More GP Consultations by Violence Victims: Results from the Representative German DEGS1 Study
Abstract
1. Introduction
2. Materials and Methods
- 1.
- DEGS1 measurements of socio-demographic information
- 2.
- DEGS1 measurements of participants’ GP contacts and health status
- Subjective health status based on the Minimum European Health Module (MEHM): “What is your health status in general?” (Answer options based on a five-point Likert scale were dichotomized: very good/good health vs. middle/poor/very poor health);
- The presence of chronic health problems (i.e., long-standing illness with constant treatment and control, e.g., diabetes or heart diseases);
- The presence of mental health problems, i.e., physician-diagnosed depression ever in life/depression in the last 12 months, and anxiety disorders ever diagnosed in life;
- The presence of (undiagnosed) current depressive symptoms using the 2-item Patient Health Questionnaire (PHQ-2) [44]. This self-report scale included two items addressing disinterest and depressed mood during the past two weeks on a four-point Likert scale (not at all to nearly every day) [45]. Based on the sum score 0–6, subjects were categorized into two subgroups: no depressive symptoms (0–2) and depressive symptoms (3–6);
- Data on substance abuse identified risky health behaviors. The level of alcoholic risky consumption (defined as 10 g of pure alcohol for women or 20 g of pure alcohol for men) had been measured by the Alcohol Use Disorder Identification Test—Consumption [AUDIT-C] [46,47] and was categorized into three groups (never drinking, moderate drinking, risk consumption). Participants´ actual smoking behavior was classified into “(occasional) smoker” and “former/never smoker” [48].
- 3.
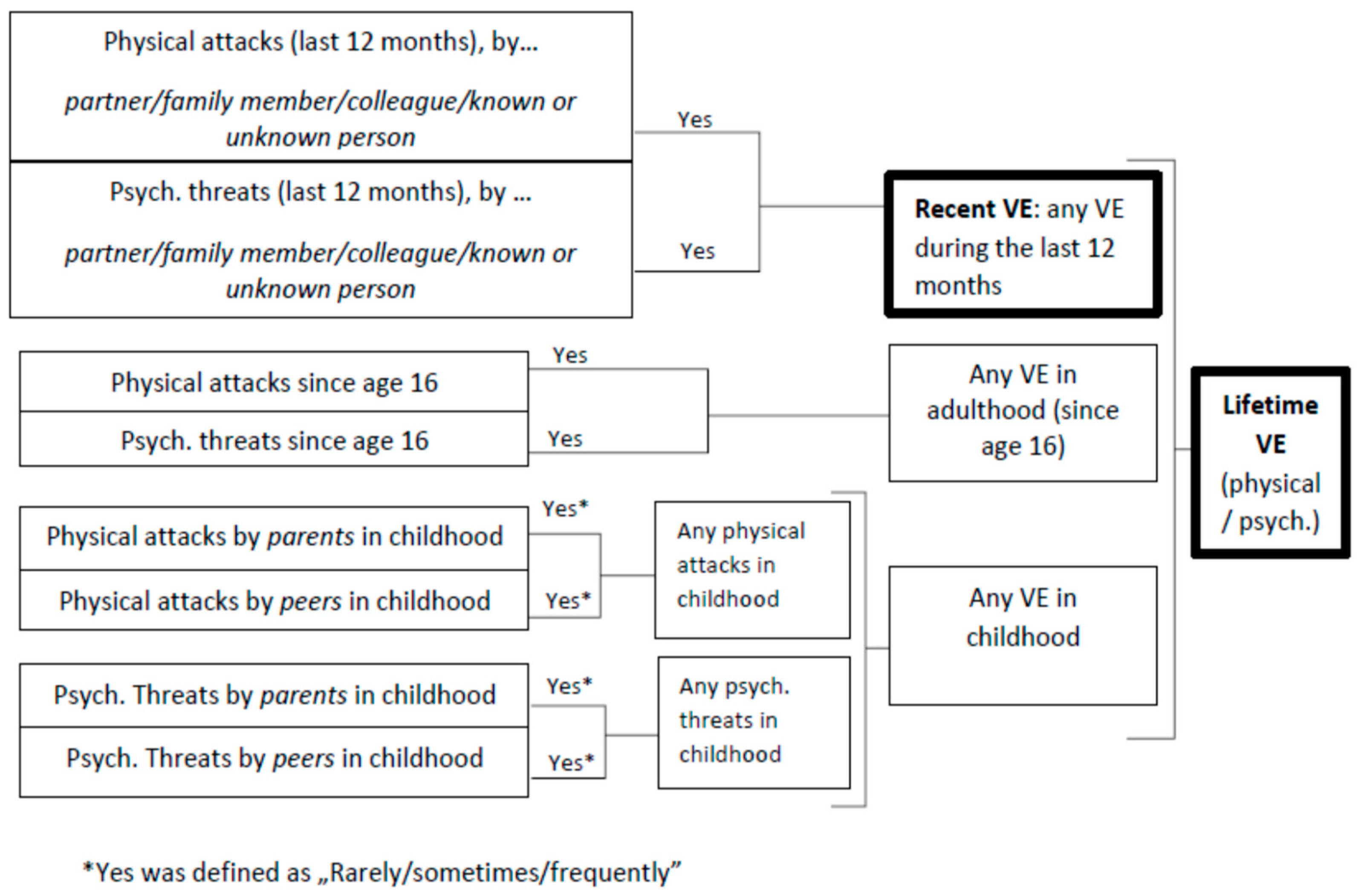
- DEGS1 measurements of self-reported violence
3. Results
3.1. Socio-Demographic Characteristics, Prevalence of VE, and GP Contacts
3.2. Associations between VE and (Mental) Health Problems
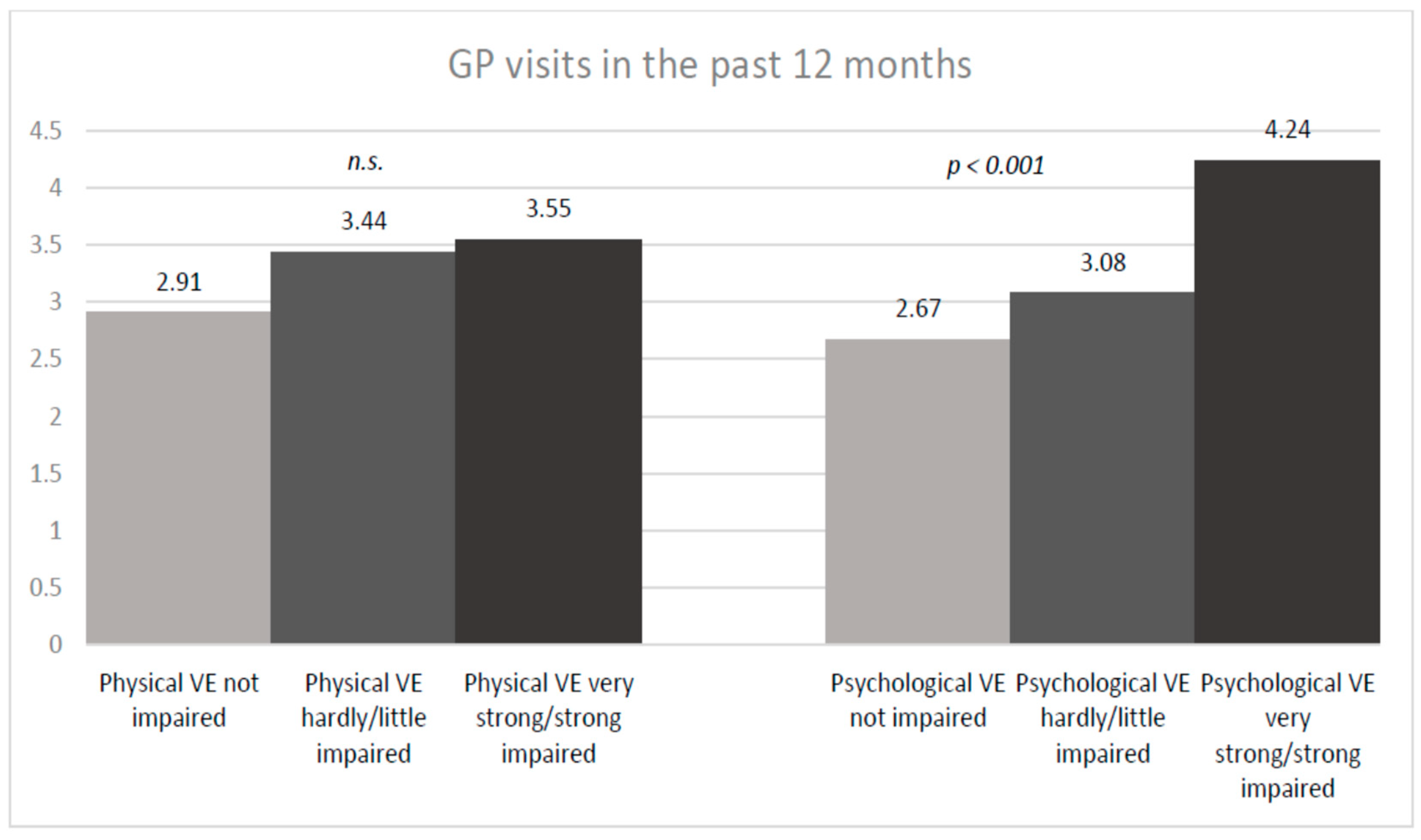
3.3. Associations between VE, Impairment by VE, and GP Contacts
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Campbell, J.C. Health consequences of intimate partner violence. Lancet 2002, 359, 1331–1336. [Google Scholar] [CrossRef]
- Rivara, F.; Adhia, A.; Lyons, V.; Massey, A.; Mills, B.; Morgan, E.; Simckes, M.; Rowhani-Rahbar, A. The Effects of Violence on Health. Health Aff. 2019, 38, 1622–1629. [Google Scholar] [CrossRef]
- Jawad, M.; Vamos, E.P.; Najim, M.; Roberts, B.; Millett, C. Impact of arMed. conflict on cardiovascular disease risk: A systematic review. Heart 2019, 105, 1388–1394. [Google Scholar] [CrossRef] [PubMed]
- Thurston, R.C.; Chang, Y.; Matthews, K.A.; Känel, R.; Koenen, K. Association of Sexual Harassment and Sexual Assault with Midlife Women’s Mental and Physical Health. JAMA Intern. Med. 2019, 179, 48–53. [Google Scholar] [CrossRef]
- Krug, E.G.; Mercy, J.A.; Dahlberg, L.L.; Anthony, B. The world report on violence and health. Lancet 2002, 360, 1083–1088. [Google Scholar] [CrossRef] [PubMed]
- Kalmakis, K.A.; Chandler, G.E. Health consequences of adverse childhood experiences: A systematic review. J. Am. Assoc. Nurse Pract. 2015, 27, 457–465. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.J.; Alonso, A.; Everson-Rose, S.A.; Spencer, R.A.; Brady, S.S.; Resnick, M.D.; Borowsky, I.W.; Connett, J.E.; Krueger, R.F.; Nguyen-Feng, V.N.; et al. Intimate partner violence in late adolescence and young adulthood and subsequent cardiovascular risk in adulthood. Prev. Med. 2016, 87, 132–137. [Google Scholar] [CrossRef]
- García-Moreno, C.; Pallitto, C.; Devries, K.; Abrahams, N.; Bacchus, L.; Child, J.; Hill, A.; Mak, J.; McCleary-Sills, J. Global and Regional Estimates of Violence against Women: Prevalence and Health Effects of Intimate Partner Violence and Non-Partner Sexual Violence; WHO Press: Geneva, Switzerland, 2013. [Google Scholar]
- Suglia, S.F.; Sapra, K.J.; Koenen, K.C. Violence and cardiovascular health: A systematic review. Am. J. Prev. Med. 2015, 48, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Gilchrist, G.; Hegarty, K.; Chondros, P.; Herrman, H.; Gunn, J. The association between intimate partner violence, alcohol and depression in family practice. BMC Fam. Pract. 2010, 11, 72. [Google Scholar] [CrossRef]
- Bonomi, A.E.; Anderson, M.L.; Rivara, F.P.; Thompson, R.S. Health outcomes in women with physical and sexual intimate partner violence exposure. J. Womens Health 2007, 16, 987–997. [Google Scholar] [CrossRef]
- Brygger Venø, L.; Jarbøl, D.E.; Pedersen, L.B.; Søndergaard, J.; Ertmann, R.K. General practitioners’ perceived indicators of vulnerability in pregnancy—A qualitative interview study. BMC Fam. Pract. 2021, 22, 135. [Google Scholar] [CrossRef]
- Coker, A.L.; Davis, K.E.; Arias, I.; Desai, S.; Sanderson, M.; Brandt, H.M.; Smith, P.H. Physical and mental health effects of intimate partner violence for men and women. Am. J. Prev. Med. 2002, 23, 260–268. [Google Scholar] [CrossRef]
- Devries, K.M.; Mak, J.Y.; Bacchus, L.J.; Child, J.C.; Falder, G.; Petzold, M.; Astbury, J.; Watts, C.H. Intimate partner violence and incident depressive symptoms and suicide attempts: A systematic review of longitudinal studies. PLoS Med. 2013, 10, e1001439. [Google Scholar] [CrossRef]
- Ackard, D.M.; Eisenberg, M.E.; Neumark-Sztainer, D. Long-term impact of adolescent dating violence on the behavioral and psychological health of male and female youth. J. Pediatr. X 2007, 151, 476–481. [Google Scholar] [CrossRef] [PubMed]
- Øverup, C.S.; DiBello, A.M.; Brunson, J.A.; Acitelli, L.K.; Neighbors, C. Drowning the pain: Intimate partner violence and drinking to cope prospectively predict problem drinking. Addict. Behav. 2015, 41, 152–161. [Google Scholar] [CrossRef] [PubMed]
- European Union Agency for Fundamental Rights (FRA). Violence against Women: An EU-Wide Survey. Results at a Glance 2014. Available online: https://fra.europa.eu/de/publication/2014/gewalt-gegen-frauen-eine-eu-weite-erhebung-ergebnisse-auf-einen-blick (accessed on 13 July 2020).
- Schlack, R.; Rüdel, J.; Karger, A.; Hölling, H. Körperliche und psychische Gewalterfahrungen in der deutschen Erwachsenenbevölkerung: Ergebnisse der Studie zur Gesundheit von Erwachsenen in Deutschland (DEGS1). Bundesgesundheitsblatt Gesundh. Gesundh. 2013, 56, 755–764. [Google Scholar] [CrossRef]
- Chester, D.S.; DeWall, C.N. The roots of intimate partner violence. Curr. Opin. Psychol. 2018, 19, 55–59. [Google Scholar] [CrossRef]
- Birkel, C.; Church, D.; Hummelsheim-Doss, D.; Leitgöb-Guzy, N.; Oberwittler, D. Der Deutsche Viktimisierungssurvey 2017: Opfererfahrungen, Kriminalitätsbezogene Einstellungen Sowie Die Wahrnehmung von Unsicherheit und Kriminalität in Deutschland 2019. Available online: https://www.bka.de/DE/AktuelleInformationen/StatistikenLagebilder/ViktimisierungssurveyDunkelfeldforschung/viktimisierungssurveyDunkelfeldforschung_node.html (accessed on 8 July 2020).
- Müller, U.; Schöttle, M. Lebenssituation, Sicherheit und Gesundheit von Frauen in Deutschland. Eine Repräsentative Untersuchung zu Gewalt gegen Frauen in Deutschland im Auftrag des Bundesministeriums für Familie, Senioren, Frauen und Jugend; Bielefeld University: Bielefeld, Germany, 2004. [Google Scholar]
- Kolbe, V.; Büttner, A. Häusliche Gewalt gegen Männer—Auch ein rechtsmedizinisches Problem? Rechtsmedizin 2020, 117, 534–541. [Google Scholar] [CrossRef]
- Mark, H. Häusliche Gewalt gegen Frauen aus der Sicht niedergelassener Ärztinnen und Ärzte: Ergebnisse einer Befragung in den Berliner Bezirken Hohenschönhausen und Lichtenberg. Z. Gesundh. 2000, 8, 332–346. [Google Scholar] [CrossRef]
- World Health Organization. Caring for Women Subjected to Violence: A WHO Curriculum for Training Health-Care Providers. 2019. Available online: https://apps.who.int/iris/bitstream/handle/10665/330084/9789241517102-eng.pdf (accessed on 9 January 2022).
- World Health Organization. Health Care for Women Subjected to Intimate Partner Violence or Sexual Violence: A Clinical Handbook; WHO Press: Luxembourg, 2014. [Google Scholar]
- World Health Organization. Responding to Intimate Partner Violence and Sexual Violence against Women: WHO Clinical and Policy Guidelines; WHO Press: Geneva, Switzerland, 2013. [Google Scholar]
- Hornberg, C. Gesundheitliche Folgen von Gewalt: Unter besonderer Berücksichtigung von Häuslicher Gewalt gegen Frauen; Robert-Koch-Inst: Berlin, Germany, 2008. [Google Scholar]
- Zimmermann, T.; Mews, C.; Kloppe, T.; Tetzlaff, B.; Hadwiger, M.; Knesebeck von dem, O.; Scherer, M. Soziale Probleme in der hausärztlichen Versorgung—Häufigkeit, Reaktionen, Handlungsoptionen und erwünschter Unterstützungsbedarf aus der Sicht von Hausärztinnen und Hausärzten. Z. Evid. Fortbild. Qual. Gesundhwes 2018, 131, 81–89. [Google Scholar] [CrossRef]
- Mark, H.; Bitzker, K.; Grimm, A.; Klapp, B.; Rauchfuß, M. Gesundheitsstörungen erwachsener Frauen im Zusammenhang mit körperlicher und sexueller Gewalt—Ergebnisse einer Berliner Patientinnenstudie. Geburtshilfe Frauenheilkd 2007, 67, 43–49. [Google Scholar] [CrossRef]
- Tan, E.; O´Doherty, L.; Hegarty, K. GPs’ communication skills: A study into women’s comfort to disclose intimate partner violence. Aust. Fam. Physician 2012, 41, 513–517. [Google Scholar]
- Yeung, H.; Chowdhury, N.; Malpass, A.; Feder, G.S. Responding to domestic violence in general practice: A qualitative study on perceptions and experiences. Int. J. Fam. Med. 2012, 2012, 960523. [Google Scholar] [CrossRef] [PubMed]
- Arnocky, S.; Vaillancourt, T. Sex Differences in Response to Victimization by an Intimate Partner: More Stigmatization and Less Help-Seeking among Males. J. Aggress. Maltreatment Trauma 2014, 23, 705–724. [Google Scholar] [CrossRef]
- Simmons, J.; BrüggemAnn, A.J.; Swahnberg, K. Disclosing victimisation to healthcare professionals in Sweden: A constructivist grounded theory study of experiences among men exposed to interpersonal violence. BMJ Open 2016, 6, e010847. [Google Scholar] [CrossRef]
- Huntley, A.L.; Potter, L.; Williamson, E.; Malpass, A.; Szilassy, E.; Feder, G. Help-seeking by male victims of domestic violence and abuse (DVA): A systematic review and qualitative evidence synthesis. BMJ Open 2019, 9, e021960. [Google Scholar] [CrossRef] [PubMed]
- Luppa, M.; Giersdorf, J.; Riedel-Heller, S.; Prütz, F.; Rommel, A. Frequent attenders in the German healthcare system: Determinants of high utilization of primary care services. Results from the cross-sectional German health interview and examination survey for adults (DEGS). BMC Fam. Pract. 2020, 21, 10. [Google Scholar] [CrossRef]
- Brzank, P.; Blättner, B.; Hahn, D. Valide Aussagen zu Gewalt im Geschlechterverhältnis erfordern gendersensible Erfassung. Bundesgesundheitsblatt Gesundh. Gesundh. 2013, 56, 1335–1336. [Google Scholar]
- Kurth, B.-M.; Lange, C.; Kamtsiuris, P.; Hölling, H. Gesundheitsmonitoring Am. Robert Koch-Institut. Sachstand und Perspektiven. Bundesgesundheitsbl 2009, 52, 557–570. [Google Scholar] [CrossRef]
- Scheidt-Nave, C.; Kamtsiuris, P.; Gößwald, A.; Hölling, H.; Lange, M.; Busch, M.A.; Dahm, S.; Dölle, R.; Ellert, U.; Fuchs, J.; et al. German health interview and examination survey for adults (DEGS)—design, objectives and implementation of the first data collection wave. BMC Public Health 2012, 12, 730. [Google Scholar] [CrossRef]
- Kamtsiuris, P.; Lange, M.; Hoffmann, R.; Schaffrath Rosario, A.; Dahm, S.; Kuhnert, R.; Kurth, B.M. Die erste Welle der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1): Stichprobendesign, Response, Gewichtung und Repräsentativität. Bundesgesundheitsbl 2013, 56, 620–630. [Google Scholar] [CrossRef]
- Gößwald, A.; Lange, M.; Kamtsiuris, P.; Kurth, B-M. DEGS: Studie zur Gesundheit Erwachsener in Deutschland. Bundesweite Quer- und Längsschnittstudie im Rahmen des Gesundheitsmonitorings des Robert Koch-Instituts. Bundesgesundheitsbl 2012, 55, 80. [Google Scholar] [CrossRef]
- Gößwald, A.; Lange, M.; Dölle, R.; Hölling, H. Die erste Welle der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1): Gewinnung von Studienteilnehmenden, Durchführung der Feldarbeit und Qualitätsmanagement. Bundesgesundheitsbl 2013, 56, 611–619. [Google Scholar] [CrossRef]
- Lampert, T.; Kroll, L.; Müters, S.; Stolzenberg, H. Messung des sozioökonomischen Status in der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1). Bundesgesundheitsbl 2013, 56, 631–636. [Google Scholar] [CrossRef]
- Brauns, H.; Scherer, S.; SteinmAnn, S. The CASMIN Educational Classification in International Comparative Research. In Advances in Cross-National Comparison: A European Working Book for Demographic and Socio-Economic Variables; Hoffmeyer-Zlotnik, J.H.P., Wolf, C., Eds.; Springer: Boston, MA, USA, 2003; pp. 221–244. [Google Scholar]
- Arroll, B.; Goodyear-Smith, F.; Crengle, S.; Gunn, J.; Kerse, N.; Fishman, T.; Falloon, K.; Hatcher, S. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann. Fam. Med. 2010, 8, 348–353. [Google Scholar] [CrossRef]
- Löwe, B.; Kroenke, K.; Gräfe, K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J. Psychosom. Res. 2005, 58, 163–171. [Google Scholar] [CrossRef]
- Bush, K.; Kivlahan, D.R.; McDonell, M.B.; Fihn, S.D.; Bradley, K.A.; Ambulatory Care Quality Improvement Project (ACQUIP). The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Arch. Intern. Med. 1998, 158, 1789–1795. [Google Scholar] [CrossRef]
- Hapke, U.; Von der Lippe, E.; Gaertner, B. Riskanter Alkoholkonsum und Rauschtrinken unter Berücksichtigung von Verletzungen und der Inanspruchnahme alkoholspezifischer medizinischer Beratung: Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1). Bundesgesundheitsblatt Gesundh. Gesundh. 2013, 56, 809–813. [Google Scholar] [CrossRef]
- Lampert, T.; Lippe E von der Müters, S. Verbreitung des Rauchens in der Erwachsenenbevölkerung in Deutschland: Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1). Bundesgesundheitsblatt Gesundh. Gesundh. 2013, 56, 802–808. [Google Scholar] [CrossRef]
- Lange, C.; Starker, A.; von der Lippe, E.; Hölling, H. Psychische und körperliche Gewalterfahrungen in den vergangenen 12 Monaten in der Allgemeinbevölkerung. Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1). Bundesgesundheitsbl 2016, 59, 4–16. [Google Scholar] [CrossRef]
- Brzank, P.; Hellbernd, H.; Maschewsky-Schneider, U.; Kallischnigg, G. Häusliche Gewalt gegen Frauen und Versorgungsbedarf. Ergebnisse einer Befragung von Patientinnen einer Ersten Hilfe/Rettungsstelle. Bundesgesundheitsblatt Gesundh. Gesundh. 2005, 48, 337–345. [Google Scholar] [CrossRef]
- Sugg, N.K. Primary Care Physicians’ Response to Domestic Violence. JAMA 1992, 267, 3157–3160. [Google Scholar] [CrossRef]
- Birkhoff, E.M.L.; Krouwel, E.M.; Nicolai, M.P.J.; De Boer, B.-J.; Beck, J.J.; Putter, H.; Pelger, R.C.M.; Elzevier, H.W. Dealing with patients facing a history of sexual abuse: A cross-sectional survey among Dutch general practitioners. Eur. J. Gen. Pract. 2016, 22, 126–133. [Google Scholar] [CrossRef]
- Black, M.C. Intimate Partner Violence and Adverse Health Consequences. Am. J. Lifestyle Med. 2011, 5, 428–439. [Google Scholar] [CrossRef]
- Sprague, S.; Madden, K.; Simunovic, N.; Godin, K.; Pham, N.K.; Bhandari, M.; Goslings, J.C. Barriers to screening for intimate partner violence. Women Health 2012, 52, 587–605. [Google Scholar] [CrossRef]
- Narula, A.; Agarwal, G.; McCarthy, L. Intimate partner violence: Patients’ experiences and perceptions in family practice. Fam. Pract. 2012, 29, 593–600. [Google Scholar] [CrossRef]
- Sugg, N. Intimate partner violence: Prevalence, health consequences, and intervention. Med. Clin. N. Am. 2015, 99, 629–649. [Google Scholar] [CrossRef]
- Hegarty, K.L.; Taft, A.J. Overcoming the barriers to disclosure and inquiry of partner abuse for women attending general practice. Aust. N. Z. J. Public Health 2001, 25, 433–437. [Google Scholar] [CrossRef]
- Bradley, F. Reported frequency of domestic violence: Cross sectional survey of women attending general practice. BMJ 2002, 324, 271. [Google Scholar] [CrossRef]
- Recupero, P.R. The Notion of Truth and Our Evolving Understanding of Sexual Harassment. J. Am. Acad. Psychiatry Law 2018, 46, 23–30. [Google Scholar]
- Hegarty, K.; Gunn, J.; Chondros, P.; Taft, A. Physical and social predictors of partner abuse in women attending general practice: A cross-sectional study. Br. J. Gen. Pract. 2008, 58, 484–487. [Google Scholar] [CrossRef]
- Kimmel, M.S. ‘Gender Symmetry’ in Domestic Violence: A Substantive and Methodological Research. Review. Violence Women 2002, 8, 1332–1363. [Google Scholar] [CrossRef]
- Richardson, J.; Feder, G. Domestic violence: A hidden problem for general practice. Br. J. Gen. Pract. 1996, 46, 239–242. [Google Scholar]
- Alejo, K. Long-term physical and mental health effects of domestic violence. ThemisRes. J. Justice Stud. Forensic Sci. 2014, 2, 82–98. [Google Scholar] [CrossRef]
- Howard, L.M.; Trevillion, K.; Agnew-Davies, R. Domestic violence and mental health. Int. Rev. Psychiatry 2010, 22, 525–534. [Google Scholar] [CrossRef]
- McEwen, B.S. Stress and the Individual. Arch. Intern. Med. 1993, 153, 2093. [Google Scholar] [CrossRef]
- Black, P.H.; Garbutt, L.D. Stress, inflammation and cardiovascular disease. J. Psychosom. Res. 2002, 52, 1–23. [Google Scholar] [CrossRef]
- Olive, P. First contact: Acute stress reactions and experiences of emergency department consultations following an incident of intimate partner violence. J. Clin. Nurs. 2017, 26, 2317–2327. [Google Scholar] [CrossRef]
- Warda, G.; Bryant, R.A. Cognitive bias in acute stress disorder. Behav. Res. Ther. 1998, 36, 1177–1183. [Google Scholar] [CrossRef]
- Trevillion, K.; Oram, S.; Feder, G.; Howard, L.M. Experiences of domestic violence and mental disorders: A systematic review and meta-analysis. PLoS ONE 2012, 7, e51740. [Google Scholar] [CrossRef]
- Crane, C.A.; Hawes, S.W.; Weinberger, A.H. Intimate partner violence victimization and cigarette smoking: A meta-analytic review. Trauma Violence Abus. 2013, 14, 305–315. [Google Scholar] [CrossRef]
- Campbell, A.M. An increasing risk of family violence during the COVID-19 pandemic: Strengthening community collaborations to save lives. Forensic Sci. Int. Rep. 2020, 2, 100089. [Google Scholar] [CrossRef]
- Sacco, M.A.; Caputo, F.; Ricci, P.; Sicilia, F.; De Aloe, L.; Bonetta, C.F.; Cordasco, F.; Scalise, C.; Cacciatore, G.; Zibetti, A.; et al. The impact of the COVID-19 pandemic on domestic violence: The dark side of home isolation during quarantine. Med. Leg. J. 2020, 88, 71–73. [Google Scholar] [CrossRef]
- Szilassy, E.; Barbosa, E.C.; Dixon, S.; Feder, G.; Griffiths, C.; Johnson, M.; De Simoni, A.; Wileman, V.; Panovska-Griffiths, J.; Dowrick, A. PRimary care rEsponse to domestic violence and abuse in the COVID-19 panDEmic (PRECODE): Protocol of a rapid mixed-methods study in the UK. BMC Fam. Pract. 2021, 22, 91. [Google Scholar] [CrossRef]
- Feder, G.; Davies, R.A.; Baird, K.; Dunne, D.; Eldridge, S.; Griffiths, C.; Gregory, A.; Howell, A.; Johnson, M.; Ramsay, J.; et al. Identification and Referral to Improve Safety (IRIS) of women experiencing domestic violence with a primary care training and support programme: A cluster randomised controlled trial. Lancet 2011, 378, 1788–1795. [Google Scholar] [CrossRef]
- Williamson, E.; Jones, S.K.; Ferrari, G.; Debbonaire, T.; Feder, G.; Hester, M. Health professionals responding to men for safety (HERMES): Feasibility of a general practice training intervention to improve the response to male patients who have experienced or perpetrated domestic violence and abuse. Prim. Health Care Res. Dev. 2015, 16, 281–288. [Google Scholar] [CrossRef]
- Gear, C.; Koziol-McLain, J.; Wilson, D.; Clark, F. Developing a response to family violence in primary health care: The New Zealand experience. BMC Fam. Pract. 2016, 17, 115. [Google Scholar] [CrossRef]

| N * (n = 5938) | % * | |
|---|---|---|
| Gender (female) | 3149 | 49.4 |
| Age, mean, SD | 41.63 | 13.06 |
| Age groups | ||
| 1072 | 23.2 |
| 1730 | 31.4 |
| 3136 | 45.4 |
| SES | ||
| 847 | 18.0 |
| 3521 | 60.6 |
| 1506 | 21.4 |
| Health and medical information | ||
| Middle to very poor subjective health | 1219 | 20.6 |
| Physician-diagnosed depression (ever in life) | 677 | 11.2 |
| Depression in last 12 months (n = 709) | 335 | 54.4 |
| Current depressive symptoms (PHQ2) | 414 | 7.8 |
| Anxiety disorder (ever diagnosed in life) | 316 | 5.4 |
| Chronic disease | 1501 | 24.4 |
| Health behavior | ||
| (Occasional) Smoker | 2115 | 29.8 |
| Risky alcohol consumption | 2517 | 31.8 |
| Violence experiences (VE) | ||
| Lifetime VE | 4042 | 71.1 |
| 3544 | 62.5 |
| 2927 | 51.7 |
| Recent VE (past 12 months) | 1106 | 20.7 |
| 1027 | 18.7 |
| 203 | 4.8 |
| 124 | 2.9 |
| Impaired in well-being due to any recent VE (psychological and/or physical) (N = 949) | 933 | 86.9 |
| 416 | 42.4 |
| 58 | 28.9 |
| GP contact | ||
| Has a GP | 5261 | 89.1 |
| GP visits in past 12 months, mean, SD | 2.99 | 4.54 |
| Recent VE (n = 1106) | No Recent VE (n = 4700) | p-Value | |||
|---|---|---|---|---|---|
| N * | % | N * | % | ||
| Gender (female) | 594 | 21.1 | 2486 | 78.9 | n.s. |
| Age, mean, SD | 36.4 | 13.0 | 42.9 | 12.8 | <0.001 |
| Age groups | |||||
| 347 | 32.8 | 717 | 67.2 | <0.001 |
| 337 | 21.2 | 1351 | 78.9 | |
| 422 | 14.0 | 2632 | 86.0 | |
| SES | |||||
| 189 | 24.3 | 625 | 75.7 | 0.001 |
| 665 | 20.9 | 2812 | 79.1 | |
| 246 | 16.3 | 1249 | 83.7 | |
| Health and medical information | |||||
| Middle to very poor subjective health | 273 | 23.7 | 915 | 19.5 | 0.010 |
| Physician-diagnosed depression in life | 208 | 18.0 | 448 | 9.3 | <0.001 |
| Depression in last 12 months (n = 709) | 117 | 62.2 | 202 | 49.5 | 0.025 |
| Current depressive symptoms (PHQ2) | 165 | 15.7 | 239 | 5.5 | <0.001 |
| Anxiety disorder (ever diagnosed in life) | 93 | 8.7 | 214 | 4.5 | <0.001 |
| Chronic disease | 293 | 25.9 | 1176 | 23.8 | n.s. |
| Health behavior | |||||
| (Occasional) Smoker | 430 | 43.0 | 1445 | 32.3 | <0.001 |
| Risky alcohol consumption | 400 | 37.4 | 1610 | 34.0 | 0.026 |
| Contact to GP | |||||
| Has a GP | 976 | 86.4 | 4244 | 89.7 | 0.006 |
| GP visits in past 12 months, mean, SD | 3.47 | 4.98 | 2.87 | 4.42 | <0.001 |
| Estimates | Standard Error | 95%-CI Lower Limit | 95%-CI Upper Limit | p-Value | |
|---|---|---|---|---|---|
| Constant | 2.590 | 0.182 | 2.231 | 2.949 | <0.001 |
| Women (ref.: men) | 0.352 | 0.072 | 0.210 | 0.493 | <0.001 |
| Having recent VE * (ref.: no recent VE *) | 0.327 | 0.123 | 0.084 | 0.570 | 0.009 |
| Middle to very poor subjective health (ref.: very good/good) | 1.461 | 0.165 | 1.135 | 1.788 | <0.001 |
| Having a chronic disease (ref.: no chronic disease) | 1.560 | 0.126 | 1.311 | 1.808 | <0.001 |
| Physician-diagnosed depression in life (ref.: never) | 0.900 | 0.197 | 0.511 | 1.290 | <0.001 |
| Age in years | −0.006 | 0.003 | 0.003 | 0.001 | 0.086 |
| SES sum score | −0.600 | 0.011 | −0.083 | −0.038 | <0.001 |
| R2 Adj | 18.1% | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hunzelar, C.; Krumpholtz, Y.; Schlack, R.; Weltermann, B. More GP Consultations by Violence Victims: Results from the Representative German DEGS1 Study. Int. J. Environ. Res. Public Health 2023, 20, 4646. https://doi.org/10.3390/ijerph20054646
Hunzelar C, Krumpholtz Y, Schlack R, Weltermann B. More GP Consultations by Violence Victims: Results from the Representative German DEGS1 Study. International Journal of Environmental Research and Public Health. 2023; 20(5):4646. https://doi.org/10.3390/ijerph20054646
Chicago/Turabian StyleHunzelar, Carmen, Yelda Krumpholtz, Robert Schlack, and Birgitta Weltermann. 2023. "More GP Consultations by Violence Victims: Results from the Representative German DEGS1 Study" International Journal of Environmental Research and Public Health 20, no. 5: 4646. https://doi.org/10.3390/ijerph20054646
APA StyleHunzelar, C., Krumpholtz, Y., Schlack, R., & Weltermann, B. (2023). More GP Consultations by Violence Victims: Results from the Representative German DEGS1 Study. International Journal of Environmental Research and Public Health, 20(5), 4646. https://doi.org/10.3390/ijerph20054646






