Correlates of Social Isolation in Forensic Psychiatric Patients with Schizophrenia Spectrum Disorders: An Explorative Analysis Using Machine Learning
Abstract
1. Introduction
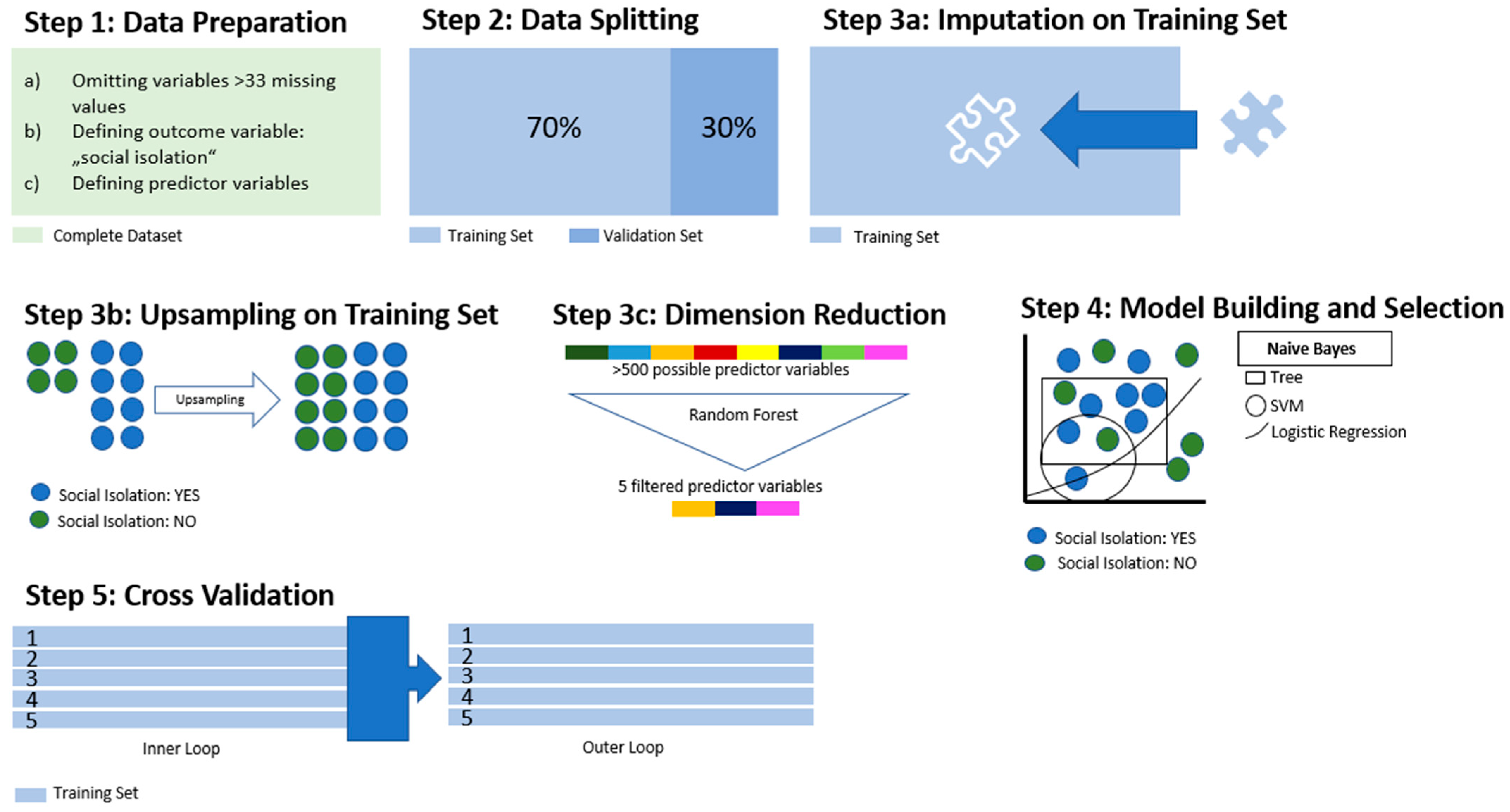
2. Materials and Methods
3. Results
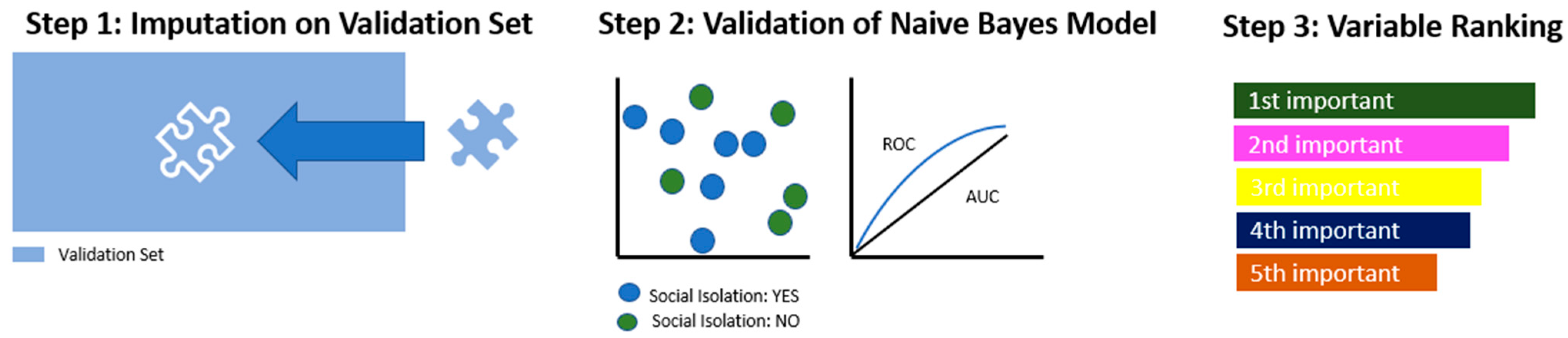
3.1. Model Building through ML
3.2. Applying the Model
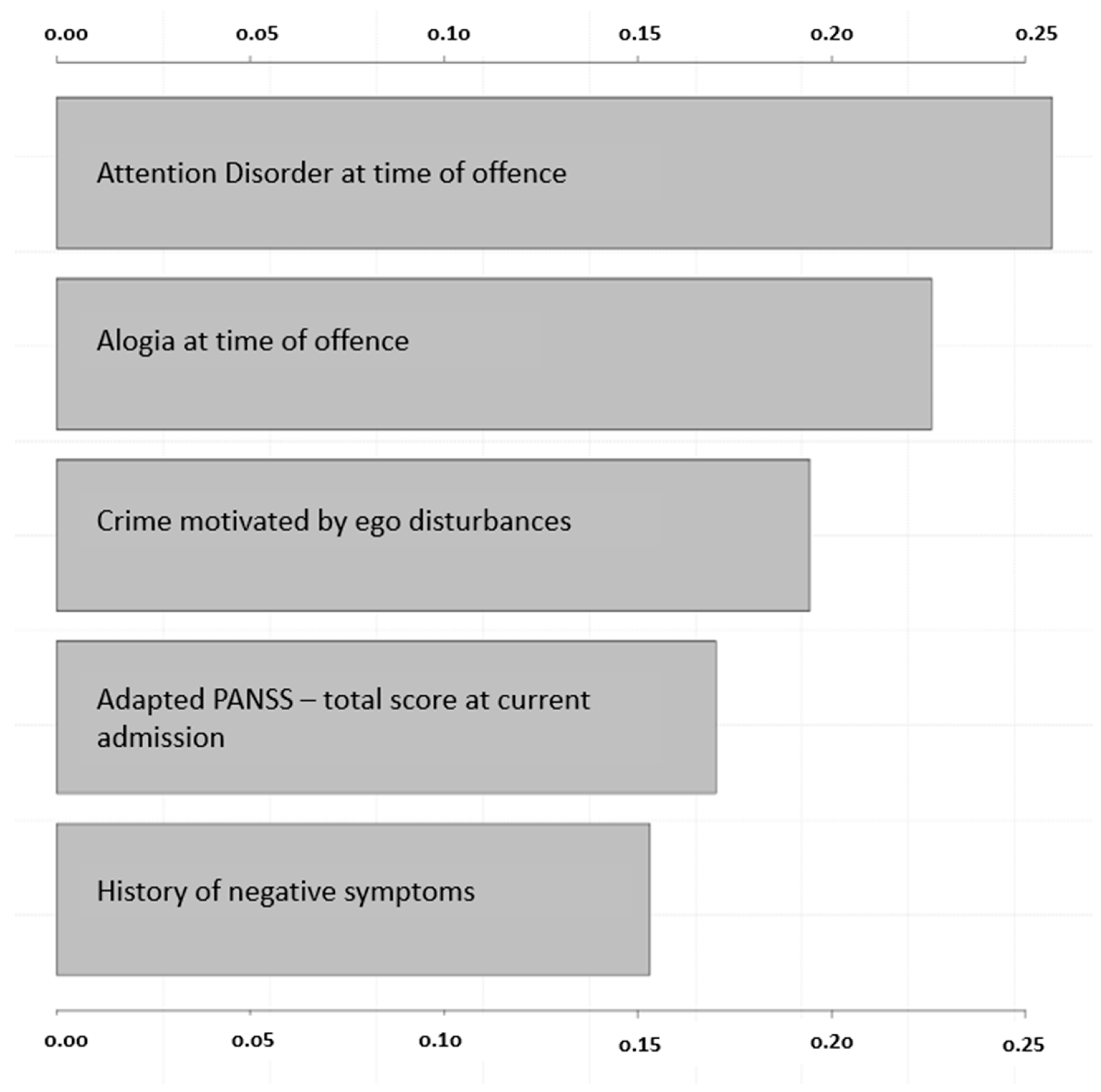
3.3. Predictor Variables Regarding Social Isolation: Influence in the Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Leary, M.; Baumeister, R. The need to belong. Psychol. Bull. 1995, 117, 497–529. [Google Scholar]
- Berkman, L.; Glass, T.; Brissette, I.; Seeman, T. From social integration to health: Durkheim in the new millennium. Soc. Sci. Med. 2000, 51, 843–857. [Google Scholar] [CrossRef] [PubMed]
- Holt-Lunstad, J.; Smith, T.; Layton, J. Social relationships and mortality risk: A meta-analytic review. PLoS Med. 2010, 7, e1000316. [Google Scholar] [CrossRef] [PubMed]
- Xia, N.; Li, H. Loneliness, Social Isolation, and Cardiovascular Health. Antioxid. Redox. Signal. 2018, 28, 837–851. [Google Scholar] [CrossRef] [PubMed]
- Tanskanen, J.; Anttila, T. A Prospective Study of Social Isolation, Loneliness, and Mortality in Finland. Am. J. Public Health 2016, 106, 2042–2048. [Google Scholar] [CrossRef]
- Holt-Lunstad, J.; Smith, T.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef]
- Koenders, J.; de Mooij, L.; Dekker, J.; Kikkert, M. Social inclusion and relationship satisfaction of patients with a severe mental illness. Int. J. Soc. Psychiatry 2017, 63, 773–781. [Google Scholar] [CrossRef]
- Brooker, C.; Ullmann, B. Out of Sight, Out of Mind—The State of Mental Healthcare in Prison; Policy Exchange: London, UK, 2008. [Google Scholar]
- Porcelli, S.; Van Der Wee, N.; van der Werff, S.; Aghajani, M.; Glennon, J.; van Heukelum, S.; Mogavero, F.; Lobo, A.; Olivera, F.; Lobo, E.; et al. Social brain, social dysfunction and social withdrawal. Neurosci. Biobehav. Rev. 2019, 97, 10–33. [Google Scholar] [CrossRef]
- Baumann, A.E. Stigmatization, social distance and exclusion because of mental illness: The individual with mental illness as a “stranger”. Int. Rev. Psychiatry 2007, 19, 131–135. [Google Scholar] [CrossRef]
- Oberndorfer, R.; Alexandrowicz, R.; Unger, A.; Koch, M.; Markiewicz, I.; Gosek, P.; Heitzman, J.; Iozzino, L.; Ferrari, C.; Salize, H.; et al. Needs of forensic psychiatric patients with schizophrenia in five European countries. Soc. Psychiatry Psychiatr. Epidemiol. 2023, 58, 53–63. [Google Scholar] [CrossRef]
- De Tribolet-Hardy, F.; Habermeyer, E. Schizophrenic Patients between General and Forensic Psychiatry. Front. Public Health 2016, 4, 135. [Google Scholar] [CrossRef] [PubMed]
- Suman, A.; Nehra, R.; Sahoo, S.; Grover, S. Prevalence of loneliness and its correlates among patients with schizophrenia. Int. J. Soc. Psychiatry 2022, 207640221141646. [Google Scholar] [CrossRef] [PubMed]
- Culbreth, A.; Barch, D.; Moran, E. An ecological examination of loneliness and social functioning in people with schizophrenia. J. Abnorm. Psychol. 2021, 130, 899–908. [Google Scholar] [CrossRef] [PubMed]
- Reddy, L.; Irwin, M.; Breen, E.; Reavis, E.; Green, M. Social exclusion in schizophrenia: Psychological and cognitive consequences. J. Psychiatr. Res. 2019, 114, 120–125. [Google Scholar] [CrossRef]
- Killaspy, H.; White, S.; Lalvani, N.; Berg, R.; Thachil, A.; Kallumpuram, S.; Nasiruddin, O.; Wright, C.; Mezey, G. The impact of psychosis on social inclusion and associated factors. Int. J. Soc. Psychiatry 2014, 60, 148–154. [Google Scholar] [CrossRef]
- Li, B.; Liu, P.; Chu, Z.; Shang, Y.; Huan, M.; Dang, Y.; Gao, C. Social isolation induces schizophrenia-like behavior potentially associated with HINT1, NMDA receptor 1, and dopamine receptor 2. Neuroreport 2017, 28, 462–469. [Google Scholar] [CrossRef]
- Oliveras, I.; Sánchez-González, A.; Piludu, M.; Gerboles, C.; Río-Álamos, C.; Tobeña, A.; Fernández-Teruel, A. Divergent effects of isolation rearing on prepulse inhibition, activity, anxiety and hippocampal-dependent memory in Roman high- and low-avoidance rats: A putative model of schizophrenia-relevant features. Behav. Brain Res. 2016, 314, 6–15. [Google Scholar] [CrossRef]
- Takahashi, A. The role of social isolation stress in escalated aggression in rodent models. Neurosci. Res. 2022. [Google Scholar] [CrossRef]
- Douglas, C.; Wood, L.; Taggart, D. Recovery priorities of people with psychosis in acute mental health in-patient settings: A Q-methodology study. Behav. Cogn. Psychother. 2022, 50, 1–14. [Google Scholar] [CrossRef]
- Shepherd, A.; Doyle, M.; Sanders, C.; Shaw, J. Personal recovery within forensic settings--Systematic review and meta-synthesis of qualitative methods studies. Crim. Behav. Ment. Health 2016, 26, 59–75. [Google Scholar] [CrossRef]
- Schoppmann, S.; Balensiefen, J.; Lau, S.; Graf, M.; Hachtel, H. Patients’ Views with Regard to Personal Recovery in Forensic Psychiatry in German-Speaking Switzerland—An Explorative Study. Front. Psychiatry 2021, 12, 695096. [Google Scholar] [CrossRef]
- Hofmann, L.; Lau, S.; Kirchebner, J. Advantages of machine learning in forensic psychiatric research—Uncovering the complexities of aggressive behavior in schizophrenia. Appl. Sci. 2022, 12, 819. [Google Scholar] [CrossRef]
- Sonnweber, M.; Kirchebner, J.; Günther, M.; Kappes, J.; Lau, S. Exploring substance use as rule-violating behaviour during inpatient treatment of offender patients with schizophrenia. Crim. Behav. Ment. Health 2022, 32, 255–266. [Google Scholar] [CrossRef] [PubMed]
- JKirchebner; Günther, M.; Sonnweber, M.; King, A.; Lau, S. Factors and predictors of length of stay in offenders diagnosed with schizophrenia—A machine-learning-based approach. BMC Psychiatry 2020, 20, 201. [Google Scholar] [CrossRef]
- Sonnweber, M.; Lau, S.; Kirchebner, J. Violent and non-violent offending in patients with schizophrenia: Exploring influences and differences via machine learning. Compr. Psychiatry 2021, 107, 152238. [Google Scholar] [CrossRef] [PubMed]
- Seifert, D. Die entwicklung des psychiatrischen massregelvollzzugs (§ 63StGB) in Nordrhein-Wesfalen. Psychiat. Prax. 1997, 24, 237–244. [Google Scholar]
- Hsieh, H.-F.; Shannon, S. Three approaches to qualitative content analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef]
- Schalast, N.; Seifert, D.; Leygraf, N. Patienten des Maßregelvollzugs gemäß § 63 StGB mit geringen Entlassungsaussichten. Forens. Psychiatr. Psychol. Kriminol. 2007, 1, 34–42. [Google Scholar] [CrossRef]
- Kay, S.; Fiszbein, A.; Opler, L. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 1987, 13, 261–276. [Google Scholar] [CrossRef]
- Brennan, P.; Hays, B. Focus on psychometrics the kappa statistic for establishing interrater reliability in the secondary analysis of qualitative clinical data. Res. Nurs. Health 1992, 15, 153–158. [Google Scholar] [CrossRef]
- Osisanwo, F.; Akinsola, J.; Awodele, O.; Hinmikaiye, J.; Olakanmi, O.; Akinjobi, J. Supervised machine learning algorithms: Classification and comparison. Int. J. Comput. Trends Technol. (IJCTT) 2017, 48, 128–138. [Google Scholar]
- Bischl, B.; Lang, M.; Kotthoff, L.; Schiffner, J.; Richter, J.; Studerus, E.; Casalicchio, G.; Jones, Z. Machine learning in RJ Mach. Learn. Res. 2016, 17, 5938–5942. [Google Scholar]
- Brodersen, K.; Ong, C.; Stephan, K.; Buhmann, J. The balanced accuracy and its posterior distribution, 2010 20th international conference on pattern recognition. In Proceedings of the 2010 20th International Conference on Pattern Recognition, Istanbul, Turkey, 23–26 August 2010; pp. 3121–3124. [Google Scholar]
- Mihaljević-Peleš, A.; Janović, M.B.; Šagud, M.; Živković, M.; Janović, Š.; Jevtović, S. Cognitive deficit in schizophrenia: An overview. Psychiatr. Danub. 2019, 31, 139–142. [Google Scholar] [PubMed]
- Couture, S.; Penn, D.; Roberts, D. The functional significance of social cognition in schizophrenia: A review. Schizophr. Bull. 2006, 32, S44–S63. [Google Scholar] [CrossRef]
- Pinkham, A.; Penn, D.; Green, M.; Buck, B.; Healey, K.; Harvey, P. The social cognition psychometric evaluation study: Results of the expert survey and RAND panel. Schizophr. Bull. 2014, 40, 813–823. [Google Scholar] [CrossRef] [PubMed]
- Green, M.; Horan, W.; Lee, J. Social cognition in schizophrenia. Nat. Rev. Neurosci. 2015, 16, 620–631. [Google Scholar] [CrossRef]
- Miller, D.; Arndt, S.; Andreasen, N. Alogia, attentional impairment, and inappropriate affect: Their status in the dimensions of schizophrenia. Compr. Psychiatry 1993, 34, 221–226. [Google Scholar] [CrossRef]
- Cohen, A.; Cox, C.; Le, T.; Cowan, T.; Masucci, M.; Strauss, G.; Kirkpatrick, B. Using machine learning of computerized vocal expression to measure blunted vocal affect and alogia. NPJ Schizophr. 2020, 6, 26. [Google Scholar] [CrossRef]
- Strauss, G.; Cohen, A. A transdiagnostic review of negative symptom phenomenology and etiology. Schizophr. Bull. 2017, 43, 712–719. [Google Scholar] [CrossRef]
- Schimansky, J.; Rössler, W.; Haker, H. The influence of social cognition on ego disturbances in patients with schizophrenia. Psychopathology 2012, 45, 117–125. [Google Scholar] [CrossRef]
- Schneider, K. Clinical Psychopathology; Grune and Stratton: New York, NY, USA, 1959. [Google Scholar]
- Decety, J.; Moriguchi, Y. The empathic brain and its dysfunction in psychiatric populations: Implications for intervention across different clinical conditions. BioPsychoSocial Med. 2007, 1, 22. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Garety, P. Connecting neurosis and psychosis: The direct influence of emotion on delusions and hallucinations. Behav. Res. 2003, 41, 923–947. [Google Scholar] [CrossRef] [PubMed]
- Da Rocha, B.M.; Rhodes, S.; Vasilopoulou, E.; Hutton, P. Loneliness in Psychosis: A Meta-analytical Review. Schizophr. Bull. 2018, 44, 114–125. [Google Scholar] [CrossRef] [PubMed]
- Hawkley, L.; Cacioppo, J. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann. Behav. Med. 2010, 40, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Stahl, S.; Buckley, P. Negative symptoms of schizophrenia: A problem that will not go away. Acta Psychiatr. Scand. 2007, 115, 4–11. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, J.; Bradshaw, K.; Catalano, L.; Garcia, C.; Malik, A.; Bennett, M.; Blanchard, J. Negative symptoms and the formation of social affiliative bonds in schizophrenia. Schizophr. Res. 2018, 193, 225–231. [Google Scholar] [CrossRef]
- Foussias, G.; Remington, G. Negative symptoms in schizophrenia: Avolition and Occam’s razor. Schizophr. Bull. 2010, 36, 359–369. [Google Scholar] [CrossRef]
- Riehle, M.; Mehl, S.; Lincoln, T. The specific social costs of expressive negative symptoms in schizophrenia: Reduced smiling predicts interactional outcome. Acta Psychiatr. Scand. 2018, 138, 133–144. [Google Scholar] [CrossRef]
- Hofmann, L.; Lau, S.; Kirchebner, J. Maintaining social capital in offenders with schizophrenia spectrum disorder—An explorative analysis of influential factors. Front. Psychiatry 2022, 13, 945732. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, Medicine. Social Isolation and Loneliness in Older Adults: Opportunities for the Health care System; National Academies Press: Washington, DC, USA, 2020. [Google Scholar]
- Hutten, E.; Jongen, E.; Hajema, K.; Ruiter, R.; Hamers, F.; Bos, A. Risk factors of loneliness across the life span. J. Soc. Pers. Relatsh. 2022, 39, 1482–1507. [Google Scholar] [CrossRef]
- Coyle, C.; Dugan, E. Social isolation, loneliness and health among older adults. J. Aging Health 2012, 24, 1346–1363. [Google Scholar] [CrossRef] [PubMed]
- Kokol, P.; Kokol, M.; Zagoranski, S. Machine learning on small size samples: A synthetic knowledge synthesis. Sci. Prog. 2022, 105, 00368504211029777. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total n/N (%) | Social Isolation n/N (%) | No Social Isolation n/N (%) |
|---|---|---|---|
| Sex: male | 291/320 (90.9) | 205/226 (90.7) | 86/94 (91.5) |
| Age at admission (mean, SD) | 34.3 (10.4) | 34.7 (10.0) | 33.2 (11.2) |
| Native country: Switzerland | 158/320 (49.4) | 114/226 (50.4) | 44/94 (46.8) |
| Single (at offence) | 260/318 (81.3) | 186/225 (82.7) | 74/93 (79.6) |
| Diagnosis: schizophrenia | 264/320 (82.5) | 189/226 (83.6) | 75/94 (79.8) |
| Algorithm | Balanced Accuracy (%) | AUC | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|---|---|
| Logistic Regression | 65.7 | 0.77 | 63.60 | 67.80 | 45.90 | 82.50 |
| Tree | 67.8 | 0.70 | 63.50 | 72.10 | 47.90 | 82.50 |
| Random Forest | 65.6 | 0.76 | 64.9 | 66.2 | 43.7 | 81.9 |
| Gradient Boosting | 67.7 | 0.76 | 65.7 | 69.7 | 48.9 | 83.5 |
| KNN | 64.4 | 0.73 | 60.9 | 67.9 | 44.5 | 81.1 |
| SVM | 67.8 | 0.75 | 62.4 | 73.1 | 49.5 | 82.8 |
| Naive Bayes | 70.1 | 0.80 | 75.1 | 65.1 | 46.4 | 85.1 |
| Variable Description | Social Isolation n/N (%) | No Social Isolation n/N (%) |
|---|---|---|
| History of negative symptoms | 166/225 (73.8) | 43/94 (45.7) |
| Alogia at time of offence | 66/154 (42.9) | 4/45 (8.9) |
| Attention disorder at time of offence | 89/152 (58.6) | 11/44 (25) |
| Adapted PANSS—total score at current admission | 25.1 (SD = 13.5) | 20.1 (SD = 10.9) |
| Crime motivated by ego disturbances | 127/225 (56.4) | 27/94 (28.7) |
| Performance Parameters | % (95%-CI) |
|---|---|
| Balanced accuracy | 69.2 (64.4–81.7) |
| AUC | 0.74 (0.64–0.84) |
| Sensitivity | 60.7 (60.1–61.3) |
| Specificity | 79.4 (79.1–79.7) |
| PPV | 54.8 (54.3–55.4) |
| NPV | 83.1 (82.8–83.4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Machetanz, L.; Lau, S.; Huber, D.; Kirchebner, J. Correlates of Social Isolation in Forensic Psychiatric Patients with Schizophrenia Spectrum Disorders: An Explorative Analysis Using Machine Learning. Int. J. Environ. Res. Public Health 2023, 20, 4392. https://doi.org/10.3390/ijerph20054392
Machetanz L, Lau S, Huber D, Kirchebner J. Correlates of Social Isolation in Forensic Psychiatric Patients with Schizophrenia Spectrum Disorders: An Explorative Analysis Using Machine Learning. International Journal of Environmental Research and Public Health. 2023; 20(5):4392. https://doi.org/10.3390/ijerph20054392
Chicago/Turabian StyleMachetanz, Lena, Steffen Lau, David Huber, and Johannes Kirchebner. 2023. "Correlates of Social Isolation in Forensic Psychiatric Patients with Schizophrenia Spectrum Disorders: An Explorative Analysis Using Machine Learning" International Journal of Environmental Research and Public Health 20, no. 5: 4392. https://doi.org/10.3390/ijerph20054392
APA StyleMachetanz, L., Lau, S., Huber, D., & Kirchebner, J. (2023). Correlates of Social Isolation in Forensic Psychiatric Patients with Schizophrenia Spectrum Disorders: An Explorative Analysis Using Machine Learning. International Journal of Environmental Research and Public Health, 20(5), 4392. https://doi.org/10.3390/ijerph20054392





