The Impact of the COVID-19 Pandemic on Pediatric Bicycle Injury
Abstract
1. Introduction
2. Materials and Methods
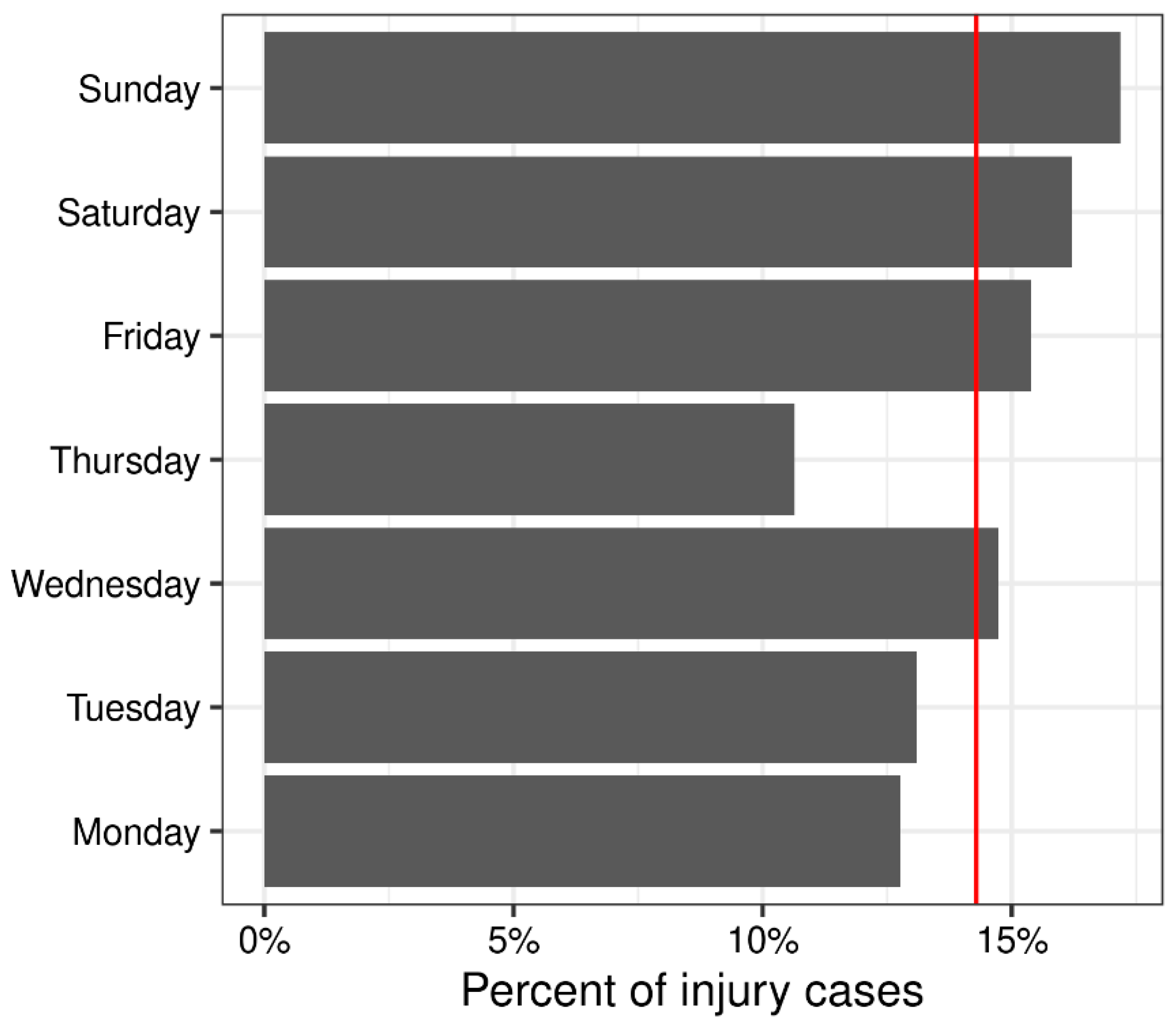
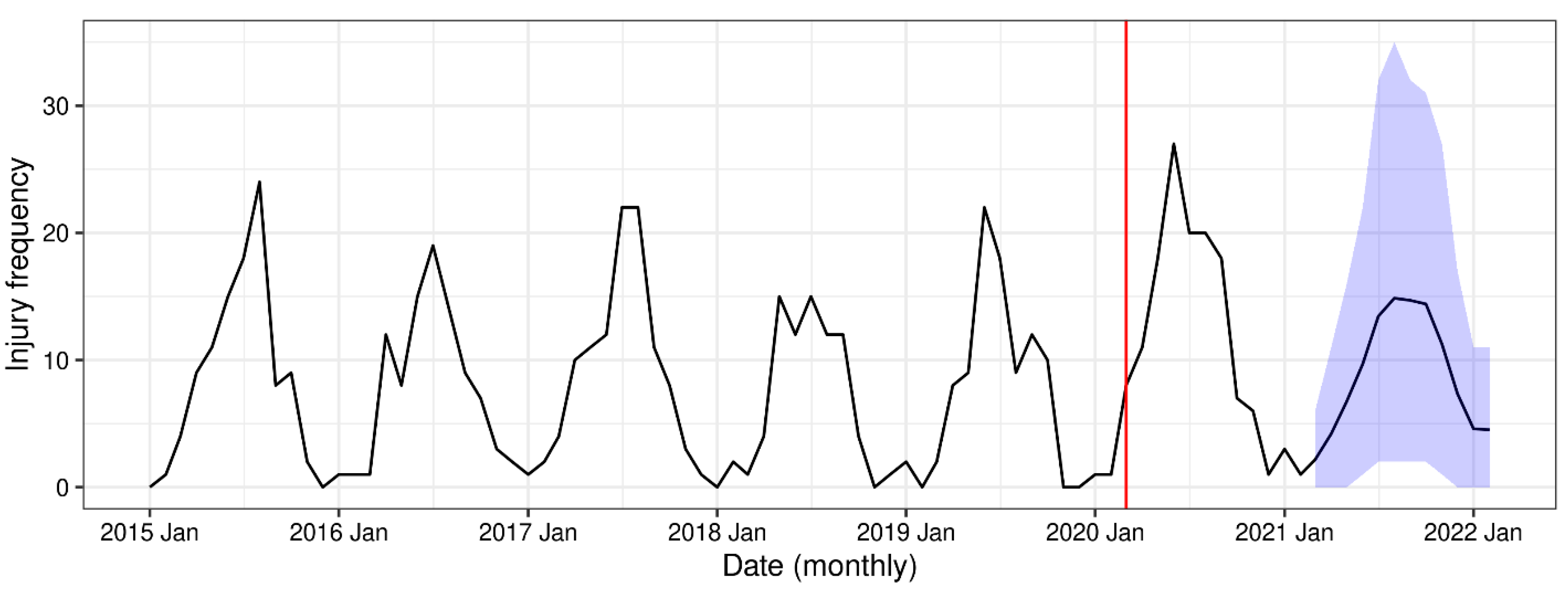
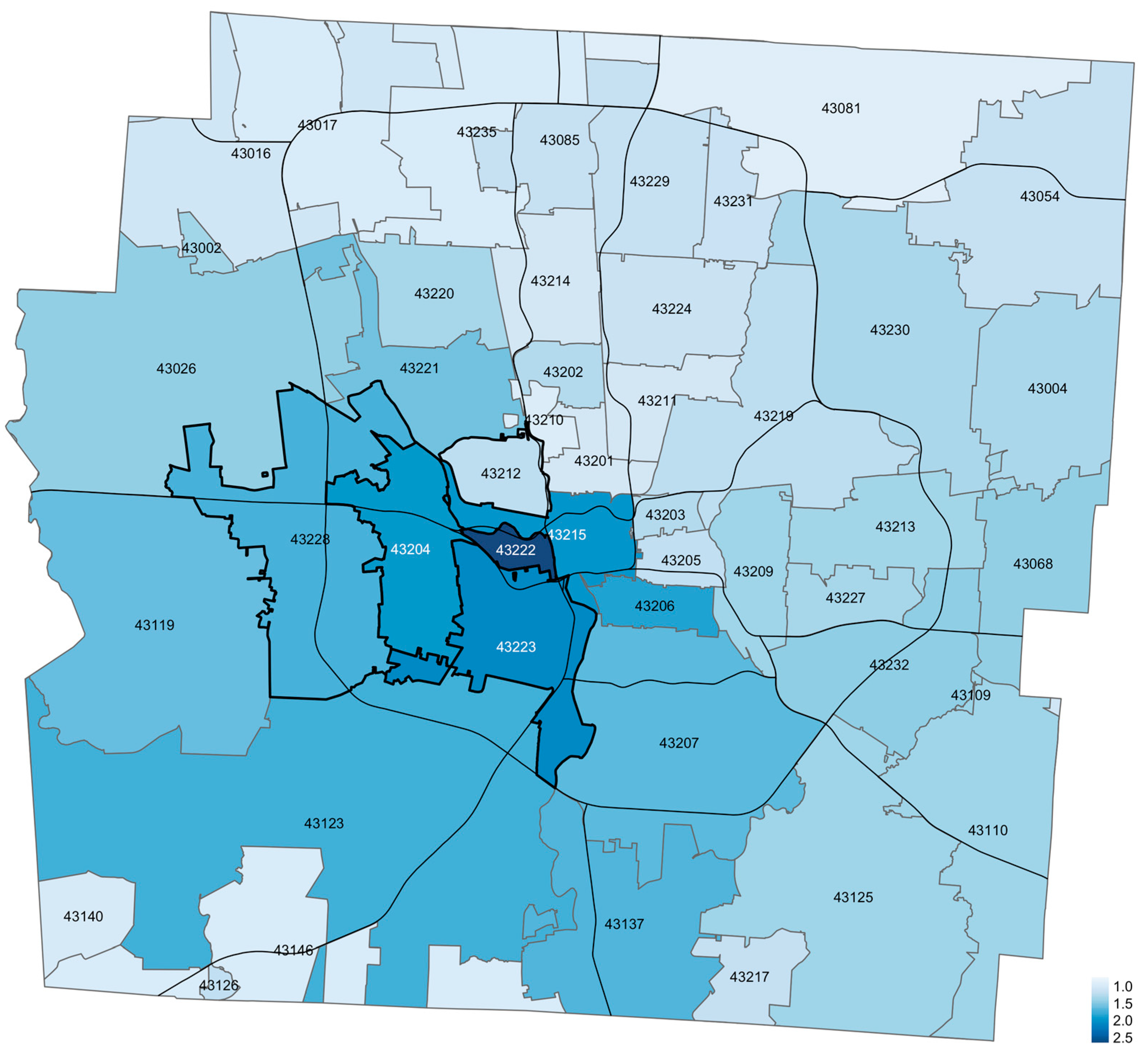
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bogage, J. Fewer Kids Are Riding and Buying Bicycles and the Industry Is Worried. Available online: https://www.washingtonpost.com/sports/2019/06/04/fewer-kids-are-riding-buying-bicycles-industry-is-worried (accessed on 15 March 2022).
- Centers for Disease Control and Prevention. Web-Based Injury Statistics Query and Reporting System (WISQARS). Available online: https://www.cdc.gov/injury/wisqars/ (accessed on 15 March 2022).
- Mehan, T.J.; Gardner, R.; Smith, G.A.; McKenzie, L.B. Bicycle-Related Injuries Among Children and Adolescents in the United States. Clin. Pediatr. 2009, 48, 166–173. [Google Scholar] [CrossRef] [PubMed]
- McAdams, R.J.; Swidarski, K.; Clark, R.M.; Roberts, K.J.; Yang, J.; Mckenzie, L.B. Bicycle-related injuries among children treated in US emergency departments, 2006–2015. Accid. Anal. Prev. 2018, 118, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Høye, A. Bicycle helmets—To wear or not to wear? A meta-analyses of the effects of bicycle helmets on injuries. Accid. Anal. Prev. 2018, 117, 85–97. [Google Scholar] [CrossRef] [PubMed]
- Høye, A.K.; Jensen, M.L.; Sørensen, M.W.J. Are helmeted cyclists taking more risk at signalized intersections? Traffic Inj. Prev. 2020, 21, 552–557. [Google Scholar] [CrossRef]
- Esmaeilikia, M.; Radun, I.; Grzebieta, R.; Olivier, J. Bicycle helmets and risky behaviour: A systematic review. Transp. Res. Part F Traffic Psychol. Behav. 2019, 60, 299–310. [Google Scholar] [CrossRef]
- Walker, I. Drivers overtaking bicyclists: Objective data on the effects of riding position, helmet use, vehicle type and apparent gender. Accid. Anal. Prev. 2007, 39, 417–425. [Google Scholar] [CrossRef]
- Gamble, T.; Walker, I. Wearing a Bicycle Helmet Can Increase Risk Taking and Sensation Seeking in Adults. Psychol. Sci. 2016, 27, 289–294. [Google Scholar] [CrossRef]
- Olivier, J.; Walter, S.R. Bicycle Helmet Wearing Is Not Associated with Close Motor Vehicle Passing: A Re-Analysis of Walker, 2007. PLoS ONE 2013, 8, e75424. [Google Scholar] [CrossRef]
- Lee, L.K.; Flaherty, D.M.R.; Blanchard, A.M.; Agarwal, M. Helmet Use in Preventing Head Injuries in Bicycling, Snow Sports, and Other Recreational Activities and Sports. Pediatrics 2022, 150, e2022058877. [Google Scholar] [CrossRef]
- Yu, C.-Y. Environmental supports for walking/biking and traffic safety: Income and ethnicity disparities. Prev. Med. 2014, 67, 12–16. [Google Scholar] [CrossRef]
- Gilna, G.P.; Stoler, J.; Saberi, R.A.; Baez, A.C.; Ramsey, W.A.; Huerta, C.T.; O’Neil, C.F.; Rattan, R.; Perez, E.A.; Sola, J.E.; et al. Analyzing pediatric bicycle injuries using geo-demographic data. J. Pediatr. Surg. 2022, 57, 915–917. [Google Scholar] [CrossRef] [PubMed]
- Doubleday, A.; Choe, Y.; Miles, S.; Errett, N.A. Daily Bicycle and Pedestrian Activity as an Indicator of Disaster Recovery: A Hurricane Harvey Case Study. Int. J. Environ. Res. Public Health 2019, 16, 2836. [Google Scholar] [CrossRef] [PubMed]
- Rebentisch, H.; Wasfi, R.; Piatkowski, D.P.; Manaugh, K. Safe Streets for All? Analyzing Infrastructural Response to Pedestrian and Cyclist Crashes in New York City, 2009–2018. Transp. Res. Board 2019, 2673, 672–685. [Google Scholar] [CrossRef]
- Bram, J.T.; Johnson, M.A.; Magee, L.C.; Mehta, N.N.; Fazal, F.Z.; Baldwin, K.D.; Riley, J.; Shah, A.S. Where Have All the Fractures Gone? The Epidemiology of Pediatric Fractures During the COVID-19 Pandemic. J. Pediatr. Orthop. 2020, 40, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Keays, G.; Friedman, D.; Gagnon, I. Pediatric injuries in the time of COVID-19. Health Promot. Chronic Dis. Prev. Can. 2020, 40, 336–341. [Google Scholar] [CrossRef]
- Shack, M.; Davis, A.L.; Zhang, E.W.J.; Rosenfield, D. Bicycle injuries presenting to the emergency department during COVID-19 lockdown. J. Paediatr. Child Health 2022, 58, 600–603. [Google Scholar] [CrossRef]
- van Oudtshoorn, S.; Chiu, K.Y.C.; Khosa, J. Beware of the bicycle! An increase in paediatric bicycle related injuries during the COVID-19 period in Western Australia. ANZ J. Surg. 2021, 91, 1154–1158. [Google Scholar] [CrossRef]
- Chiba, H.; Lewis, M.; Benjamin, E.R.; Jakob, D.A.; Liasidis, P.; Wong, M.D.; Navarrete, S.; Carreon, R.; Demetriades, D. “Safer at home”: The effect of the COVID-19 lockdown on epidemiology, resource utilization, and outcomes at a large urban trauma center. J. Trauma Acute Care Surg. 2021, 90, 708–713. [Google Scholar] [CrossRef]
- Abbreviated Injury Scale (AIS)—Overview. Available online: https://www.aaam.org/abbreviated-injury-scale-ais/ (accessed on 15 March 2022).
- Centers for Disease Control and Prevention. CDC Museum COVID-19 Timeline. Available online: https://www.cdc.gov/museum/timeline/covid19.html (accessed on 11 March 2023).
- Liboschik, T.; Fokianos, K.; Fried, R. Tscount: An R Package for Analysis of Count Time Series Following Generalized Linear Models. J. Stat. Softw. 2017, 82, 1–51. [Google Scholar] [CrossRef]
- Liboschik, T.; Kerschke, P.; Fokianos, K.; Fried, R. Modelling interventions in INGARCH processes. Int. J. Comput. Math. 2016, 93, 640–657. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021; Available online: https://www.R-project.org/ (accessed on 15 March 2022).
- Wickham, H.; Averick, M.; Bryan, J.; Chang, W.; McGowan, L.D.A.; François, R.; Grolemund, G.; Hayes, A.; Henry, L.; Hester, J.; et al. Welcome to the Tidyverse. J. Open Source Softw. 2019, 4, 1686. [Google Scholar] [CrossRef]
- Walker, K.; Herman, M. Tidycensus: Load US Census Boundary and Attribute Data as ‘Tidyverse’ and ‘sf’-Ready Data Frames. Available online: https://CRAN.R-project.org/package=tidycensus (accessed on 15 March 2022).
- US Census Bureau 2020: American Community Survey 5-Year Estimates Subject Tables [SAS Data File]. Available online: https://data.census.gov/cedsci/table?g=0500000US39049XX00US43205,43228,43222,43223,43017&tid=ACSST5Y2020.S0101 (accessed on 2 August 2022).
- Anselin, L.; Syabri, I.; Kho, Y. GeoDa: An introduction to spatial data analysis. Geogr. Anal. 2006, 38, 5–22. [Google Scholar] [CrossRef]
- Tennekes, M. Tmap: Thematic Maps in R. J. Stat. Softw. 2018, 84, 1–39. [Google Scholar] [CrossRef]
- Kim, A.Y.; Wakefield, J.; Moise, M. SpatialEpi: Methods and Data for Spatial Epidemiology. Available online: https://CRAN.R-project.org/package=SpatialEpi (accessed on 2 August 2022).
- Kulldorff, M. A spatial scan statistic. Commun. Stat. Theory Methods 1997, 26, 1481–1496. [Google Scholar] [CrossRef]
- Gillory, L.; Cairo, S.; Megison, S.; Vinson, L.; Chung, D.H.; Ryan, M.L. Effect of Quarantine and Reopening Measures on Pediatric Trauma Admissions During the 2019 SARS-CoV2 Virus Pandemic. J. Am. Coll. Surg. 2022, 234, 685–689. [Google Scholar] [CrossRef] [PubMed]
- Dunton, G.F.; Do, B.; Wang, S.D. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health 2020, 20, 1351. [Google Scholar] [CrossRef] [PubMed]
- Hillier, L.M.; Morrongiello, B.A. Age and gender differences in school-age children’s appraisals of injury risk. J. Pediatr. Psychol. 1998, 23, 229–238. [Google Scholar] [CrossRef]
- Teisch, L.F.; Allen, C.J.; Tashiro, J.; Golpanian, S.; Lasko, D.; Namias, N.; Neville, H.L.; Sola, J.E. Injury patterns and outcomes following pediatric bicycle accidents. Pediatr. Surg. Int. 2015, 31, 1021–1025. [Google Scholar] [CrossRef] [PubMed]
- Hamra, G.B.; Schinasi, L.H.; Quistberg, D.A. Motor Vehicle Crashes Involving a Bicycle Before and After Introduction of a Bike Share Program in Philadelphia, Pennsylvania, 2010–2018. Am. J. Public Health 2020, 110, 863–867. [Google Scholar] [CrossRef]
- Kondo, M.C.; Morrison, C.; Guerra, E.; Kaufman, E.J.; Wiebe, D.J. Where do bike lanes work best? A Bayesian spatial model of bicycle lanes and bicycle crashes. Saf. Sci. 2018, 103, 225–233. [Google Scholar] [CrossRef]
- Wheeler-Martin, K.C.; Curry, A.E.; Metzger, K.B.; DiMaggio, C.J. Trends in school-age pedestrian and pedalcyclist crashes in the USA: 26 states, 2000–2014. Inj. Prev. 2020, 26, 448–455. [Google Scholar] [CrossRef] [PubMed]
- US Census Bureau—American Community Survey: Accuracy of the Data. 2019. Available online: https://www2.census.gov/programs-surveys/acs/tech_docs/accuracy/ACS_Accuracy_of_Data_20.pdf (accessed on 15 March 2022).

| Characteristic | Pre-Pandemic, N = 471 1 | Pandemic, N = 140 1 | p-Value 2 |
|---|---|---|---|
| Age (years) | 10.0 (7.0, 12.0) | 10.0 (7.0, 12.0) | 0.8 |
| Sex | 0.035 | ||
| Male | 341 (72%) | 88 (63%) | |
| Female | 130 (28%) | 52 (37%) | |
| Race | 0.4 | ||
| White | 354 (77%) | 108 (77%) | |
| Black | 72 (16%) | 17 (12%) | |
| Asian | 13 (2.8%) | 3 (2.1%) | |
| Hispanic | 13 (2.8%) | 6 (4.3%) | |
| Other | 10 (2.2%) | 6 (4.3%) | |
| (N Missing) | 9 | 0 | |
| Injury location | 0.7 | ||
| Home Residence | 71 (19%) | 21 (21%) | |
| Street/Parking lot/Driveway | 253 (69%) | 70 (69%) | |
| Recreational/Sports area | 26 (7.1%) | 8 (7.9%) | |
| Other | 17 (4.6%) | 2 (2.0%) | |
| (N Missing) | 104 | 39 | |
| Trauma level | 0.10 | ||
| Level 1 Trauma | 43 (9.1%) | 14 (10%) | |
| Level 2 Trauma | 187 (40%) | 43 (31%) | |
| Level 1 Neuro trauma | 7 (1.5%) | 0 (0%) | |
| No trauma alert activation | 234 (50%) | 83 (59%) | |
| Protective devices | 0.9 | ||
| Helmet worn | 61 (16%) | 19 (15%) | |
| Helmet not worn | 330 (84%) | 111 (85%) | |
| (N Missing) | 80 | 10 | |
| Head injury | 0.2 | ||
| No head injury present | 342 (73%) | 94 (67%) | |
| Head injury present | 129 (27%) | 46 (33%) | |
| AIS | 0.2 | ||
| 1 | 41 (33%) | 10 (23%) | |
| 2 | 36 (29%) | 18 (41%) | |
| 3 | 32 (25%) | 11 (25%) | |
| 4 | 9 (7.1%) | 5 (11%) | |
| 5 | 8 (6.3%) | 0 (0%) | |
| (N Missing) | 345 | 96 | |
| ISS | 4.0 (1.0, 6.0) | 4.0 (3.5, 8.2) | 0.066 |
| (N Missing) | 7 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Failing, G.R.L.; Klamer, B.G.; Gorham, T.J.; Groner, J.I. The Impact of the COVID-19 Pandemic on Pediatric Bicycle Injury. Int. J. Environ. Res. Public Health 2023, 20, 5515. https://doi.org/10.3390/ijerph20085515
Failing GRL, Klamer BG, Gorham TJ, Groner JI. The Impact of the COVID-19 Pandemic on Pediatric Bicycle Injury. International Journal of Environmental Research and Public Health. 2023; 20(8):5515. https://doi.org/10.3390/ijerph20085515
Chicago/Turabian StyleFailing, Gates R. L., Brett G. Klamer, Tyler J. Gorham, and Jonathan I. Groner. 2023. "The Impact of the COVID-19 Pandemic on Pediatric Bicycle Injury" International Journal of Environmental Research and Public Health 20, no. 8: 5515. https://doi.org/10.3390/ijerph20085515
APA StyleFailing, G. R. L., Klamer, B. G., Gorham, T. J., & Groner, J. I. (2023). The Impact of the COVID-19 Pandemic on Pediatric Bicycle Injury. International Journal of Environmental Research and Public Health, 20(8), 5515. https://doi.org/10.3390/ijerph20085515







