Abstract
Background: Africa is unlikely to end hunger and all forms of malnutrition by 2030 due to public health problems such as the double burden of malnutrition (DBM). Thus, the aim of this study is to determine the prevalence of DBM and degree of socio-economic inequality in double burden of malnutrition among children under 5 years in sub-Saharan Africa. Methods: This study used multi-country data collected by the Demographic and Health Surveys (DHS) Program. Data for this analysis were drawn from the DHS women’s questionnaire focusing on children under 5 years. The outcome variable for this study was the double burden of malnutrition (DBM). This variable was computed from four indicators: stunting, wasting, underweight and overweight. Inequalities in DBM among children under 5 years were measured using concentration indices (CI). Results: The total number of children included in this analysis was 55,285. DBM was highest in Burundi (26.74%) and lowest in Senegal (8.80%). The computed adjusted Erreygers Concentration Indices showed pro-poor socio-economic child health inequalities relative to the double burden of malnutrition. The DBM pro-poor inequalities were most intense in Zimbabwe (−0.0294) and least intense in Burundi (−0.2206). Conclusions: This study has shown that across SSA, among under-five children, the poor suffer more from the DBM relative to the wealthy. If we are not to leave any child behind, we must address these socio-economic inequalities in sub-Saharan Africa.
1. Introduction
According to the World Food Programme (WFP), malnutrition is “a state in which the physical function of an individual is impaired to the point where he or she can no longer maintain adequate bodily performance process such as growth, pregnancy, lactation, physical work and resisting and recovering from disease” [1]. Malnutrition can also be termed as an abuse of food or bad nutrition, such as over-nutrition and under-nutrition. Hunger and protein-energy malnutrition (PEM) have led to high mortality rates in children and mothers, contributing to poor growth and a rise in opportunistic infections and comprised brain development [2]. On the other hand, overweight and obesity develop because of over-nutrition and have led to an increase in major chronic diseases, which can be life-threatening sometimes. Additionally, micronutrient deficiency has also become rampant in children, which is the major cause of the slow development in children at their developmental stage [3]. The most common micronutrient deficiencies clinically shown to have affected over two billion children under under-five include iron, calcium, zinc, and vitamin A [4]. In the past, many fortification programs have been implemented, drastically improving the situation; however, some developing countries still suffer a significant rate of morbidity [5]. Malnutrition presents a significant threat to humans and has been a public health problem that has resulted in about 45% of childhood deaths [6].
Stunting has been cited to be related to poverty and poor diet [7]. In China, while the prevalence of undernutrition among children has reduced [8], a worrisome new trend is emerging: the co-existence of under-nutrition and over-nutrition [9], and the rising prevalence of overweight and obesity especially in urban areas and affluent rural areas [10]. Despite experiencing economic growth in recent times, India still reports high rates of child malnutrition with 35%, 33% and 17% of children under 5 years being stunted, underweight and wasted, respectively [11]. As of 2019, the number of malnourished people was reported to be around 27% and 29% of the total population for Eastern and Middle sub-regions of Sub-Saharan Africa [12]. These rates were projected to grow, with Sub-Saharan Africa unlikely to achieve the Sustainable Development Goals of ending hunger and all forms of malnutrition by 2030 [12]. The Food and Agriculture Organization (FAO) reported 161 million children under 5 to be stunted as of 2020 [13]. At the same time, 3.4 million people die each year due to being overweight and obese [14]. Between 2000 and 2017, the number of children under 5 presenting with stunting rose from 50.6 to 58.7 million, and the number of overweight children under 5 rose from 6.6 million in 2000 to 9.7 million in 2017 [15]. In 2020, which happens to be the pandemic year recorded, over 140 million under-five children were stunted, 59 million were wasted, and 85 million were moderately or severely underweight [13]. Today, Africa bears a double burden of undernutrition and over-nutrition [16].
The coexistence of two contrasting extremes on the malnutrition spectrum, such as undernutrition and overweight, is known as the double burden of malnutrition (DBM) [17]. DBM can present at an individual, household, or population level. An individual can present both stature and obesity, or different members within a household could be underweight whilst the other is overweight. Many low-income and middle-income countries (LMICs) grapple with challenges associated with DBM [18]. A 2018 World Health Organization (WHO) series found that DBM poses a significant public health threat, as high levels of undernutrition and overweight are rising in LMIC [19]. Sub-Saharan Africa has been characterized by a high prevalence of undernutrition and increasing obesity, which is a typical example of the double burden of malnutrition [6]. Considering the latter at the current status, there is a high chance that Africa may not achieve Sustainable Development Goal 2 (SDG2) by 2030. There are a lot of factors that may have increased the under-nutrition in Africa than in other continents. One may be improper environmental sanitation, which depicts the growth of micronutrients in the environment [13,20]
The DBM is intricately bound to the socio-economic conditions present in sub-Saharan Africa. Socio-economic factors include occupation, education, income, wealth, and where an individual resides [21]. Inequalities arising from socio-economic factors will exacerbate the major causes of malnutrition in children under 5 [22]. Inadequate nutritional intake, insufficient care and household discriminatory food distribution are some of the causes of malnutrition in LMIC [23]. Nutrition in children is heavily reliant on socio-economic factors [24]. Studies have found that children from higher socio-economic status are more likely to have healthier food habits than those from low socio-economic background who display unhealthier food habits that will contribute to malnutrition and have dietary profiles consistent with nutritional guidelines [12,22,23,24,25,26,27,28,29,30,31,32].
The underlying causes of DBM vary by sub-region in sub-Saharan Africa. For example, one study found that cultural perceptions such as a heavier body size in females may signify wealth, good, stable marital home, and exceptional achievement [33]. However, these perceptions differ across sub-regions as some regions expect women to work hard and have increased physical activity. Another study attributed obesity and increased weight to the rise in consumption of cheap, processed food at the expense of fresh, non-processed foods of subsistence farming [34]. The rise in the commercialization of food production is correlated to the decrease in subsistence farming. This has led to household diets with low nutritional value, high sugar, high fat, and energy-dense food that leads to obesity [35]. This article uses a population-based study on ten African countries (Burundi, Ethiopia, Guinea, Malawi, Mali, Senegal, Sierra Leone, South Africa, Zambia, and Zimbabwe) to understand the socio-economic inequalities in the double burden malnutrition among under-5 children in the continent. Thus, the aim of this study is to determine the prevalence of DBM and degree of socio-economic inequality in double burden of malnutrition among children under 5 years in sub-Saharan Africa.
2. Materials and Methods
2.1. Data Source
This study used multi-country data collected by the Demographic and Health Surveys (DHS) Program. The countries included in this study were: Zimbabwe (2015), Malawi (2015), Burundi (2016), South Africa (2016), Guinea (2018), Mali (2018), Zambia (2018), Sierra Leone (2019), Senegal (2019), and Ethiopia (2019). Data for this analysis were drawn from the DHS women’s questionnaire focusing on children under 5 years (under 60 months). DHS employs a two-stage sampling method. Sample sizes for children under 5 included in our analysis are as follows: Zimbabwe (n = 5253), Malawi (5384), Burundi (6096), South Africa (1460), Guinea (3582), Mali (8908), Zambia (9100), Sierra Leone (4540), Senegal (5682), and Ethiopia (5280). These 10 countries were chosen based on the availability of recent data for secondary analysis.
2.2. Study Variables
2.2.1. Stunting
Children whose height-for-age Z-score was below minus three standard deviations (−3 SD) were considered stunted, and those above minus three standard deviations (−3 SD) were considered not stunted. Stunting was coded as binary variable assigned values of zero and one. Those that were not stunted above −3 SD were coded as “0”, and those that were stunted below −3 SD were coded as “1”.
2.2.2. Wasting
Children whose Z-score was below minus three standard deviations (−3 SD) from the median of the reference population were considered thin (wasted), and those above a Z-score above −3 SD were considered not wasted. Wasting was coded as binary variable assigned values of zero and one. Those that were not wasted above −3 SD were coded as “0” and those that were wasted below −3 SD were coded as “1”.
2.2.3. Underweight
Children whose weight-for-age Z-score was below minus three standard deviations (−3 SD) from the median of the reference population were classified as underweight, and those that were above −3 SD considered not underweight. Underweight was coded as binary variable assigned values of zero and one. Those that were not underweight above −3 SD were coded as “0” and those that were underweight below −3 SD were coded as “1”.
2.2.4. Overweight
Children whose weight-for-height Z-score was more than 2 standard deviations (+2 SD) above the median of the reference population were considered overweight. Overweight was coded as binary variable assigned values of zero and one. Those that were not overweight below +2 SD were coded as “0” and those that were overweight above +2 SD were coded as “1”.
2.2.5. Double Burden of Malnutrition (DBM)
The outcome variable for this study is the double burden of malnutrition (DBM). This variable was computed from 4 indicators: stunting, wasting, underweight and overweight. The first step was calculating the row total of stunted, wasted, and underweight children. Then children who had a row total greater than 1 and were overweight were defined as having experienced a double burden of malnutrition. The outcome variable, double burden of malnutrition (DBM), was then recorded as a binary variable where a value of “1” was assigned if DBM was present, and a value of “0” was given if DBM was absent.
2.2.6. Socio-Economic Status (SES)
Socio-economic status was depicted by the household wealth index, which measures a household’s cumulative standard of living, such as ownership of select assets, type of housing, sanitation services, and type of water access, among others, using Principal Component Analysis (PCA) [32]. The household wealth index is considered a more reliable measure of wealth compared to income and consumption because it reflects a household’s long-term standard of living, and this makes it possible to identify problems particular to the poor members of society, such as unequal access to health care and unequal access to recommended nutrition [33]. For this study, wealth was grouped into 5 quintiles—poorest (Q1), poorer (Q2), middle (Q3), richer (Q4) and richest (Q5).
2.3. Statistical Analysis
Data Analysis
The study analyzed the data using STATA 17.1 statistical software. Univariate and bivariate analyses were performed to describe the sample and patterns of DBM. Inequalities in DBM among children under 5 years were measured using concentration indices (CI). The concentration index approach is a standard measure of assessing health inequalities. The indices and curves investigate whether health inequalities exist in one group. However, they do not estimate the magnitude of health inequalities [36]. This paper used the Erreygers normalized concentration indices [37] to measure the socio-economic inequalities among children in DBM: wasting, stunting, underweight and overweight. Among many of the indices that could have been used, we opted to adopt the Normalized Erreygers Indices as they have been corrected for bound issues; hence, they give more robust standard errors. The concentration index ranges from −1 to +1 and estimates the extent to which a health outcome (DBM) is concentrated among the rich or the poor. A negative concentration index value denotes a health outcome (DBM) concentrated among the poor. In contrast, a positive value implies that a health outcome (DBM) is concentrated among the rich [36]. A concentration index of zero implies that there is no socio-economic-related inequality, and a large absolute value of the concentration index depicts a greater concentration of inequality [36,38].
The concentration index can be computed by making use of the ‘covariance’ as shown below:
where: yi is the health variable;
ŷ is the mean of yi;
Ri is the fractional rank of the ith individual;
COV denotes the covariance.
3. Results
3.1. Demographic Characteristics
After data cleaning, the total number of children included in this analysis was 55,285. Across the 10 countries, the majority of the children resided in the rural areas (Burundi (84.25%), Ethiopia (76.97%), Guinea (71.44%), Malawi (83.67%), Mali (74.15%), Senegal (70.89%), Sierra Leone (70.55%), Zambia (70.47%), and Zimbabwe (63.14)) except for South Africa (48.63) (Table 1). Across all countries, a higher prevalence of DBM was reported in rural areas compared to urban areas (Table 2).

Table 1.
Demographic characteristics by country (N = 55,285).

Table 2.
Estimated prevalence of children who experience DBM by residence status.
3.2. Prevalence of Wasting, Stunting, Underweight and Overweight
The total average prevalence of stunting across the 10 countries was 11.6% (Figure 1A). Of 10 countries, 3 were above the total average: Ethiopia (12.2%), Guinea (13.7%) and Burundi (24.8%), and Burundi had the highest stunting prevalence of (24.8%) (Figure 1A). Zambia had the same stunting prevalence as the total average of 11.6%, while the remaining 6 countries had stunting prevalence below the total average: Malawi (10.5%), Sierra Leone (10.3%), Mali (10%), South Africa (9.9%), Zimbabwe (8.1%) and Senegal, which had the lowest stunting prevalence of 4.8% (Figure 1A).
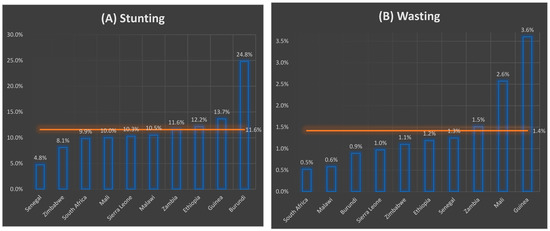

Figure 1.
(A–D) Prevalence of wasting, stunting, underweight and overweight by country.
Meanwhile, for wasting, the prevalence was highest in Guinea (3.6%) and lowest in South Africa (0.5%) (Figure 1B). Zambia (1.5%), Mali (2.6%) and Guinea (3.6%) reported the wasting prevalence values that were higher than the total average of 1.4% (Figure 1B). In contrast, Senegal (1.3%), Ethiopia (1.2%), Zimbabwe (1.1%), Sierra Leone (1.0%), Burundi (0.9%), Malawi (0.6%) and South Africa (0.5%) had wasting prevalence values that were below the total average (Figure 1B). Burundi (8.3%) had the highest underweight prevalence again, while South Africa (1.0%) had the lowest underweight prevalence (Figure 1C). Guinea (5.3%), Mali (5.3%), Ethiopia (5.8%) and Burundi (8.3%) had underweight prevalence values which were above the total average (Figure 1C). Meanwhile, Sierra Leone (3.4%), Senegal (3.0%), Malawi (2.5%), Zambia (2.4%), Zimbabwe (1.4%) and South Africa (1.0%) had underweight prevalence values that were below the total underweight average for the 10 countries (3.8%) (Figure 1C). Additionally, the overweight prevalence was highest in South Africa (13.8%) and lowest in Burundi (1.4%) (Figure 1D). Sierra Leone (5.0%), Zambia (5.4%), Guinea (6.0%), Zimbabwe (6.0%) and South Africa (13.8%) had overweight prevalence values above the overweight total average (4.9%) (Figure 1D).
3.3. Socio-Economic Inequalities
Across all countries, stunting disproportionately affected the poorest, as stunting was more prevalent in the poorest quintile (Q1) (Table 3). The concentration indices for stunting were all negative and statistically significant at a 95% confidence interval in all countries, ranging from −0.21 in Burundi to −0.03 in Zimbabwe (Table 3).

Table 3.
Estimated prevalence of stunting among children by socio-economic status (SES) quintile.
Burundi, Ethiopia, Guinea, Mali, Senegal, Sierra Leone, and Zimbabwe all reported pro-poor wasting child health inequalities (Table 4). The latter concentration indices were statistically significant at a 95% confidence interval. While Malawi, South Africa and Zambia reported pro-rich inequalities, the concentration indices were not statistically significant at a 95% confidence interval (Table 4).

Table 4.
Estimated prevalence of wasting among children by socio-economic status (SES) quintile.
Underweight children were also more prevalent in the poorest quintile (Q1) for most of the countries except for Zimbabwe (31.43%; Q2) and South Africa (35.71; Q3): Burundi (38.84%), Ethiopia (51.52%), Guinea (30.69%), Malawi (34.11%), Mali (28.94%), Senegal (52.50%), Sierra Leone (33.33%), and Zambia (38.57%) (Table 5). All the underweight concentration indices were statistically significant at a 95% confidence interval across countries except for South Africa which had pro-rich inequalities; otherwise, all other countries reported negative indices, indicating pro-poor underweight inequalities (Table 5).

Table 5.
Estimated prevalence of underweight among children by socio-economic status (SES) quintile.
Conversely, overweight disproportionately affected children from the rich households in many of the countries (Burundi, Ethiopia, Malawi, Mali, Senegal, Sierra Leone, Zambia and Zimbabwe); however, only Burundi, Mali, Senegal and Zimbabwe had statistically significant concentration indices at a 95% confidence interval (Table 6). While Guinea and South Africa reported pro-poor inequalities, the concentration indices were not statistically significant at a 95% confidence interval (Table 6).

Table 6.
Estimated prevalence of overweight among children by socio-economic status (SES) quintile.
DBM was highest in Burundi (27.4%), followed by Guinea (21.5%), Zambia (16.7%), Ethiopia (16.6%), South Africa (15.5%), Malawi (15.2%), Sierra Leone (14.3%), Mali (14.1%), Zimbabwe (13.6%) and lowest in Senegal (8.6%) (Figure 2). Across all countries, DBM was most prevalent among children in the poorest quintile (Q1) except in Zimbabwe, where DBM was most prevalent among children from the richer quintile (Q4) (Table 7). However, the adjusted Erreygers concentration indices were negative, showing pro-poor DBM inequalities among children across all countries (Table 7).
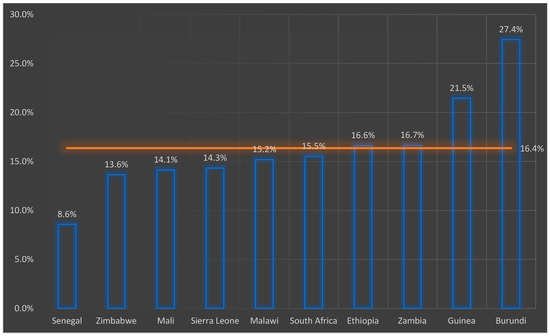
Figure 2.
Double burden of malnutrition by country.

Table 7.
Estimated prevalence of DBM among children by socio-economic status (SES) quintile.
DBM across all countries reported pro-poor inequalities as all the concentration indices were negative and statistically significant at a 95% confidence interval (Table 8). The computed adjusted Erreygers Concentration Indices showed pro-poor socio-economic child health inequalities relative to the double burden of malnutrition. All the concentration indices were negative across all countries and were statistically significant at a 95% confidence interval (Table 8). The DBM pro-poor inequalities were more intense in Zimbabwe (−0.0294) and least intense in Burundi (−0.2206) (Table 8). Meanwhile, between Zimbabwe and Burundi, the intensity of the child health pro-poor inequalities was as follows: Sierra Leone (−0.0356), Zambia (−0.0460), Malawi (−0.0536), Senegal (−0.0597), South Africa (−0.0652), Mali (−0.0689), Guinea (−0.0765) and Ethiopia (−0.1161) (Table 8).

Table 8.
Erreygers Normalized Concentration Indices for DBM by country.
4. Discussion
SDG Target 2.2 aims to “End all forms of malnutrition, including achieving, by 2020, the internationally agreed targets on stunting and wasting in children under 5 years of age”. In this regard, our study contributes several ways to the debate on DBM among children in African countries. First, our results provide evidence on individual nutritional status (underweight, wasting, stunting, and overweight) prevalence of children under 5 years of age at the national level and explain the existence of socio-economic inequalities. The quality of evidence for our approach is supported by representative DHS data from 10 African countries. The completeness of the dataset for analysis, as this study has drawn insights from the most recent dataset from 2015 to 2019, suggests that the geographic and social differences in DBM of under-five children in Africa and the extent of economic inequality can be fully understood.
Sub-Saharan Africa has been cited to be characterized by the double burden of malnutrition (DBM) and high levels of undernutrition as well as a growing burden of overweight/obesity and diet-related non-communicable diseases (NCDs) [39]. Recent research shows that despite a high prevalence of hunger and malnutrition, overweight and obesity epidemics are increasing in Africa [40]. This is still the case, as our study findings showed a significantly high prevalence of DBM, with Senegal reporting the least DBM prevalence of about 9%. In comparison, Burundi had the highest DBM prevalence of about 27%. A recent study raised a concern, citing the possibility that most countries will not meet the global nutrition targets by 2030 [39] and Africa is unlikely to reach the Sustainable Development Goals and end hunger and all forms of malnutrition by 2030. The current study findings seem to show the concern raised in earlier papers becoming a sad reality as this study reported a significantly high prevalence of stunting (Burundi; 24%), underweight (Burundi; 8%) and overweight (South Africa; 13%). Earlier research reported malnutrition commonly observed in developed and affluent communities, but as early as 1996, it was noticed in low-to-middle-income countries (LMICs) [41,42,43].
A recent study reported the prevalence of overweight and obesity among under-five children in South Africa to be almost double that of Malawi [44]. Our results also showed similar findings: South Africa had the highest overweight prevalence of 13% compared to Senegal, which had about 2%. However, it had the 5th highest DBM prevalence of 16%, with Burundi with the highest DBM prevalence of 27%. The reported that the high DBM prevalence of Burundi could be attributed to earlier trends of stunting and underweight among children, which have shown little to no changes since the 1980s [43].
Contrary to what was observed in previous studies that reported relatively socio-economic well-off groups at a greater risk for the double burden of malnutrition [44,45,46], our study showed that DBM was more prevalent among the children from the poorest households (Q1). This may be because of a shift in NCDs’ epidemiology, as they were earlier perceived as diseases for developed countries but are currently more prevalent in developing countries. Furthermore, a DBM is a global problem. It has been argued that it occurs when the prevalence of overweight and obesity in LMICs is increasing rapidly, while at the same time, the prevalence of malnutrition in these countries is declining slowly [47]. This was true for our study, as Burundi had the highest prevalence of stunting (24%) and underweight (8%). As a result, it had the highest DBM prevalence (27%).
Obesity in children under 5 years of age is still overlooked in the current literature. Our study provided evidence of the increasing burden of obesity in this age group, which was found primarily in households of high socio-economic status. Previous studies reported similar findings arguing that wealthier groups pose strong risk factors for the double burden of malnutrition as well as community-level poverty [48,49,50]. Considering that findings from this study showed that DBM is intertwined in underweight, stunting, wasting and overweight, addressing the social inequalities that share the double burden of child malnutrition in the African region therefore requires strategies that address why certain sub-populations are more exposed to these nutritional problems to avoid strategies that solve one nutritional problem and exacerbate another.
There is a need to increase the engagement of various stakeholders to mitigate the double burden of malnutrition in sub-Saharan Africa. The active collaboration and participation of representatives from local and international non-governmental organizations, major corporations, and government institutions across various sectors such as agriculture, finance, environment, education, communications, health care and nutrition will possibly stimulate dialogues around this menace and proffer solutions and recommendations. Furthermore, progress toward ending hunger and malnutrition by 2030 requires intensified efforts to reduce undernutrition and focused action on reducing obesity and diet-related non-communicable diseases. Key strengths of this study lie in it being a compilation of representative and generalizable DHS datasets from 10 countries. These are typically high-quality, highly responsive datasets from DHS surveys conducted using robust methodologies using well-documented data sources. These DHS surveys are conducted using standardized survey modules and implementations that allow comparisons between countries. However, these are cross-cutting datasets, which limited our ability to assign causality.
5. Conclusions
In summary, there is a shift in nutrition in Africa, with the increasing prevalence of overweight and obesity among children under five, making optimal child nutrition a key factor in achieving global health goals. The inequality of DBM was consistently pro-poor socio-economic across the ten SSA countries, such that the lower socio-economic groups were more likely to be experiencing DBM and bear a higher burden of the problem than the higher socio-economic groups. In addition, DBM was pro-poor although some of the nutritional indicators were pro-rich. Therefore, the double burden of malnutrition in low- and middle-income countries poses a major global public health problem that could hinder the achievement of the SDGs if not properly addressed. Furthermore, this study has shown the existence of pro-poor inequalities relative to the double burden of malnutrition among under-five children. Therefore, if we are not to leave any child behind, we must address these socio-economic inequalities in sub-Saharan Africa.
Author Contributions
O.A.A. and A.T.L. designed the study, wrote the paper, analyzed data, reviewed the paper, and submitted it for publication. K.N. and E.N. wrote the background section and reviewed all drafts in preparation for publication, D.O. wrote the methods section and reviewed all drafts in preparation for publication, A.S. wrote the discussion section and reviewed all drafts in preparation for publication. P.C. and O.A.S. wrote the paper and reviewed all drafts in preparation for publication. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding; however, the International Journal of Environmental Research and Public Health (IJERPH) supported the study as they waived the APC charges for processing this manuscript.
Institutional Review Board Statement
This study used secondary analysis based on publicly available DHS datasets. Since the data used in this study were secondary, no ethics approval was sought.
Informed Consent Statement
The parent study DHS surveys sort the consent from the participants.
Data Availability Statement
All data sets are publicly available on the Demographic Health Survey website at: https://dhsprogram.com/what-we-do/survey/survey-display-406.cfm (accessed on 10 January 2023) and can be accessed upon request from the Demographic Health Survey team.
Acknowledgments
We sincerely thank the University of Cape Town Health Economics Unit for its unwavering support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Food Programme. Food and Nutrition Handbook; World Food Programme: Rome, Italy, 2015. [Google Scholar]
- Ekholuenetale, M.; Tudeme, G.; Onikan, A.; Ekholuenetale, C.E. Socioeconomic Inequalities in Hidden Hunger, Undernutrition, and Overweight among under-Five Children in 35 Sub-Saharan Africa Countries. J. Egypt. Public Health Assoc. 2020, 95, 9. [Google Scholar] [CrossRef] [PubMed]
- Benton, D.; Be, I.E. aisbl+ 32-2/762-0044 publications@ ilsieurope. Micronutrient Status, Cognition and Behavioral Problems in Childhood. Eur. J. Nutr. 2008, 47, 38–50. [Google Scholar] [CrossRef] [PubMed]
- Black, R. Micronutrient deficiency: An underlying cause of morbidity and mortality. Bull. World Health Organ. 2003, 81, 79. [Google Scholar] [PubMed]
- World Health Organization. New Global Alliance Brings Food Fortification to World’s Poor; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R. Maternal and Child Undernutrition and Overweight in Low-Income and Middle-Income Countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Siddiqui, F.; Salam, R.A.; Lassi, Z.S.; Das, J.K. The Intertwined Relationship between Malnutrition and Poverty. Front. Public Health 2020, 8, 453. [Google Scholar] [CrossRef]
- Chen, C.; He, W.; Wang, Y.; Deng, L.; Jia, F. Nutritional Status of Children during and Post-Global Economic Crisis in China. Biomed. Environ. Sci. 2011, 24, 321–328. [Google Scholar]
- Pei, L.; Ren, L.; Yan, H. A Survey of Undernutrition in Children under Three Years of Age in Rural Western China. BMC Public Health 2014, 14, 121. [Google Scholar] [CrossRef]
- Zong, X.-N.; Li, H. Physical Growth of Children and Adolescents in China over the Past 35 Years. Bull. World Health Organ. 2014, 92, 555–564. [Google Scholar] [CrossRef]
- Jiang, Y.; Su, X.; Wang, C.; Zhang, L.; Zhang, X.; Wang, L.; Cui, Y. Prevalence and Risk Factors for Stunting and Severe Stunting among Children under Three Years Old in Mid-western Rural Areas of C Hina. Child Care Health Dev. 2015, 41, 45–51. [Google Scholar] [CrossRef]
- Giancola, A.; Hauerslev, M.; Ndinda, C.; Farmer, M.; Musah, L.; Msengi, G.; Bhutta, Z. Addressing the Double-Burden of Malnutrition among Children and Adolescents in Sub-Saharan Africa. J. Glob. Health Rep. 2022, 6, e2022033. [Google Scholar] [CrossRef]
- FAO; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World, (SOFI); World Health Organization: Geneva, Switzerland; WFP: Rome, Italy, 2020; p. 2340. [Google Scholar]
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 10 January 2023).
- UNICEF. Joint Child Malnutrition Estimates—2018 Edition; UNICEF-WHO-The World Bank: New York, NY, USA, 2018. [Google Scholar]
- Mbogori, T.; Kimmel, K.; Zhang, M.; Kandiah, J.; Wang, Y. Nutrition Transition and Double Burden of Malnutrition in Africa: A Case Study of Four Selected Countries with Different Social Economic Development. AIMS Public Health 2020, 7, 425. [Google Scholar] [CrossRef]
- Popkin, B.M.; Corvalan, C.; Grummer-Strawn, L.M. Dynamics of the Double Burden of Malnutrition and the Changing Nutrition Reality. Lancet 2020, 395, 65–74. [Google Scholar] [CrossRef]
- Winichagoon, P.; Margetts, B.M. The Double Burden of Malnutrition in Low-and Middle-Income Countries. Energy Balance Obes. 2017, 1, 6–8. [Google Scholar]
- World Health Organization. The Double Burden of Malnutrition: Priority Actions on Ending Childhood Obesity; Regional Office for South-East Asia: New Delhi, India, 2020. [Google Scholar]
- World Health Organization. The State of Food Security and Nutrition in the World 2020: Transforming Food Systems for Affordable Healthy Diets; Food & Agriculture Org: Rome, Italy, 2020. [Google Scholar]
- Darin-Mattsson, A.; Fors, S.; Kåreholt, I. Different Indicators of Socioeconomic Status and Their Relative Importance as Determinants of Health in Old Age. Int. J. Equity Health 2017, 16, 173. [Google Scholar] [CrossRef]
- Singh, S.; Srivastava, S.; Upadhyay, A.K. Socio-Economic Inequality in Malnutrition among Children in India: An Analysis of 640 Districts from National Family Health Survey (2015–2016). Int. J. Equity Health 2019, 18, 203. [Google Scholar] [CrossRef]
- Bhutta, Z.A.; Berkley, J.A.; Bandsma, R.H.J.; Kerac, M.; Trehan, I.; Briend, A. Severe Childhood Malnutrition. Nat. Rev. Dis. Prim. 2017, 3, 17067. [Google Scholar] [CrossRef]
- Galgamuwa, L.S.; Iddawela, D.; Dharmaratne, S.D.; Galgamuwa, G.L.S. Nutritional Status and Correlated Socio-Economic Factors among Preschool and School Children in Plantation Communities, Sri Lanka. BMC Public Health 2017, 17, 377. [Google Scholar] [CrossRef]
- Darmon, N.; Drewnowski, A. Does Social Class Predict Diet Quality? Am. J. Clin. Nutr. 2008, 87, 1107–1117. [Google Scholar] [CrossRef]
- Casari, S.; di Paola, M.; Banci, E.; Diallo, S.; Scarallo, L.; Renzo, S.; Gori, A.; Renzi, S.; Paci, M.; de Mast, Q. Changing Dietary Habits: The Impact of Urbanization and Rising Socio-Economic Status in Families from Burkina Faso in Sub-Saharan Africa. Nutrients 2022, 14, 1782. [Google Scholar] [CrossRef]
- UNICEF. The State of The World’s Children 2019-Growing Well in a Changing World; UNICEF: New York, NY, USA, 2019. [Google Scholar]
- Faber, M.; Wenhold, F. Nutrition in Contemporary South Africa. Water SA 2007, 33, 393–400. [Google Scholar] [CrossRef]
- French, S.A.; Tangney, C.C.; Crane, M.M.; Wang, Y.; Appelhans, B.M. Nutrition Quality of Food Purchases Varies by Household Income: The SHoPPER Study. BMC Public Health 2019, 19, 231. [Google Scholar] [CrossRef] [PubMed]
- Alkerwi, A.; Vernier, C.; Sauvageot, N.; Crichton, G.E.; Elias, M.F. Demographic and Socioeconomic Disparity in Nutrition: Application of a Novel Correlated Component Regression Approach. BMJ Open 2015, 5, e006814. [Google Scholar] [CrossRef] [PubMed]
- Scaglioni, S.; de Cosmi, V.; Ciappolino, V.; Parazzini, F.; Brambilla, P.; Agostoni, C. Factors Influencing Children’s Eating Behaviours. Nutrients 2018, 10, 706. [Google Scholar] [CrossRef] [PubMed]
- Lytle, L.A. Examining the Etiology of Childhood Obesity: The IDEA Study. Am. J. Community Psychol. 2009, 44, 338–349. [Google Scholar] [CrossRef]
- Onyango, A.W.; Jean-Baptiste, J.; Samburu, B.; Mahlangu, T.L.M. Regional Overview on the Double Burden of Malnutrition and Examples of Program and Policy Responses: African Region. Ann. Nutr. Metab. 2019, 75, 127–130. [Google Scholar] [CrossRef]
- Reardon, T.; Tschirley, D.; Liverpool-Tasie, L.S.O.; Awokuse, T.; Fanzo, J.; Minten, B.; Vos, R.; Dolislager, M.; Sauer, C.; Dhar, R. The Processed Food Revolution in African Food Systems and the Double Burden of Malnutrition. Glob. Food Sec. 2021, 28, 100466. [Google Scholar] [CrossRef]
- Popkin, B.M.; Adair, L.S.; Ng, S.W. NOW AND THEN: The Global Nutrition Transition: The Pandemic of Obesity in Developing Countries. Nutrients 2017, 58, 1–10. [Google Scholar]
- Kakwani, N.; Wagstaff, A.; van Doorslaer, E. Socioeconomic Inequalities in Health: Measurement, Computation, and Statistical Inference. J. Econom. 1997, 77, 87–103. [Google Scholar] [CrossRef]
- Erreygers, G. Correcting the Concentration Index. J. Health Econ. 2009, 28, 504–515. [Google Scholar] [CrossRef]
- Bilger, M.; Sajaia, Z.; Lokshin, M. Health Equity and Financial Protection: Streamlined Analysis with ADePT Software; World Bank Publications: Washington, DC, USA, 2011. [Google Scholar]
- Tzioumis, E.; Kay, M.C.; Bentley, M.E.; Adair, L.S. Prevalence and Trends in the Childhood Dual Burden of Malnutrition in Low-and Middle-Income Countries, 1990–2012. Public Health Nutr. 2016, 19, 1375–1388. [Google Scholar] [CrossRef]
- Kimani-Murage, E.W. Exploring the Paradox: Double Burden of Malnutrition in Rural South Africa. Glob. Health Action 2013, 6, 19249. [Google Scholar] [CrossRef]
- Popkin, B.M.; Richards, M.K.; Montiero, C.A. Stunting Is Associated with Overweight in Children of Four Nations that Are Undergoing the Nutrition Transition. J. Nutr. 1996, 126, 3009–3016. [Google Scholar] [CrossRef]
- Tzioumis, E.; Adair, L.S. Childhood Dual Burden of Under-and Overnutrition in Low-and Middle-Income Countries: A Critical Review. Food Nutr. Bull. 2014, 35, 230–243. [Google Scholar] [CrossRef]
- Ministry of Health Burundi. Nutritional Status Stunting Disparities Demographics and Background Information Infant and Young Child Feeding Under-Five Mortality Rate Deaths per 1000 Live Births; Ministry of Health Burundi: Burundi, South Africa, 2012. [Google Scholar]
- Oddo, V.M.; Rah, J.H.; Semba, R.D.; Sun, K.; Akhter, N.; Sari, M.; de Pee, S.; Moench-Pfanner, R.; Bloem, M.; Kraemer, K. Predictors of Maternal and Child Double Burden of Malnutrition in Rural Indonesia and Bangladesh. Am. J. Clin. Nutr. 2012, 95, 951–958. [Google Scholar] [CrossRef]
- Anik, A.I.; Rahman, M.M.; Rahman, M.M.; Tareque, M.I.; Khan, M.N.; Alam, M.M. Double Burden of Malnutrition at Household Level: A Comparative Study among Bangladesh, Nepal, Pakistan, and Myanmar. PLoS ONE 2019, 14, e0221274. [Google Scholar] [CrossRef]
- Leroy, J.L.; Habicht, J.-P.; Gonzalez de Cossio, T.; Ruel, M.T. Maternal Education Mitigates the Negative Effects of Higher Income on the Double Burden of Child Stunting and Maternal Overweight in Rural Mexico. J. Nutr. 2014, 144, 765–770. [Google Scholar] [CrossRef]
- Mushtaq, M.U.; Gull, S.; Abdullah, H.M.; Shahid, U.; Shad, M.A.; Akram, J. Prevalence and Socioeconomic Correlates of Overweight and Obesity among Pakistani Primary School Children. BMC Public Health 2011, 11, 724. [Google Scholar] [CrossRef]
- Ranjani, H.; Mehreen, T.S.; Pradeepa, R.; Anjana, R.M.; Garg, R.; Anand, K.; Mohan, V. Epidemiology of Childhood Overweight & Obesity in India: A Systematic Review. Indian J. Med. Res. 2016, 143, 160. [Google Scholar]
- Gupta, N.; Goel, K.; Shah, P.; Misra, A. Childhood Obesity in Developing Countries: Epidemiology, Determinants, and Prevention. Endocr. Rev. 2012, 33, 48–70. [Google Scholar] [CrossRef]
- Hemmingsson, E. Early Childhood Obesity Risk Factors: Socioeconomic Adversity, Family Dysfunction, Offspring Distress, and Junk Food Self-Medication. Curr. Obes. Rep. 2018, 7, 204–209. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).