Bracket Bond Failures: Incidence and Association with Different Risk Factors—A Retrospective Study
Abstract
1. Background
2. Materials and Methods
2.1. Data Collection
2.2. Statistical Analysis
3. Results
3.1. Study Sample
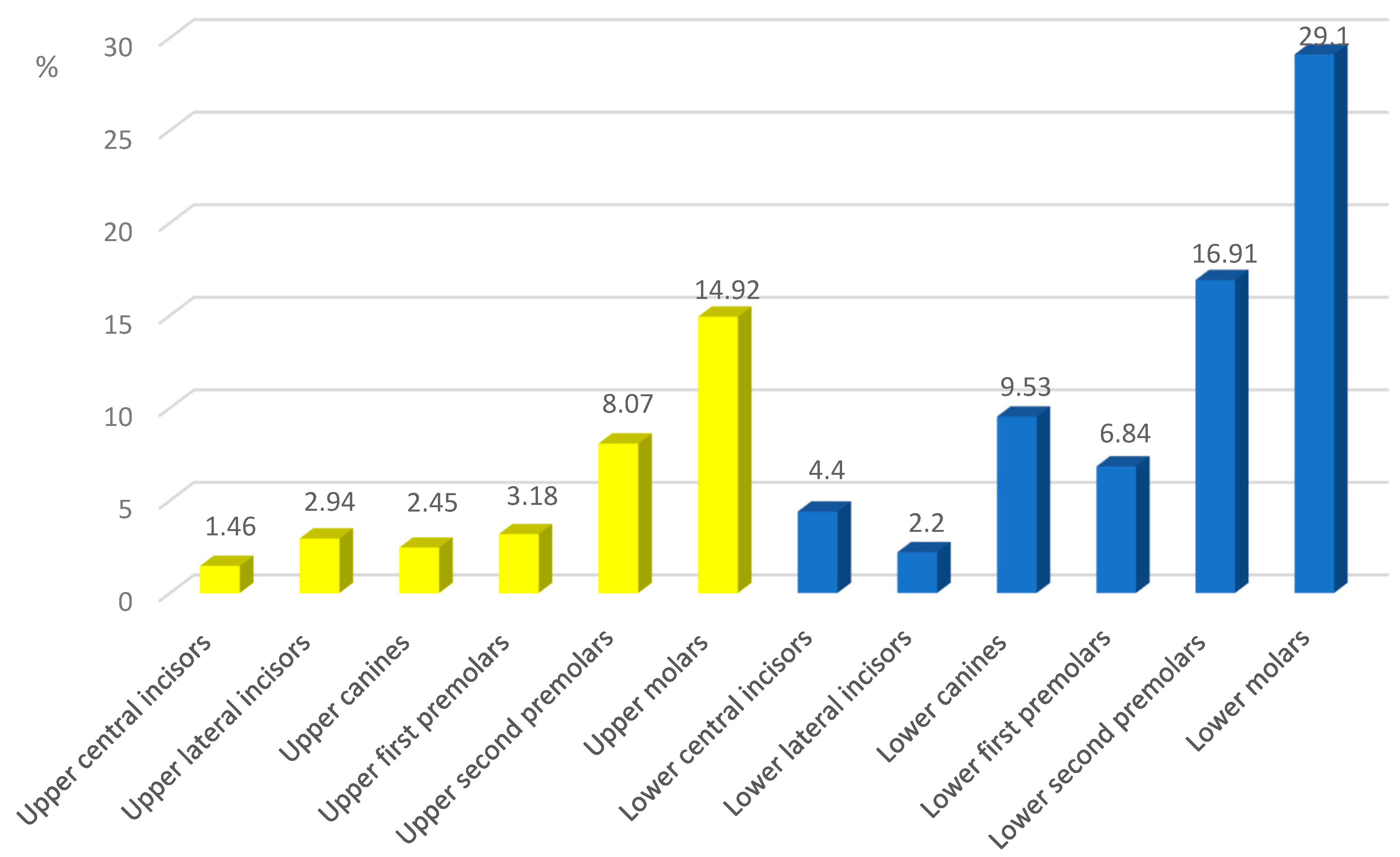
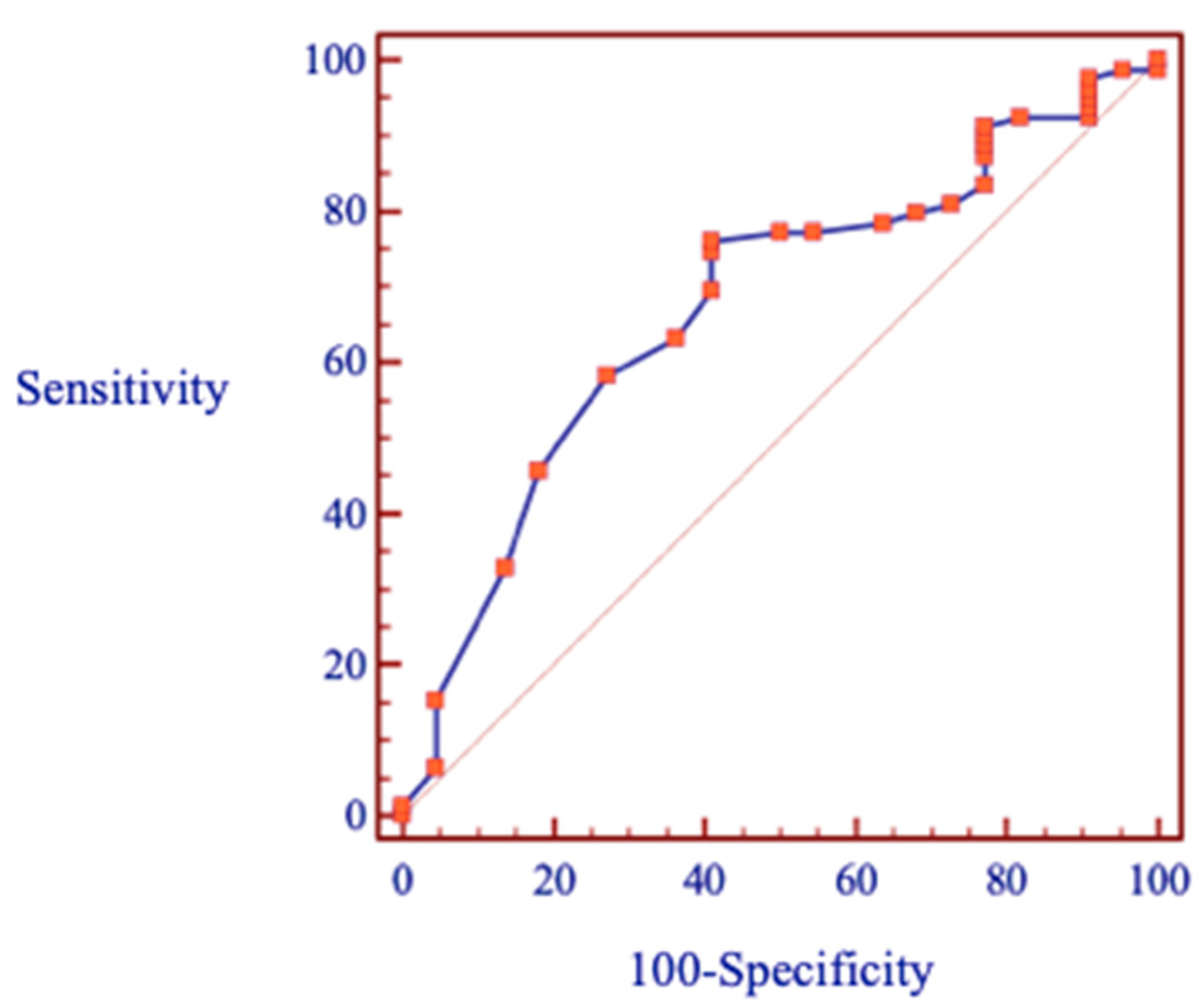
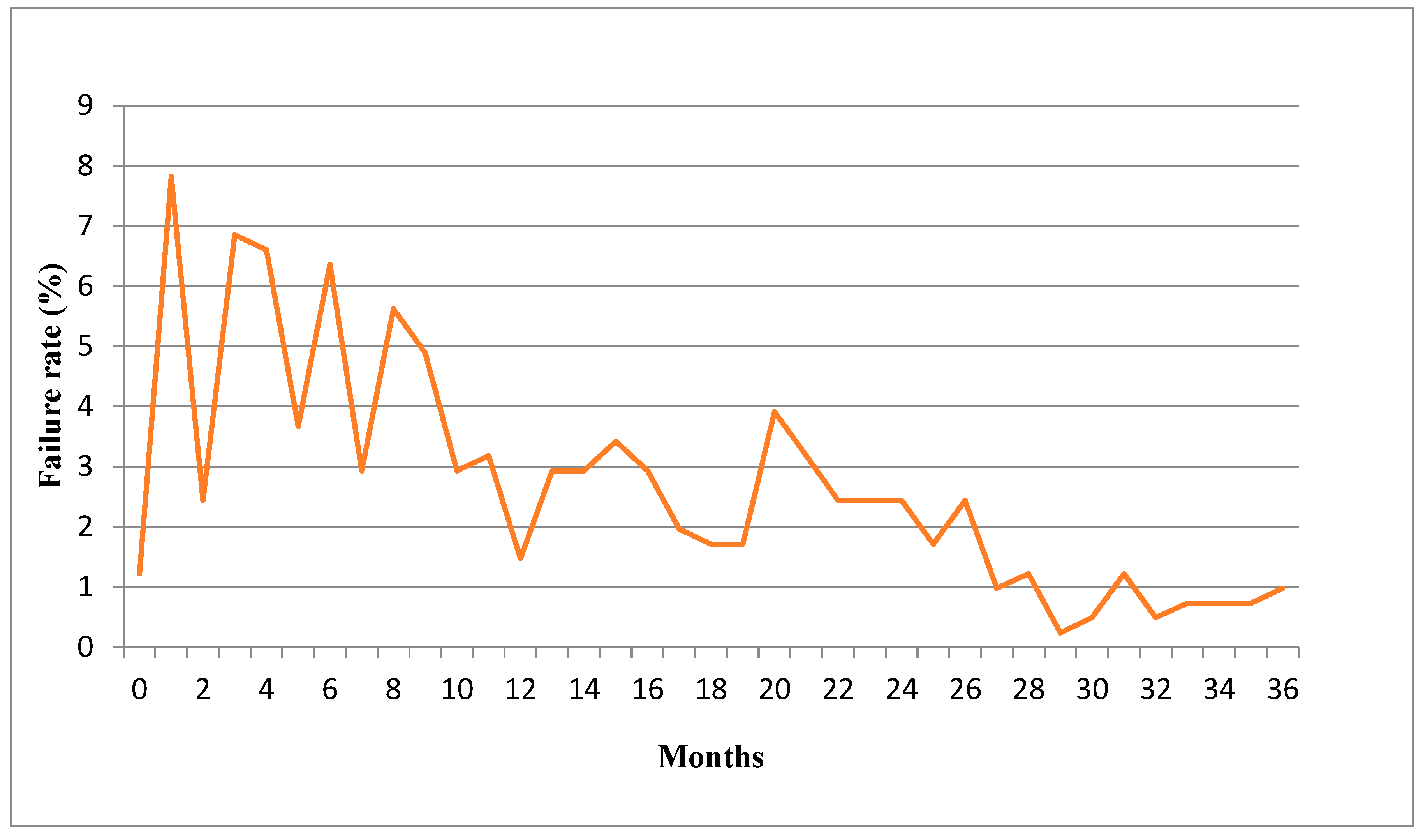
3.2. Failure Rate and Patients-Related Factors
3.3. Malocclusion-Related Factors
3.4. Treatment-Related Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Freitas, H.V.; Alves, C.M.C.; Silva, L.F.G.E.; Pereira, A.L.P.; Hugo, F.N.; Thomaz, E.B.A.F. Alterations of oral functions and dental malocclusions in adolescents: A cross-sectional population-based study. Cien. Saude Colet. 2021, 26, 5261–5272. [Google Scholar] [CrossRef] [PubMed]
- Cenzato, N.; Nobili, A.; Maspero, C. Prevalence of Dental Malocclusions in Different Geographical Areas: Scoping Review. Dent. J. 2021, 9, 117. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, G.; Vena, F.; Negri, P.; Pagano, S.; Barilotti, C.; Paglia, L.; Colombo, S.; Orso, M.; Cianetti, S. Worldwide prevalence of maloc-clusion in the different stages of dentition: A systematic review and meta-analysis. Eur. J. Paediatr. Dent. 2020, 21, 115–122. [Google Scholar] [PubMed]
- Kafle, D.; Mishra, R.K.; Hasan, M.R.; Saito, T. A Retrospective Clinical Audit of Bracket Failure among Patients Undergoing Ortho-dontic Therapy. Int. J. Dent. 2020, 2020, 8810964. [Google Scholar] [CrossRef] [PubMed]
- Bernhardt, O.; Krey, K.F.; Daboul, A.; Völzke, H.; Kindler, S.; Kocher, T.; Schwahn, C. New insights in the link between malocclusion and periodontal disease. J. Clin. Periodontol. 2019, 46, 144–159. [Google Scholar] [CrossRef]
- Macrì, M.; Murmura, G.; Scarano, A.; Festa, F. Prevalence of temporomandibular disorders and its association with malocclusion in children: A transversal study. Front. Public Health 2022, 10, 860833. [Google Scholar] [CrossRef]
- Omara, M.; Stamm, T.; Bekes, K. Four-dimensional oral health-related quality of life impact in children: A systematic review. J. Oral Rehabil. 2020, 48, 293–304. [Google Scholar] [CrossRef]
- Khan, H.; Mheissen, S.; Iqbal, A.; Jafri, A.R.; Alam, M.K. Bracket Failure in Orthodontic Patients: The Incidence and the Influence of Different Factors. BioMed Res. Int. 2022, 2022, 5128870. [Google Scholar] [CrossRef]
- Stasinopoulos, D.; Papageorgiou, S.N.; Kirsch, F.; Daratsianos, N.; Jäger, A.; Bourauel, C. Failure patterns of different bracket systems and their influence on treatment duration: A retrospective cohort study. Angle Orthod. 2018, 88, 338–347. [Google Scholar] [CrossRef]
- Romano, F.L.; Correr, A.B.; Sobrinho, L.; Magnani, M.B.; Ruellas, A.C. Clinical evaluation of the failure rates of metallic brackets. J. Appl. Oral Sci. 2012, 20, 228–234. [Google Scholar] [CrossRef]
- Campoy, M.D.; Plasencia, E.; Vicente, A.; Bravo, L.A.; Cibrian, R. Effect of saliva contamination on bracket failure with a self-etching primer: A prospective controlled clinical trial. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 679–683. [Google Scholar] [CrossRef]
- Aikins, E.A.; Ututu, C. An audit of bonding failure among orthodontic patients in a tertiary hospital in South-South Nigeria. Int. J. Orthod. Rehabil. 2017, 8, 91. [Google Scholar] [CrossRef]
- Ogiński, T.; Kawala, B.; Mikulewicz, M.; Antoszewska-Smith, J. A Clinical Comparison of Failure Rates of Metallic and Ceramic Brackets: A Twelve-Month Study. BioMed Res. Int. 2020, 2020, 9725101. [Google Scholar] [CrossRef]
- Leódido Gda, R.; Fernandes, H.O.; Tonetto, M.R.; Presoto, C.D.; Bandéca, M.C.; Firoozmand, L.M. Effect of fluoride solutions on the shear bond strength of orthodontic brackets. Braz. Dent. J. 2012, 23, 698–702. [Google Scholar] [CrossRef]
- Ayyed, A.B.; Shahba RY, A.; Saleh, M.H.; Hussain, F. A comparison of bracket failure rate between direct and indirect bonding techniques: A prospective clinical study. Al-Azhar J. Dent. Sci. 2020, 23, 79–86. [Google Scholar]
- Thiyagarajah, S.; Spary, D.J.; Rock, W.P. A clinical comparison of bracket bond failures in association with direct and indirect bonding. J. Orthod. 2006, 33, 198–204. [Google Scholar] [CrossRef]
- Costa, A.R.; Correr, A.B.; Puppin-Rontani, R.M.; Vedovello, S.A.; Valdrighi, H.C.; Correr-Sobrinho, L.; Filho, M.V. Effect of bonding material, etching time and silane on the bond strength of metallic orthodontic brackets to ceramic. Braz. Dent. J. 2012, 23, 223–227. [Google Scholar] [CrossRef]
- Dandachli, M.G. Bond Failure Rate of MBT Brackets Bonded with either Self-Etching Primer or Resin Modified Glass Ionomer vs Conventional Method—An in Vivo Study. Dent. Med. Probl. 2015, 52, 440–446. [Google Scholar] [CrossRef]
- Nimplod, P.; Tansalarak, R.; Sornsuwan, T. Effect of the different debonding strength of metal and ceramic brackets on the degree of enamel microcrack healing. Dent. Press J. Orthod. 2021, 26, e2119177. [Google Scholar] [CrossRef]
- Jung, M.-H. Survival analysis of brackets and tubes: A twelve-month assessment. Angle Orthod. 2014, 84, 1034–1040. [Google Scholar] [CrossRef]
- Sakrani, H.; Masood, S.; Alavi, F.B.; Dahar, M.; Saleem, M.K.M.; Lal, A. Frequency of Bonded Bracket Failure in Patients, Undergoing Fixed Orthodontic Treatment. J. Pak. Dent. Assoc. 2021, 30, 189–193. [Google Scholar] [CrossRef]
- Hammad, S.M.; El Banna, M.S.; Elsaka, S.E. Twelve-month Bracket Failure Rate with Amorphous Calcium Phosphate Bonding System. Eur. J. Orthod. 2012, 35, 622–627. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, S.; Pandian, S.; Rajagopal, R. Six-month bracket failure rate with a flowable composite: A split-mouth randomized controlled trial. Dent. Press J. Orthod. 2017, 22, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Naqvi, Z.A.; Shaikh, S.; Pasha, Z. Evaluation of bond failure rate of orthodontic brackets bonded with Green Gloo-two way color changes adhesive: A clinical study. Ethiop. J. Health Sci. 2019, 29, 187. [Google Scholar] [PubMed]
- Daniel, W.W. Biostatistics: A Foundation for Analysis in the Health Sciences, 7th ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 1999. [Google Scholar]
- Barnhart, E.C.; Campbell, P.M.; Noureldin, A.; Julien, K.; Buschang, P.H. The quality of etched enamel in different regions and tooth types and its significance in bonding and the development of white spot lesions. Angle Orthod. 2021, 91, 576–582. [Google Scholar] [CrossRef]
- Piancino, M.G.; Tortarolo, A.; Di Benedetto, L.; Crincoli, V.; Falla, D. Chewing Patterns and Muscular Activation in Deep Bite Malocclusion. J. Clin. Med. 2022, 11, 1702. [Google Scholar] [CrossRef]
- AL-Duliamy, M.J.A. The effect of oral hygiene status on the bond failure rate of the orthodontic bracket. J. Oral Dent. Res. 2018, 5, 2–12. [Google Scholar] [CrossRef]
- Sharma, S.; Singh, G.; Singh, A.; Tandon, P.; Nagar, A. A comparison of shear bond strength of orthodontic brackets bonded with four different orthodontic adhesives. J. Orthod. Sci. 2014, 3, 29–33. [Google Scholar] [CrossRef]
- Vaheed, N.A.; Gupta, M.; David, S.A.; Sam, G.; Ramanna, P.K.; Bhagvandas, S.C. In vitro Analysis of Shear Bond Strength and Adhesive Remnant Index of Stainless Steel Brackets with Different Adhesive Systems to Enamel. J. Contemp. Dent. Pract. 2018, 19, 1047–1051. [Google Scholar]
- Dudás, C.; Czumbel, L.M.; Kiss, S.; Gede, N.; Hegyi, P.; Mártha, K.; Varga, G. Clinical bracket failure rates between different bonding techniques: A systematic review and meta-analysis. Eur. J. Orthod. 2022, 12, cjac050. [Google Scholar] [CrossRef]
- Ozer, M.; Bayram, M.; Dincyurek, C.; Tokalak, F. Clinical bond failure rates of adhesive precoated self-ligating brackets using a self-etching primer. Angle Orthod. 2014, 84, 155–160. [Google Scholar] [CrossRef]
- Sabatini, C. Effect of phosphoric acid etching on the shear bond strength of two self-etch adhesives. J. Appl. Oral Sci. 2013, 21, 56–62. [Google Scholar] [CrossRef]
- Nandhra, S.S.; Littlewood, S.J.; Houghton, N.; Luther, F.; Prabhu, J.; Munyombwe, T.; Wood, S.R. Do we need primer for orthodontic bonding? A randomized controlled trial. Eur. J. Orthod. 2015, 37, 147–155. [Google Scholar] [CrossRef]
- Bazargani, F.; Magnuson, A.; Löthgren, H.; Kowalczyk, A. Orthodontic bonding with and without primer: A randomized controlled trial. Eur. J. Orthod. 2016, 38, 503–507. [Google Scholar] [CrossRef]
- Iijima, M.; Ito, S.; Muguruma, T.; Saito, T.; Mizoguchi, I. Bracket bond strength comparison between new unfilled experimental self-etching primer adhesive and conventional filled adhesives. Angle Orthod. 2010, 80, 1095–1099. [Google Scholar] [CrossRef]
- Reis, A.; dos Santos, J.E.; Loguercio, A.D.; de Oliveira Bauer, J.R. Eighteen-month bracket survival rate: Conventional versus self-etch adhesive. Eur. J. Orthod. 2008, 30, 94–99. [Google Scholar] [CrossRef]
- Trites, B.; Foley, T.F.; Banting, D. Bond strength comparison of 2 self-etching primers over a 3-month storage period. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 709–716. [Google Scholar] [CrossRef]
- Pandis, N.; Polychronopoulou, A.; Eliades, T. Failure rate of self-ligating and edgewise brackets bonded with conventional acid etching and a self-etching primer: A prospective in vivo study. Angle Orthod. 2006, 76, 119–122. [Google Scholar] [CrossRef]
| Variable | |
|---|---|
| Gender, n (%) | |
| Male | 28 (27.7) |
| Female | 73 (72.3) |
| Age at start of orthodontic treatment (years) | |
| Mean | 20.0 |
| ≤20 years, n (%) | 68 (67.3) |
| >20 years, n (%) | 33 (32.7) |
| Type of bracket system, n (%) | |
| MBT 0.022 Forestadent | 54 (53.5) |
| Damon Q2 | 47 (46.5) |
| Duration of orthodontic treatment (months) | |
| Mean | 30.2 (range 12–76) |
| Variable | |
|---|---|
| Angle class of molars at the start of orthodontic treatment, n (%) | |
| Class I | 49 (48.5) |
| Class II | 37 (36.6) |
| Class III | 15 (14.9) |
| Overjet, n (%) | |
| Decreased overjet | 28 (27.7) |
| Normal overjet | 32 (31.7) |
| Increased overjet | 41 (40.6) |
| Overbite, n (%) | |
| Decreased overbite | 26 (25.7) |
| Normal overbite | 36 (35.6) |
| Increased overbite | 39 (38.6) |
| Crowding mandibular arch, n (%) | |
| Mild (0–4 mm) | 45 (44.6) |
| Moderate (5–8 mm) | 22 (21.8) |
| Severe (>8 mm) | 17 (16.8) |
| Space excess | 17 (16.8) |
| Failure | Non-Failure | p | ||
|---|---|---|---|---|
| Gender, n (%) | Male | 25 (89.3) | 3 (10.7) | 0.095 |
| Female | 54 (74.0) | 19 (26.0) | ||
| Age, n (%) | ≤20 | 59 (86.8) | 9 (13.2) | 0.003 ** |
| >20 | 13 (39.4) | 20 (60.6) | ||
| Oral health, n (%) | Complicated | 14 (82.4) | 3 (17.6) | 0.065 |
| Non-complicated | 65 (77.4) | 19 (22.6) |
| Factor | Category | n | Mean Rank | df | pa | χ2 |
|---|---|---|---|---|---|---|
| Angle class | Class I | 49 | 48.02 | 2 | 0.396 | 1.851 |
| Class II | 37 | 56.16 | ||||
| Class III | 15 | 48.00 | ||||
| Overbite | Increased | 39 | 52.13 | 2 | 0.381 | 1.930 |
| Normal | 36 | 54.53 | ||||
| Decreased | 26 | 44.42 | ||||
| Overjet | Increased | 41 | 57.27 | 2 | 0.119 | 4.250 |
| Normal | 32 | 43.17 | ||||
| Decreased | 28 | 50.77 | ||||
| Crowding | Mild | 45 | 43.58 | 2 | 0.903 | 0.204 |
| Moderate | 22 | 41.59 | ||||
| Severe | 17 | 40.82 |
| Factor | Category | N | Coefficient | Odds Ratio (95% CI) | p |
|---|---|---|---|---|---|
| Angle class | Class I | 49 | – | – | 0.200 |
| Class II | 37 | 1.162 | 0.313 (0.081–1.213) | 0.093 | |
| Class III | 15 | −0.811 | 0.444 (0.075–2.619) | 0.370 | |
| Overbite | Increased | 39 | 1.434 | 4.196 (1.055–16.692) | 0.042 * |
| Average | 36 | – | – | 0.081 | |
| Decreased | 26 | −0.048 | 0.953 (0.168–5.407) | 0.957 | |
| Overjet | Increased | 41 | – | – | 0.078 |
| Average | 32 | 1.404 | 4.073 (0.811–20.453) | 0.088 | |
| Decreased | 28 | −0.732 | 0.481 (0.099–2.335) | 0.364 | |
| Crowding | Mild | 45 | 1.187 | 3.277 (0.438–24.508) | 0.248 |
| Moderate | 22 | 2.538 | 12.656 (1.388–115.442) | 0.024 * | |
| Severe | 17 | 1.539 | 4.660 (0.510–42.611) | 0.173 | |
| Space excess | 17 | – | – | 0.100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jakavičė, R.; Kubiliūtė, K.; Smailienė, D. Bracket Bond Failures: Incidence and Association with Different Risk Factors—A Retrospective Study. Int. J. Environ. Res. Public Health 2023, 20, 4452. https://doi.org/10.3390/ijerph20054452
Jakavičė R, Kubiliūtė K, Smailienė D. Bracket Bond Failures: Incidence and Association with Different Risk Factors—A Retrospective Study. International Journal of Environmental Research and Public Health. 2023; 20(5):4452. https://doi.org/10.3390/ijerph20054452
Chicago/Turabian StyleJakavičė, Reda, Kristina Kubiliūtė, and Dalia Smailienė. 2023. "Bracket Bond Failures: Incidence and Association with Different Risk Factors—A Retrospective Study" International Journal of Environmental Research and Public Health 20, no. 5: 4452. https://doi.org/10.3390/ijerph20054452
APA StyleJakavičė, R., Kubiliūtė, K., & Smailienė, D. (2023). Bracket Bond Failures: Incidence and Association with Different Risk Factors—A Retrospective Study. International Journal of Environmental Research and Public Health, 20(5), 4452. https://doi.org/10.3390/ijerph20054452






