Profile of Maternal Mortality of COVID-19 in Ceará, in the Period of 2020
Abstract
1. Introduction
2. Materials and Methods (Track Changes)
2.1. Design
2.2. Place, Period, and Population of the Study
2.3. Data Collection Instruments and Variables
2.4. Data Analysis
2.5. Ethical Aspects
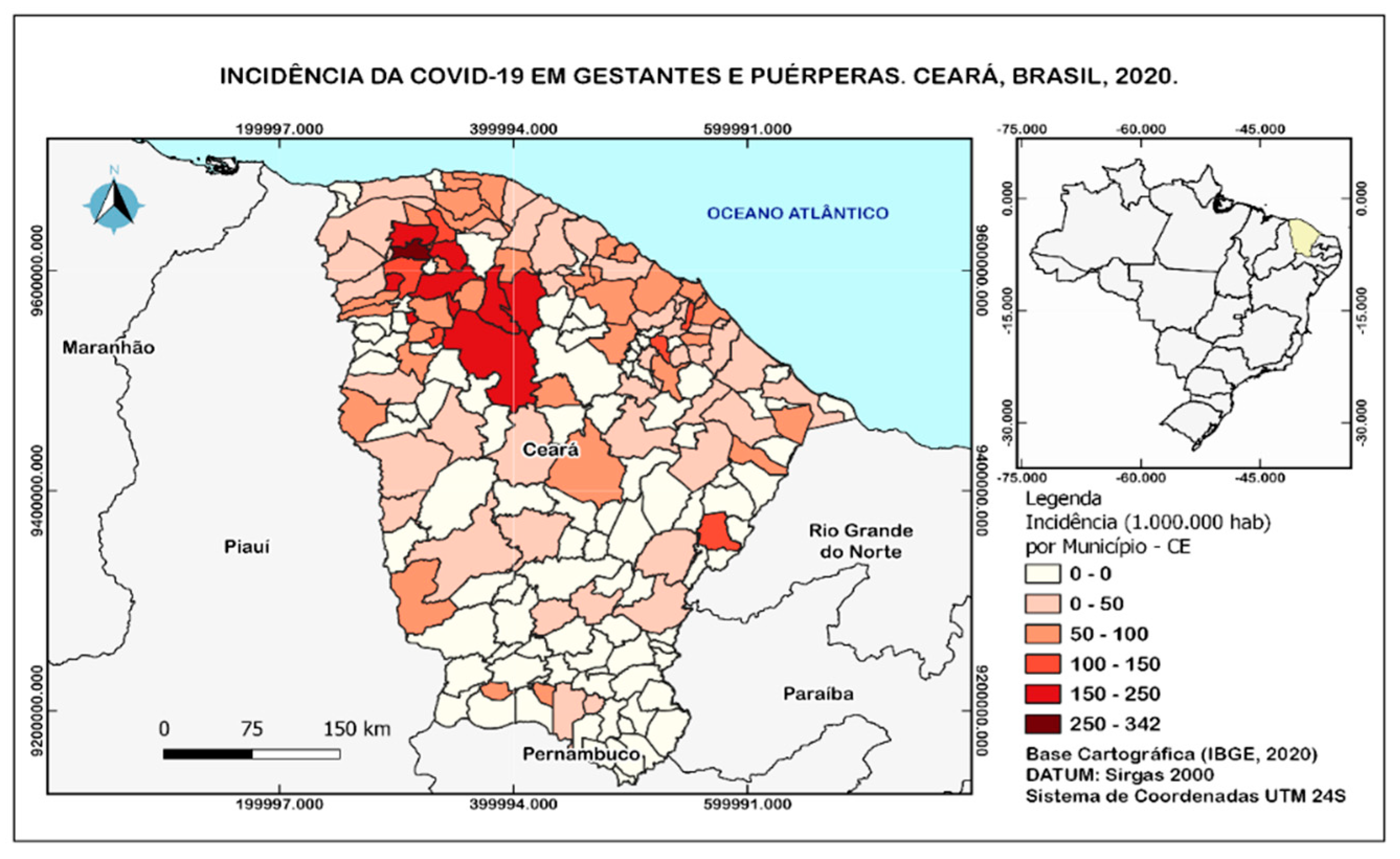
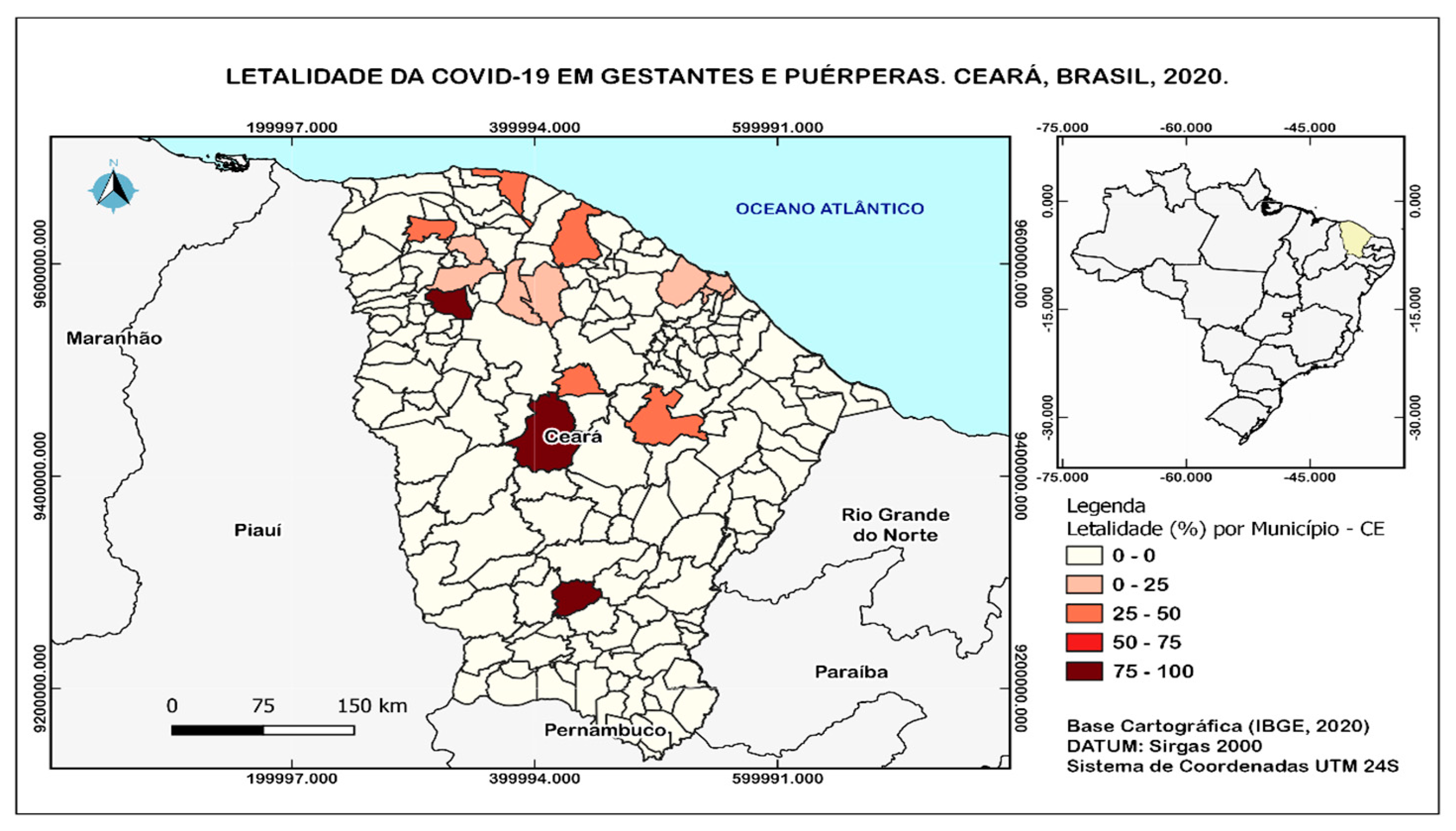
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Albuquerque, N.; Pedrosa, N. Evolução de casos confirmados de COVID-19 em cinco países com transmissão comunitária da doença. SciELO Prepr. 2020. [Google Scholar] [CrossRef]
- Brasil. Ministério da Saúde. Centro de Operações de Emergência em Saúde Pública [Homepage on the Internet]. Brasília: O Ministério; c2020 [Updated 2020 April 20; Cited 2020 April 26]. Boletim COE COVID-19 no. 13: Situação Epidemiológica--Doença pelo Coronavírus 2019. [Adobe Acrobat Document, 18p.]. Available online: https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/boletins/epidemiologicos/covid-19/2020/boletim_epidemiologico_covid_39.pdf (accessed on 16 January 2022).
- Silva, F.V.D.; Souza, K.V.D. A inaceitável tragédia das mortes maternas associadas à COVID-19:(re) politização da saúde e dos direitos das mulheres e o posicionamento da enfermagem brasileira. Rev. Bras. Enferm. 2020, 73 (Suppl. 4), e73supl04. [Google Scholar] [CrossRef]
- Godoi, A.P.N.; Bernardes, G.C.S.; de Almeida, N.A.; de Melo, S.N.; Belo, V.S.; Nogueira, L.S.; Pinheiro, M.D.B. Severe Acute Respiratory Syndrome by COVID-19 in pregnant and postpartum women. Rev. Bras. Saúde Matern. Infant. 2021, 21, 461–469. [Google Scholar] [CrossRef]
- Souza, D.O. A pandemia de COVID-19 para além das Ciências da Saúde: Reflexões sobre sua determinação social. Ciência Saúde Coletiva 2020, 25, 2469–2477. [Google Scholar] [CrossRef] [PubMed]
- Elshafeey, F.; Magdi, R.; Hindi, N.; Elshebiny, M.; Farrag, N.; Mahdy, S.; Sabbour, M.; Gebril, S.; Nasser, M.; Kamel, M.; et al. A systematic scoping review of COVID-19 during pregnancy and childbirth. Int. J. Gynaecol. Obstet. 2020, 150, 47–52. [Google Scholar] [CrossRef]
- Takemoto, M.L.S.; Menezes, M.d.O.; Andreucci, C.B.; Nakamura-Pereira, M.; Amorim, M.M.; Katz, L.; Knobel, R. The tragedy of COVID-19 in Brazil: 124 maternal deaths andcounting. Int. J. Gynecol. Obstet. 2020, 151, 154–156. [Google Scholar] [CrossRef]
- UNFPA Brasil. COVID-19: Um Olhar para Gênero. Promoção da Saúde e Dos Direitos Sexuais e Reprodutivos e Promoção da Igualdade de Gênero, Março. 2020. Available online: https://www.unfpa.org/sites/default/files/resource-pdf/Portoguese-covid19_olhar_genero.pdf (accessed on 16 March 2020).
- Vieira, F.R.P.; Lacerda, L.; Rodrigues, A.S. ‘Obstetric Observatory BRAZIL-COVID-19: 1031 Maternal Deaths Because of COVID-19 and the Unequal Access to Health Care Services. 2021. Available online: https://observatorio.fm.usp.br/handle/OPI/42293 (accessed on 16 March 2020).
- Rodrigues, A.; Lacerda, L.; Francisco, R.P.V. Brazilian Obstetric Observatory. arXiv 2021, arXiv:2105.06534. [Google Scholar]
- Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Indicadores e Dados Básicos; Diário Oficial União: Brasília, Brazil, 2011. Available online: http://tabnet.datasus.gov.br/cgi/idb2011/C03b.htm (accessed on 20 January 2022).
- Cavalcante, J.R.; Abreu, A.J.L. COVID-19 no município do Rio de Janeiro: Análise espacial da ocorrência dos primeiros casos e óbitos confirmados. Epidemiol. Serv. Saude 2020, 29, e2020204. [Google Scholar] [CrossRef] [PubMed]
- Gomes, D.R.; Souza, R.C.; Oliveira, U.R.; Mattos, M.P.; Aleluia, I.R.S.; Mapeli, A.M. Interiorização da COVID-19 no Oeste da Bahia: Perfil epidemiológico e análise espacial dos óbitos e casos confirmados. Ciência Saúde Coletiva 2021, 26, 4665–4680. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, L.M.C.; de Souza, D.R.X.; Bezerra, K.K.S.; Batista, H.M.T.; Sousa, E.S.S.; Bezerra, A.M.F.; de Leite, E.S. Distribuição da Mortalidade Materna no Estado da Paraíba no período de 2007 a 2016/Distribution of Maternal Mortality in Paraiba State from 2007 to 2016. ID on line. Rev. Psicol. 2020, 14, 486–501. [Google Scholar] [CrossRef]
- Duarte, E.M.d.S.; Alencar, É.T.d.S.; Fonseca, L.G.A.d.; Silva, S.M.d.; Machado, M.F.; Araújo, M.D.P.d.; Correia, D.S.; Souza, C.D.F.d. Mortalidade materna e vulnerabilidade social no Estado de Alagoas no Nordeste brasileiro: Uma abordagem espaço-temporal. Rev. Bras. Saúde Matern. Infant. 2020, 20, 575–586. [Google Scholar] [CrossRef]
- Menezes, M.O.; Takemoto, M.L.S.; Nakamura-Pereira, M.; Katz, L.; Amorim, M.M.R.; Salgado, H.O.; Melo, A.; Diniz, C.G.S.; de Sousa, L.A.R.; Magalhaes, C.G.; et al. Risk factors for adverse outcomes among pregnant and postpartum women with acute respiratory distress syndrome due to COVID-19 in Brazil. Int. J. Gynecol. Obstet. 2020, 151, 415–423. [Google Scholar] [CrossRef] [PubMed]
- Brasil. Portaria nº 1.459, de 24 de Junho de 2011. Institui, no Âmbito do Sistema Único de Saúde—SUS—A Rede Cegonha. 2011. Available online: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2011/prt1459_24_06_2011.html (accessed on 5 February 2022).
- Mascarenhas, P.M.; da Silva, G.R.; Reis, T.T.; Casotti, C.A.; Nery, A.A. Análise da mortalidade materna. Rev. Enferm. UFPE Online 2017, 2017, 4653–4662. [Google Scholar]
- Felczak, C.; Ravelli, A.P.X.; Skupien, S.V.; Ricken, M.H.; Bayer, L.C.D.; Almeida, E.A. Profile of cardiac pregnant women: High-risk. Cogitare Enferm. 2018, 23, e49605. [Google Scholar] [CrossRef]
- Brito, J.G.E.; de Alencar, C.C.A.; Lemos, A.C.; Caetano, C.L.R.; Max Oliveira Menezes Barreiro, M.S.C. Características clínicas, sociodemográficas e desfechos de gestantes hospitalizadas com COVID-19. Res. Soc. Dev. 2021, 10, e33101723049. [Google Scholar] [CrossRef]
- Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. (2021). Boletim Epidemiológico Especial COE- COVID-19 nº 86. Available online: https://www.gov.br/saude/pt-br/media/pdf/2021/outubro/29/boletim_epidemiologico_covid_86-final-_29out.pdf (accessed on 12 February 2022).
- Marinho, A.C.D.N.; Paes, N.A. Maternal mortality in the state of Paraíba-Brazil: Association between variables. Rev. Esc. Enferm. USP 2010, 44, 732–738. [Google Scholar] [CrossRef]
- Burton, G.J.; Redman, C.W.; Roberts, J.M.; Moffett, A. Pre-eclampsia: Pathophysiology and clinical implications. BMJ 2019, 366, 12381. [Google Scholar] [CrossRef]
- Do Leal, M.C.; Szwarcwald, C.L.; Almeida, P.V.; Aquino EM, L.; Barreto, M.L.; Barros, F.; Victora, C. Saúde reprodutiva, materna, neonatal e infantil nos 30 anos do Sistema Único de Saúde (SUS). Ciência Saúde Coletiva 2018, 23, 1915–1928. [Google Scholar] [CrossRef]
- Qeadan, F.; Mensah, N.A.; Tingey, B.; Stanford, J.B. The risk of clinical complications and death among pregnant women with COVID-19 in the Cerner COVID-19 cohort: A retrospective analysis. BMC Pregnancy Childbirth 2021, 21, 305. Available online: https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-021-03772-y#citeas (accessed on 12 February 2022). [CrossRef]
- Souza, A.S.R.; Amorim, M.M.R. Maternal mortality by COVID-19 in Brazil. Rev. Bras. Saúde Matern. Infant. 2021, 2, S253–S256. [Google Scholar] [CrossRef]
- Goes, E.F.; Ramos, D.O.; Ferreira, A.J.F. Desigualdades raciais em saúde e a pandemia da COVID-19. Trab. Educ. Saude 2020, 18, e00278110. [Google Scholar] [CrossRef]
- Santos, A.L.; Santos, M.C.; Santos, L.C.; Meneses, M.O.; Santana, E.M.d.; Borges, C.L. Análise e georreferenciamento da mortalidade materna em Aracaju de 2010 a 2018. Res. Soc. Dev. 2021, 10, e373101220657. [Google Scholar] [CrossRef]
- Rodrigues, A.R.M.; da Dantas, S.L.C.; Pereira, A.M.M.; da Silveira, M.A.M.; Rodrigues, D.P. High-Risk Pregnancy: Analysis of Health Determinants. SANARE-Rev. Políticas Públicas 2017, 16, 23–28. [Google Scholar]
- Gadelha, I.P.; Diniz, F.F.; Aquino, P.S.; Silva, D.M.; Balsells, M.M.D.; Pinheiro, A.K.B. Social determinants of health of high-risk pregnant women during prenatal follow-up. Rev. Rene 2020, 21, e42198. [Google Scholar] [CrossRef]
- Boscarino, J.C.R.; Silva, M.B.; Oliveira, L.L.; Souza, R.R. Gravidez na paciente portadora de insuficiência renal crônica. Glob. Acad. Nurs. 2021, 2, e100. [Google Scholar] [CrossRef]
- Lokken, E.M.; Taylor, G.G.; Huebner, E.M.; Vanderhoe, J.V.; Hendrick, S.; Coler, B.; Sheng, J.S.; Walker, C.L.; McCartney, S.A.; Kretzer, N.M.; et al. Higher severe acute respiratory syndrome coronavirus 2 infection rate in pregnant patients. Am. J. Obstet. Gynecol. 2021, 25, 75.e1–75.e16. [Google Scholar] [CrossRef]
- Di Guardo, F.; Di Grazia, F.M.; Di Gregorio, L.M.; Zambrotta, E.; Carrara, G.; Gulino, F.A.; Tuscano, A.; Palumbo, M. Poor maternal-neonatal outcomes in pregnant patients with confirmed SARS-CoV-2 infection: Analysis of 145 cases. Arch. Gynecol. Obstet. 2021, 303, 1483–1488. [Google Scholar] [CrossRef] [PubMed]
- Kolhe, N.V.; Fluck, R.J.; Selby, N.M.; Taal, M.W. Acute kidney injury associated with COVID-19: A retrospective cohort study. Remuzzi G, organizador. PLoS Med. 2020, 1, e1003406. [Google Scholar]
- Marchiori, J.S.; de Oliveira, M.A.S.; Bezerra, I.M.P. COVID-19 and its relationship with kidney diseases: A scope review. J. Hum. Growth Dev. 2021, 31, 533–548. [Google Scholar] [CrossRef]
- Coelho, V.C.; Andrade, M.S.; de Sena, C.D.; Costa, L.E.L.; Bittencourt, I.S. Caracterização Dos Óbitos Maternos em Três Regiões de Saúde do Centro-Norte Baiano. Cogitare Enferm. 2016, 21, 1. [Google Scholar] [CrossRef]
- Medeiros, L.T.; Sousa, A.M.; Arinana, L.O.; Inácio, A.S.; Prata, M.d.L.C.; Vasconcelos, M.N.G. Mortalidade Materna No Estado do Amazonas: Estudo Epidemiológico. Rev. Baiana Enferm. 2018. [Google Scholar] [CrossRef]
- Monteiro, M.F.G.; Romio, J.A.F.; Drezett, J. Is there race/color differential on femicide in Brazil? The inequality of mortality rates for violent causes among white and black women. J. Hum. Growth Dev. 2021, 31, 358–366. [Google Scholar] [CrossRef]
- Nakamura-Pereira, M.; Amorim, M.M.; Pacagnella, R.C.; Takemoto, M.L.; Penso, F.C.; Rezende-Filho, J.; Leal, M.C. COVID-19 e morte materna no Brasil: Uma tragédia invisível. Femina 2020, 48, 496–498. [Google Scholar]
| Disease Evolution | n | % |
|---|---|---|
| Confirmed cases | 485 | 100.0 |
| Confirmed cure | 411 | 84.7 |
| Confirmed deaths | 28 | 5.8 |
| Ward admission | 463 | 95.5 |
| ICU admission | 61 | 12.6 |
| Non-invasive ventilatory support | 67 | 13.8 |
| Invasive ventilatory support | 35 | 7.2 |
| Profile | n (485) | % |
|---|---|---|
| Age group | ||
| ˂20 | 64 | 13 |
| 20–34 | 320 | 66 |
| ˃35 | 98 | 20 |
| Race/skin color | ||
| Asiatic | 2 | 0.4 |
| White | 17 | 3.5 |
| Aboriginal | 1 | 0.2 |
| Mixed | 341 | 70.3 |
| Black | 2 | 0.4 |
| Ignored | 122 | 25.2 |
| Place of residence | ||
| Periurban | 1 | 0.2 |
| Rural | 72 | 14.8 |
| Urban | 345 | 71.1 |
| Ignored | 67 | 13.8 |
| Education | ||
| No education | 0 | 0.0 |
| Middle school | 21 | 4.3 |
| Elementary school | 29 | 6.0 |
| High school | 82 | 16.9 |
| Graduation | 18 | 3.7 |
| Not informed | 335 | 69.1 |
| Variable | n (485) | % |
|---|---|---|
| Gestational age | ||
| 1st gestational trimester | 26 | 5.4 |
| 2nd gestational trimester | 45 | 9.3 |
| 3rd gestational trimester | 320 | 66.0 |
| Idade Gestacional ignorada | 12 | 2.5 |
| postpartum | 82 | 16.9 |
| Comorbidities | ||
| Cardiovascular | 21 | 4.3 |
| Diabetes | 18 | 3.7 |
| Neuropathies | 3 | 0.6 |
| Pneumopatia | 1 | 0.2 |
| Kidney disease | 67 | 13.8 |
| Obesity | 5 | 1.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Francelino, S.M.A.; Bezerra, I.M.P.; Alves, S.A.A.; Leitão, F.N.C.; de Deus Morais, M.J.; Ramos, J.L.S.; da Rocha, J.B.F.; Antunes, T.P.C.; Smiderle, F.R.N.; de Abreu, L.C. Profile of Maternal Mortality of COVID-19 in Ceará, in the Period of 2020. Int. J. Environ. Res. Public Health 2023, 20, 4645. https://doi.org/10.3390/ijerph20054645
Francelino SMA, Bezerra IMP, Alves SAA, Leitão FNC, de Deus Morais MJ, Ramos JLS, da Rocha JBF, Antunes TPC, Smiderle FRN, de Abreu LC. Profile of Maternal Mortality of COVID-19 in Ceará, in the Period of 2020. International Journal of Environmental Research and Public Health. 2023; 20(5):4645. https://doi.org/10.3390/ijerph20054645
Chicago/Turabian StyleFrancelino, Sheyla Martins Alves, Italla Maria Pinheiro Bezerra, Sabrina Alaide Amorim Alves, Francisco Naildo Cardoso Leitão, Mauro José de Deus Morais, José Lucas Souza Ramos, João Batista Francalino da Rocha, Thaiany Pedrozo Campos Antunes, Fabiana Rosa Neves Smiderle, and Luíz Carlos de Abreu. 2023. "Profile of Maternal Mortality of COVID-19 in Ceará, in the Period of 2020" International Journal of Environmental Research and Public Health 20, no. 5: 4645. https://doi.org/10.3390/ijerph20054645
APA StyleFrancelino, S. M. A., Bezerra, I. M. P., Alves, S. A. A., Leitão, F. N. C., de Deus Morais, M. J., Ramos, J. L. S., da Rocha, J. B. F., Antunes, T. P. C., Smiderle, F. R. N., & de Abreu, L. C. (2023). Profile of Maternal Mortality of COVID-19 in Ceará, in the Period of 2020. International Journal of Environmental Research and Public Health, 20(5), 4645. https://doi.org/10.3390/ijerph20054645






