Evidence of Disaster Planning by Home Care Providers: An Integrative Literature Review
Abstract
1. Introduction
2. Methods
3. Results
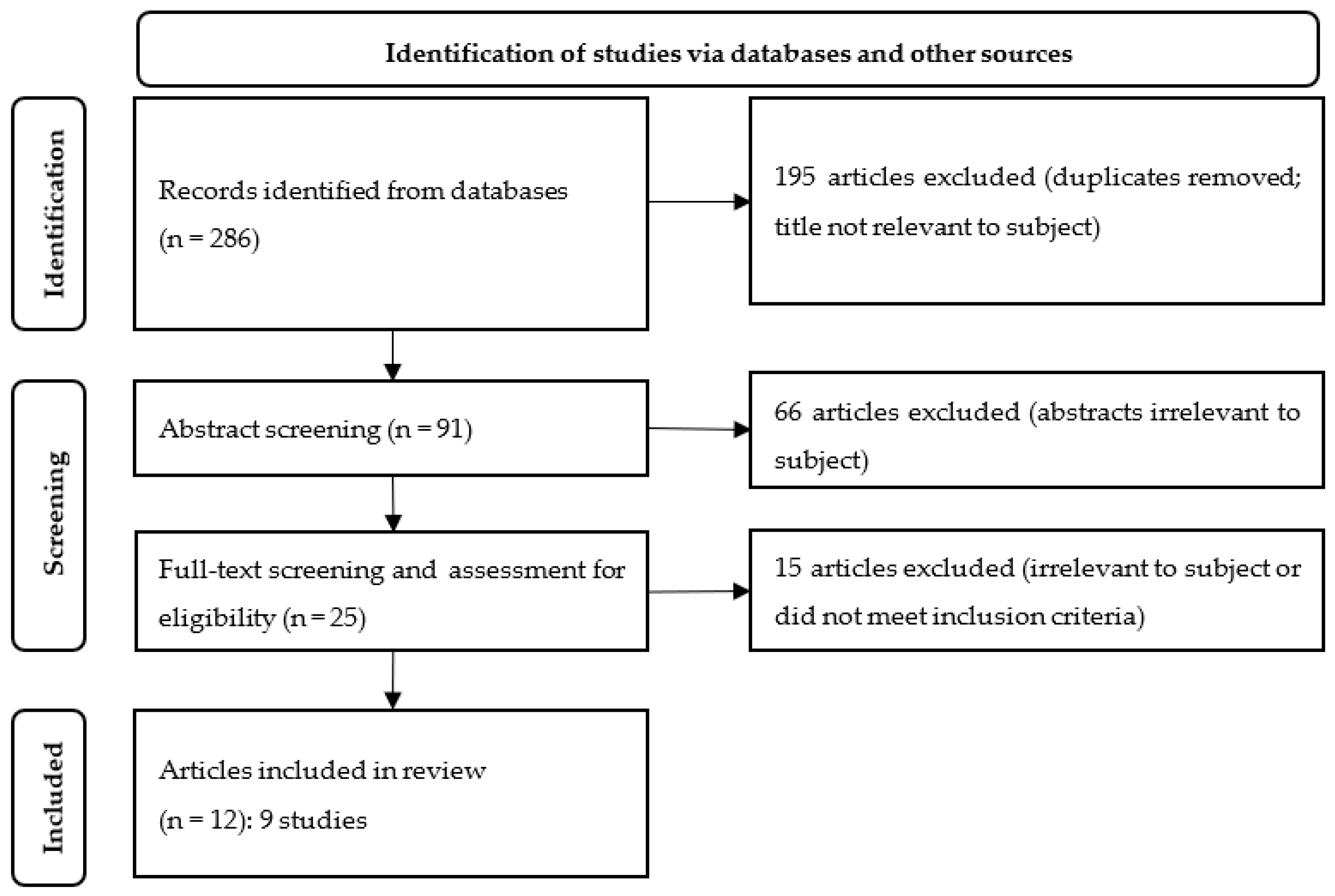
3.1. Results of the Literature Search
3.2. Characteristics of the Included Studies
3.3. Thematic Analysis
3.3.1. Internal Operational Arrangements
- Organisational disaster plan
- Staff disaster arrangements
- In-house disaster training
3.3.2. Information and Networking Activities
- Disseminating information to staff (internally)
- Disseminating information to home care users
- Disseminating information to others (externally)
- Networking
3.3.3. Measures for Safeguarding Patient Care
- Personal patient disaster plan
- Disaster education
- Triage/patient classification
- Evacuation preparedness
3.4. Quality Appraisal
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centre for Research on the Epidemiology of Disasters (CRED). 2021 Disasters in Numbers; CRED: Brussels, Belgium, 2022; Available online: https://cred.be/sites/default/files/2021_EMDAT_report.pdf (accessed on 2 December 2022).
- Hiete, M.; Merz, M.; Schultmann, F. Scenario-based impact analysis of a power outage on healthcare facilities in Germany. Int. J. Disaster Resil. Built Environ. 2011, 2, 222–244. [Google Scholar] [CrossRef]
- UNDRR—United Nations Office for Disaster Risk Reduction. Sendai Framework for Disaster Risk Reduction 2015—2030. Available online: https://www.undrr.org/publication/sendai-framework-disaster-risk-reduction-2015-2030 (accessed on 2 December 2022).
- Federal Ministry of the Interior and Community (BMI). German Strategy for Strengthening Resilience to Disasters Implementing the Sendai Framework for Disaster Risk Reduction (2015–2030)—Germany’s Contribution 2022–2030. Available online: https://www.bbk.bund.de/SharedDocs/Downloads/DE/Mediathek/Publikationen/Sendai-Katrima/deutsche-strategie-resilienz-kurz-eng_download.pdf?__blob=publicationFile&v=4 (accessed on 12 December 2022).
- Eurostat. 1 in 5 Households in Need in the EU Use Professional Homecare Services. Available online: https://ec.europa.eu/eurostat/de/web/products-eurostat-news/-/ddn-20180228-1 (accessed on 2 December 2022).
- WHO—World Health Organization. Home Care in Europe. The Solid Facts; WHO Regional Office for Europe: Copenhagen, Denmark, 2008. [Google Scholar]
- Al-Rousan, T.M.; Rubenstein, L.M.; Wallace, R.B. Preparedness for natural disasters among older US adults: A nationwide survey. Am. J. Public Health 2015, 105 (Suppl. S4), 621–626. [Google Scholar] [CrossRef] [PubMed]
- Dostal, P.J. Vulnerability of Urban Homebound Older Adults in Disasters: A Survey of Evacuation Preparedness. Disaster Med. Public Health Prep. 2015, 9, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Ewers, M.; Lehmann, Y. Krisen, Notfälle und Katastrophen in der Häuslichen und Gemeindebasierten Pflege; Literatursynthese & Bibliograpfie. Working Paper No. 21-02 der Unit Gesundheitswissenschaften und ihre Didaktik; Charité—Universitätsmedizin: Berlin, Germany, 2021. [Google Scholar] [CrossRef]
- Genet, N.; Boerma, W. Chapter 1 Introduction and background. In Home Care across Europe: Current Structure and Future Challenges; WHO, Regional Office for Europe: Copenhagen, Denmark, 2012. [Google Scholar]
- WHO—World Health Organization. Health Emergency and Disaster Risk Management Framework; WHO: Geneva, Switzerland, 2019; Available online: https://apps.who.int/iris/bitstream/handle/10665/326106/9789241516181-eng.pdf (accessed on 16 December 2022).
- Teramoto, C.; Nagata, S.; Okamoto, R.; Suzuki, R.; Kishi, E.; Nomura, M.; Jojima, N.; Nishida, M.; Koide, K.; Kusano, E.; et al. Identifying Residents’ Health Issues Six Weeks after the Great East Japan Earthquake. Public Health Nurs. 2015, 32, 654–661. [Google Scholar] [CrossRef] [PubMed]
- Claver, M.L.; Wyte-Lake, T.; Dobalian, A. Disaster Preparedness in Home-based Primary Care: Policy and Training. Prehosp. Disaster Med. 2015, 30, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Department of Health and Human Services (HHS); Centers for Medicare & Medicaid Services (CMS). Medicare and Medicaid Programs; Emergency Preparedness Requirements for Medicare and Medicaid Participating Providers and Suppliers. Fed. Regist. 2016, 81, 63859–64044. [Google Scholar]
- Wyte-Lake, T.; Claver, M.; Griffin, A.; Dobalian, A. The role of the home-based provider in disaster preparedness of a vulnerable population. Gerontology 2014, 60, 336–345. [Google Scholar] [CrossRef] [PubMed]
- Bell, S.A.; Dickey, S.; Rosemberg, M.A. “You get three different hats on and try to figure it out:” home based care provision during a disaster. BMC Nurs. 2021, 20, 155. [Google Scholar] [CrossRef] [PubMed]
- Blättner, B.; Georgy, S.; Grewe, H.A. Sicherstellung ambulanter Pflege in ländlichen Regionen bei Extremwetterereignissen. In Regionale Klimaanpassung. Herausforderungen—Lösungen—Hemmnisse—Umsetzungen am Beispiel Nordhessens; Roßnagel, A., Ed.; University Press: Kassel, Germany, 2013; pp. 267–296. [Google Scholar]
- Lehmann, Y.; Thiele, A.; Ewers, M. Vorsorge, Management und Bewältigung von Katastrophen aus Sicht Ambulanter Pflegedienste; Befragungsergebnisse Zum IST-Zustand. Working Paper No. 21-03 der Unit Gesundheitswissenschaften und ihre Didaktik; Charité—Universitätsmedizin Berlin: Berlin, Germany, 2021. [Google Scholar] [CrossRef]
- Wyte-Lake, T.; Claver, M.; Dalton, S.; Dobalian, A. Disaster Planning for Home Health Patients and Providers: A Literature Review of Best Practices. Home Health Care Manag. Pract. 2015, 27, 247–255. [Google Scholar] [CrossRef]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef] [PubMed]
- Whittemore, R.; Knafl, R. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef] [PubMed]
- Booth, A. Clear and present questions: Formulating questions for evidence-based practice. Library Hi Tech 2006, 24, 355–368. [Google Scholar] [CrossRef]
- Inglesby, T. Progress in Disaster Planning and Preparedness Since 2001. JAMA 2011, 306, 1372–1373. [Google Scholar] [CrossRef]
- Carbone, E.; Thomas, E. Science as the Basis of Public Health Emergency Preparedness and Response Practice: The Slow but Crucial Evolution. Am. J. Public Health 2018, 108 (Suppl. S5), S383–S386. [Google Scholar] [CrossRef] [PubMed]
- Hong, Q.A.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; et al. Improving the content validity of the mixed methods appraisal tool: A modified e-Delphi study. J. Clin. Epidemiol. 2019, 111, 49–59. [Google Scholar] [CrossRef]
- Pace, R.; Pluye, P.; Bartlett, G.; Macaulay, A.C.; Salsberg, J.; Jagosh, J.; Seller, R. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int. J. Nurs. Stud. 2012, 49, 47–53. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, A.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Balinsky, W. The Home Care Emergency Response to the September 11 Tragedy. Caring 2003, 22, 38–40. [Google Scholar] [PubMed]
- Balinsky, W.; Sturman, M. Since 9/11, Where has the Urgency Gone? Emergency Preparedness in the Home Care Environment—A Follow Up Study—Part I. Caring 2006, 25, 41–47. [Google Scholar]
- Balinsky, W.; Sturman, M. Since 9/11, Where has the Urgency Gone? Emergency Preparedness in the Home Care Environment—A Follow Up Study—Part 2. Caring 2006, 25, 76–81. [Google Scholar] [PubMed]
- Wyte-Lake, T.; Claver, M.; Johnson-Koenke, R.; Davis, D.; Dobalian, A. Hurricanes Harvey, Irma, and Maria: Exploring the Role of Home-Based Care Programs. Disaster Med. Public Health Prep. 2020, 14, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Wyte-Lake, T.; Der-Martirosian, C.; Chu, K.; Johnson-Koenke, R.; Dobalian, A. Preparedness and response activities of the US Department of Veterans Affairs (VA) home-based primary care program around the fall 2017 hurricane season. BMC Public Health 2020, 26, 20. [Google Scholar] [CrossRef]
- ASPR TRACIE—Administration for Strategic Preparedness and Response, Technical Resources, Assistance Center, and Information Exchange. Medical Surge and the Role of Home Health and Hospice Agencies; Department of Health & Human Services: Washington, DC, USA, 2019.
- Daugherty, J.D.; Eiring, H.; Blake, S.; Howard, D. Disaster preparedness in home health and personal-care agencies: Are they ready? Gerontology 2012, 58, 322–330. [Google Scholar] [CrossRef] [PubMed]
- Kirkpatrick, D.V.; Bryan, M. Hurricane emergency planning by home health providers serving the poor. J. Health Care Poor Underserved 2007, 18, 299–314. [Google Scholar] [CrossRef]
- Laditka, S.B.; Laditka, J.N.; Cornman, C.B.; Davis, C.B.; Chandlee, M.J. Disaster preparedness for vulnerable persons receiving in-home, long-term care in South Carolina. Prehosp. Disaster Med. 2008, 23, 133–142. [Google Scholar] [CrossRef]
- Wyte-Lake, T.; Claver, M.; Der-Martirosian, C.; Davis, D.; Dobalian, A. Developing a Home-Based Primary Care Disaster Preparedness Toolkit. Disaster Med. Public Health Prep. 2017, 11, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Wyte-Lake, T.; Claver, M.; Tubbesing, S.; Davis, D.; Dobalian, A. Development of a Home Health Patient Assessment Tool for Disaster Planning. Gerontology 2019, 65, 353–361. [Google Scholar] [CrossRef]
- Zane, R.; Biddinger, P. Home Health Patient Assessment Tools: Preparing for Emergency Triage; Prepared by Abt Associates under Contract No. 290-02-0600-011. AHRQ Publication No. 11-M020-EF; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2011.
- Kimin, A.; Nurachmah, E.; Lestari, F.; Gayatri, D. Factors affecting nurses’ ability to provide effective care in a disaster response: A review. J. Public Health Res. 2021, 11, 2732. [Google Scholar] [CrossRef] [PubMed]
- Pierce, R.J.; Morley, S.K.; West, T.A.; Pentecost, P.; Upton, L.A.; Banks, L. Improving Long-Term Care Facility Disaster Preparedness and Response: A Literature Review. Disaster Med. Public Health Prep. 2017, 11, 140–149. [Google Scholar] [CrossRef]
- Labrague, L.J.; Hammad, K.; Gloe, D.S.; McEnroe-Petitte, D.M.; Fronda, D.C.; Obeidat, A.A.; Leocadio, M.C.; Cayaban, A.R.; Mirafuentes, E.C. Disaster preparedness among nurses: A systematic review of literature. Int. Nurs. Rev. 2018, 65, 41–53. [Google Scholar] [CrossRef]
- Miyamori, D.; Yoshida, S.; Kashima, S.; Koike, S.; Ishii, S.; Matsumoto, M. Discontinuation of long-term care among persons affected by the 2018 Japan Floods: A longitudinal study using the Long-term Care Insurance Comprehensive Database. BMC Geriatr. 2022, 22, 168. [Google Scholar] [CrossRef] [PubMed]
- Hata, K.; Hata, M. Study on the Issues Faced by Home-Visit Nursing Stations for Repletion and Reinforcement of Disasters Preparedness. Gan Kagaku Ryoho 2019, 46 (Suppl. S1), 129–131. [Google Scholar]
- Kyota, K.; Tsukasaki, K.; Itatani, T. Disaster preparedness among families of older adults taking oral medications. Home Health Care Serv. Q. 2018, 37, 325–335. [Google Scholar] [CrossRef] [PubMed]
- Rokkas, P.; Cornell, V.; Steenkamp, M. Disaster preparedness and response: Challenges for Australian public health nurses—A literature review. Nurs. Health Sci. 2014, 16, 60–66. [Google Scholar] [CrossRef] [PubMed]
| Search Components | Search Terms |
|---|---|
| Setting: Home care | home care services [MeSH Terms]; agency, home care [MeSH Terms]; home care [TIAB]; home nursing [TIAB]; home- and community-based service * [TIAB]; home-based primary care program * [TIAB]; HBPC [TIAB]; home health [TIAB]; domestic health care [TIAB]; domiciliary care [TIAB] |
| Intervention and Evaluation: Measures designed to help home care organisations improve disaster preparedness, and the outcome/evaluation of these measures | disaster planning [MeSH Terms]; emergency shelter [MeSH Terms]; disaster medicine [MeSH Terms]; emergency medicine [MeSH Terms]; civil defense [MeSH Terms]; disaster management [TIAB]; emergency management [TIAB]; disaster nursing [TIAB]; disaster role [TIAB]; disaster training [TIAB]; relief planning [TIAB]; evacuation [TIAB]; disaster evaluation [TIAB]; disaster mitigation [TIAB]; disaster preparedness [TIAB]; disaster response [TIAB]; disaster recovery [TIAB]; emergency preparedness [TIAB]; emergency response [TIAB]; disaster relief [TIAB]; disaster risk reduction [TIAB] |
| Authors (Year); Origin | Title | Aims |
|---|---|---|
| ASPR TRACIE (2019) [33]; USA | Medical Surge and the Role of Home Health and Hospice Agencies (HHA) | To learn more about the implementation of the emergency management activities of Medicare-certified home health care and hospice agencies following the 2016 Final Rule of Centers for Medicare & Medicaid Services; to address these agencies’ (technical) assistance needs. |
| Balinsky 2003 [28]; Balinsky & Sturman 2006 [29]; Balinsky & Sturman 2006 [30]; USA | The Home Care Emergency Response to the September 11 Tragedy (1); Emergency Preparedness in the Home Care Environment–A Follow Up Study -Part I. Since 9/11, where has the urgency gone? (2); Emergency Preparedness in the Home Care Environment–A Follow Up Study -Part II. Since 9/11, where has the urgency gone? Are we really prepared? (3) | To examine the experiences of home care agencies in New York City and their losses after the 11 September attacks in order to develop recommendations (1); to examine the progress made in implementing the recommendations (2, 3). |
| Daugherty et al. (2012) [34]; USA | Disaster Preparedness in Home Health and Personal-Care Agencies: Are they ready? | To explore disaster preparedness policies and agency practices; to identify opportunities for coordination with disaster preparedness officials. |
| Kirkpatrick & Bryan (2007) [35]; USA | Hurricane Emergency Planning by Home Health Providers. Serving the Poor. | To gather critical information in order to help improve the response to community disasters that affect indigent populations, with a focus on emergency planning among home health care providers. |
| Laditka et al. (2008) [36]; USA | Disaster Preparedness for Vulnerable Persons Receiving In-Home, Long-Term Care in South Carolina. | To examine how agencies in South Carolina that provide in-home health care and personal care services help vulnerable clients prepare for disasters as well as how these agencies could improve their clients’ preparedness. |
| Wyte-Lake et al. (2017) [37]; USA | Developing a Home-based Primary Care Disaster Preparedness Toolkit | To examine the utility of an evidence-based disaster preparedness toolkit in the Veterans Health Administration’s (VHA) Home-Based Primary Care (HBPC) programme; to evaluate the toolkit. |
| Wyte-Lake et al. (2019) [38]; USA | Development of a Home Health Patient Assessment Tool for Disaster Planning | To develop a checklist-style tool that can be used to guide practitioners of the Veterans Health Administration’s (VHA) Home-Based Primary Care (HBPC) programme in assessing their patients’ disaster preparedness; to explore the utility of the tool’s implementation. |
| Wyte-Lake et al. (2020) [31]; Wyte-Lake et al. (2020) [32]; USA | Hurricanes Harvey, Irma and Maria: Exploring the Role of Home-based Care Programs (1) Preparedness and response activities of the US Department of Veterans Affairs (VA) home-based primary care (HBPC) program around the fall 2017 hurricane season (2) | To examine the activities of the nine VA HBPC programmes that were impacted during the 2017 Fall Hurricane Season; to develop a multi-layered understanding of what support the programmes need in the aftermath of hurricanes in order to better prepare their patients and staff for future disasters. |
| Zane & Biddinger (2011) [39]; USA | Home health Assessment Tools: Preparing for Emergency Triage | To develop a patient risk assessment tool that enables home care services, hospitals, and emergency planners to anticipate the care needs of all home care patients in a community in the event of a disaster. |
| Study | Organisational Disaster Plans | Staff Disaster Arrangements | In-house Disaster Training |
|---|---|---|---|
| ASPR TRACIE (2019) [33] | ✓ | ✓ | |
| Balinsky (2003) [28]; Balinsky & Sturman (2006) [29]; Balinsky & Sturman (2006) [30] | ✓ | ✓ | ✓ |
| Daugherty et al. (2012) [34] | ✓ | ✓ | |
| Kirkpatrick & Bryan (2007) [35] | ✓ | ✓ | |
| Laditka et al. (2008) [36] | ✓ | ✓ | |
| Wyte-Lake et al. (2017) [37] | ✓ | ✓ | |
| Wyte-Lake et al. (2019) [38] | |||
| Wyte-Lake et al. (2020) [31]; Wyte-Lake et al. (2020) [32] | ✓ | ||
| Zane & Biddinger (2011) [39] |
| Study | Information Procedures | Networking | ||
|---|---|---|---|---|
| Internal | For Home Care Users | External | ||
| ASPR TRACIE (2019) [33] | ✓ | ✓ | ✓ | ✓ |
| Balinsky (2003) [28]; Balinsky & Sturman (2006) [29]; Balinsky & Sturman (2006) [30] | ✓ | ✓ | ✓ | ✓ |
| Daugherty et al. (2012) [34] | ✓ | ✓ | ||
| Kirkpatrick & Bryan (2007) [35] | ✓ | ✓ | ✓ | ✓ |
| Laditka et al. (2008) [36] | ✓ | ✓ | ✓ | |
| Wyte-Lake et al. (2017) [37] | ✓ | |||
| Wyte-Lake et al. (2019) [38] | ✓ | ✓ | ||
| Wyte-Lake et al. (2020) [31]; Wyte-Lake et al. (2020) [32] | ✓ | ✓ | ✓ | |
| Zane & Biddinger (2011) [39] | ✓ | ✓ | ||
| Study | Personal Patient Disaster Plan | Disaster Education | Triage/Patient Classification | Evacuation |
|---|---|---|---|---|
| ASPR TRACIE (2019) [33] | ✓ | ✓ | ✓ | ✓ |
| Balinsky (2003) [28]; Balinsky & Sturman (2006) [29]; Balinsky & Sturman (2006) [30] | ✓ | |||
| Daugherty et al. (2012) [34] | ✓ | ✓ | ✓ | |
| Kirkpatrick & Bryan (2007) [35] | ✓ | ✓ | ||
| Laditka et al. (2008) [36] | ✓ | ✓ | ✓ | ✓ |
| Wyte-Lake et al. (2017) [37] | ||||
| Wyte-Lake et al. (2019) [38] | ✓ | ✓ | ✓ | ✓ |
| Wyte-Lake et al. (2020) [31]; Wyte-Lake et al. (2020) [32] | ✓ | ✓ | ✓ | ✓ |
| Zane & Biddinger (2011) [39] | ✓ | ✓ |
| Authors (Year); Origin | Methods/Sample | Quality Appraisal (MMAT) |
|---|---|---|
| ASPR TRACIE (2019) [33]; USA | Mixed-methods design; quantitative: online survey of leaders of Medicare-certified home health and hospice agencies from 43 states (n = 245); qualitative: semi-structured in-depth telephone interviews (n = 25) | 5/5 criteria met; self-selection bias |
| Balinsky (2003) [28]; Balinsky & Sturman (2006) [29]; Balinsky & Sturman (2006) [30]; USA | Follow-up survey with qualitative interviews; roundtable discussion; home care agencies (n = 8) in Lower Manhattan that were impacted by the 11 September attacks (follow-up: n = 6); roundtable discussion: the 8 home care agencies as well as representatives from government, academia, and other home care agencies (n = unknown) | 0/5 criteria met; insufficient indication of data sampling, data collection detail, data analysis, and data consistence |
| Daugherty et al. (2012) [34]; USA | Qualitative; semi-structured interviews; administrators (n = 21) of home health and personal care agencies in Georgia and Southern California | 5/5 criteria met; self-selection bias |
| Kirkpatrick & Bryan (2007) [35]; USA | Qualitative; case study approach; retrospective; in-depth interviews; the two top administrative staff of 5 selected home health agency facilities that operate in Orleans Parish (n = 10?) | 2/5 criteria met; insufficient indication of study sampling, data collection detail, and analysis |
| Laditka et al. (2008) [36]; USA | Qualitative; semi-structured interviews; state-level preparedness experts (n = 9), administrators of home health (n = 5), and in-home personal care agencies (n = 16) in South Carolina | 2/5 criteria met; insufficient indication of study sampling, data collection detail, and analysis |
| Wyte-Lake et al. (2017) [37]; USA | Quantitative online survey; programme managers of Veterans Health Administration Home-Based Primary Care (VHA HBPC) programmes across the country (n = 77) | 4/5 criteria met; insufficient indication of non-response analysis |
| Wyte-Lake et al. (2019) [38]; USA | Mixed-methods design; quantitative: online survey of practitioners (n = 64) at 10 sites of (VHA HBPC) programmes in 8 states as a natural cohort from an existing study that used the tool and completed patient questionnaires (n = 754); follow-up survey with practitioners (n = 33) of 2 sites; qualitative: follow-up feedback interviews with programme manager (n = unknown) | 5/5 criteria met; self-selection bias |
| Wyte-Lake et al. (2020) [31]; (Wyte-Lake et al. (2020) [32]; USA | Qualitative (1); mixed-methods design (2); qualitative: semi-structured interviews; clinical staff (n = 34) with key functions of the 9 Veterinary Affairs (VA) HBPC from Texas, Florida, and Puerto Rico (1,2); quantitative: secondary data analysis; timeline of activities of the same 9 sites that use the VA’s Corporate Data Warehouse (CDW) (2) | 2/5 criteria met; insufficient indication of data collection detail, data analysis, and data consistency |
| Zane & Biddinger (2011) [39]; USA | Qualitative; unstructured interviews; home health and hospice agencies (n = 21) and other community service providers (n = 4) from 6 states | 2/5 criteria met; insufficient indication of data collection detail and data analysis |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lessinnes, S.; Köhler, M.; Ewers, M. Evidence of Disaster Planning by Home Care Providers: An Integrative Literature Review. Int. J. Environ. Res. Public Health 2023, 20, 5658. https://doi.org/10.3390/ijerph20095658
Lessinnes S, Köhler M, Ewers M. Evidence of Disaster Planning by Home Care Providers: An Integrative Literature Review. International Journal of Environmental Research and Public Health. 2023; 20(9):5658. https://doi.org/10.3390/ijerph20095658
Chicago/Turabian StyleLessinnes, Sanne, Michael Köhler, and Michael Ewers. 2023. "Evidence of Disaster Planning by Home Care Providers: An Integrative Literature Review" International Journal of Environmental Research and Public Health 20, no. 9: 5658. https://doi.org/10.3390/ijerph20095658
APA StyleLessinnes, S., Köhler, M., & Ewers, M. (2023). Evidence of Disaster Planning by Home Care Providers: An Integrative Literature Review. International Journal of Environmental Research and Public Health, 20(9), 5658. https://doi.org/10.3390/ijerph20095658







