Digital Maturity and Its Measurement of General Practitioners: A Scoping Review
Abstract
1. Introduction
1.1. General Practitioners in the Context of Digital Transformation
1.2. Maturity Measurements as a Roadmap for Digital Transformation
1.3. Objective
2. Materials and Methods
2.1. Defining the Research Question
2.2. Identifying Relevant Studies
2.3. Selection of Studies
2.4. Preparation of the Data
2.5. Reporting the Results
3. Results
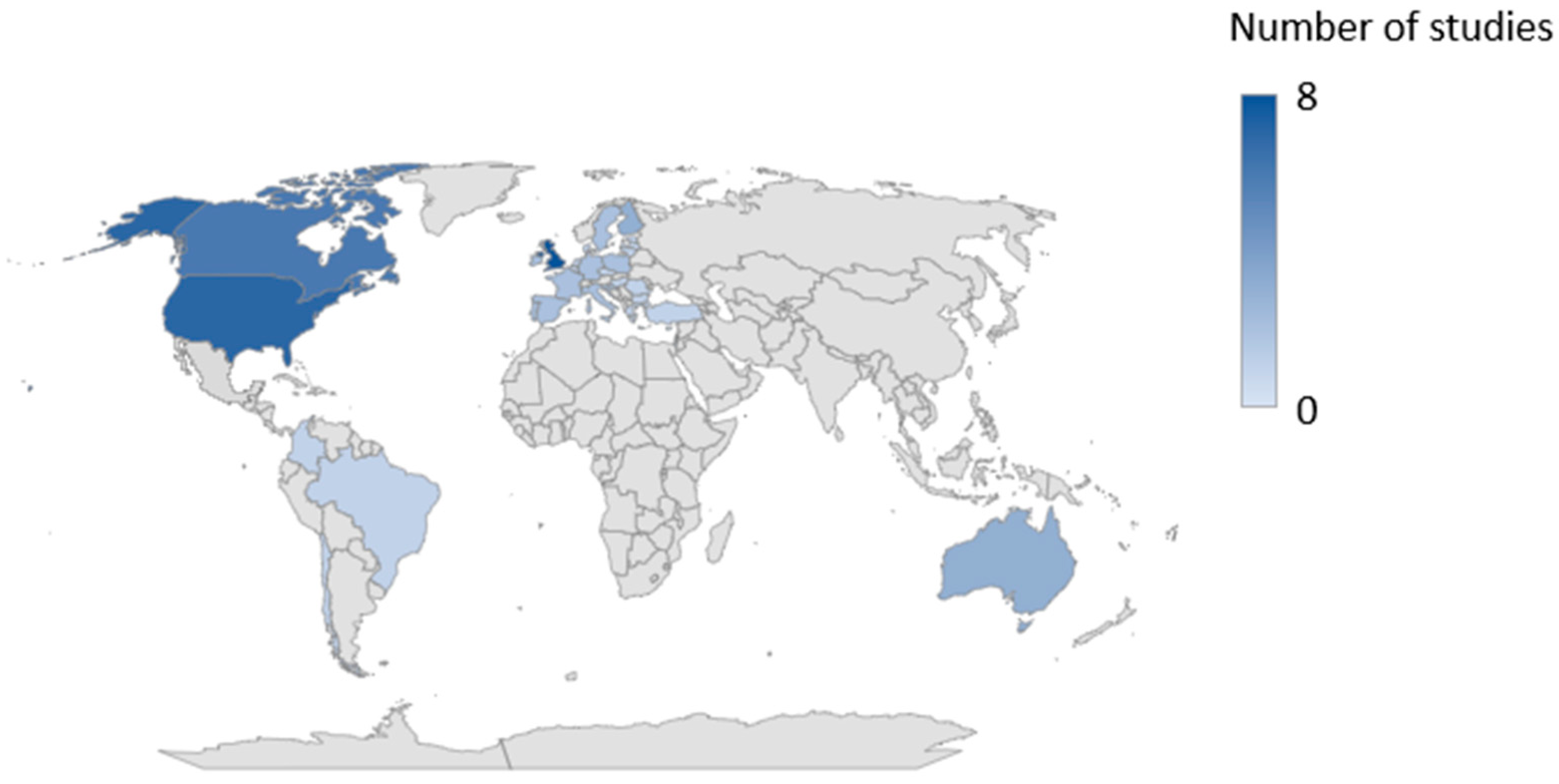
3.1. Study Characteristics
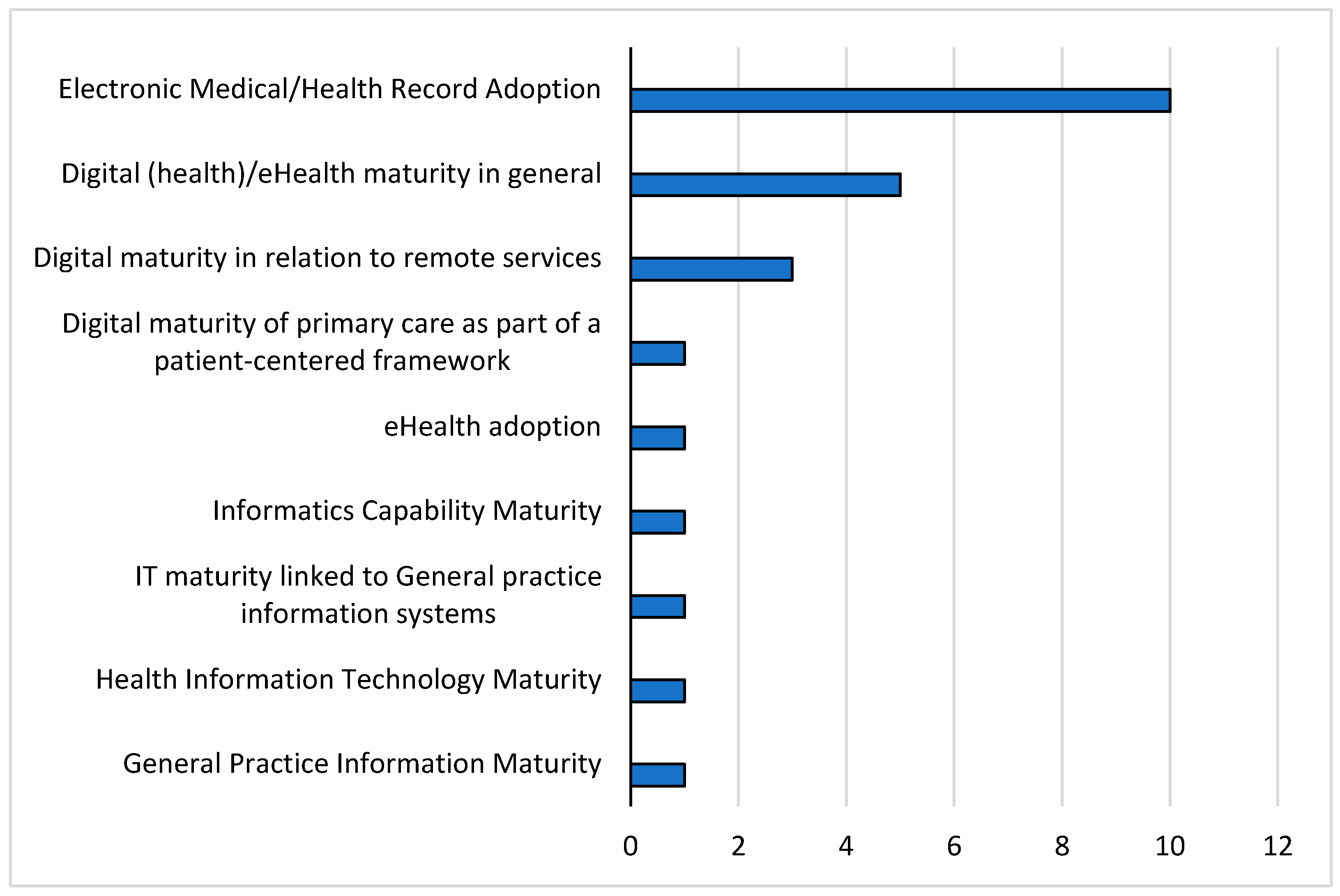
3.2. Context of Digital Maturity
3.3. Operationalization of Digital Maturity
3.4. Maturity Development
3.5. Maturity Survey and Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Maturity Context | Maturity Model | Operationalization | Maturity Development | Refer-ence |
|---|---|---|---|---|
| EMR/HER Adoption | Outpatient-EMRAM (O-EMRAM) | Used EMR capabilities | 8 levels from 0–7
| [37] |
| EMR Maturity Model | Used EMR capabilities | 6 levels from 0–5
| [38] | |
| EMR Adoption Model | Used EMR capabilities | 6 levels from 0–5 and 1–6, respectively (Tagg recoded the original scale)
Hospitals, other practices, labs, and pharmacists for collaborative care | [39,40,41] | |
| Clinical Value Model | Used EMR-Capabilities | 5 levels from 1–5
| [70] | |
| Miller et al. Model | Used EMR/EHR-Capabilties | 5 EMR/EHR user types of physicians:
| [42,43] | |
| Lanham et al. Model |
| 3 EHR use categories at the practice level and physician level from low to high | [44,45] | |
| Digital (health)/eHealth maturity in general | eHealth Maturity scale by Haverinen et al. | 3 areas, 16 indicators
| Each indicator is measured on a scale from 0 up to 10 | [49] |
| Digital maturity framework adapted from Flott et al. [54] |
| Maturity scale from 0–6 | [50] | |
| Digital health maturity assessment for general practice by Gippsland Primary Health Network |
| 3 levels from 1–3
| [47] | |
| Victoria’s Digital Health Maturity Model | The model is built around nine pillars. “Governance and stewardship” sits across the nine pillars:
| 5 Levels from 1–5
| [46] | |
| NHS‘ Digital Primary Care Maturity Assurance Model | IT capabilities | 3 categories:
| [48] | |
| Digital maturity in relation to remote services | Digital maturity scale for healthcare organizations in relation to remote services |
| 5 Levels from 1–5
| [51,52,53] |
| Digital maturity of primary care as a part of a patient-centered framework | Patient-Centered Framework for Evaluating Digital Maturity |
| Point scale from 0–14 | [54] |
| eHealth adoption | Composite index for overall ICT adoption | Used ICT-Capabilities
| Composite eHealth index for ICT adoption. 0 = Not known 4 = Routine use | [5] |
| Informatics Capabilty Maturity | Informatics Capability Maturity Model |
| 5 levels from 1–5 per indicator
| [55] |
| IT maturity linked to General practice information systems | Hermanns’s Focus area maturity model to assess IT maturity in general practices | Focus areas and capabilities of a physician information system | Each focus area has its own number of specific maturity levels, and the overall maturity level of a physician information system is expressed as a combination of the maturity levels of these focus areas | [57] |
| Health Information Technology Maturity | Wallace’s adapted SMPP IT Value Hierarchy Model | Including HIT applications used, integration of HIT applications, system stability, quality and speed of information reception, attitude toward the system, interaction with the system, patient interaction | 5 levels, depending on the distinctiveness of the IT
| [56] |
| General Practice Information Maturity | General practice information maturity model |
| 6 levels from 0–5
| [58] |
| Maturity Context | Maturity Model | Maturity Results | Reference |
|---|---|---|---|
| EMR/EHR Adoption | Outpatient-EMRAM (O-EMRAM) | Not available (N/A) | [37] |
| EMR Maturity Model | More than half were at level 1 or 2 for current EMR maturity level. | [38] | |
| EMR Adoption Model | Overall EMR adoption
| [39,40,41] | |
| Clinical Value Model | 2.5 and 3.5, respectively | [70] | |
| Miller et al. Model |
| [42,43] | |
| Lanham et al. Model |
| [44,45] | |
| Digital (health) /eHealth maturity in general | eHealth Maturity scale by Haverinen et al. |
| [49] |
| Adapted digital maturity framework developed by Flott et al. [54] | Median digital maturity level of 4 | [50] | |
| Digital health maturity assessment for general practice by Gippsland Primary Health Network | Just under two-thirds of the practices surveyed achieved Level 2. | [47] | |
| Victoria’s Digital Health Maturity Model | N/A | [46] | |
| NHS‘ Digital Primary Care Maturity Assurance Model | N/A | [48] | |
| Digital maturity in relation to remote services | Digital maturity scale for healthcare organizations in relation to remote services |
| [51,52,53] |
| Digital maturity of primary care as a part of a patient-centered framework | Patient-Centered Framework for Evaluating Digital Maturity | N/A | [54] |
| eHealth adoption | Composite index for overall ICT adoption | EU average of the composite index is 2.131 | [5] |
| Informatics Capabilty Maturity | Informatics Capability Maturity Model |
| [55] |
| IT maturity linked to General practice information systems | Hermanns’s Focus area maturity model to assess IT maturity in general practices | The maturity of physician information systems from individual manufacturers was measured. These showed different levels of maturity. | [57] |
| Health Information Technology Maturity | Wallace’s adapted SMPP IT Value Hierarchy Model | Most practices met the requirements of level 3. | [56] |
| General Practice Information Maturity | General practice information maturity model | Most practices had a maturity score of 1. | [58] |
References
- Bashshur, R.L.; Howell, J.D.; Krupinski, E.A.; Harms, K.M.; Bashshur, N.; Doarn, C.R. The Empirical Foundations of Telemedicine Interventions in Primary Care. Telemed J. e-Health 2016, 22, 342–375. [Google Scholar] [CrossRef] [PubMed]
- Naumann, J. Die Digitale Arztpraxis—Vision Oder Fiktion? In Die Digitale Transformation im Gesundheitswesen: Transformation, Innovation, Disruption; Matusiewicz, D., Pittelkau, C., Elmer, A., Addam, M., Eds.; Medizinisch Wissenschaftliche Verlagsgesellschaft: Berlin, Germany, 2017; pp. 131–133. ISBN 978-3-95466-326-2. [Google Scholar]
- Deutscher Hausärzteverband. Idealbild Einer Digitalen Hausärztlichen Versorgung. Available online: https://www.hausaerzteverband.de/fileadmin/user_upload/News_Dateien/2022/2022_05_09_Hausaerzteverband_Konzeptpapier_Digitale_hausaerztliche_Versorgung.pdf (accessed on 26 February 2023).
- De Rosis, S.; Seghieri, C. Basic ICT Adoption and Use by General Practitioners: An Analysis of Primary Care Systems in 31 European Countries. BMC Med. Inform. Decis. Mak. 2015, 15, 70. [Google Scholar] [CrossRef]
- European Commission; Directorate-General for Communications Networks, Content and Technology; Valverde-Albacete, J.; Folkvord, F.; Lupiáñez-Villanueva, F.; Hocking, L.; Devaux, A.; Altenhofer, M.; Harshfield, A.; Faulí, C. Benchmarking Deployment of EHealth among General Practitioners (2018): Final Report; Publications Office: Mercier, Luxembourg, 2019.
- World Health Organization. Global Strategy on Digital Health 2020–2025; World Health Organization: Geneva, Switzerland, 2021; ISBN 978-92-4-002092-4.
- OECD; European Union. Health at a Glance: Europe 2016: State of Health in the EU Cycle; OECD: Paris, France, 2016; ISBN 978-92-64-26558-5. [Google Scholar]
- International Conference on Primary Health Care; World Health Organization; United Nations Children’s Fund (UNICEF). Primary Health Care: Report of the International Conference on Primary Health Care, Alma-Ata, USSR, 6–12 September 1978; World Health Organization: Geneva, Switzerland; the United Nations Children’s Fund: New York, NY, USA, 1978.
- WONCA Europe. The European Definition of General Practice/Family Medicine. Available online: https://www.globalfamilydoctor.com/site/DefaultSite/filesystem/documents/regionDocs/European%20Definition%20of%20general%20practice%203rd%20ed%202011.pdf (accessed on 26 February 2023).
- Ebert, C.; Duarte, C.H. Digital Transformation. IEEE Softw. 2018, 35, 16–21. [Google Scholar] [CrossRef]
- Krcmar, H. Digitale Transformation aus Perspektive von Wissenschaft und Forschung. In Digitale Transformation: Fallbeispiele and Branchenanalysen; Oswald, G., Saueressig, T., Krcmar, H., Eds.; Springer Gabler: Wiesbaden, Germany, 2022; ISBN 978-3-658-37571-3. [Google Scholar]
- Lehmann, A.; Matusiewicz, D. Die Smarte Arztpraxis Und Das Digitale Wartezimmer. In Die digitale Arztpraxis: Technik, Tools and Tipps zur Umsetzung; Henningsen, M., Stachwitz, P., Fahimi-Weber, S., Eds.; Medizinisch Wissenschaftliche Verlagsgesellschaft: Berlin, Germany, 2022; pp. 188–198. ISBN 978-3-95466-577-8. [Google Scholar]
- Versluis, A.; van Luenen, S.; Meijer, E.; Honkoop, P.J.; Pinnock, H.; Mohr, D.C.; Neves, A.L.; Chavannes, N.H.; van der Kleij, R.M.J.J. SERIES: EHealth in Primary Care. Part 4: Addressing the Challenges of Implementation. Eur. J. Gen. Pr. 2020, 26, 140–145. [Google Scholar] [CrossRef] [PubMed]
- Cresswell, K.; Sheikh, A. Organizational Issues in the Implementation and Adoption of Health Information Technology Innovations: An Interpretative Review. Int. J. Med. Inform. 2013, 82, e73–e86. [Google Scholar] [CrossRef]
- De Bruin, T.; Freeze, R.; Kulkarni, U.; Rosemann, M. Understanding the Main Phases of Developing a Maturity Assessment Model. Australas. Conf. Inf. Syst. 2005, 8–19. [Google Scholar]
- Mettler, T. Maturity Assessment Models: A Design Science Research Approach. Int. J. Soc. Syst. Sci. 2011, 3, 81–98. [Google Scholar] [CrossRef]
- Fraser, P.; Moultrie, J.; Gregory, M. The Use of Maturity Models/Grids as a Tool in Assessing Product Development Capability. In Proceedings of the IEEE International Engineering Management Conference, Cambridge, UK, 18–20 August 2002; Volume 1, pp. 244–249. [Google Scholar]
- Becker, J.; Knackstedt, R.; Pöppelbuß, J. Developing Maturity Models for IT Management. Bus. Inf. Syst. Eng. 2009, 1, 213–222. [Google Scholar] [CrossRef]
- Humphrey, W.S. Characterizing the Software Process: A Maturity Framework. IEEE Softw. 1988, 5, 73–79. [Google Scholar] [CrossRef]
- De Bruin, T.; Rosemann, M. Towards a Business Process Management Maturity Model. In Proceedings of the 13th European Conference on Information Systems, Regensburg, Germany, 26–28 May 2005; pp. 521–532. [Google Scholar]
- Freeze, R.; Kulkarni, U. Knowledge Management Capability Assessment: Validating a Knowledge Assets Measurement Instrument. In Proceedings of the 38th Annual Hawaii International Conference on System Sciences, Big Island, HA, USA, 3–6 January 2005; p. 251a. [Google Scholar]
- Carvalho, J.V.; Rocha, Á.; Abreu, A. Maturity Models of Healthcare Information Systems and Technologies: A Literature Review. J. Med Syst. 2016, 40, 131. [Google Scholar] [CrossRef]
- Gomes, J.; Romão, M. Information System Maturity Models in Healthcare. J. Med. Syst. 2018, 42, 235. [Google Scholar] [CrossRef] [PubMed]
- World Health Assembly 71. Seventy-First World Health Assembly: Geneva, 21–26 May 2018: Summary Records of Committees, Reports of Committees; World Health Organization: Geneva, Switzerland, 2018.
- HIMSS. EMRAM. HIMSS Solution. Available online: https://www.himss.org/sites/hde/files/2022-01/emram-info.pdf (accessed on 26 February 2023).
- HIMSS. Electronic Medical Record Adoption Model (EMRAM). Available online: https://www.himss.org/what-we-do-solutions/digital-health-transformation/maturity-models/electronic-medical-record-adoption-model-emram (accessed on 26 February 2023).
- DigitalRadar Krankenhaus Konsortium. Instrument zur Evaluierung des Reifegrades der Krankenhäuser Hinsichtlich der Digitalisierung; Universität St. Gallen, School of Medicine, Lehrstuhl für Management im Gesundheitswesen: St.Gallen, Switzerland, 2021. [Google Scholar]
- NHS England. Digital Maturity Assessment. Available online: https://digital.nhs.uk/services/cloud-centre-of-excellence/ccoe-services/capability-maturity-assessment (accessed on 26 February 2023).
- Duncan, R.; Eden, R.; Woods, L.; Wong, I.; Sullivan, C. Synthesizing Dimensions of Digital Maturity in Hospitals: Systematic Review. J. Med. Internet Res. 2022, 24, e32994. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Colquhoun, H.L.; Levac, D.; O’Brien, K.K.; Straus, S.; Tricco, A.C.; Perrier, L.; Kastner, M.; Moher, D. Scoping Reviews: Time for Clarity in Definition, Methods, and Reporting. J. Clin. Epidemiol. 2014, 67, 1291–1294. [Google Scholar] [CrossRef]
- Harzing, A.-W. Publish or Perish. Available online: https://harzing.com/resources/publish-or-perish (accessed on 26 February 2023).
- WHO Regional Office for Europe General Practitioners (PP) per 100,000. European Health for All Database (HFA-DB). 01 September 2022. Available online: https://gateway.euro.who.int/en/indicators/hfa_507-5290-general-practitioners-pp-per-100-000/ (accessed on 26 February 2023).
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R Package and Shiny App for Producing PRISMA 2020-Compliant Flow Diagrams, with Interactivity for Optimised Digital Transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef]
- Rethlefsen, M.L.; Page, M.J. PRISMA 2020 and PRISMA-S: Common Questions on Tracking Records and the Flow Diagram. J. Med Libr. Assoc. 2021, 110, 253–257. [Google Scholar] [CrossRef] [PubMed]
- HIMSS. Outpatient Electronic Medical Record Adoption Model (O-EMRAM). Available online: https://www.himss.org/what-we-do-solutions/digital-health-transformation/maturity-models/outpatient-electronic-medical-record-adoption-model-o-emram (accessed on 26 February 2023).
- Chong, J.; Jason, T.; Jones, M.; Larsen, D. A Model to Measure Self-Assessed Proficiency in Electronic Medical Records: Validation Using Maturity Survey Data from Canadian Community-Based Physicians. Int. J. Med. Inform. 2020, 141, 104218. [Google Scholar] [CrossRef]
- Price, M.; Lau, F.; Lai, J. Measuring EMR Adoption: A Framework and Case Study. Electron. Healthc. 2011, 10, e25–e30. [Google Scholar]
- Price, M.; Singer, A.; Kim, J. Adopting Electronic Medical Records: Are They Just Electronic Paper Records? Can. Fam. Physician 2013, 59, e322–e329. [Google Scholar]
- Tagg, B.L. Meaningful Electronic Medical Record Use: A Survey of Famly Practice Clinics; University of Lethbridge: Lethbridge, AB, Canada, 2015. [Google Scholar]
- Miller, R.H.; Sim, I.; Newman, J. Electronic Medical Records in Solo/Small Groups: A Qualitative Study of Physician User Types. Stud. Health Technol. Inform. 2004, 107, 658–662. [Google Scholar] [PubMed]
- Wilcox, A.; Bowes, W.A.; Thornton, S.N.; Narus, S.P. Physician Use of Outpatient Electronic Health Records to Improve Care. AMIA Annu. Symp. Proc. 2008, 2008, 809–813. [Google Scholar] [PubMed]
- Lanham, H.J.; Leykum, L.K.; McDaniel, R.R. Same Organization, Same Electronic Health Records (EHRs) System, Different Use: Exploring the Linkage between Practice Member Communication Patterns and EHR Use Patterns in an Ambulatory Care Setting. J. Am. Med Informatics Assoc. 2012, 19, 382–391. [Google Scholar] [CrossRef] [PubMed]
- Lanham, H.J.; Sittig, D.F.; Leykum, L.K.; Parchman, M.L.; Pugh, J.A.; McDaniel, R.R. Understanding Differences in Electronic Health Record (EHR) Use: Linking Individual Physicians’ Perceptions of Uncertainty and EHR Use Patterns in Ambulatory Care. J. Am. Med Informatics Assoc. 2014, 21, 73–81. [Google Scholar] [CrossRef]
- EY. Victoria’s Digital Health Maturity Model. Available online: https://assets.ey.com/content/dam/ey-sites/ey-com/en_au/noindex/ey-digital-health-maturity-model-whitepaper.pdf (accessed on 26 February 2023).
- Azar, D.; Cuman, A.; Blake, T.; Proposch, A. A Digital Health Maturity Assessment for General Practice. Available online: https://apo.org.au/node/317828 (accessed on 26 February 2023).
- NHS England. Digital Maturity Assurance. Available online: https://www.england.nhs.uk/digitaltechnology/digital-primary-care/digital-maturity-assurance/ (accessed on 26 February 2023).
- Haverinen, J.; Keränen, N.; Tuovinen, T.; Ruotanen, R.; Reponen, J. National Development and Regional Differences in EHealth Maturity in Finnish Public Health Care: Survey Study. JMIR Med. Inform. 2022, 10, e35612. [Google Scholar] [CrossRef]
- Teixeira, F.; Li, E.; Laranjo, L.; Collins, C.; Irving, G.; Fernandez, M.J.; Car, J.; Ungan, M.; Petek, D.; Hoffman, R.; et al. Digital Maturity and Its Determinants in General Practice: A Cross-Sectional Study in 20 Countries. medRxiv 2022. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Rosen, R.; Shaw, S.E.; Byng, R.; Faulkner, S.; Finlay, T.; Grundy, E.; Husain, L.; Hughes, G.; Leone, C.; et al. Planning and Evaluating Remote Consultation Services: A New Conceptual Framework Incorporating Complexity and Practical Ethics. Front. Digit. Health 2021, 3, 726095. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Shaw, S.E.; Alvarez Nishio, A.; Byng, R.; Clarke, A.; Dakin, F.; Faulkner, S.; Hemmings, N.; Husain, L.; Kalin, A.; et al. Remote Care in UK General Practice: Baseline Data on 11 Case Studies. NIHR Open Res. 2022, 2, 47. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Ladds, E.; Hughes, G.; Moore, L.; Wherton, J.; Shaw, S.E.; Papoutsi, C.; Wieringa, S.; Rosen, R.; Rushforth, A.; et al. Why Do GPs Rarely Do Video Consultations? Qualitative Study in UK General Practice. Br. J. Gen. Pr. 2022, 72, e351–e360. [Google Scholar] [CrossRef] [PubMed]
- Flott, K.; Callahan, R.; Darzi, A.; Mayer, E. A Patient-Centered Framework for Evaluating Digital Maturity of Health Services: A Systematic Review. J. Med Internet Res. 2016, 18, e75. [Google Scholar] [CrossRef]
- Liaw, S.-T.; Kearns, R.; Taggart, J.; Frank, O.; Lane, R.; Tam, M.; Dennis, S.; Walker, C.; Russell, G.; Harris, M. The Informatics Capability Maturity of Integrated Primary Care Centres in Australia. Int. J. Med. Inform. 2017, 105, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Wallace, S. Health Information Technology (HIT) in Small and Medium Sized Physician Practices: Examination of Impacts and HIT Maturity; University of North Carolina at Greensboro: Greensboro, NC, USA, 2015. [Google Scholar]
- Hermanns, T. Towards an IT Maturity Model for General Practice Information Systems; Universiteit Utrecht: Utrecht, The Netherlands, 2014. [Google Scholar]
- Gillies, A. Information Support for General Practice in the New NHS. Health Libr. Rev. 2000, 17, 91–96. [Google Scholar] [CrossRef]
- OECD. Health Expenditure by Type of Service. In Health at a Glance 2017; OECD: Paris, France, 2017; pp. 140–141. ISBN 978-92-64-28039-7. [Google Scholar]
- Burmann, A.; Meister, S. Practical Application of Maturity Models in Healthcare: Findings from Multiple Digitalization Case Studies. HEALTHINF 2021, 5, 100–110. [Google Scholar]
- Jamoulle, M.; Resnick, M.; Vander Stichele, R.; Ittoo, A.; Cardillo, E.; Vanmeerbeek, M. Analysis of Definitions of General Practice, Family Medicine, and Primary Health Care: A Terminological Analysis. BJGP Open 2017, 1, 101049. [Google Scholar] [CrossRef]
- Burmann, A.; Fischer, B.; Brinkkötter, N.; Meister, S. Managing Directors’ Perspectives on Digital Maturity in German Hospitals—A Multi-Point Online-Based Survey Study. IJERPH 2022, 19, 9709. [Google Scholar] [CrossRef]
- Albrecht, M.; Mansky, T.; Sander, M.; Schiffhorst, G. Gutachten Nach § 115b Abs. 1a SGB V. Available online: https://www.iges.com/sites/igesgroup/iges.de/myzms/content/e6/e1621/e10211/e27603/e27841/e27842/e27844/attr_objs27932/IGES_AOP_Gutachten_032022_ger.pdf (accessed on 24 February 2023).
- Gartner Inc. Definition of Digitization—Gartner Information Technology Glossary. Available online: https://www.gartner.com/en/information-technology/glossary/digitization (accessed on 25 February 2023).
- Cresswell, K.; Sheikh, A.; Krasuska, M.; Heeney, C.; Franklin, B.D.; Lane, W.; Mozaffar, H.; Mason, K.; Eason, S.; Hinder, S.; et al. Reconceptualising the Digital Maturity of Health Systems. Lancet Digit. Health 2019, 1, e200–e201. [Google Scholar] [CrossRef]
- Von Huben, A.; Howell, M.; Howard, K.; Carrello, J.; Norris, S. Health Technology Assessment for Digital Technologies That Manage Chronic Disease: A Systematic Review. Int. J. Technol. Assess. Health Care 2021, 37, e66. [Google Scholar] [CrossRef]
- Haverinen, J.; Keränen, N.; Falkenbach, P.; Maijala, A.; Kolehmainen, T.; Reponen, J. Digi-HTA: Health Technology Assessment Framework for Digital Healthcare Services. Finn. J. eHealth eWelfare 2019, 11, 326–341. [Google Scholar] [CrossRef]
- Knapp, A.; Harst, L.; Hager, S.; Schmitt, J.; Scheibe, M. Use of Patient-Reported Outcome Measures and Patient-Reported Experience Measures Within Evaluation Studies of Telemedicine Applications: Systematic Review. J. Med Internet Res. 2021, 23, e30042. [Google Scholar] [CrossRef]
- Unsworth, H.; Dillon, B.; Collinson, L.; Powell, H.; Salmon, M.; Oladapo, T.; Ayiku, L.; Shield, G.; Holden, J.; Patel, N.; et al. The NICE Evidence Standards Framework for Digital Health and Care Technologies—Developing and Maintaining an Innovative Evidence Framework with Global Impact. Digit. Health 2021, 7, 205520762110186. [Google Scholar] [CrossRef]
- Rimmer, C.; Hagens, S.; Baldwin, A.; Anderson, C. Measuring Maturity of Use for Electronic Medical Records in British Columbia: The Physician Information Technology Office. Healthc. Q. 2015, 17, 75–80. [Google Scholar] [CrossRef] [PubMed]

| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Publication in German or English | Publication in languages other than German or English |
| Addressing digital maturity and its measurement among general practitioners | Examining digital maturity among other physician groups (e.g., specialists) or in other health care sectors (e.g., inpatient care) |
| Maturity measurements enable GPs to be ranked in terms of their level of digitalization | Loose measurement of the level of digitalization without using a development plan |
| Reviews |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neunaber, T.; Meister, S. Digital Maturity and Its Measurement of General Practitioners: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 4377. https://doi.org/10.3390/ijerph20054377
Neunaber T, Meister S. Digital Maturity and Its Measurement of General Practitioners: A Scoping Review. International Journal of Environmental Research and Public Health. 2023; 20(5):4377. https://doi.org/10.3390/ijerph20054377
Chicago/Turabian StyleNeunaber, Timo, and Sven Meister. 2023. "Digital Maturity and Its Measurement of General Practitioners: A Scoping Review" International Journal of Environmental Research and Public Health 20, no. 5: 4377. https://doi.org/10.3390/ijerph20054377
APA StyleNeunaber, T., & Meister, S. (2023). Digital Maturity and Its Measurement of General Practitioners: A Scoping Review. International Journal of Environmental Research and Public Health, 20(5), 4377. https://doi.org/10.3390/ijerph20054377







