?” | ||
| “Did you suffer any injury due to the fires?” | ||
| “Did any relative or friend die or suffer injury due to the fires?” | ||
| “Did you own any animal that suffered as a result of the fires?” | ||
| “Did you feel very frightened or upset during the period of the fires?” | ||
| “Apart from defending your own home and neighbourhood, did you do any work involving the bushfires and/or their effects? (e.g., fighting fires, keeping order, dealing with health effects, restoring power, caring for victims)”. | ||
| “Were buildings in your suburb or area damaged or destroyed by fire?”, | ||
| “Did any relative or friend have their home, possessions or workplace damaged or destroyed?” | ||
| “Did you suffer significant financial loss due to the fires?” | ||
| “Did the bushfires impact on your health care appointments?” | ||
| “Did the bushfires impact on your access to medications/other health care supplies/baby care supplies?” | ||
| Smoke Exposure | During the period of 1st December 2019 to 14th of February 2020 what do you consider your bushfire smoke exposure was?” | |
| Broad COVID-19 Exposure | Acute COVID-19 Exposure | “I have been diagnosed positive for COVID-19” |
| “I have a family member who has been diagnosed positive by a laboratory test” | ||
| “I was directed by the health department to self-isolate” | ||
| “I have a family member who is currently or has been required to self-isolate” | ||
| “I have been tested for COVID-19—awaiting result” | ||
| “I have been tested for COVID-19—negative result” | ||
| “I have voluntarily self-isolated (current or previous)” | ||
| “I have been a contact of someone who has been diagnosed positive by a laboratory test” | ||
| “I know someone who has been or is currently required to self-isolate” | ||
| Preconception (n = 66) | Pregnant (n = 636) | New Baby (n = 217) | Total (n = 919) | p Value | |
|---|---|---|---|---|---|
| Age (years) | 0.009 | ||||
| Mean (SD) | 31.74 (4.63) | 31.80 (4.42) | 32.84 (4.30) | 32.04 (4.43) | |
| Tertiary education | 50 (75.8%) | 472 (74.2%) | 164 (75.6%) | 686 (74.6%) | 0.903 |
| Middle/high income | 62 (93.9%) | 611 (96.1%) | 213 (98.2%) | 886 (96.4%) | 0.193 |
| Parity | 0.916 | ||||
| Median (IQR) | 1 (1) | 1 (1) | 1 (1) | 1 (1) | |
| Prior depression | 22 (33.3%) | 108 (17.0%) | 30 (13.8%) | 160 (17.4%) | 0.001 |
| Prior anxiety | 28 (42.4%) | 220 (34.6%) | 66 (30.4%) | 314 (34.2%) | 0.182 |
| Wellbeing (WHO-5) | 0.667 | ||||
| Mean (SD) | 48.55 (19.51) | 50.29 (20.26) | 49.16 (20.77) | 49.90 (20.31) | |
| DASS depression score | 0.295 | ||||
| Mean (SD) | 2.35 (3.08) | 2.89 (3.36) | 3.09 (3.59) | 2.90 (3.40) | |
| DASS anxiety score | 0.628 | ||||
| Mean (SD) | 2.59 (2.95) | 2.24 (2.71) | 2.32 (3.12) | 2.29 (2.83) | |
| DASS stress score | 0.488 | ||||
| Mean (SD) | 5.45 (3.90) | 5.61 (4.16) | 5.97 (4.32) | 5.69 (4.18) | |
| DASS total score | 0.621 | ||||
| Mean (SD) | 10.39 (8.97) | 10.75 (9.16) | 11.39 (9.77) | 10.87 (9.29) | |
| Acute bushfire exposure | 0.782 | ||||
| Mean (SD) | 1.06 (0.93) | 1.15 (1.11) | 1.12 (0.95) | 1.13 (1.06) | |
| Broad bushfire exposure | 0.655 | ||||
| Mean (SD) | 1.97 (1.99) | 2.21 (2.21) | 2.24 (1.96) | 2.20 (2.14) | |
| Smoke exposure | 0.667 | ||||
| Not/mildly exposed | 5 (7.6%) | 44 (6.9%) | 13 (6.0%) | 62 (6.7%) | |
| Moderately exposed | 18 (27.3%) | 199 (31.3%) | 58 (26.7%) | 275 (29.9%) | |
| Severely exposed | 43 (65.2%) | 393 (61.8%) | 146 (67.3%) | 582 (63.3%) | |
| Acute COVID exposure | 0.214 | ||||
| Mean (SD) | 0.33 (0.57) | 0.22 (0.47) | 0.22 (0.45) | 0.23 (0.47) | |
| Broad COVID exposure | 0.139 | ||||
| Mean (SD) | 1.38 (1.30) | 1.11 (1.11) | 1.21 (1.12) | 1.15 (1.13) |
| Study | Population | Depression | Dep SD | Anxiety | Anx SD | Stress | Str SD | Total Score | SD |
|---|---|---|---|---|---|---|---|---|---|
| MC2020 | Preconception/pregnant/ post-partum women | 2.9 | 3.4 | 2.3 | 2.8 | 5.7 | 4.2 | 10.9 | 9.3 |
| Bryson et al. | Pregnant women | 2.9 | 3.3 | 3.4 | 3.3 | 5.4 | 4.0 | 11.7 | 9.4 |
| Crawford et al. | Adult Australian population | 2.6 | 3.9 | 1.7 | 2.8 | 4.0 | 4.2 | 8.3 | 9.8 |
| WHO-5 | Depression | Anxiety | Stress | |||||
|---|---|---|---|---|---|---|---|---|
| Intercept | 54.722 *** | 54.691 *** | 5.131 *** | 5.105 *** | 6.588 *** | 6.487 *** | 7.350 *** | 7.276 *** |
| p < 0.001 | p < 0.001 | p < 0.00001 | p < 0.00001 | p < 0.001 | p < 0.001 | p < 0.001 | p < 0.001 | |
| Age, yrs | −0.033 | −0.039 | −0.094 *** | −0.092 *** | −0.140 *** | −0.137 *** | −0.103 ** | −0.100 ** |
| p = 0.841 | p = 0.816 | p = 0.001 | p = 0.001 | p < 0.001 | p < 0.001 | p = 0.003 | p = 0.003 | |
| Parity, number | −1.599 | −1.541 | 0.439 ** | 0.423 ** | 0.535 *** | 0.516 *** | 0.615 *** | 0.588 *** |
| p = 0.062 | p = 0.073 | p = 0.002 | p = 0.003 | p = 0.00001 | p = 0.00001 | p = 0.0004 | p = 0.001 | |
| Tertiary education (yes) | 1.605 | 1.507 | −0.684 ** | −0.656 * | −0.901 *** | −0.869 *** | −0.824 * | −0.777 * |
| p = 0.331 | p = 0.363 | p = 0.012 | p = 0.016 | p = 0.00004 | p = 0.0001 | p = 0.013 | p = 0.020 | |
| Pregnancy phase (pregnant) | 1.889 | 1.952 | 0.515 | 0.499 | −0.368 | −0.383 | 0.105 | 0.079 |
| p = 0.470 | p = 0.456 | p = 0.229 | p = 0.243 | p = 0.287 | p = 0.266 | p = 0.842 | p = 0.880 | |
| Pregnancy phase (new baby) | 0.774 | 0.919 | 0.837 | 0.803 | −0.124 | −0.152 | 0.602 | 0.549 |
| p = 0.786 | p = 0.747 | p = 0.072 | p = 0.085 | p = 0.741 | p = 0.686 | p = 0.291 | p = 0.335 | |
| Bushfire exposure (acute) | −1.826 ** | 0.390 *** | 0.214 * | 0.565 *** | ||||
| p = 0.006 | p = 0.0003 | p = 0.013 | p = 0.00002 | |||||
| Bushfire exposure (broad) | −0.902 ** | 0.203 *** | 0.138 ** | 0.304 *** | ||||
| p = 0.006 | p = 0.0002 | p = 0.002 | p = 0.00001 | |||||
| Smoke exposure (moderate) | −2.552 | −2.528 | −0.171 | −0.181 | 0.479 | 0.459 | 0.888 | 0.867 |
| p = 0.371 | p = 0.375 | p = 0.714 | p = 0.697 | p = 0.204 | p = 0.222 | p = 0.120 | p = 0.128 | |
| Smoke exposure (severe) | −3.898 | −3.793 | 0.035 | 0.002 | 0.592 | 0.545 | 1.078 * | 1.018 |
| p = 0.152 | p = 0.165 | p = 0.938 | p = 0.998 | p = 0.100 | p = 0.130 | p = 0.048 | p = 0.062 | |
| Observations | 919 | 919 | 919 | 919 | 919 | 919 | 919 | 919 |
| Log Likelihood | −4061.52 | −4061.64 | −2396.80 | −2396.29 | −2201.50 | −2199.47 | −2583.26 | −2581.78 |
| Akaike Inf. Crit. | 8141.04 | 8141.28 | 4811.60 | 4810.58 | 4421.00 | 4416.93 | 5184.52 | 5181.57 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cherbuin, N.; Bansal, A.; Dahlstrom, J.E.; Carlisle, H.; Broom, M.; Nanan, R.; Sutherland, S.; Vardoulakis, S.; Phillips, C.B.; Peek, M.J.; et al. Bushfires and Mothers’ Mental Health in Pregnancy and Recent Post-Partum. Int. J. Environ. Res. Public Health 2024, 21, 7. https://doi.org/10.3390/ijerph21010007
Cherbuin N, Bansal A, Dahlstrom JE, Carlisle H, Broom M, Nanan R, Sutherland S, Vardoulakis S, Phillips CB, Peek MJ, et al. Bushfires and Mothers’ Mental Health in Pregnancy and Recent Post-Partum. International Journal of Environmental Research and Public Health. 2024; 21(1):7. https://doi.org/10.3390/ijerph21010007
Chicago/Turabian StyleCherbuin, Nicolas, Amita Bansal, Jane E. Dahlstrom, Hazel Carlisle, Margaret Broom, Ralph Nanan, Stewart Sutherland, Sotiris Vardoulakis, Christine B. Phillips, Michael J. Peek, and et al. 2024. "Bushfires and Mothers’ Mental Health in Pregnancy and Recent Post-Partum" International Journal of Environmental Research and Public Health 21, no. 1: 7. https://doi.org/10.3390/ijerph21010007
APA StyleCherbuin, N., Bansal, A., Dahlstrom, J. E., Carlisle, H., Broom, M., Nanan, R., Sutherland, S., Vardoulakis, S., Phillips, C. B., Peek, M. J., Christensen, B. K., Davis, D., & Nolan, C. J. (2024). Bushfires and Mothers’ Mental Health in Pregnancy and Recent Post-Partum. International Journal of Environmental Research and Public Health, 21(1), 7. https://doi.org/10.3390/ijerph21010007








