Reproductive and Obstetric Outcomes after UAE, HIFU, and TFA of Uterine Fibroids: Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Study Registration and Methodological Standards
2.2. Information Sources and Search Strategy
2.3. Eligibility Criteria and PICO Statement
2.4. Data Collection and Synthesis
2.5. Assessment of Risk of Bias
2.6. Statistical Analysis
3. Results
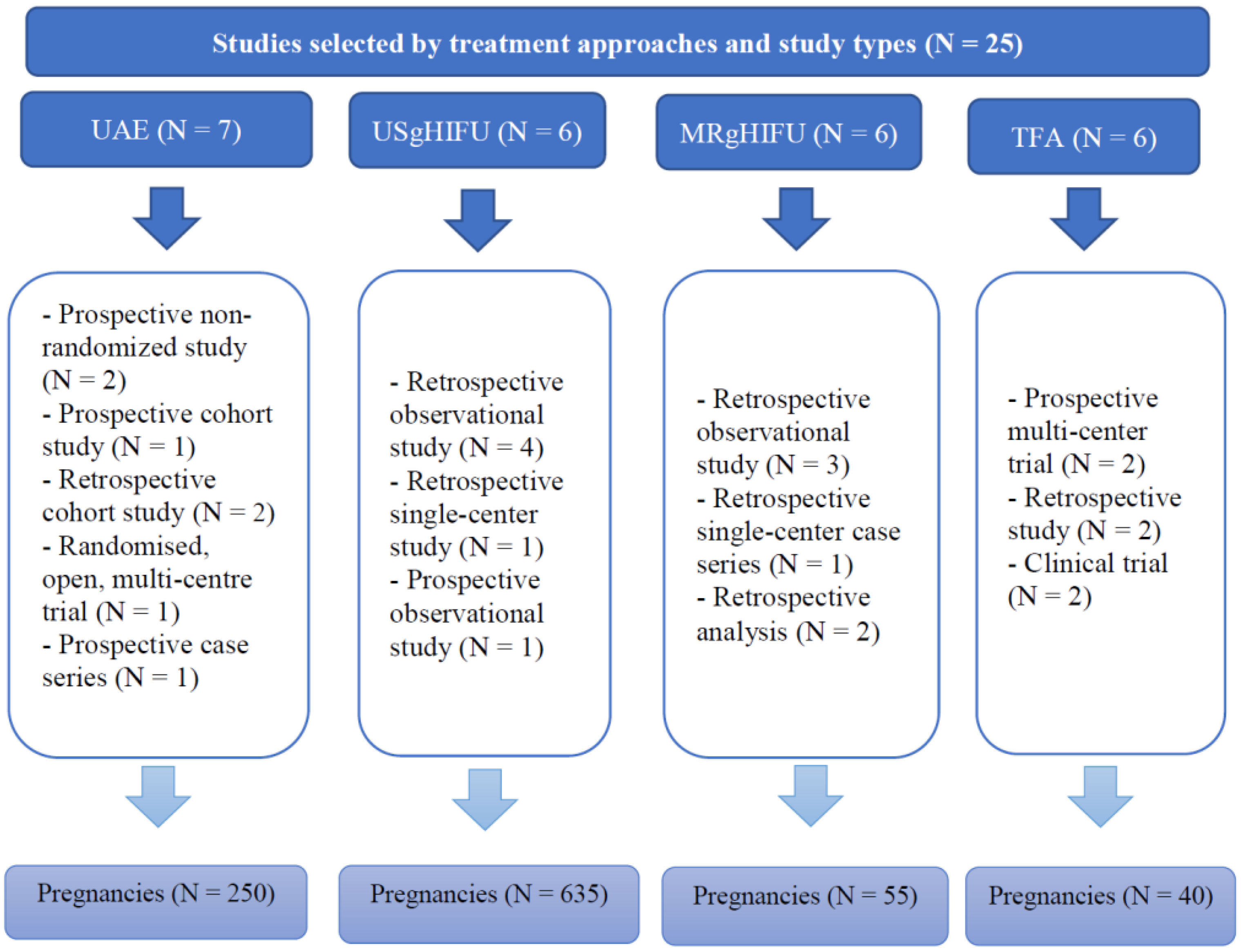
3.1. Study Identification and Selection
3.2. Risk of Bias
3.3. Synthesis of Results
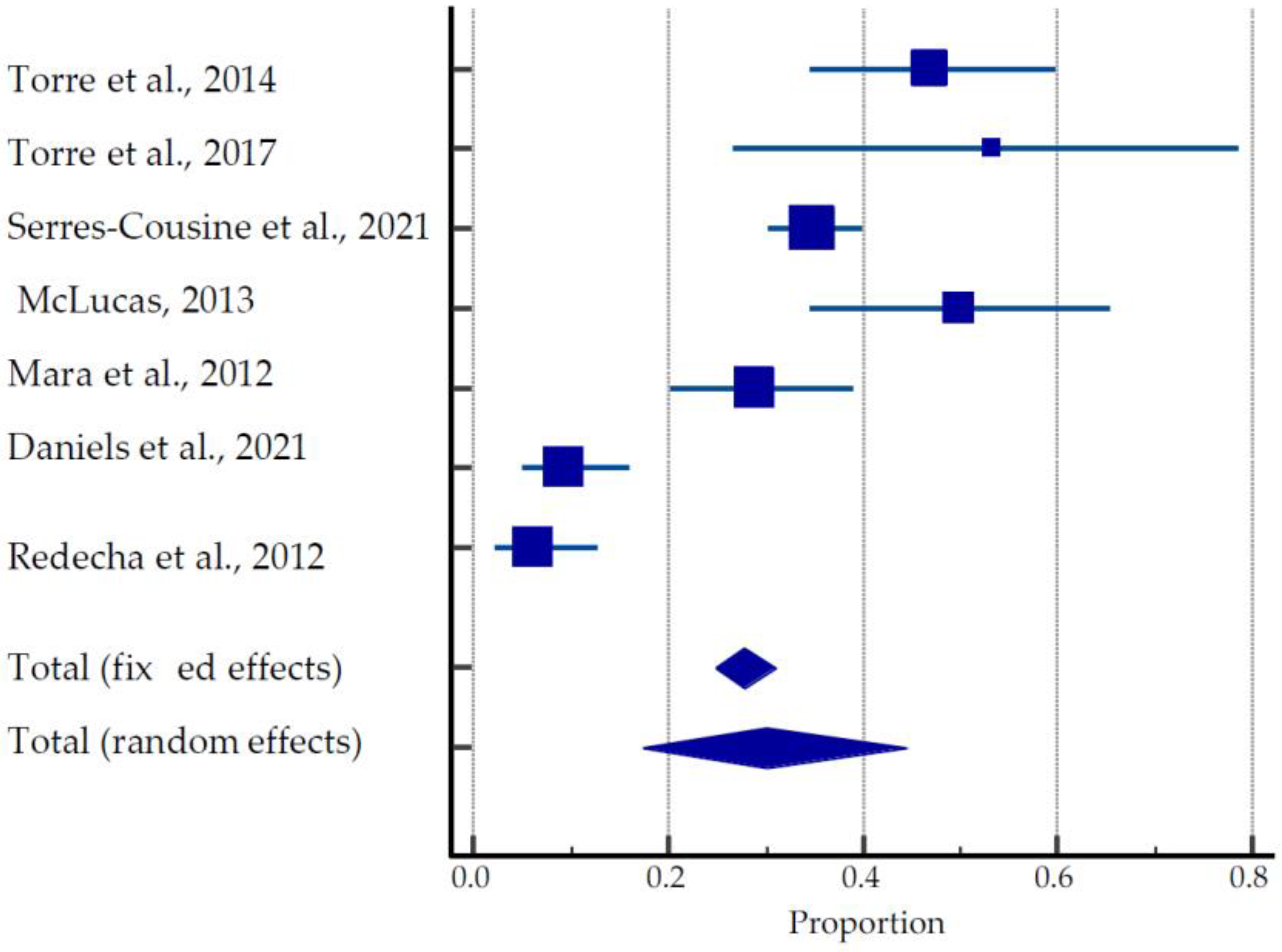
3.3.1. Uterine Artery Embolization
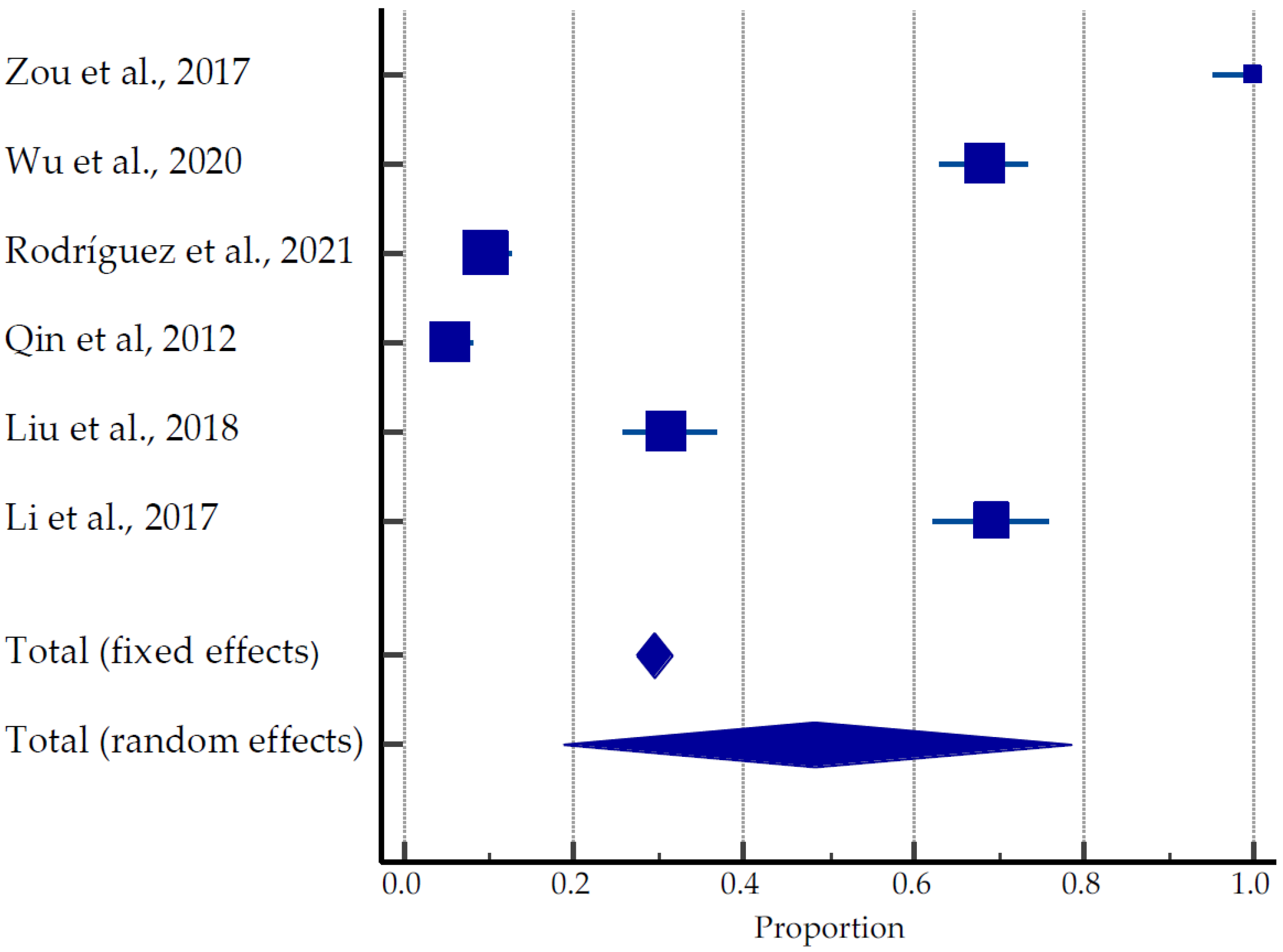
3.3.2. US-Guided HIFU
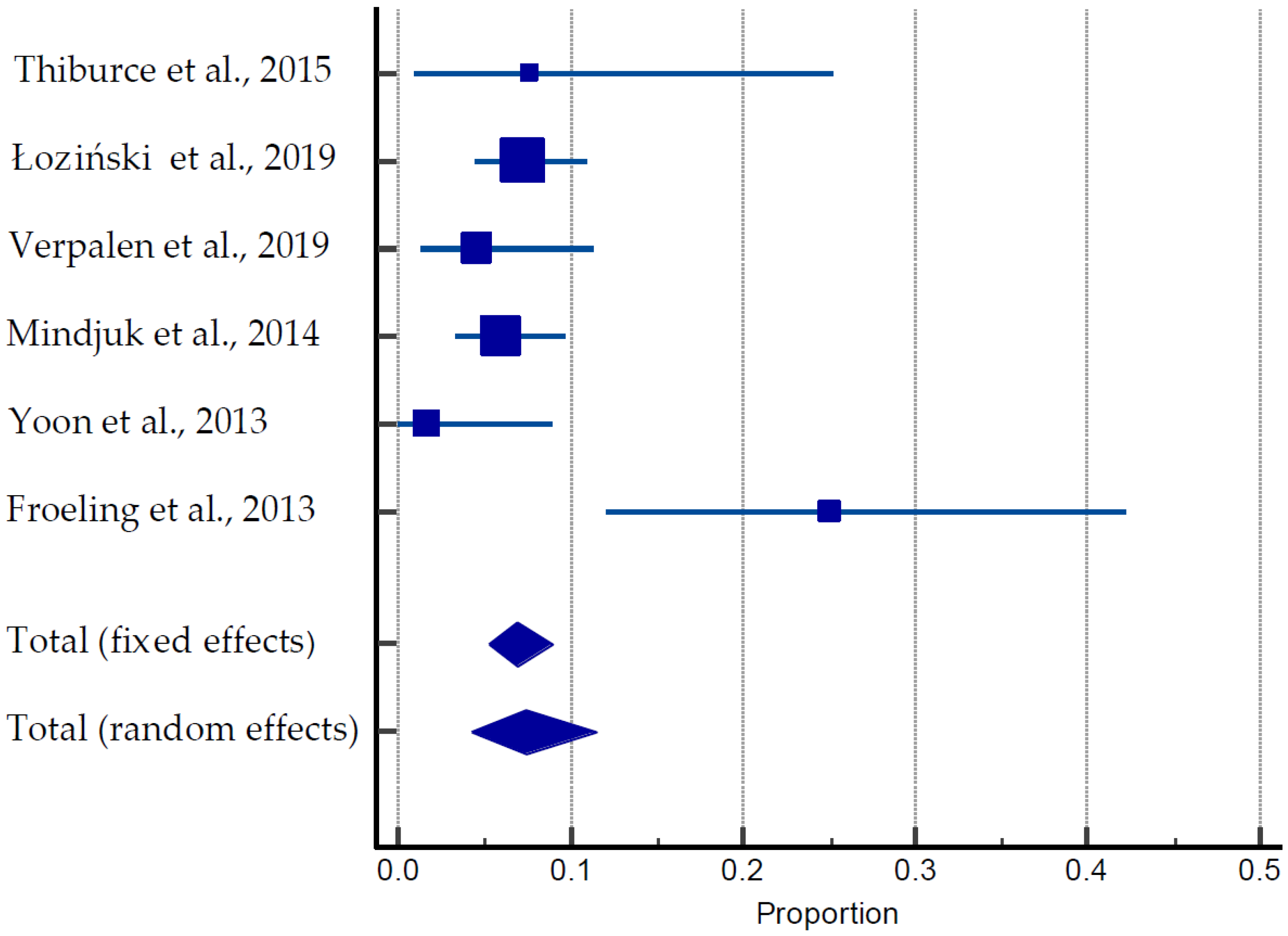
3.3.3. MRI-Guided HIFU
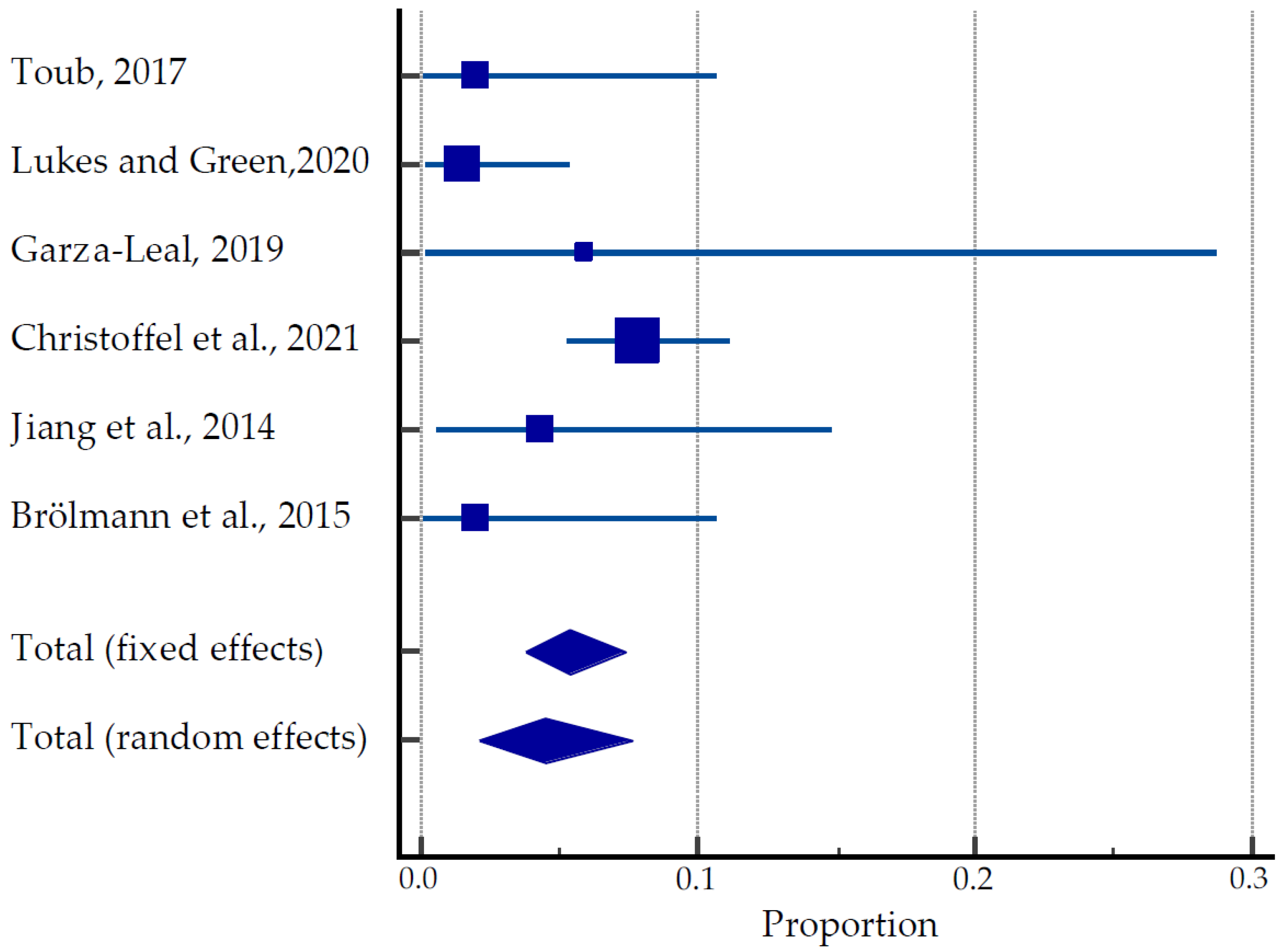
3.3.4. Transcervical Radiofrequency Ablation Systems
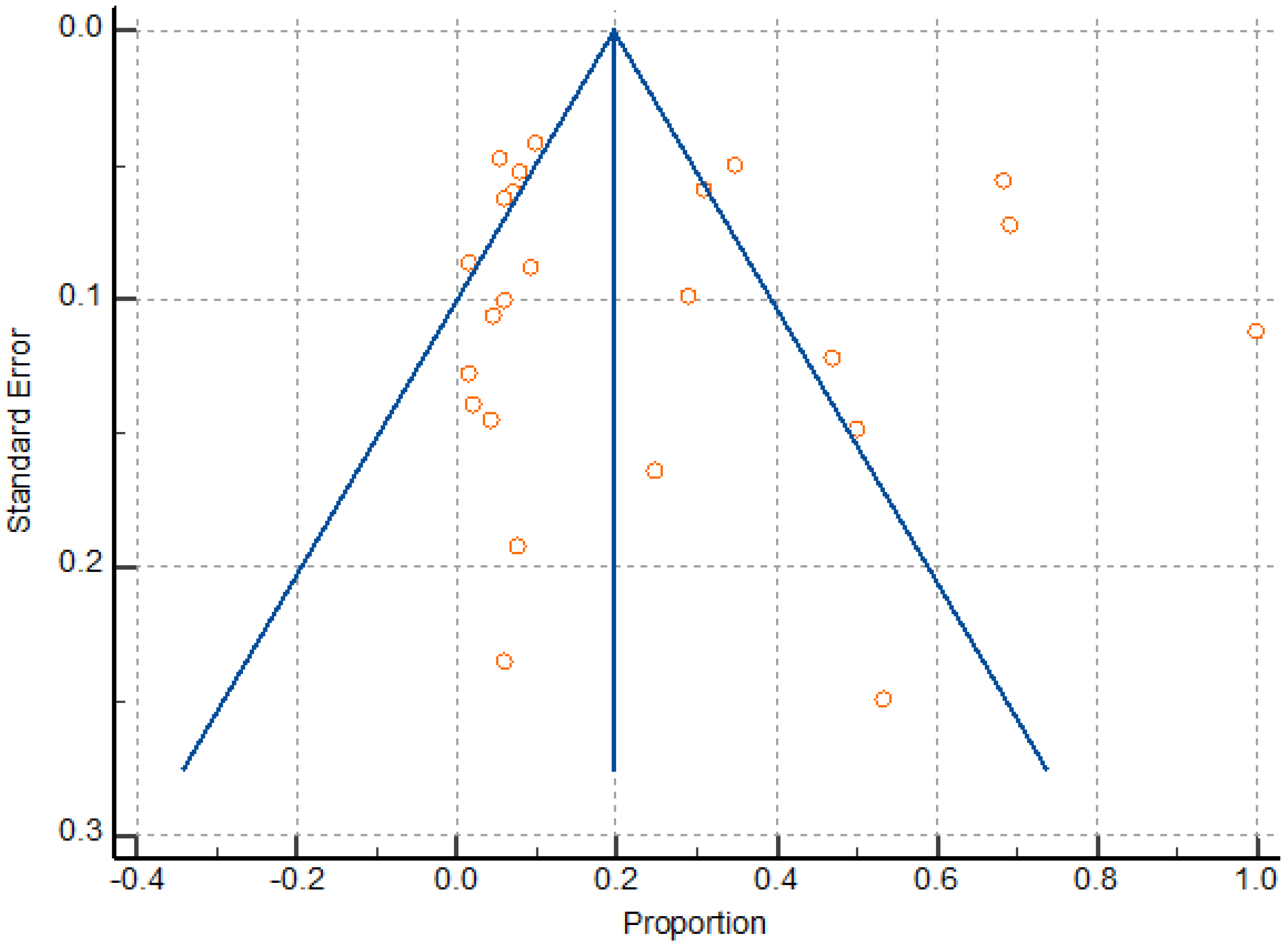
3.4. Meta Analysis
4. Discussion
4.1. Main Findings and Comparison with the Existing Literature
4.2. Study Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McWilliams, M.M.; Chennathukuzhi, V.M. Recent Advances in Uterine Fibroid Etiology. Semin. Reprod. Med. 2017, 35, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Pavone, D.; Clemenza, S.; Sorbi, F.; Fambrini, M.; Petraglia, F. Epidemiology and Risk Factors of Uterine Fibroids. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 46, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Stewart, E.A.; Cookson, C.L.; Gandolfo, R.A.; Schulze-Rath, R. Epidemiology of uterine fibroids: A systematic review. BJOG 2017, 124, 1501–1512. [Google Scholar] [CrossRef] [PubMed]
- Ryan, G.L.; Syrop, C.H.; Van Voorhis, B.J. Role, epidemiology, and natural history of benign uterine mass lesions. Clin. Obstet. Gynecol. 2005, 48, 312–324. [Google Scholar] [CrossRef]
- Al-Hendy, A.; Myers, E.R.; Stewart, E. Uterine Fibroids: Burden and Unmet Medical Need. Semin. Reprod. Med. 2017, 35, 473–480. [Google Scholar] [CrossRef]
- Sparic, R.; Terzic, M.; Malvasi, A.; Tinelli, A. Uterine fibroids—Clinical presentation and complications. ACI 2015, 51, 41–48. [Google Scholar] [CrossRef]
- Laganà, A.S.; Vergara, D.; Favilli, A.; La Rosa, V.L.; Tinelli, A.; Gerli, S.; Noventa, M.; Vitagliano, A.; Triolo, O.; Rapisarda, A.M.C.; et al. Epigenetic and genetic landscape of uterine leiomyomas: A current view over a common gynecological disease. Arch. Gynecol. Obstet. 2017, 296, 855–867. [Google Scholar] [CrossRef]
- Yerezhepbayeva, M.; Terzic, M.; Aimagambetova, A.; Crape, B. Comparison of two invasive non-surgical treatment options for uterine myomas: Uterine artery embolization and magnetic resonance guided high intensity focused ultrasound—Systematic review. BMC Women’s Health 2022, 22, 55. [Google Scholar] [CrossRef]
- Pérez-Roncero, G.R.; López-Baena, M.T.; Ornat, L.; Cuerva, M.J.; Garcia-Casarrubios, P.; Chedraui, P.; Pérez-López, F.R. Uterine fibroids and preterm birth risk: A systematic review and meta-analysis. J. Obstet. Gynaecol. Res. 2020, 46, 1711–1727. [Google Scholar] [CrossRef]
- Coutinho, L.M.; Assis, W.A.; Spagnuolo-Souza, A.; Reis, F.M. Uterine Fibroids and Pregnancy: How Do They Affect Each Other? Reprod. Sci. 2021, 29, 2145–2151. [Google Scholar] [CrossRef]
- Laganà, A.S.; Alonso Pacheco, L.; Tinelli, A.; Haimovich, S.; Carugno, J.; Ghezzi, F.; Mazzon, I.; Bettocchi, S. Management of Asymptomatic Submucous Myomas in Women of Reproductive Age: A Consensus Statement from the Global Congress on Hysteroscopy Scientific Committee. J. Minim. Invasive Gynecol. 2019, 26, 381–383. [Google Scholar] [CrossRef]
- Zepiridis, L.I.; Grimbizis, G.F.; Tarlatzis, B.C. Infertility and uterine fibroids. Best Pract. Res. Clin. Obstet. Gynaecol. 2016, 34, 66–73. [Google Scholar] [CrossRef]
- Tanvir, T.; Garzon, S.; Alonso Pacheco, L.; Lopez Yarto, M.; Rios, M.; Stamenov, G.; Moratalla, E.; Shokeir, T.; Adel, S.; Mikulasek, L.; et al. Office hysteroscopic myomectomy without myoma extraction: A multicenter prospective study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 256, 358–363. [Google Scholar] [CrossRef]
- Terzic, M. Focused ultrasound for treatment of uterine myoma: From experimental model to clinical practice. Srp. Arh. Celok. Lek. 2008, 136, 193–195. [Google Scholar] [CrossRef]
- Terzic, M.; Maricic, S.; Dotlic, J. Vaginal Removal of Very Large Nascent Uterine Myoma—Case Report and Literature Review. Geburtsh. Frauenheilk. 2013, 73, 724–726. [Google Scholar] [CrossRef]
- Dedden, S.J.; Geomini, P.M.A.J.; Huirne, J.A.F.; Bongers, M.Y. Vaginal and Laparoscopic hysterectomy as an outpatient procedure: A systematic review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 216, 212–223. [Google Scholar] [CrossRef]
- Khaw, S.C.; Anderson, R.A.; Lui, M.-W. Systematic Review of Pregnancy Outcomes after Fertility-Preserving Treatment of Uterine Fibroids. Reprod. BioMed. Online 2020, 40, 429–444. [Google Scholar] [CrossRef]
- Parazzini, F.; Tozzi, L.; Bianchi, S. Pregnancy outcome and uterine fibroids. Best Pract. Res. Clin. Obstet. Gynaecol. 2016, 34, 74–84. [Google Scholar] [CrossRef]
- Laganà, A.S.; Garzon, S.; Dababou, S.; Uccella, S.; Medvediev, M.; Pokrovenko, D.; Babunashvili, E.L.; Buyanova, S.N.; Schukina, N.A.; Kaschchuk, M.G.S.; et al. Prevalence of Intrauterine Adhesions after Myomectomy: A Prospective Multicenter Observational Study. Gynecol. Obstet. Invest. 2022, 87, 62–69. [Google Scholar] [CrossRef]
- Borah, B.J.; Nicholson, W.K.; Bradley, L.; Stewart, E.A. The impact of uterine leiomyomas: A national survey of affected women. Am. J. Obstet. Gynecol. 2013, 209, 319.e1. [Google Scholar] [CrossRef]
- Miller, C.E.; Osman, K.M. Transcervical Radiofrequency Ablation of Symptomatic Uterine Fibroids: 2-Year Results of the SONATA Pivotal Trial. J. Gynecol. Surg. 2019, 35, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Arnreiter, C.; Oppelt, P. A Systematic Review of the Treatment of Uterine Myomas Using Transcervical Ultrasound-Guided Radiofrequency Ablation with the Sonata System. J. Minim. Invasive. Gynecol. 2021, 28, 1462–1469. [Google Scholar] [CrossRef] [PubMed]
- Römer, T.; Bends, R.; Christoffel, L.; Felberbaum, R.; Hildebrandt, T.; Meinhold-Heerlein, I.; Mueller, M.; Oppelt, P.; Renner, S.P.; Runnebaum, I.B.; et al. The significance of transcervical ultrasound-guided radiofrequency ablation in the treatment of symptomatic fibroids: Results of an expert consensus from German-speaking countries. Arch. Gynecol. Obstet. 2022, 306, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Ukybassova, T.; Terzic, M.; Dotlic, J.; Imankulova, B.; Terzic, S.; Shauyen, F.; Garzon, S.; Guo, L.; Sui, L. Evaluation of Uterine Artery Embolization on Myoma Shrinkage: Results from a Large Cohort Analysis. Gynecol. Minim. Invasive. Ther. 2019, 8, 165–171. [Google Scholar] [CrossRef]
- Baumgarten, M.N.; Polanski, L.T. Modern Management of Fibroids. Obstet. Gynaecol. Reprod. Med. 2020, 30, 104–108. [Google Scholar] [CrossRef]
- Torre, A.; Fauconnier, A.; Kahn, V.; Limot, O.; Bussierres, L.; Pelage, J.P. Fertility after uterine artery embolization for symptomatic multiple fibroids with no other infertility factors. Eur. Radiol. 2017, 27, 2850–2859. [Google Scholar] [CrossRef]
- Łoziński, T.; Filipowska, J.; Gurynowicz, G.; Zgliczyńska, M.; Kluz, T.; Jędra, R.; Skowyra, A.; Ciebiera, M. The effect of high-intensity focused ultrasound guided by magnetic resonance therapy on obstetrical outcomes in patients with uterine fibroids—Experiences from the main Polish center and a review of current data. Int. J. Hyperth. 2019, 36, 582–590. [Google Scholar] [CrossRef]
- Wu, G.; Li, R.; He, M.; Pu, Y.; Wang, J.; Chen, J.; Qi, H. A comparison of the pregnancy outcomes between ultrasound-guided high-intensity focused ultrasound ablation and laparoscopic myomectomy for uterine fibroids: A comparative study. Int. J. Hyperth. 2020, 37, 617–623. [Google Scholar] [CrossRef]
- Recker, F.; Thudium, M.; Strunk, H.; Tonguc, T.; Dohmen, S.; Luechters, G.; Bette, B.; Welz, S.; Salam, B.; Wilhelm, K.; et al. Multidisciplinary management to optimize outcome of ultrasound-guided high-intensity focused ultrasound (HIFU) in patients with uterine fibroids. Sci. Rep. 2021, 11, 22768. [Google Scholar] [CrossRef]
- Jeng, C.J.; Ou, K.Y.; Long, C.Y.; Chuang, L.; Ker, C.R. 500 Cases of High-intensity Focused Ultrasound (HIFU) Ablated Uterine Fibroids and Adenomyosis. Taiwan J. Obstet. Gynecol. 2020, 59, 865–871. [Google Scholar] [CrossRef]
- Christoffel, L.; Römer, T.; Schiermeier, S. Transcervical Radiofrequency Ablation of Uterine Fibroids Global Registry (SAGE): Study Protocol and Preliminary Results. Med. Devices 2021, 14, 77–84. [Google Scholar] [CrossRef]
- Polin, M.; Hur, H.C. Radiofrequency Ablation of Uterine Myomas and Pregnancy Outcomes: An Updated Review of the Literature. J. Minim. Invasive. Gynecol. 2021, ume 14, 77–84. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLoS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef]
- Higgins, J.; Altman, D.; Sterne, J. Chapter 8: Assessing Risk of Bias in Included Studies. In Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (Updated March 2011); The Cochrane Collaboration: London, UK, 2011; Available online: www.training.cochrane.org/handbook (accessed on 4 July 2022).
- Schaap, T.; Bloemenkamp, K.; Deneux-Tharaux, C.; Knight, M.; Langhoff-Roos, J.; Sullivan, E.; Akker, T.V.D. Defining definitions: A Delphi study to develop a core outcome set for conditions of severe maternal morbidity. BJOG 2019, 126, 394–401. [Google Scholar] [CrossRef]
- Wells, G.; Shea, S.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: https://www.ohri.ca//programs/clinical_epidemiology/oxford.asp (accessed on 29 June 2022).
- Torre, A.; Paillusson, B.; Fain, V.; Labauge, P.; Pelage, J.P.; Fauconnier, A. Uterine artery embolization for severe symptomatic fibroids: Effects on fertility and symptoms. Hum. Reprod. 2014, 29, 490–501. [Google Scholar] [CrossRef]
- McLucas, B. Pregnancy following uterine artery embolization: An update. Minim. Invasive. Ther. Allied. Technol. 2013, 22, 39–44. [Google Scholar] [CrossRef]
- Mara, M.; Kubinova, K.; Maskova, J.; Horak, P.; Belsan, T.; Kuzel, D. Uterine artery embolization versus laparoscopic uterine artery occlusion: The outcomes of a prospective, nonrandomized clinical trial. Cardiovasc. Intervent. Radiol. 2012, 35, 1041–1052. [Google Scholar] [CrossRef]
- Daniels, J.; Middleton, L.J.; Cheed, V.; McKinnon, W.; Sirkeci, F.; Manyonda, I.; Belli, A.-M.; Lumsden, M.A.; Moss, J.; Wu, O.; et al. Uterine artery embolization or myomectomy for women with uterine fibroids: Four-year follow-up of a randomised controlled trial. Eur. J. Obstet. Gynecol. Reprod. Biol. X 2021, 13, 100139. [Google Scholar] [CrossRef]
- Redecha, M., Jr.; Mižičková, M.; Javorka, V.; Redecha, M.S.; Kurimská, S.; Holomáň, K. Pregnancy after uterine artery embolization for the treatment of myomas: A case series. Arch. Gynecol. Obstet. 2013, 287, 71–76. [Google Scholar] [CrossRef]
- Zou, M.; Chen, L.; Wu, C.; Hu, C.; Xiong, Y. Pregnancy outcomes in patients with uterine fibroids treated with ultrasound-guided high-intensity focused ultrasound. BJOG 2017, 124, 30–35. [Google Scholar] [CrossRef]
- Rodríguez, J.; Isern, J.; Pons, N.; Carmona, A.; Vallejo, E.; Cassadó, J.; De Marcos, J.A.; Paraira, M.; Giménez, N.; Pessarrodona, A. Pregnancy outcomes after ultrasound-guided high-intensity focused ultrasound (USgHIFU) for conservative treatment of uterine fibroids: Experience of a single institution. Int. J. Hyperth. 2021, 38, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Qin, J.; Chen, J.Y.; Zhao, W.P.; Hu, L.; Chen, W.Z.; Wang, Z.B. Outcome of unintended pregnancy after ultrasound-guided high-intensity focused ultrasound ablation of uterine fibroids. Int. J. Gynaecol. Obstet. 2012, 117, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Xue, L.; Wang, Y.; Wang, W.; Tang, J. Vaginal delivery outcomes of pregnancies following ultrasound-guided high-intensity focused ultrasound ablation treatment for uterine fibroids. Int. J. Hyperth. 2018, 35, 510–517. [Google Scholar] [CrossRef] [PubMed]
- Li, J.S.; Wang, Y.; Chen, J.Y.; Chen, W.Z. Pregnancy outcomes in nulliparous women after ultrasound ablation of uterine fibroids: A single-central retrospective study. Sci. Rep. 2017, 7, 3977. [Google Scholar] [CrossRef]
- Thiburce, A.C.; Frulio, N.; Hocquelet, A.; Maire, F.; Salut, C.; Balageas, P.; Bouzgarrou, M.; Hocké, C.; Trillaud, H. Magnetic resonance-guided high-intensity focused ultrasound for uterine fibroids: Mid-term outcomes of 36 patients treated with the Sonalleve system. Int. J. Hyperth. 2015, 31, 764–770. [Google Scholar] [CrossRef]
- Froeling, V.; Meckelburg, K.; Schreiter, N.F.; Scheurig-Muenkler, C.; Kamp, J.; Maurer, M.; Beck, A.; Hamm, B.; Kroencke, T. Outcome of uterine artery embolization versus MR-guided high-intensity focused ultrasound treatment for uterine fibroids: Long-term results. Eur. J. Radiol. 2013, 82, 2265–2269. [Google Scholar] [CrossRef]
- Toub, D.B. A New Paradigm for Uterine Fibroid Treatment: Transcervical, Intrauterine Sonography-Guided Radiofrequency Ablation of Uterine Fibroids with the Sonata System. Curr. Obstet. Gynecol. Rep. 2017, 6, 67–73. [Google Scholar] [CrossRef]
- Lukes, A.S.; Green, M. Three-Year Results of the Sonata Pivotal Trial of Transcervical Fibroid Ablation (TFA) for Symptomatic Uterine Myomata. J. Minim. Invasive Gynecol. 2020, 27, S48. [Google Scholar] [CrossRef]
- Garza-Leal, J.G. Long-Term Clinical Outcomes of Transcervical Radiofrequency Ablation of Uterine Fibroids: The VITALITY Study. J Gynecol. Surg. 2019, 35, 19–23. [Google Scholar] [CrossRef]
- Jiang, X.; Thapa, A.; Lu, J.; Bhujohory, V.S.; Liu, Y.; Qiao, S. Ultrasound-guided transvaginal radiofrequency myolysis for symptomatic uterine myomas. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 177, 38–43. [Google Scholar] [CrossRef]
- Brölmann, H.; Bongers, M.; Garza-Leal, J.G.; Gupta, J.K.; Veersema, S.; Quartero, R.W.P.; Toub, D. The FAST-EU trial: 12-month clinical outcomes of women after intrauterine sonography-guided transcervical radiofrequency ablation of uterine fibroids. Gynecol. Surg. 2016, 13, 27–35. [Google Scholar] [CrossRef]
- Serres-Cousine, O.; Kuijper, F.M.; Curis, E.; Atashroo, D. Clinical investigation of fertility after uterine artery embolization. Am. J. Obstet. Gynecol. 2021, 225, e1–e403. [Google Scholar] [CrossRef]
- Verpalen, I.M.; de Boer, J.P.; Linstra, M.; Pol, R.L.I.; Nijholt, I.M.; Moonen, C.T.W.; Bartels, L.W.; Franx, A.; Boomsma, M.F.; Braat, M.N.G. The Focused Ultrasound Myoma Outcome Study (FUMOS); a retrospective cohort study on long-term outcomes of MR-HIFU therapy. Eur. Radiol. 2020, 30, 2473–2482. [Google Scholar] [CrossRef]
- Mindjuk, I.; Trumm, C.G.; Herzog, P.; Stahl, R.; Matzko, M. MRI predictors of clinical success in MR-guided focused ultrasound (MRgFUS) treatments of uterine fibroids: Results from a single centre. Eur. Radiol. 2015, 25, 1317–1328. [Google Scholar] [CrossRef]
- Yoon, S.W.; Cha, S.H.; Ji, Y.G.; Kim, H.C.; Lee, M.H.; Cho, J.H. Magnetic resonance imaging-guided focused ultrasound surgery for symptomatic uterine fibroids: Estimation of treatment efficacy using thermal dose calculations. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 169, 304–308. [Google Scholar] [CrossRef]
- Cavazos-Rehg, P.A.; Krauss, M.J.; Spitznagel, E.L.; Bommarito, K.; Madden, T.; Olsen, M.A.; Subramaniam, H.; Peipert, J.F.; Bierut, L.J. Maternal age and risk of labor and delivery complications. Matern Child Health J. 2015, 19, 1202–1211. [Google Scholar] [CrossRef]
- Ciancimino, L.; Laganà, A.S.; Chiofalo, B.; Granese, R.; Grasso, R.; Triolo, O. Would it be too late? A retrospective case-control analysis to evaluate maternal-fetal outcomes in advanced maternal age. Arch. Gynecol. Obstet. 2014, 290, 1109–1114. [Google Scholar] [CrossRef]
- Cho, H. Rupture of a myomectomy site in the third trimester of pregnancy after myomectomy, septoplasty and cesarean section: A case report. Case Rep. Womens Health. 2018, 19, e00066. [Google Scholar] [CrossRef]
- Tinelli, A.; Kosmas, I.P.; Carugno, J.T.; Carp, H.; Malvasi, A.; Cohen, S.B.; Laganà, A.S.; Angelini, M.; Casadio, P.; Chayo, J.; et al. Uterine rupture during pregnancy: The URIDA (uterine rupture international data acquisition) study. Int. J. Gynaecol. Obstet. 2022, 157, 76–84. [Google Scholar] [CrossRef]
- Jansa, V.; Laganà, A.S.; Ferrari, F.; Ghezzi, F.; Papler, T.B.; Bokal, E.V.; Frangež, H.B. Uterine rupture in pregnancy after hysteroscopic septum resection: A 20-year retrospective analysis. Minim. Invasive. Ther. Allied. Technol. 2022, 31, 448–455. [Google Scholar] [CrossRef]
- Liu, L.; Wang, T.; Lei, B. Uterine Artery Embolization Compared with High-intensity Focused Ultrasound Ablation for the Treatment of Symptomatic Uterine Myomas: A Systematic Review and Meta-analysis. J. Minim. Invasive. Gynecol. 2021, 28, 218–227. [Google Scholar] [CrossRef] [PubMed]

| Study, Year | Study Design | Mean Age, Years | Total Number of Women, (N) | Number of Pregnant Women, (N) | Pregnancies, (N) | Pregnancy Outcomes (N) | IVF | Time to Conception, (Months) | Mode of Delivery, (N) | Birth Weight, (g) | Complications, (N) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Live Birth, (N) | Ongoing Pregnancies, (N) | Miscarriages, (N) | Gestational Age at Delivery, (Weeks) | |||||||||||
| Torre et al., 2017 [26] | Prospective non-comparative open-label trial | 34.8 ± 4.8 | 15 | 8 | 12 | 10 | 1 | 1 | 38.0 ± 3.0 | 3 | 27.8 | VD—6/10 CS—4/10 | 2857 | Moderately low birth weight (i.e., slightly below the 10th percentile)—1 |
| Torre et al., 2014 [37] | Prospective cohort study | 37.3 ± 3.9 | 66 | 31 | 1 | 0 | 0 | 1 | - | 5 | 28.9 ± 16.2 | - | - | Not reported |
| McLucas, 2013 [38] | Retrospective chart review | 33.4 | 44 | 22 | 28 | 21 | 1 | 3 | 36.8 | 1 | 41 | VD—6 CS—17 | 2523 | Borderline oligohydramnios—1 Low-lying placenta—1 |
| Mara et al., 2012 [39] | Prospective, parallel-group, nonrandomized study | 33.1 ± 3.7 | 100 | 29 | 42 | 23 | 2 | 13 (abortions spontaneous or missed) | 38.1 ± 1.6 | 4 | 26.7 ± 14.5/7–52 | VD—5 CS—18 (78.3%) Pregnancy terminations—2 | 3270 ± 451 | Preterm birth—1 IUGR—3 Preeclampsia—1 Placenta accreta—1 |
| Daniels et al., 2021 [40] | Randomized, open, parallel multi-center trial | 40.2 ± 6.5 | 127 | 12 | 12 | 7 | 0 | 4 | - | - | - | Pregnancy terminations—1 | - | - |
| Redecha et al., 2012 [41] | Prospective case series | 38.7 | 98 | 6 | 7 | 7 | 0 | 0 | 39.0 ± 1.4 | - | 13.14 | VD—6 CS—1 | 3338.57 | PROM—2 |
| Serres-Cousine et al., 2021 [54] | Retrospective cohort study | 37.13 ± 4.87 | 398 | 139 | 148 | 109 | - | 26 | - | 11 | 24.82 + 24 | VD—58/109 (53.2%) CS—51/109 (46,8%) | 3209 g ± 574.9 | GDM—2 Gestational hypertension—1 Threats of preterm birth—4 Extra-uterine pregnancy—1 Craniofacial abnormalities—1 Placenta previa—1 Fibroid previa—1 “Hard-to-detach” placenta—1 Intrauterine fetal deaths—2 |
| Study, Year | Study Design | Mean age, Years | Total Number of Women, (N) | Number of Pregnant Women, (N) | Pregnancies, (N) | Pregnancy Outcomes | IVF | Time to Conception (Months) | Mode of Delivery, (N) | Birth Weight, (g) | Complications (N) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Live Birth, (N) | Ongoing Pregnancies, (N) | Miscarriages, (N) | Gestational Age at Delivery, (Weeks) | |||||||||||
| Wu et al., 2020 [28] | Retrospective observational study | 31.6 | 320 | 219 | 248 | 178 | 6 | 12 | - | 21 | 13.6 ± 9.5 | VD—91 (51.1%) CS—74 (41.6%) Forceps—13 Pregnancy terminations—21 | - | Preterm birth—16 Hypertensive disorder—13 IHCP—6 GDM—15 Fetal distress—5 IUGR—4 Fetal macrosomia—14 Placental disorders—11 Abnormal AFV—6 Umbilical cord anomaly—3 Uterine rupture—1 Postpartum infection—1 Postpartum hemorrhage—8 |
| Zou et al., 2017 [42] | Retrospective observational study | 37.3 ± 3.9 | 78 | 78 | 80 | 71 | 5 | 3 | 38.1 ± 2.2 | 4 | 5.6 ± 2.7 | VD—15 (19.2%) CS—56 (80.8%) (PROM—1 fetal distress—2 CPD—2, oligohydramnios—1) Termination —1 | - | Preterm birth—3 PROM—1 Fetal distress—2 Breech presentation—1 CPD—2 Oligohydramnios—1 Neonatal asphyxia—2 |
| Rodríguez et al., 2021 [43] | Retrospective observational study | 35 ± 4 | 560 | 55 | 71 | 43 | 26 | 39 ± 2 | 8 | 12 | VD—25 (57%) CS—19 (43%) with indications: Malpresentation—5 CPD—1 IUGR—1 Placenta previa—2 Fetal distress—1 Previous myomectomies—1 Failed labor induction—4 Fetal bradycardia—4 “Advice of obstetrician”—2 Renal colic—1 | 3100 ± 600 (1.4–4.3) | Preterm birth—4 SGA—2 Congenital malformations—2 PROM—2 Polyhydramnios—1 Retained placenta with manual removal—3 Severe preeclampsia—1 | |
| Qin et al., 2012 [44] | Retrospective observational study | 34.5 ± 4.5 | 435 | 24 | 24 | 7 | 0 | 2 | 39 | - | 20 ± 8.85 (for live births only) | CS—7 Pregnancy termination—14 | 3085.71 ± 459.81 | No data |
| Liu et al., 2018 [45] | Prospective observational study | 31.1 ± 3.8 | 284 | 88 | 81 | 74 | - | 9 | 38 | 5 | 16 | VD—21 CS—53 Pregnancy terminations—5 | Preterm birth—5 Fetal macrosomia—5 Fetal malpresentation—4 Placenta previa—1 IUGR—1 | |
| Li et al., 2017 [46] | Single-center retrospective study | 31.4 ± 4.3 | 189 | 131 | 131 | 94 | 19 | 17 | - | 6 | 12.3 ± 9.9 | VD—26 CS—67 Pregnancy terminations—4 | 3300 ± 0.4 | Placenta previa—5 Placental insufficient—1 IHCP—1 Ovarian cysts—1 PROM—1 Fetal distress—1 Hemorrhoea due to central placenta—1 |
| Study, Year | Study Design | Mean Age, Years | Total Number of Women, (N) | Number of Pregnant Women, (N) | Pregnancies, (N) | Pregnancy Outcomes | IVF, (N) | Time to Conception | Mode of Delivery, (N) | Complications, (N) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Live Birth, (N) | Ongoing Pregnancies, (N) | Miscarriages, (N) | Gestational Age at Delivery, (Weeks) | ||||||||||
| Łoziński et al., 2019 [27] | Single-center retrospective cohort study | 33.2 ± 3.65 | 276 | 20 | 21 | 11 | 7 | 3 | 38.8 | 0 | - | CS—7, VD—4 | - |
| Thiburce et al., 2015 [47] | Single-center retrospective case series | 43.5 | 36 | 2 | 2 | 2 | 0 | 0 | - | - | 2.5 years | VD—2 | - |
| Froeling et al., 2013 [48] | Retrospective analysis | 36 | 36 | 9 | 10 | 7 | 0 | 3 | - | - | 16.1 months | NA | |
| Verpalen et al., 2019 [55] | Retrospective cohort study | 44.6 ± 4.7 | 87 | 4 | 9 | 7 | 0 | 2 | - | - | CS—3, VD—2 | CPD—1 Postpartum hemorrhage—2 | |
| Mindjuk et al., 2014 [56] | Retrospective cohort study |
42.1 ± 6.9 35.3 ± 3.4 | 252 | 15 | 15 | 12 | 2 | 1 | - | - | 19.7 months | - | - |
| Yoon et al., 2013 [57] | Retrospective analysis | 41.3 ± 6.3 | 60 | 1 | 1 | 1 | 0 | 0 | Term | - | 4 months | - | NA |
| Study, Year | Study Design | Mean Age, Years | Total Number of Women, (N) | Number of Pregnant Women, (N) | Pregnancies | Pregnancy Outcomes | IVF, (N) | Time to Conception, (Months) | Mode of Delivery, (N) | Complications, (N) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Live Birth, (N) | Ongoing Pregnancies, (N) | Miscarriages, (N) | Gestational Age at Delivery, (Weeks) | ||||||||||
| Christoffel et al., 2021 [31] | Retrospective study | 35.6 + 5.0 | 357 | 28 | 36 | 20 | 5 | 8 | >37 weeks, except one at 35 6/7 | 4 | NA | VD—8, CS—12, Terminations—3 | HELLP syndrome—1 Fetal macrosomia—3 Preterm birth—1 |
| Toub, 2017 [49] | Prospective, multi-center trial | 37.3 ± 3.9 | 50 | 1 | 1 | 1 | 0 | 0 | - | 0 | 6 months | CS—1 | Not reported |
| Lukes and Green, 2020 [50] | Prospective, controlled, multi-center interventional trial | 43 | 132 | 2 | 2 | 1 | 0 | 1 | 38 | 30 months | CS—1 | Not reported | |
| Garza-Leal, 2019 [51] | Retrospective, single-arm, long-term data-collection study | 41–45 | 17 | 1 | 1 | 1 | 0 | 0 | Term | - | - | CS—1 | Not reported |
| Jiang et al., 2014 [52] | Clinical trial | 40.80 | 46 | 2 | 2 | 2 | NA | NA | Term | NA | 16.5 months | CS—1, VD—1 | No complications |
| Brölmann et al., 2015 [53] | Follow-up analysis of clinical trial | 41–45 years of age | 50 | 1 | 1 | 1 | NA | NA | Term | NA | 6 months | CS—1 | No complications. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akhatova, A.; Aimagambetova, G.; Bapayeva, G.; Laganà, A.S.; Chiantera, V.; Oppelt, P.; Sarria-Santamera, A.; Terzic, M. Reproductive and Obstetric Outcomes after UAE, HIFU, and TFA of Uterine Fibroids: Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 4480. https://doi.org/10.3390/ijerph20054480
Akhatova A, Aimagambetova G, Bapayeva G, Laganà AS, Chiantera V, Oppelt P, Sarria-Santamera A, Terzic M. Reproductive and Obstetric Outcomes after UAE, HIFU, and TFA of Uterine Fibroids: Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2023; 20(5):4480. https://doi.org/10.3390/ijerph20054480
Chicago/Turabian StyleAkhatova, Ayazhan, Gulzhanat Aimagambetova, Gauri Bapayeva, Antonio Simone Laganà, Vito Chiantera, Peter Oppelt, Antonio Sarria-Santamera, and Milan Terzic. 2023. "Reproductive and Obstetric Outcomes after UAE, HIFU, and TFA of Uterine Fibroids: Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 20, no. 5: 4480. https://doi.org/10.3390/ijerph20054480
APA StyleAkhatova, A., Aimagambetova, G., Bapayeva, G., Laganà, A. S., Chiantera, V., Oppelt, P., Sarria-Santamera, A., & Terzic, M. (2023). Reproductive and Obstetric Outcomes after UAE, HIFU, and TFA of Uterine Fibroids: Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 20(5), 4480. https://doi.org/10.3390/ijerph20054480