Adherence to Pre-Exposure Prophylaxis (PrEP) among Men Who Have Sex with Men (MSM) in Portuguese-Speaking Countries
Abstract
1. Introduction
2. Materials and Methods
2.1. Type of Study
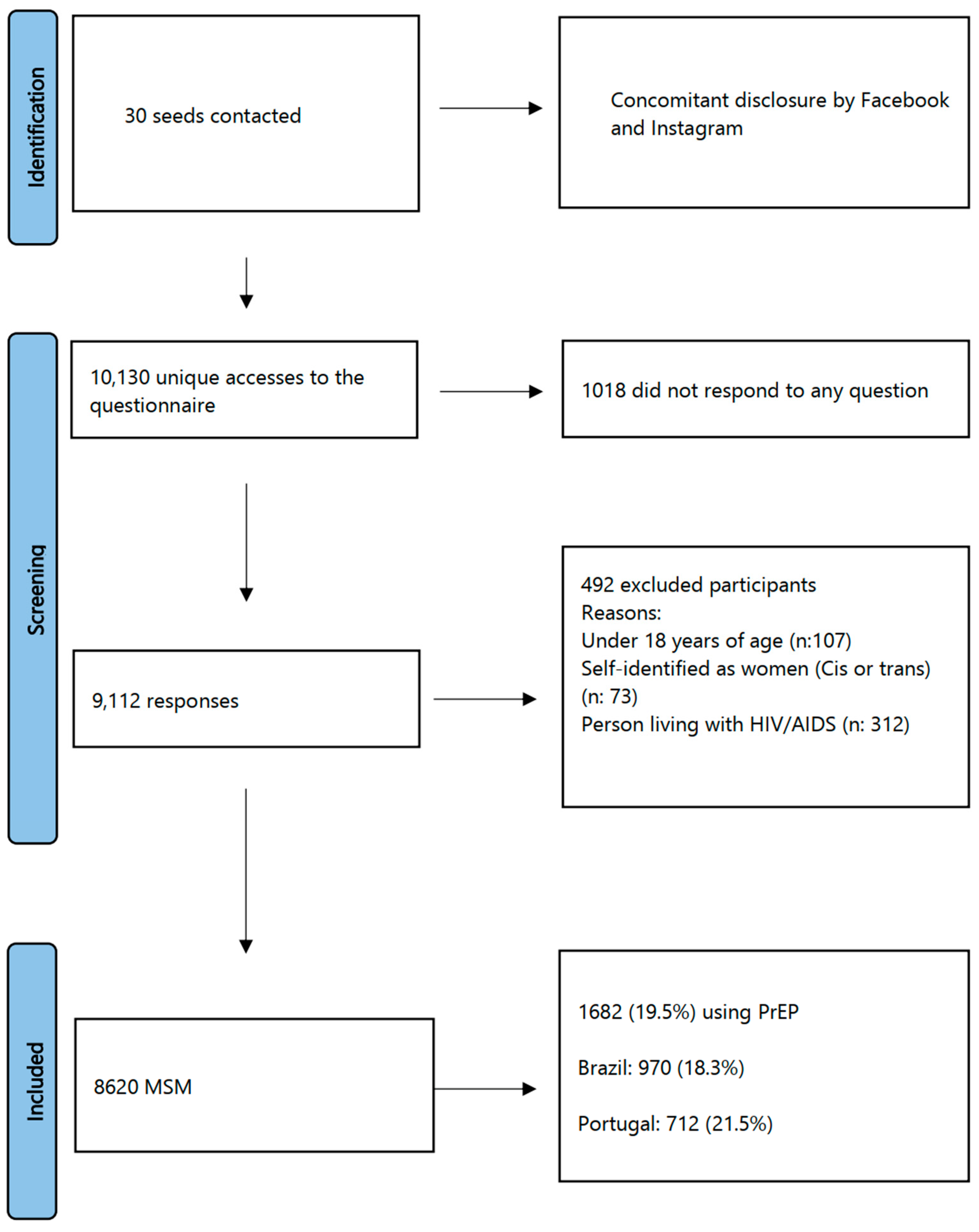
2.2. Population, Sample and Eligibility Criteria
2.3. Data Collection Procedures
2.4. Data Collection Instruments
2.5. Outcomes
- Chemsex: consumption of a drug immediately before and/or during sexual intercourse that is capable of altering the subjects’ perception and causing negligence in the use of protective measures against HIV [45]. In our study, we considered the following drugs alone or in combination: gamma-hydroxybutyric acid or “Gisele”, alkyl nitrites or “poppers”, and methamphetamine or mephedrone in the past 6 months.
- Fisting or footing: anal penetration using the fist or foot.
- Double penetration (DP): simultaneous sexual penetration by two or more penises.
- Cruising: free, consensual and anonymous sex practiced between men in public spaces, such as parks, bushes, beaches or parking lots.
- Challenging sexual practice: adherence to the recurrent use of two or three of these practices, defined according to the circumstances in which they take place.
2.6. Data Analysis
2.7. Ethical Considerations
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Queiroz, A.A.F.L.N.; Sousa, A.F.L. PrEP Forum: An on-line debate on pre-exposure prophylaxis in Brazil. Cad. Saude Publica 2017, 33, e00112516. [Google Scholar] [CrossRef]
- Fonner, V.A.; Dalglish, S.L.; Kennedy, C.E.; Baggaley, R.; O’Reilly, K.R.; Koechlin, F.M.; Rodolph, M.; Hodges-Mameletzis, I.; Grant, R.M. Effectiveness and safety of oral HIV preexposure prophylaxis for all populations. AIDS 2016, 30, 1973–1983. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline on When to Start Antiretroviral Therapy and on Pre-Exposure Prophylaxis for HIV; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Molina, J.M.; Capitant, C.; Spire, B.; Pialoux, G.; Cotte, L.; Charreau, I.; Tremblay, C.; Le Gall, J.M.; Cua, E.; Pasquet, A.; et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 Infection. N. Engl. J. Med. 2015, 373, 2237–2246. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration. FDA Approves First Injectable Treatment for HIV Pre-Exposure Prevention. 2021. Available online: https://www.fda.gov/news-events/press-announcements/fda-approves-first-injectable-treatment-hiv-pre-exposure-prevention (accessed on 10 February 2022).
- Blair, K.J.; Torres, T.S.; Hoagland, B.; Bezerra, D.R.B.; Veloso, V.G.; Grinsztejn, B.; Clark, J.; Luz, P.M. Pre-exposure prophylaxis use, HIV knowledge, and internalized homonegativity among men who have sex with men in Brazil: A cross-sectional study. Lancet Reg. Health Am. 2022, 6, 100152. [Google Scholar] [CrossRef]
- World Health Organization. Global PrEP Network. 2021. Available online: https://www.who.int/groups/global-prep-network/global-state-of-prep#:~:text=There%20were%20about%20940%20000,in%202018%20(370%20000) (accessed on 10 October 2022).
- Kerzner, M.; De, A.K.; Yee, R.; Keating, R.; Djomand, G.; Stash, S.; Rana, S.; Kimmel, A.; Eakle, R.; Klucking, S.; et al. PEPFAR HIV Pre-exposure Prophylaxis Collaborators. Pre-exposure prophylaxis (PrEP) uptake and service delivery adaptations during the first wave of the COVID-19 pandemic in 21 PEPFAR-funded countries. PLoS ONE 2022, 17, e0266280. [Google Scholar] [CrossRef] [PubMed]
- Viera, A.; Berg, J.J.; Sosnowy, C.D.; Mehta, N.A.; Edelman, E.J.; Kershaw, T.; Chan, P.A. Barriers and facilitators to HIV pre-exposure prophylaxis uptake among men who have sex with men who use stimulants: A qualitative study. AIDS Behav. 2022, 26, 3016–3028. [Google Scholar] [CrossRef]
- Golub, S.A.; Gamarel, K.E.; Rendina, H.J.; Surace, A.; Lelutiu-Weinberger, C.L. From efficacy to effectiveness: Facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in New York City. AIDS Patient Care STDs 2013, 27, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Brooks, R.A.; Kaplan, R.L.; Lieber, E.; Landovitz, R.J.; Lee, S.-J.; Leibowitz, A.A. Motivators, concerns, and barriers to adoption of preexposure prophylaxis for HIV prevention among gay and bisexual men in HIV-serodiscordant male relationships. AIDS Care 2011, 23, 1136–1145. [Google Scholar] [CrossRef]
- Liu, A.; Cohen, S.; Follansbee, S.; Cohan, D.; Weber, S.; Sachdev, D.; Buchbinder, S. Early experiences implementing pre-exposure prophylaxis (PrEP) for HIV prevention in San Francisco. PLoS Med. 2014, 11, e1001613. [Google Scholar] [CrossRef] [PubMed]
- Holt, M.; Lea, T.; Murphy, D.; Ellard, J.; Rosengarten, M.; Kippax, S.; Wit, J.D. Willingness to use HIV pre-exposure prophylaxis has declined among australian gay and bisexual men: Results from repeated national surveys, 2011–2013. J. Acquir. Immune Defic. Syndr. 2014, 67, 222–226. [Google Scholar] [CrossRef]
- Qu, D.; Zhong, X.; Xiao, G.; Dai, J.; Liang, H.; Huang, A. Adherence to pre-exposure prophylaxis among men who have sex with men: A prospective cohort study. Int. J. Infect. Dis. 2018, 75, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Mannheimer, S.; Hirsch-Moverman, Y.; Franks, J.; Loquere, A.; Hughes, J.P.; Li, M.; Amico, K.R.; Grant, R.M. Factors Associated with Sex-Related Pre-exposure Prophylaxis Adherence among Men Who Have Sex with Men in New York City in HPTN 067. J. Acquir. Immune Defic. Syndr. 2019, 80, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Cáceres, C.F.; O’Reilly, K.R.; Mayer, K.H.; Baggaley, R. PrEP implementation: Moving from trials to policy and practice. J. Int. AIDS Soc. 2015, 18, 20222. [Google Scholar] [CrossRef]
- Spinelli, M.A.; Scott, H.M.; Vittinghoff, E.; Liu, A.Y.; Morehead-Gee, A.; Gonzalez, R.; Buchbinder, S.P. Provider Adherence to Pre-exposure Prophylaxis Monitoring Guidelines in a Large Primary Care Network. Open Forum Infect. Dis. 2018, 5, ofy099. [Google Scholar] [CrossRef]
- Irungu, E.M.; Baeten, J.M. PrEP rollout in Africa: Status and opportunity. Nat. Med. 2020, 26, 655–664. [Google Scholar] [CrossRef]
- Demartini, Z.B.F. 27 Brazil: Immigration in Brazil: The Insertion of Different Groups. In Immigration Worldwide: Policies, Practices, and Trends; Segal, U.A., Elliott, D., Mayadas, N.S., Eds.; Oxford University Press: New York, NY, USA, 2009; pp. 409–424. [Google Scholar]
- Bäckström, B. Migrants and Health in Portugal. Health Cult. Soc. 2014, 7, 80–93. [Google Scholar] [CrossRef]
- Newitt, M. (Ed.) The Portuguese in Brazil. In Emigration and the Sea: An Alternative History of Portugal and the Portuguese; Oxford University Press: New York, NY, USA, 2015; pp. 107–128. [Google Scholar]
- Casquilho-Martins, I.; Ferreira, S. Migrants’ Health Policies and Access to Health Care in Portugal within the European Framework. Societies 2022, 12, 55. [Google Scholar] [CrossRef]
- UNAIDS: Focus in Brazil. 2019. Available online: https://www.unaids.org/en/20191011_country_focus_Brazil (accessed on 8 March 2020).
- Amoo, E.O.; Solanke, B.L.; Amoo, A.I.; Onipede, W.; Osadolor, U.E. Descriptive analysis of men’s sexual behaviour in sub-Saharan Africa: Simplicity-parsimony approach. Cogent Arts Humanit. 2020, 7, 1796227. [Google Scholar] [CrossRef]
- UNAIDS. Countries: Portugal. Available online: https://www.unaids.org/en/regionscountries/countries/portugal (accessed on 8 March 2020).
- Ministério da Saúde. Instituto Nacional de Saúde Doutor Ricardo Jorge, IP, e outro Infeção VIH e SIDA: A situação em Portugal a 31 de dezembro de 2019. Instituto Nacional de Saúde Doutor Ricardo Jorge. Lisboa: INSA IP, 2020.-80. Available online: https://www.insa.min-saude.pt/wp-content/uploads/2019/11/RelatVIHSIDA2019.pdf (accessed on 8 March 2020).
- UNAIDS. Portugal: Putting People at the Centre of the AIDS Response. 2017. Available online: https://www.unaids.org/en/resources/presscentre/featurestories/2017/may/checkpointlx (accessed on 10 October 2022).
- Galea, J.T.; Baruch, R.; Brown, B. ¡PrEP Ya! Latin America wants PrEP, and Brazil leads the way. Lancet HIV 2018, 5, e110–e112. [Google Scholar] [CrossRef]
- UNAIDS: Use of Pre-Exposure Prophylaxis (PrEP) Is Growing, but Not Fast Enough. 2022. Available online: https://unaids.org.br/2022/01/o-uso-de-prep-cresce-mas-nao-rapido-o-suficiente/ (accessed on 8 March 2020).
- Brasil. Ministério da Saúde. Relatório de Monitoramento de Profilaxias do HIV—PrEP e PEP|2021 Brasília: Ministério da Saúde, 2022. 41 p.: Il. Available online: https://www.gov.br/aids/pt-br/centrais-de-conteudo/publicacoes/2022/relatorio-de-profilaxias-prep-e-pep-2021.pdf (accessed on 10 October 2022).
- Augusto, G.F.; Hodges-Mameletzis, I.; Karanikolos, M.; Abrantes, A.; Martins, M.R.O. HIV prevention and treatment in Southern Europe in the aftermath of bailout programmes. Eur. J. Public Health 2020, 30, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, R.L.A.; Cordeiro, J.F.C.; Bim, L.L.; Gomide, E.B.G.; Andrade, D.; Santos, A.P. Adherence to the Pre-Exposure Prophylaxis to the HIV: How are we doing it in Brazil? Rev. Prevenção Infecção Saúde 2017, 7, 10778. [Google Scholar] [CrossRef]
- Ribeiro, L.; Pinho, A.A.; Carneiro, R.L. Narrative review of studies on HIV pre-exposure prophylaxis in Brazil and its implementation in the public health network. Glob. Public Health 2022, 17, 3721–3734. [Google Scholar] [CrossRef] [PubMed]
- Simões, D.; Meireles, P.; Rocha, M.; Freitas, R.; Aguiar, A.; Barros, H. Knowledge and Use of PEP and PrEP Among Key Populations Tested in Community Centers in Portugal. Front. Public Health 2021, 9, 673959. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, F.; Meireles, P.; Rocha, M.; Rojas, J.; Barros, H. PrEP users among Lisbon MSM Cohort participants—A first look after PrEP implementation in Portugal. Eur. J. Public Health 2019, 29, ckz185-355. [Google Scholar] [CrossRef]
- Pyra, M.N.; Haberer, J.E.; Hasen, N.; Reed, J.; Mugo, N.R.; Baeten, J.M. Global implementation of PrEP for HIV prevention: Setting expectations for impact. J. Int. AIDS Soc. 2019, 22, e25370. [Google Scholar] [CrossRef]
- Portaria Nº 232, de 7 de Fevereiro de 2022. Aprova os Novos Valores da Transferência Fundo a Fundo do Incentivo às Ações de Vigilância, Prevenção e Controle das IST, Aids e Hepatites Virais, do Bloco de Manutenção das Ações e Serviços Públicos de Saúde, do Grupo de Vigilância em Saúde e dá Outras Providências. Diário Oficial da União 2022. Available online: http://antigo.aids.gov.br/pt-br/legislacao/portaria-gmms-no-232-de-7-de-fevereiro-de-2022 (accessed on 8 March 2020).
- Lemos, M.G. Potenciais Candidatos a Profilaxia Pré-Exposição (PrEP): Reflexões de uma Equipa de Intervenção Psiquiátrica num Serviço de Doenças Infeciosas. Acta Médica Port. 2022, 35, 313–331. [Google Scholar] [CrossRef]
- ECDC. Pre-Exposure Prophylaxis for HIV Prevention in Europe and Central Asia. European Centre for Disease Prevention and Control: Stockholm, 2022. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/DD_PrEP_brief_May-2022-final.pdf (accessed on 8 March 2020).
- Queiroz, A.A.F.L.N.; Matos, M.C.B.; Araújo, T.M.E.; Reis, R.K.; Sousa, A.F.L. Sexually transmitted infections and factors associated with condom use in dating app users in Brazil. Acta Paul. Enferm. 2019, 32, 546–553. [Google Scholar] [CrossRef]
- Queiroz, A.A.F.L.N.; Sousa, A.F.L.; Matos, M.C.B.; Araújo, T.M.E.; Reis, R.K.; Moura, M.E.B. Knowledge about HIV/AIDS and implications of establishing partnerships among Hornet® users. Rev. Bras. Enferm. 2018, 71, 1949–1955. [Google Scholar] [CrossRef] [PubMed]
- Sousa, A.F.L.; Queiroz, A.A.F.L.N.; Lima, S.V.M.A.; Almeida, P.D.; Oliveira, L.B.; Chone, J.S.; Araújo, T.M.E.; Brignol, S.M.S.; Sousa, A.R.; Mendes, I.A.C.; et al. Chemsex practice among men who have sex with men (MSM) during social isolation from COVID-19: Multicentric online survey. Cad. Saude Publica 2020, 36, e00202420. [Google Scholar] [CrossRef]
- Sousa, A.F.L.; Oliveira, L.B.; Queiroz, A.A.F.L.N.; Carvalho, H.E.F.; Schneider, G.; Camargo, E.L.S.; Araújo, T.M.E.; Brignol, S.; Mendes, I.A.C.; Fronteira, I.; et al. Casual Sex among Men Who Have Sex with Men (MSM) during the Period of Sheltering in Place to Prevent the Spread of COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 3266. [Google Scholar] [CrossRef]
- Brazil. Protocolo Clinico e Diretrizes Terapêuticas Para Manejo da Infecção Pelo Hiv em Adultos. Brasilia, 2018. Available online: https://www.gov.br/aids/pt-br/centrais-de-conteudo/pcdts/2013/hiv-aids/pcdt_manejo_adulto_12_2018_web.pdf/view (accessed on 8 March 2020).
- Chone, J.S.; Lima, S.V.M.A.; Fronteira, I.; Mendes, I.A.C.; Shaaban, A.N.; Martins, M.R.O.; Sousa, A.F.L. Factors associated with chemsex in Portugal during the COVID-19 pandemic. Rev. Lat. Am. Enfermagem. 2021, 29, e3474. [Google Scholar] [CrossRef]
- Meireles, P.; Fernandes, F.; Rocha, M.; Plankey, M.; Barros, H. Provision of Preexposure Prophylaxis at the Portuguese National Health Service and Uptake in the Lisbon Cohort of Men Who Have Sex with Men. AIDS Behav. 2021, 25, 1975–1983. [Google Scholar] [CrossRef] [PubMed]
- ECDC. Pre-Exposure Prophylaxis for HIV Prevention in Europe and Central Asia. European Centre for Disease Prevention and Control: Stockholm, 2019. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/HIV-pre-exposure-prophylaxis-evidence-2019.pdf (accessed on 8 March 2020).
- The EMIS Network. EMIS-2017—The European Men-Who-Have-Sex-with-Men Internet Survey. Key Findings from 50,564 Countries. 2019. Available online: https://www.ecdc.europa.eu/en/publications-data/emis-2017-european-men-who-have-sex-meninternet-survey (accessed on 8 March 2020).
- UNAIDS/WHO. HIV Epidemic and Response in Latin America and the Caribbean. 2022. Available online: https://www.paho.org/en/documents/hiv-epidemic-and-response-latin-america-and-caribbean-october-2022 (accessed on 8 March 2020).
- Teixeira, J.R.B.; Lima, S.V.M.A.; Sousa, A.R.; Queiroz, A.A.F.L.N.; Barreto, N.M.P.V.; Mendes, I.A.C.; Fronteira, I.; Sousa, A.F.L. Determinants of sexual exposure to HIV in Portuguese and Brazilian adolescents: A path analysis. Rev. Lat. Am. Enfermagem. 2022, 30, e3715. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, S.; Rocha, M. Pre-Exposure Prophylaxis Counseling in a Community Sexual Health Clinic for Men Who Have Sex with Men in Lisbon, Portugal. Acta Med. Port. 2019, 32, 441–447. [Google Scholar] [CrossRef]
- Kowalska, J.D.; Bursa, D.; Gökengin, D.; Jilich, D.; Vasylyev, M.; Bukovinowa, P.; Mulabdic, V.; Antonyak, S.; Horban, A.; ECEE Network Group. HIV health care providers are ready to introduce pre-exposure prophylaxis in Central and Eastern Europe and neighbouring countries: Data from the Euroguidelines in Central and Eastern Europe (ECEE) Network Group. HIV Med. 2018, 19, 629–633. [Google Scholar] [CrossRef] [PubMed]
- Meireles, P.; Plankey, M.; Rocha, M.; Brito, J.; Mendão, L.; Barros, H. Different guidelines for pre-exposure prophylaxis (PrEP) eligibility estimate HIV risk differently: An incidence study in a cohort of HIV-negative men who have sex with men, Portugal, 2014–2018. Eurosurveillance 2020, 25, 1900636. [Google Scholar] [CrossRef] [PubMed]
- Doblecki-Lewis, S.; Jones, D. Community Federally Qualified Health Centers as Homes for HIV Preexposure Prophylaxis: Perspectives from South Florida. J. Int. Assoc. Provid. AIDS Care 2016, 15, 522–528. [Google Scholar] [CrossRef]
- Decreto-Lei N.º 131/2017, de 10 de Outubro de 2017. Alarga o Elenco de Cuidados de Saúde Dispensados do Pagamento de Taxas Moderadoras No Serviço Nacional de Saúde. Diário da República Eletrónico 2017. Available online: https://dre.pt/dre/detalhe/decreto-lei/131-2017-108280429 (accessed on 10 October 2022).
- Serviço Nacional de Saúde. Profilaxia de Pré-Exposição da Infeção por VIH No Adulto. Available online: https://normas.dgs.min-saude.pt/2017/11/28/profilaxia-de-pre-exposicao-da-infecao-por-vih-no-adulto/ (accessed on 10 October 2022).
- CONITEC. 2021. Available online: http://conitec.gov.br/images/Consultas/Relatorios/2022/20220414_Relatorio_prep_CP_21.pdf (accessed on 8 March 2020).
- Brasil. Nota Informativa Nº 11/2021-CGAHV/.DCCI/ SVS/MS. Available online: http://www.aids.gov.br/pt-br/legislacao/nota-informativa-no-112021-cgahvdccisvsms (accessed on 8 March 2020).
- Sullivan, P.S.; Mena, L.; Elopre, L.; Siegler, A.J. Implementation Strategies to Increase PrEP Uptake in the South. Curr. HIV/AIDS Rep. 2019, 16, 259–269. [Google Scholar] [CrossRef]
- Fleischman, J.; Kachale, F.; Mhuriro, F.; Mugambi, M.; Ncube, G.; Ndwiga, A.; Nyirenda, R.; Carter, A.; Rodrigues, J.; Segal, K. Catalyzing action on HIV/SRH integration: Lessons from Kenya, Malawi, and Zimbabwe to spur investment. Glob. Health Action 2022, 15, 2029335. [Google Scholar] [CrossRef]
| Variables | PrEP Use | ||||
|---|---|---|---|---|---|
| Portugal (n = 712) | Brazil (n = 970) | ||||
| n (%) | PR (95% CI) p-Value | n (%) | PR (95% CI) p-Value | ||
| Social and demographic characteristics | |||||
| Immigrant | Yes | 387 (32.1) | 2.0 (1.8–2.4) <0.001 | 171 (20.7) | 1.2 (1.0–1.3) 0.046 |
| No [ref] | 325 (15.5) | 799 (17.8) | |||
| Age | <35 years old | 517 (21.4) | 1.0 (0.9–1.1) 0.817 | 746 (18.1) | 0.96 (0.84–1.10) 0.570 |
| ≥35 years old [ref] | 195 (21.8) | 224 (18.8) | |||
| Schooling level | Low | 158 (18.4) | 0.8 (0.7–0.9) 0.01 | 292 (21.9) | 1.3 (1.1–1.5) <0.001 |
| Higher Education [ref] | 554 (22.6) | 678 (17.1) | |||
| Attracted to women | Yes | 168 (24.0) | 1.14 (0.98–1.33) 0.073 | 233 (22.8) | 1.32 (1.16–1.51) <0.001 |
| No [ref] | 544 (20.9) | 737 (17.2) | |||
| Type of relationship | Single | 501 (21.6) | 1.32 (1.11–1.58) 0.002 | 734 (19.7) | 2.00 (1.67–2.39) <0.001 |
| Polyamorous | 81 (42.4) | 2.60 (2.07–3.27) <0.001 | 108 (39.6) | 4.03 (3.23–5.02) <0.001 | |
| Steady partner/In a relationship [ref] | 130 (16.3) | - | 128 (9.8) | - | |
| Sexual and affective relationships | |||||
| HIV status | Known [ref] | 616 (21.6) | 1.0 (0.81–1.18) 0.816 | 803 (17.3) | 1.44 (1.24–1.66) <0.001 |
| Unknown | 96 (21.1) | 167 (24.9) | |||
| HIV tests in the last 12 months | Yes | 699 (32.2) | 28.1 (16.3–48.4) <0.001 | 960 (26.6) | 45.2 (24.3–84.2) <0.001 |
| No [ref] | 13 (1.1) | 10 (0.6) | |||
| Number of sex partners in the last 30 days | None [ref] | 3 (0.8) | - | 3 (0.6) | - |
| 1 | 5 (0.5) | 0.7 (0.1–2.7) <0.694 * | 12 (0.6) | 1.0 (0.31–3.86) <1.000 * | |
| ≥2 | 704 (35.5) | 44.2 (14.3–136.6) <0.001 | 955 (32.3) | 54.49 (17.61–168.59) <0.001 | |
| Disclosing serological status in mobile apps | Yes | 429 (53.4) | 4.7 (4.1–5.4) <0.001 | 571 (50.3) | 5.26 (4.71–5.87) <0.001 |
| No [ref] | 283 (11.3) | 399 (9.6) | |||
| Recent sexual practices | |||||
| Sexual intercourse with a person living with HIV | Yes | 7 (10.8) | 2.01 (0.99–4.07) 0.050 | 21 (18.8) | 0.97 (0.65–1.43) 0.893 |
| No [ref] | 705 (21.7) | 949 (18.3) | |||
| Group sex and/or with 3 or more people | Yes | 253 (18.8) | 0.80 (0.70–0.92) 0.002 | 326 (14.7) | 0.70 (0.62–0.80) <0.001 |
| No [ref] | 459 (23.4) | 644 (20.8) | |||
| Gouinage | Yes | 4 (22.2) | 1.03 (0.43–2.45) 0.942 | 6 (26.1) | 1.43 (0.71–2.84) 0.209 |
| No [ref] | 708 (21.5) | 964 (18.2) | |||
| No [ref] | 201 (15.9) | 285 (12.6) | |||
| Chemsex | Yes | 290 (29.5) | 1.62 (1.42–1.84) <0.001 | 368 (24.1) | 1.52 (1.35–1.70) <0.001 |
| No [ref] | 422 (18.2) | 602 (15.9) | |||
| Fisting or footing | Yes | 87 (32.1) | 1.56 (1.29–1.88) <0.001 | 124 (25.1) | 1.43 (1.21–1.68) <0.001 |
| No [ref] | 625 (20.6) | 846 (17.6) | |||
| Cruising | Yes | 208 (79.1) | 4.78 (4.32–5.28) <0.001 | 238 (79.9) | 5.47 (5.00–5.97) <0.001 |
| No [ref] | 504 (16.5) | 732 (14.6) | |||
| Double penetration | Yes | 223 (30.3) | 1.60 (1.39–1.83) <0.001 | 268 (22.4) | 1.31 (1.15–1.48) <0.001 |
| No [ref] | 489 (19.0) | 702 (17.1) | |||
| Challenging sexual practices | Yes | 414 (32.1) | 2.18 (1.91–2.48) <0.001 | 522 (25.3) | 1.83 (1.64–2.06) <0.001 |
| No [ref] | 298 (14.7) | 448 (13.8) | |||
| Consistent condom use | Yes | 65 (22.6) | 1.05 (0.84–1.32) 0.623 | 106 (21.8) | 1.21 (1.01–1.45) 0.033 |
| No [ref] | 647 (21.4) | 864 (17.9) | |||
| Reasons for not using condoms | |||||
| Interrupted practice or coitus | Yes [ref] | 172 (18.6) | 1.21 (1.04–1.41) 0.013 | 234 (15.6) | 1.23 (1.07–1.41) 0.002 |
| No | 540 (22.6) | 736 (19.3) | |||
| Only insertive | Yes | 32 (22.9) | 1.06 (0.78–1.45) 0.691 | 40 (25.0) | 1.38 (1.05–1.82) 0.020 |
| No [ref] | 680 (21.5) | 930 (18.1) | |||
| Partner reported PrEP use | Yes | 105 (34.8) | 1.72 (1.45–2.04) <0.001 | 151 (32.8) | 1.94 (1.67–2.24) <0.001 |
| No [ref] | 607 (20.2) | 819 (16.9) | |||
| New/casual partner | Yes | 540 (22.6) | 1.21 (1.04–1.41) 0.013 | 736 (19.3) | 1.23 (1.07–1.41) 0.002 |
| No [ref] | 172 (18.6) | 234 (15.6) | |||
| Partner stated they did not have an STI | Yes | 66 (19.2) | 0.88 (0.70–1.10) 0.285 | 103 (19.5) | 1.08 (0.90–1.30) 0.420 |
| No [ref] | 646 (21.8) | 867 (18.1) | |||
| Partner reported a recent HIV test | Yes [ref] | 44 (15.7) | 1.40 (1.06–1.85) 0.017 | 76 (16.0) | 1.15 (0.93–1.43) 0.187 |
| No | 668 (22.1) | 894 (18.5) | |||
| Variables | β | aPR | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Portugal: multivariate analysis 1 | |||||
| ≥2 casual sex partners per month | 3.469 | 32.11 | 10.40 | 99.14 | <0.001 |
| Routinely undergoing HIV tests | 2957 | 19.23 | 11.20 | 33.03 | <0.001 |
| Disclosing serological status in apps | 0.741 | 2.02 | 1.88 | 2.34 | <0.001 |
| Being bisexual | 0.393 | 1.48 | 1.33 | 1.64 | <0.001 |
| Being an immigrant | 0.310 | 1.36 | 1.24 | 1.50 | <0.001 |
| Being fond of challenging sexual practices * | 0.253 | 1.29 | 1.16 | 1.43 | <0.001 |
| Knowing the partner’s serological status | 0.248 | 1.28 | 1.06 | 1.56 | 0.012 |
| Frequent bareback sex | 0.146 | 1.16 | 1.02 | 1.30 | 0.018 |
| Brazil: multivariate analysis 2 | |||||
| Routinely undergoing HIV tests | 3.467 | 32.04 | 17.23 | 59.59 | <0.001 |
| ≥2 casual sex partners per month | 3.436 | 31.05 | 9.99 | 96.42 | <0.001 |
| Not knowing the partner’s serological status | 0.806 | 2.24 | 2.03 | 2.47 | <0.001 |
| Disclosing serological status in apps | 0.774 | 2.17 | 1.97 | 2.39 | <0.001 |
| Being in a polyamorous relationship | 0.634 | 1.89 | 1.60 | 2.23 | <0.001 |
| Being single | 0.355 | 1.43 | 1.25 | 1.63 | <0.001 |
| Being fond of casual sex | 0.220 | 1.25 | 1.12 | 1.39 | <0.001 |
| Being fond of challenging sexual practices * | 0.216 | 1.24 | 1.13 | 1.36 | <0.001 |
| Schooling level | 0.126 | 1.14 | 1.03 | 1.26 | 0.014 |
| Frequent bareback sex | 0.120 | 1.13 | 1.01 | 1.25 | 0.027 |
| Group sex | −0.168 | 0.85 | 0.76 | 0.94 | 0.002 |
| Being an immigrant | −0.192 | 0.83 | 0.74 | 0.92 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sousa, A.F.L.d.; Lima, S.V.M.A.; Ribeiro, C.J.N.; de Sousa, A.R.; Barreto, N.M.P.V.; Camargo, E.L.S.; Araújo, A.A.C.; dos Santos, A.D.; Bezerra-Santos, M.; Fortunato, M.d.R.; et al. Adherence to Pre-Exposure Prophylaxis (PrEP) among Men Who Have Sex with Men (MSM) in Portuguese-Speaking Countries. Int. J. Environ. Res. Public Health 2023, 20, 4881. https://doi.org/10.3390/ijerph20064881
Sousa AFLd, Lima SVMA, Ribeiro CJN, de Sousa AR, Barreto NMPV, Camargo ELS, Araújo AAC, dos Santos AD, Bezerra-Santos M, Fortunato MdR, et al. Adherence to Pre-Exposure Prophylaxis (PrEP) among Men Who Have Sex with Men (MSM) in Portuguese-Speaking Countries. International Journal of Environmental Research and Public Health. 2023; 20(6):4881. https://doi.org/10.3390/ijerph20064881
Chicago/Turabian StyleSousa, Alvaro Francisco Lopes de, Shirley Veronica Melo Almeida Lima, Caíque Jordan Nunes Ribeiro, Anderson Reis de Sousa, Nilo Manoel Pereira Vieira Barreto, Emerson Lucas Silva Camargo, Agostinho Antônio Cruz Araújo, Allan Dantas dos Santos, Márcio Bezerra-Santos, Mariana dos Reis Fortunato, and et al. 2023. "Adherence to Pre-Exposure Prophylaxis (PrEP) among Men Who Have Sex with Men (MSM) in Portuguese-Speaking Countries" International Journal of Environmental Research and Public Health 20, no. 6: 4881. https://doi.org/10.3390/ijerph20064881
APA StyleSousa, A. F. L. d., Lima, S. V. M. A., Ribeiro, C. J. N., de Sousa, A. R., Barreto, N. M. P. V., Camargo, E. L. S., Araújo, A. A. C., dos Santos, A. D., Bezerra-Santos, M., Fortunato, M. d. R., Possani, M. A., Santos, A. J. d., Lima, J. L. T. d., Gir, E., Fronteira, I., & Mendes, I. A. C. (2023). Adherence to Pre-Exposure Prophylaxis (PrEP) among Men Who Have Sex with Men (MSM) in Portuguese-Speaking Countries. International Journal of Environmental Research and Public Health, 20(6), 4881. https://doi.org/10.3390/ijerph20064881









