Intensive Rehabilitation Program in Older Adults with Stroke: Therapy Content and Feasibility—Preliminary Results from the BRAIN-CONNECTS Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Setting
2.3. Participants
2.4. Intensive Rehabilitation Program
2.5. Treatment Record
2.6. Study Endpoints
2.7. Statistical Analysis
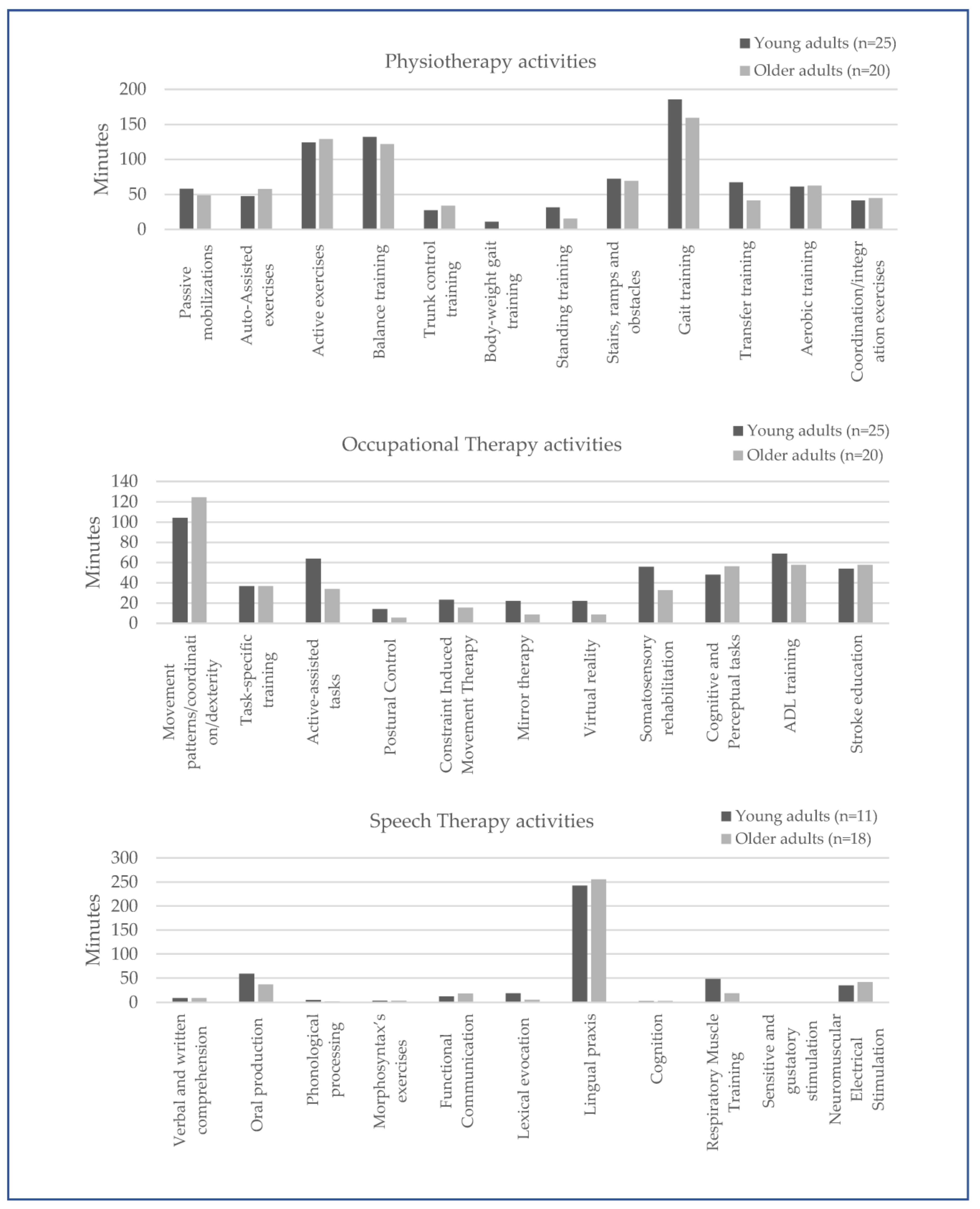
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Feigin, V.L.; Brainin, M.; Norrving, B.; Martins, S.; Sacco, R.L.; Hacke, W.; Fisher, M.; Pandian, J.; Lindsay, P. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. Int. J. Stroke 2022, 17, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Wafa, H.A.; Wolfe, C.D.; Emmett, E.; Roth, G.A.; Johnson, C.O.; Wang, Y. Burden of Stroke in Europe: Thirty-Year Projections of Incidence, Prevalence, Deaths, and Disability-Adjusted Life Years. Stroke 2020, 51, 2418–2427. [Google Scholar] [CrossRef] [PubMed]
- Sartor, M.M.; Grau-Sánchez, J.; Guillén-Solà, A.; Boza, R.; Puig, J.; Stinear, C.; Morgado-Perez, A.; Duarte, E. Intensive rehabilitation programme for patients with subacute stroke in an inpatient rehabilitation facility: Describing a protocol of a prospective cohort study. BMJ Open 2021, 11, e046346. [Google Scholar] [CrossRef] [PubMed]
- Luker, J.A.; Wall, K.; Bernhardt, J.; Edwards, I.; Grimmer-Somers, K.A. Patients’ age as a determinant of care received following acute stroke: A systematic review. BMC Health Serv. Res. 2011, 11, 161. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, D.; Lieberman, D. Rehabilitation following stroke in patients aged 85 and above. J. Rehabil. Res. Dev. 2005, 42, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, H.; Jørgensen, H.S.; Raaschou, H.O.; Olsen, T.S. The influence of age on stroke outcome. The Copenhagen Stroke Study. Stroke 1994, 25, 808–813. [Google Scholar] [CrossRef] [PubMed]
- Winstein, C.J.; Stein, J.; Arena, R.; Bates, B.; Cherney, L.R.; Cramer, S.C.; DeRuyter, F.; Eng, J.J.; Fisher, B.; Harvey, R.L.; et al. Guidelines for Adult Stroke Rehabilitation and Recovery: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2016, 47, e98–e169. [Google Scholar] [CrossRef] [PubMed]
- Summers, D.; Leonard, A.; Wentworth, D.; Saver, J.L.; Simpson, J.; Spilker, J.A.; Hock, N.; Miller, E.; Mitchell, P.H.; American Heart Association Council on Cardiovascular Nursing and the Stroke Council. Comprehensive overview of nursing and interdisciplinary rehabilitation care of the stroke patient: A scientific statement from the American heart association. Stroke 2010, 41, 2402–2448. [Google Scholar] [CrossRef]
- Chan, L.; Sandel, M.E.; Jette, A.M.; Appelman, J.; Brandt, D.E.; Cheng, P.; TeSelle, M.; Delmonico, R.; Terdiman, J.F.; Rasch, E.K. Does postacute care site matter? A longitudinal study assessing functional recovery after a stroke. Arch. Phys. Med. Rehabil. 2013, 94, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Jette, A.M. Opening the Black Box of Rehabilitation Interventions. Phys. Ther. 2020, 100, 883–884. [Google Scholar] [CrossRef] [PubMed]
- DeJong, G.; Horn, S.D.; Conroy, B.; Nichols, D.; Healton, E.B. Opening the black box of post-stroke rehabilitation: Stroke rehabilitation patients, processes, and outcomes. Arch. Phys. Med. Rehabil. 2005, 86 (Suppl. S2), S1–S7. [Google Scholar] [CrossRef] [PubMed]
- Bode, R.K.; Heinemann, A.W.; Semik, P.; Mallinson, T. Patterns of therapy activities across length of stay and impairment levels: Peering inside the "black box" of inpatient stroke rehabilitation. Arch. Phys. Med. Rehabil. 2004, 85, 1901–1908. [Google Scholar] [CrossRef] [PubMed]
- Jette, A.M. Language Matters. Phys. Ther. 2016, 96, 754–755. [Google Scholar] [CrossRef] [PubMed]
- Lang, C.E.; MacDonald, J.R.; Gnip, C. Counting repetitions: An observational study of outpatient therapy for people with hemiparesis post-stroke. J. Neurol. Phys. Ther. 2007, 31, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Veerbeek, J.M.; van Wegen, E.; van Peppen, R.; van der Wees, P.J.; Hendriks, E.; Rietberg, M.; Kwakkel, G. What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PLoS ONE 2014, 4, e87987. [Google Scholar] [CrossRef]
- Abbott, J.H. The distinction between randomized clinical trials (RCTs) and preliminary feasibility and pilot studies: What they are and are not. J. Orthop. Sports Phys. Ther. 2014, 44, 555–558. [Google Scholar] [CrossRef]
- Aguirrezabal, A.; Duarte, E.; Rueda, N.; Cervantes, C.; Marco, E.; Escalada, F. Effects of information and training provision in satisfaction of patients and carers in stroke rehabilitation. NeuroRehabilitation 2013, 33, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Duncan, P.W.; Horner, R.D.; Reker, D.M.; Samsa, G.P.; Hoenig, H.; Hamilton, B.; LaClair, B.J.; Dudley, T.K. Adherence to postacute rehabilitation guidelines is associated with functional recovery in stroke. Stroke 2002, 33, 167–177. [Google Scholar] [CrossRef] [PubMed]
| Rehabilitation Therapies | Activities |
|---|---|
| Physiotherapy | Passive mobilizations of affected extremities. Auto-assisted exercises of affected extremities. Active exercises of affected extremities. Balance training and stepping. Trunk control training. Body weight supported gait training. Standing training—standing frame. Stairs, ramps, and obstacles. Gait training. Transfer training. Aerobic training. Coordination and integration exercises of the affected side. |
| Occupational therapy | Upper limb movement patterns, coordination, and dexterity training. Task-specific training. Active-assisted tasks with upper limb weight support. Postural control and orthosis use for affected upper limb. Constraint Induced Movement Therapy (CIMT). Mirror therapy. Virtual reality for upper limb movement training. Somatosensory rehabilitation. Cognitive and perceptual tasks. Activities of daily life training. Stroke education. |
| Speech therapy | Verbal and written comprehension. Oral production (articulation, volume, tone and prosody). Phonological processing. Morphosyntax exercises. Functional communication. Lexical evocation (free, phonetic phonological, and semantic evocation). Lingual praxis. Cognition (memory, reasoning, logical reasoning, abstraction). Respiratory Muscle Training (Orygen Dual Valve©). Sensitive and gustatory stimulation. Neuromuscular Electrical Stimulation (Vital Stym©). |
| Total Sample (n = 45) | Adults (<65 Years) (n = 25) | Older Adults (≥65 Years) (n = 20) | p | |
|---|---|---|---|---|
| Sex, men (%) | 35 (77.8%) | 21 (84.0%) | 14 (70.0%) | 0.262 |
| Years of schooling, <8 years, n (%) | 22 (38.9%) | 8 (30.0%) | 14 (70.0%) | 0.011 * |
| Dominance, right-handed, n(%) | 44 (97.8%) | 24 (96.0%) | 20 (100%) | 0.556 |
| Smoking history, n (%) | ||||
| Never smoked | 25 (55.6%) | 12 (48%) | 13 (65%) | 0.129 |
| Former smoker | 9 (20.0%) | 4 (16%) | 5 (20%) | |
| Current smoker | 11 (24.4%) | 9 (36%) | 2 (10%) | |
| Alcoholic habits, n (%) | 9 (20.0%) | 6 (24.0%) | 3 (15.0%) | 0.710 |
| SDU/day | 6.0 (SD 5.3) | 5.2 (SD 1.9) | 7.7 (SD 9.9) | 0.705 |
| Comorbidities, n (%) | 37 (82.2%) | 17 (68.0%) | 20 (100%) | 0.005 * |
| Common comorbidities, n (%) | ||||
| Hypertension | 28 (62.2%) | 12 (48.0%) | 16 (80.0%) | 0.035 * |
| Dyslipidemia | 18 (40.0%) | 7 (28.0%) | 11 (55.0%) | 0.066 |
| Diabetes mellitus | 12 (26.7%) | 4 (16.0%) | 8 (40.0%) | 0.096 |
| Obesity (BMI > 30 Kg/m2) | 7 (15.6%) | 3 (12.0%) | 4 (20.0%) | 0.682 |
| Ischemic heart disease/heart failure | 5 (11.1%) | 3 (12.0%) | 2 (10.0%) | 0.608 |
| Atrial fibrillation | 2 (4.4%) | 1 (4.0%) | 1 (5.0%) | 0.697 |
| Sleep apnea | 4 (8.9%) | 1 (4.0%) | 3 (15.0%) | 0.224 |
| Stroke onset (days), mean (SD) | 6.6 (SD 3.5) | 7.1 (SD 3.7) | 6.1 (SD 3.2) | 0.331 |
| Stroke Type, n (%) | ||||
| Ischemic | 37 (82.2%) | 19 (76.0%) | 18 (90.0%) | 0.206 |
| Hemorrhagic | 8 (17.8%) | 6 (24.0%) | 2 (10.0%) | |
| Stroke Hemisphere, n (%) | ||||
| Right | 16 (35.6%) | 8 (32.0%) | 8 (40.0%) | 0.577 |
| Left | 29 (64.4%) | 17 (68.0%) | 12 (60.0%) | |
| Oxford classification, n (%) | ||||
| Total anterior circulation infarction | 9 (20.0%) | 5 (20.0%) | 4 (20.0%) | 0.168 |
| Partial anterior circulation infarction | 11 (24.4%) | 8 (32.0%) | 3 (15.0%) | |
| Posterior circulation infarction | 1 (2.2%) | 0 (0%) | 1 (5.0%) | |
| Lacunar anterior circulation infarction | 15 (33.3%) | 5 (20.0%) | 10 (50.0%) | |
| Unknown data | 9 (20.0%) | 7 (28.0%) | 2 (10.0%) | |
| Stroke Etiology (TOAST classification), n (%) | ||||
| Large-artery atherosclerosis | 5 (11.1%) | 4 (16.0%) | 1 (5.0%) | 0.004 * |
| Cardioembolism | 5 (11.1%) | 0 (0%) | 5 (25.0%) | |
| Lacunar or small vessel disease | 16 (35.6%) | 6 (24.0%) | 10 (50.0%) | |
| Undetermined etiology | 12 (26.7%) | 10 (40.0%) | 2 (11.1%) | |
| Not available in the medical record | 7 (15.6%) | 5 (20.0%) | 2 (10.0%) | |
| Reperfusion therapy, n (%) | 14 (31.1%) | 8 (32.0%) | 6 (30.0%) | 0.885 |
| NIHSS at admission, mean (SD) | 6.1 (SD 2.7) | 6.0 (SD 3.0) | 6.1 (SD 2.5) | 0.859 |
| Modified Rankin Scale at admission, mean (SD) | 3.3 (SD 0.8) | 3.4 (SD 0.8) | 3.3 (SD 0.8) | 0.268 |
| Barthel Index at admission, mean (SD) | 56.9 (SD 17.8) | 58.2 (SD 8.5) | 55.4 (SD 16.9) | 0.609 |
| Total Sample (n = 45) | Adults (<65 Years) (n = 25) | Older Adults (≥65 Years) (n = 20) | p | |
|---|---|---|---|---|
| Length of stay (days), mean (SD) | 16.4 (SD 8.9) | 16.6 (SD 11.1) | 16.2 (SD 5.5) | 0.869 |
| Therapy days (days), mean (SD) | 13.2 (SD 7.4) | 13.5 (SD 9.1) | 12.8 (SD 4.5) | 0.767 |
| Daily time of therapy (minutes), mean (SD) | 173.8 (SD 31.5) | 175.1 (SD 28.4) | 173.1 (SD 28.9) | 0.584 |
| Therapy requirements, n (%) | ||||
| Physiotherapy | 45 (100%) | 25 (100%) | 20 (100%) | - |
| Occupational therapy | 45 (100%) | 25 (100%) | 20 (100%) | - |
| Speech therapy | 29 (64.4%) | 11 (44%) | 18 (90%) | 0.002 * |
| Speech therapy needs, n (%) | ||||
| Aphasia | 5 (17.2%) | 3 (27.3%) | 2 (11.1%) | 0.339 |
| Dysphagia | 19 (65.6%) | 6 (54.5%) | 13 (72.2%) | 0.432 |
| Others | 5 (17.2%) | 2 (18.2%) | 3 (16.7%) | 0.644 |
| Daily time of each therapy (minutes), mean (SD) | ||||
| Physiotherapy | 85.3 (47.7.2%) | 87.7 (46.9%) | 82.3 (48.6%) | 0.512 |
| Occupational therapy | 52.4 (29.3%) | 55.7 (29.7%) | 48.3 (28.4%) | 0.004 * |
| Speech therapy | 40.8 (23.0%) | 43.6 (23.3%) | 39.2 (23.0%) | 0.180 |
| Patients Performing <180 min/Day of Therapy (n = 34) | Patients Performing ≥180 min/Day of Therapy (n = 11) | p | |
|---|---|---|---|
| Age (years), mean (SD) | 62.8 (SD 10.7) | 63.7 (SD 13.3) | 0.820 |
| Sex, women (%) | 10 (100%) | 0 (0%) | 0.041 * |
| Years of schooling, <8 years, n (%) | 16 (72.7%) | 6 (27.3%) | 0.666 |
| Comorbidities, n (%) | 28 (75.7%) | 9 (24.3%) | 0.968 |
| Stroke onset (days), mean (SD) | 6.7 (SD 3.6) | 6.5 (SD 3.3) | 0.857 |
| Stroke type, ischemic (%) | 27 (73.0%) | 10 (27.0%) | 0.657 |
| Stroke hemisphere, right (%) | 23 (78.9%) | 6 (20.1%) | 0.430 |
| Stroke Location (OXFORD classification), n (%) | 0.253 | ||
| Total anterior circulation infarction | 8 (88.9%) | 1 (11.1%) | |
| Partial anterior circulation infarction | 8 (72.7%) | 3 (27.3%) | |
| Posterior circulation infarction | 0 (0.0%) | 1 (100%) | |
| Lacunar anterior circulation infarction | 10 (66.7%) | 5 (33.3%) | |
| Stroke Etiology (TOAST classification), n (%) | |||
| Large-artery atherosclerosis | 1 (68.7%) | 5 (31.3%) | |
| Cardioembolism | 3 (60.0%) | 2 (40.0%) | 0.479 |
| Lacunar or small vessel disease | 5 (100%) | 0 (0%) | |
| Undetermined etiology | 9 (75.0%) | 3 (25.0%) | |
| NIHSS at admission, mean (SD) | 6 (SD 2.7) | 6.3 (SD 2.9) | 0.780 |
| Modified Rankin Scale at admission, mean (SD) | 3.3 (SD 0.8) | 3.5 (SD 0.5) | 0.316 |
| Barthel Index at admission, mean (SD) | 58.8 (SD 18.6) | 51.0 (SD 13.2) | 0.204 |
| Length of stay (days), mean (SD) | 14.2 (SD 6.7) | 23.7 (SD 11.6) | 0.002 * |
| Therapy days (days), mean (SD) | 11.5 (SD 5.6) | 18.6 (SD 9.7) | 0.004 * |
| Total Sample (n = 45) | Adults (<65 Years) (n = 25) | Older Adults (≥65 Years) (n = 20) | p | |
|---|---|---|---|---|
| Tolerability variables | ||||
| Lost to follow-up, n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | - |
| Attendance 1, mean (SD) | 95.8 (SD 5.9) | 95.4 (SD 6.0) | 96.4 (SD 5.9) | 0.632 |
| Reasons for not attending a session, n (%) | ||||
| External medical visits or examinations | 21 (46.6%) | 11 (52.4%) | 10 (47.6%) | 0.697 |
| Clinical events | 3 (6.6%) | 3 (100%) | 0 (0.0%) | 0.083 |
| Need of rest | 4 (8.9%) | 1 (25.0%) | 3 (75.0%) | 0.206 |
| Other reasons | 4 (8.9%) | 3 (75.0%) | 1 (25.0%) | 0.404 |
| Reasons for early termination, n (%) | ||||
| High fatigability | 17 (37.7%) | 9 (53.0%) | 8 (47.0%) | 0.783 |
| Poor participation | 9 (20.0%) | 5 (55.5%) | 4 (44.5%) | 1.000 |
| Other causes | 3 (6.7%) | 1 (33.3%) | 2 (66.7%) | 0.423 |
| Treatment interruption 2, n (%) | 0.317 | |||
| External medical visits or examinations | 5 (11.1%) | 4 (80.0%) | 1 (10.0%) | |
| General discomfort | 1 (2.2%) | 1 (100%) | 0 (0.0%) | |
| Safety variables | ||||
| Adverse events occurring during any sessions | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morgado-Pérez, A.; Coll-Molinos, M.; Valero, R.; Llobet, M.; Rueda, N.; Martínez, A.; Nieto, S.; Ramírez-Fuentes, C.; Sánchez-Rodríguez, D.; Marco, E.; et al. Intensive Rehabilitation Program in Older Adults with Stroke: Therapy Content and Feasibility—Preliminary Results from the BRAIN-CONNECTS Study. Int. J. Environ. Res. Public Health 2023, 20, 4696. https://doi.org/10.3390/ijerph20064696
Morgado-Pérez A, Coll-Molinos M, Valero R, Llobet M, Rueda N, Martínez A, Nieto S, Ramírez-Fuentes C, Sánchez-Rodríguez D, Marco E, et al. Intensive Rehabilitation Program in Older Adults with Stroke: Therapy Content and Feasibility—Preliminary Results from the BRAIN-CONNECTS Study. International Journal of Environmental Research and Public Health. 2023; 20(6):4696. https://doi.org/10.3390/ijerph20064696
Chicago/Turabian StyleMorgado-Pérez, Andrea, Maria Coll-Molinos, Ruben Valero, Miriam Llobet, Nohora Rueda, Andrea Martínez, Sonia Nieto, Cindry Ramírez-Fuentes, Dolores Sánchez-Rodríguez, Ester Marco, and et al. 2023. "Intensive Rehabilitation Program in Older Adults with Stroke: Therapy Content and Feasibility—Preliminary Results from the BRAIN-CONNECTS Study" International Journal of Environmental Research and Public Health 20, no. 6: 4696. https://doi.org/10.3390/ijerph20064696
APA StyleMorgado-Pérez, A., Coll-Molinos, M., Valero, R., Llobet, M., Rueda, N., Martínez, A., Nieto, S., Ramírez-Fuentes, C., Sánchez-Rodríguez, D., Marco, E., Puig, J., & Duarte, E. (2023). Intensive Rehabilitation Program in Older Adults with Stroke: Therapy Content and Feasibility—Preliminary Results from the BRAIN-CONNECTS Study. International Journal of Environmental Research and Public Health, 20(6), 4696. https://doi.org/10.3390/ijerph20064696







