Setting Patient-Centered Priorities for Cardiovascular Disease in Central Appalachia: Engaging Stakeholder Experts to Develop a Research Agenda
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
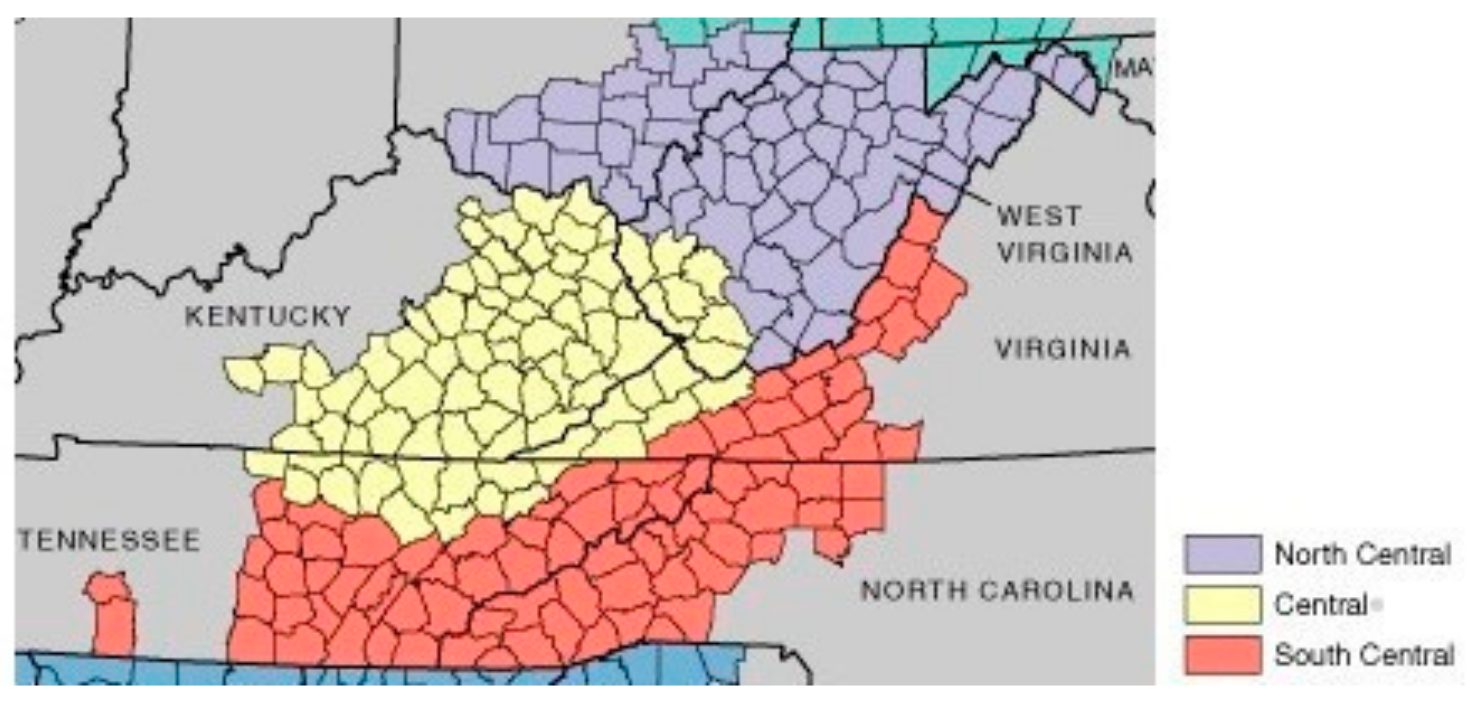
2.2. Study Setting
2.3. Study Approach
2.4. Study Design
2.5. Data Collection and Analysis
3. Results and Outcomes
CVD Patient-Centered Research Priorities
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, B.; Aversa, V.; Rouleau, K.; Lazare, K.; Sullivan, F.; Persaud, N. Identifying top 10 primary care research priorities from international stakeholders using a modified Delphi method. PLoS ONE 2018, 13, e0206096. [Google Scholar] [CrossRef]
- Farber, E.W.; Ali, M.K.; Van Sickle, K.S.; Kaslow, N.J. Psychology in patient-centered medical homes: Reducing health disparities and promoting health equity. Am. Psychol. 2017, 72, 28–41. [Google Scholar] [CrossRef]
- Mudd-Martin, G.; Biddle, M.J.; Chung, M.L.; Lennie, T.A.; Bailey, A.L.; Casey, B.R.; Novak, M.J.; Moser, D.K. Rural Appalachian Perspectives on Heart Health: Social Ecological Contexts. Am. J. Heal. Behav. 2014, 38, 134–143. [Google Scholar] [CrossRef] [PubMed]
- Mamudu, H.M.; Wang, L.; Veeranki, S.P.; Panchal, H.B.; Alamian, A.; Paul, T.K.; Budoff, M. Association Between Multiple Modifiable Risk Factors of Cardiovascular Disease and Hypertension among Asymptomatic Patients in Central Appalachia. South. Med. J. 2017, 110, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Welfare, M.R.; Colligan, J.; Molyneux, S.; Pearson, P.; Barton, J.R. The identification of topics for research that are important to people with ulcerative colitis. Eur. J. Gastroenterol. Hepatol. 2006, 18, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Lewin, P.G. “Coal is Not Just a Job, It’s a Way of Life”: The Cultural Politics of Coal Production in Central Appalachia. Soc. Probl. 2019, 66, 51–68. [Google Scholar] [CrossRef]
- Schept, J.; Mazurek, J.E. Layers of Violence: Coal Mining, Convict Leasing, and Carceral Tourism in Central Appalachia. Palgrave Handb. Prison. Tour. 2017, 171–190. [Google Scholar]
- Danzl, M.M.; Harrison, A.; Hunter, E.G.; Kuperstein, J.; Sylvia, V.; Maddy, K.; Campbell, S. “A Lot of Things Passed Me by”: Rural Stroke Survivors’ and Caregivers’ Experience of Receiving Education From Health Care Providers. J. Rural. Health 2016, 32, 13–24. [Google Scholar] [CrossRef]
- Mamudu, H.M.; Jones, A.; Paul, T.; Subedi, P.; Wang, L.; Alamian, A.; Alamin, A.E.; Blackwell, G.; Budoff, M. Geographic and Individual Correlates of Subclinical Atherosclerosis in an Asymptomatic Rural Appalachian Population. Am. J. Med. Sci. 2018, 355, 140–148. [Google Scholar] [CrossRef]
- Pollard, K.; Jacobsen, L.A. The Appalachian Region: A Data Overview from the 2011–2015 American Community Survey—Appalachian Regional Commission. Popul. Ref. Bur. Appalach. Reg. Comm. 2017, 70. [Google Scholar]
- Kwon, S.C.; Tandon, S.D.; Islam, N.; Riley, L.; Trinh-Shevrin, C. Applying a community-based participatory research framework to patient and family engagement in the development of patient-centered outcomes research and practice. Transl. Behav. Med. 2018, 8, 683–691. [Google Scholar] [CrossRef]
- PCORI. 2018. Available online: https://www.pcori.org/about-us/our-programs/engagement/public-and-patient-engagement/pcoris-stakeholders#:~:text=A%20broad%20range%20of%20communities,treating%20those%20with%20a%20condition (accessed on 23 December 2022).
- Crumby, A.S.; Holmes, E.R.; Rosenthal, M. Patient centered research to improve community involvement (PaRTICIpate) in diabetes self-management: A conference series for developing collaborations between researchers, stakeholders, and patients. J. Patient-Rep. Outcomes 2018, 2, 47. [Google Scholar] [CrossRef] [PubMed]
- Wallerstein, N.; Duran, B. Community-Based Participatory Research Contributions to Intervention Research: The Intersection of Science and Practice to Improve Health Equity. Am. J. Public Health 2010, 100 (Suppl. S1), S40–S46. [Google Scholar] [CrossRef]
- Sawford, K.; Dhand, N.K.; Toribio, J.-A.L.; Taylor, M.R. The use of a modified Delphi approach to engage stakeholders in zoonotic disease research priority setting. BMC Public Health 2014, 14, 182. [Google Scholar] [CrossRef]
- Israel, B.A.; Schulz, A.J.; Parker, E.A.; Becker, A.B. Community-based participatory research: Policy recommendations for promoting a partnership approach in health research. Educ. Health 2001, 14, 182–197. [Google Scholar]
- Khan, N.; Bacon, S.L.; Khan, S.; Perlmutter, S.; Gerlinsky, C.; Dermer, M.; Johnson, L.; Alves, F.; McLean, D.; Laupacis, A.; et al. Hypertension management research priorities from patients, caregivers, and healthcare providers: A report from the Hypertension Canada Priority Setting Partnership Group. J. Clin. Hypertens. 2017, 19, 1063–1069. [Google Scholar] [CrossRef]
- Abma, T.A.; Pittens, C.A.C.M.; Visse, M.; Elberse, J.E.; Broerse, J.E.W. Patient involvement in research programming and implementation: A responsive evaluation of the Dialogue Model for research agenda setting Patient involvement in research programming and implementation: A responsive evaluation of the Dialogue Model for res. Health Expect. 2015, 18, 2449–2464. [Google Scholar] [CrossRef]
- Pittens, C.A.C.M.; Elberse, J.E.; Visse, M.; Abma, T.A.; Broerse, J.E.W. Research agendas involving patients: Factors that facilitate or impede translation of patients’ perspectives in programming and implementation. Sci. Public Policy 2014, 41, 809–820. [Google Scholar] [CrossRef]
- Schölvinck, A.-F.M.; Pittens, C.A.C.M.; Broerse, J.E.W. Patient involvement in agenda-setting processes in health research policy: A boundary work perspective. Sci. Public Policy 2020, 47, 246–255. [Google Scholar] [CrossRef]
- Tai-Seale, M.; Sullivan, G.; Cheney, A.; Thomas, K.; Frosch, D. The Language of Engagement: “Aha!” Moments from Engaging Patients and Community Partners in Two Pilot Projects of the Patient-Centered Outcomes Research Institute. Perm. J. 2016, 20, 89–92. [Google Scholar] [CrossRef]
- Tong, A.; Chando, S.; Crowe, S.; Manns, B.; Winkelmayer, W.C.; Hemmelgarn, B.; Craig, J.C. Research Priority Setting in Kidney Disease: A Systematic Review. Am. J. Kidney Dis. 2015, 65, 674–683. [Google Scholar] [CrossRef]
- Odgers, H.L.; Tong, A.; Lopez-Vargas, P.; Davidson, A.; Jaffe, A.; McKenzie, A.; Pinkerton, R.; Wake, M.; Richmond, P.; Crowe, S.; et al. Research priority setting in childhood chronic disease: A systematic review. Arch. Dis. Child. 2018, 103, 942–951. [Google Scholar] [CrossRef] [PubMed]
- Hong, H.; Oh, H.J. The Effects of Patient-Centered Communication: Exploring the Mediating Role of Trust in Healthcare Providers. Health Commun. 2019, 35, 502–511. [Google Scholar] [CrossRef]
- Haley, B.; Heo, S.; Wright, P.; Barone, C.; Rettiganti, M.R.; Anders, M. Relationships among active listening, self-awareness, empathy, and patient-centered care in associate and baccalaureate degree nursing students. NursingPlus Open 2017, 3, 11–16. [Google Scholar] [CrossRef]
- Epstein, R.M.; Fiscella, K.; Lesser, C.S.; Strange, K.C. Why the Nation needs a policy push on patient-centred care. Health Aff. 2010, 29, 1489–1495. [Google Scholar] [CrossRef] [PubMed]
- Grady, C. Ethical Principles in Clinical Research. In Principles and Practice of Clinical Research; Elsevier Inc.: Amsterdam, The Netherlands, 2012; pp. 19–30. [Google Scholar]
- Constand, M.K.; MacDermid, J.C.; Dal Bello-Haas, V.; Law, M. Scoping review of patient-centered care approaches in healthcare. BMC Health Serv. Res. 2014, 14, 271. [Google Scholar] [CrossRef]
- Mensah, G.A.; Cooper, R.S.; Siega-Riz, A.M.; Cooper, L.A.; Smith, J.D.; Hendricks Brown, C.; Westfal, J.M.; Ofili, E.O.; Price, L.N.; Arteaga, S.; et al. Reducing cardiovascular disparities through community-engaged implementation research: A national heart, lung, and blood institute workshop report. Circ. Res. 2018, 122, 213–230. [Google Scholar] [CrossRef] [PubMed]
- Bokhour, B.G.; Fix, G.M.; Mueller, N.M.; Barker, A.M.; LaVela, S.L.; Hill, J.N.; Solomon, J.L.; Lukas, C.V. How can healthcare organizations implement patient-centered care? Examining a large-scale cultural transformation. BMC Health Serv. Res. 2018, 18, 168. [Google Scholar] [CrossRef]
- Zimmerman, E.B.; Cook, S.K.; Haley, A.D.; Woolf, S.H.; Price, S.K. A Patient and Provider Research Agenda on Diabetes and Hypertension Management. Am. J. Prev. Med. 2017, 53, 123–129. [Google Scholar] [CrossRef]
- Becker, K.L. Tell me your dreams and goals: Structuring communication exchanges to improve patient-centered care with chronic pain patients. Appl. Nurs. Res. 2020, 53, 151248. [Google Scholar] [CrossRef] [PubMed]
- Behringer, B.; Friedell, G.H. Appalachia: Where place matters in health. Prev. Chronic Dis. 2006, 3, A113. [Google Scholar] [PubMed]
- Cheng, P.; Roberts, L.; Nogaj, L.; Deprele, D.S.; Inrig, S. Comparing Two Worlds: The Impact of Trust on Preventative Medicine in Marginalized Populations in the US Appalachia and Peruvian Andes. South Calif. Conf. Undergrad. Res. 2017. [Google Scholar]
- Lindson, N.; Richards-Doran, D.; Heath, L.; Hartmann-Boyce, J. Setting research priorities in tobacco control: A stakeholder engagement project. Addiction 2017, 112, 2257–2271. [Google Scholar] [CrossRef]
- Global Burden of Cardiovascular Diseases Collaboration; Roth, G.A.; Johnson, C.O.; Abate, K.H.; Abd-Allah, F.; Ahmed, M.; Alam, K.; Alam, T.; Alvis-Guzmán, N.; Ansari, H.; et al. The Burden of Cardiovascular Diseases Among US States, 1990–2016. JAMA Cardiol. 2018, 3, 375–389. [Google Scholar] [PubMed]
- Poitras, M.-E.; Maltais, M.-E.; Bestard-Denommé, L.; Stewart, M.; Fortin, M. What are the effective elements in patient-centered and multimorbidity care? A scoping review. BMC Health Serv. Res. 2018, 18, 446. [Google Scholar] [CrossRef]
- Carroll, S.L.; Embuldeniya, G.; Abelson, J.; McGillion, M.; Berkesse, A.; Healey, J.S. Questioning patient engagement: Research scientists’ perceptions of the challenges of patient engagement in a cardiovascular research network. Patient Prefer. Adherence 2017, 11, 1573–1583. [Google Scholar] [CrossRef]
| Round Number and Activity/Goal | Methodology/Process |
|---|---|
| Round 1. Stakeholder experts vote for top five priorities | Participants were asked to compile and rank their top five priorities for cardiovascular disease, based on their expertise or experience. Thematic analysis was used to analyze the collected data. The response rate was 14%. |
| Round 2. Ranking of Priorities found within qualitative data | Using a 15-question instrument, experts were asked to select a specific number of their top research priorities based on the following categories: (1) Patient-centered care; (2) CVD risk factors; (3) Psychosocial determinants of CVD; (4) Social determinants of CVD. A total of 42/80 experts responded to Round II questionnaire (14 patients/non-licensed caregivers, 15 community stakeholders, and 13 professional/providers) The response rate was 52%. |
| Further narrowing of priorities | Round II data analyzed. Data were analyzed using descriptive statistics in MS Excel and presented as percentages with illustrations in bar graph format |
| Round 3. CVD Sharing Session at CVD Appalachia Conference II and Delphi Round III. Discussion and validation | Participants gathered at a conference to determine what priorities would move forward to make up the final research agenda. A paper-based survey was administered. Each closed-ended question asked for a priority ranking, with only one priority being selected from each question. Thirty-one out of forty stakeholders (7 patients, 18 providers, and 6 community stakeholders) submitted their responses. The response rate was 77.5%. |
| Alignment of research agenda with PCORI initiatives | Fifteen priorities mapped to major areas. Six of the 15 priorities were patient-centered |
| Characteristics | Round 1 n (%) | Round 2 n (%) | Round 3 n (%) |
|---|---|---|---|
| State | |||
| Kentucky | 0 (0) | 3 (7) | 0 (0) |
| North Carolina | 0 (0) | 2 (5) | 2 (6) |
| Ohio | 1 (10) | 5 (12) | 3 (10) |
| Tennessee | 6 (54) | 22 (52) | 15 (48) |
| Virginia | 1 (10) | 7 (17) | 6 (19) |
| West Virginia | 3 (27) | 3 (7) | 5 (17) |
| Stakeholder Type | |||
| Patient/Non-licensed caregiver | 7 (64) | 14 (33) | 7 (23) |
| Provider/Professional | 2 (18) | 13 (31) | 18 (58) |
| Community stakeholder | 2 (18) | 15 (36) | 6 (19) |
| Demographic | |||
| Sex | |||
| Male | 2 (18) | 13 (31) | 14 (45) |
| Female | 9 (82) | 29 (69) | 17 (72) |
| Round Number and Goal | Outcomes |
|---|---|
| Round 1. Stakeholder experts vote for top five priorities | Fifty-five priorities were obtained from 11 experts. The priorities were then grouped into 7 major focus areas. The top five priorities generated: (1) nutrition education and best practices; (2) education for heart disease prevention; (3) increased opportunities for free and no-cost exercise and physical activities; (4) reducing cost of healthcare for heart disease; and (5) treatment of heart disease and stroke |
| Round 2. Ranking of priorities found within qualitative data | A parsimonious set of priorities was selected by 42 experts from each category. Data ready for analysis to determine the research agenda twenty-four (24) items identified. |
| Round 3. CVD Sharing Session at CVD Appalachia Conference II and Delphi Round III. Discussion and validation | Further input from 31 experts to determine final priorities. Refined list derived. Fifteen (15) items were identified; six of the 15 priorities were patient-centered as shown in Table 2 |
| Alignment of research agenda with PCORI initiatives | Research agenda established by a consensus of Central Appalachia community stakeholders |
| Priority Areas | Round 1 | Round 2 | Round 3 |
|---|---|---|---|
| (1) Patient-centered care | Education Lifestyle | More time with healthcare providers Better communication between providers and patients Shorter wait times for scheduling appointments Communicate and provide education to patients on their level | Communicate and provide education to patients on their level Shorter wait times for scheduling appointments Empower and motivate patients to take responsibility for their health and illnesses |
| (2) CVD risk factors | Nutrition | Prevention of heart disease education Knowledge and education about the prevention of heart disease and risk factors Knowledge and skills in preparation of heart-healthy foods Knowledge and skills in reducing intake of sodium Knowledge and skills to prevent tobacco use Regular screenings for blood pressure, glucose and cardiac calcium | Knowledge and education about the prevention of heart disease and risk factors Prevention of heart disease education and skills on prevention of risk factors |
| (3) Psychosocial determinants of health | Prevention | Knowledge and skills on how to reduce and manage stress Skills to prevent nicotine addiction | Knowledge and skills on how to reduce and manage stress Skills to prevent nicotine addiction |
| (4) Social determinants of health | Physical Activity Nutrition | Access to affordable healthy food Access to care for heart disease Increase availability of no-cost walking options and exercise places in the community Lower costs for uninsured | Knowledge and education about physical activities for all ages |
| (5) CVD policies and programs | Lifestyle Education Cost | Programs that target high-risk and low-socioeconomic populations to promote healthy lifestyles Affordable public transportation to access healthy lifestyle programs and sites | Programs that target high-risk and low-socioeconomic populations to promote healthy lifestyles School budgets to promote physical education, nutrition, and health education |
| (6) Medication adherence | Cost Education | Better information and explanation of medications Affordable medications | Affordable medications |
| (7) Managing CVD patient population | Education Lifestyle Prevention Screening | Healthcare providers to conduct community outreach and/or outreach practices Availability of mobile units to screen and treat heart disease Heart disease specialists in rural areas Empower/motivate patients to take responsibility for illness/health | Access to quality healthcare providers Heart disease specialists in rural areas More information on lifestyle changes versus relying solely on medications |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nyarambi, D.; Osedeme, F.; Mamudu, H.M.; Littleton, M.A.; Poole, A.M.; Blair, C.; Voigt, C.; Gregory, R.; Drozek, D.; Stewart, D.W.; et al. Setting Patient-Centered Priorities for Cardiovascular Disease in Central Appalachia: Engaging Stakeholder Experts to Develop a Research Agenda. Int. J. Environ. Res. Public Health 2023, 20, 5660. https://doi.org/10.3390/ijerph20095660
Nyarambi D, Osedeme F, Mamudu HM, Littleton MA, Poole AM, Blair C, Voigt C, Gregory R, Drozek D, Stewart DW, et al. Setting Patient-Centered Priorities for Cardiovascular Disease in Central Appalachia: Engaging Stakeholder Experts to Develop a Research Agenda. International Journal of Environmental Research and Public Health. 2023; 20(9):5660. https://doi.org/10.3390/ijerph20095660
Chicago/Turabian StyleNyarambi, Dumisa, Fenose Osedeme, Hadii M. Mamudu, Mary A. Littleton, Amy M. Poole, Cynthia Blair, Carl Voigt, Rob Gregory, David Drozek, David W. Stewart, and et al. 2023. "Setting Patient-Centered Priorities for Cardiovascular Disease in Central Appalachia: Engaging Stakeholder Experts to Develop a Research Agenda" International Journal of Environmental Research and Public Health 20, no. 9: 5660. https://doi.org/10.3390/ijerph20095660
APA StyleNyarambi, D., Osedeme, F., Mamudu, H. M., Littleton, M. A., Poole, A. M., Blair, C., Voigt, C., Gregory, R., Drozek, D., Stewart, D. W., Weierbach, F. M., Paul, T. K., Flores, E. K., & Wei, H. (2023). Setting Patient-Centered Priorities for Cardiovascular Disease in Central Appalachia: Engaging Stakeholder Experts to Develop a Research Agenda. International Journal of Environmental Research and Public Health, 20(9), 5660. https://doi.org/10.3390/ijerph20095660







