Factors Influencing the Level of Depression and Anxiety of Community-Dwelling Patients with Schizophrenia in China during the COVID-19 Pandemic
Abstract
1. Introduction
2. Literature Review
2.1. Sleep Status
2.2. Accompanying Long-Standing Diseases
2.3. Concern about COVID-19 and the Degree of Concern about the COVID-19 Epidemic
3. Methods
3.1. Research Approach
3.2. Questionnaire Development
3.3. Measurement
3.3.1. Anxiety Scale
3.3.2. Depression Scale
3.4. Sampling and Data Collection
3.5. Ethical Approval
3.6. Statistical Analysis
4. Results
4.1. General Distribution of Patient’s Anxiety or Depression
4.2. Subgroup Analyses of Questionnaire Scores
4.3. Concern about the COVID-19 Pandemic
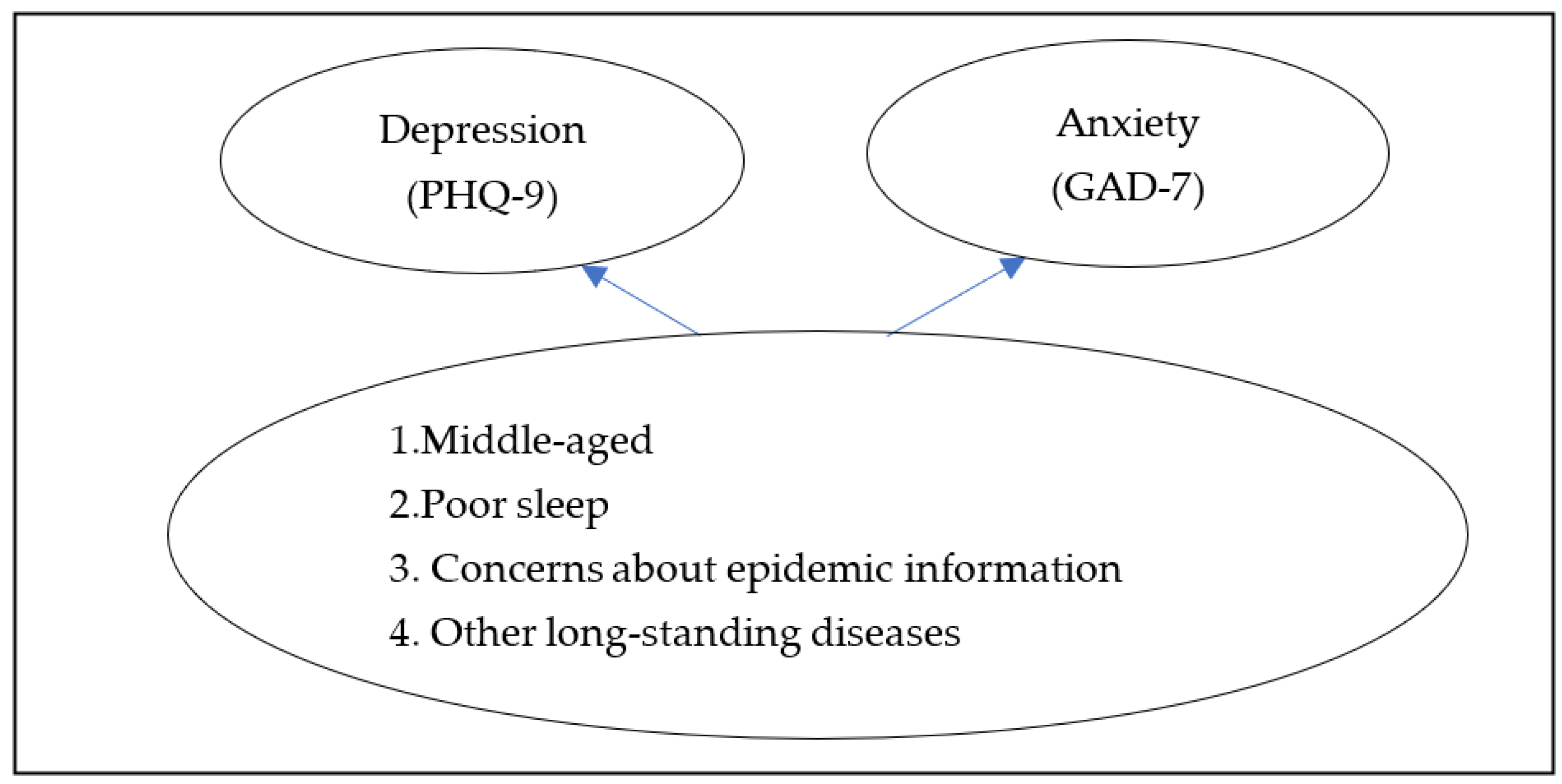
4.4. Multivariate Logistic Regression Models for Anxiety and Depression among Community-Dwelling Patients with Schizophrenia
5. Discussion
6. Conclusions, Limitations, and Future Research
6.1. Conclusions
6.2. Limitations and Future Research
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- Lebel, C.; MacKinnon, A.; Bagshawe, M.; Tomfohr-Madsen, L.; Giesbrecht, G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J. Affect. Disord. 2020, 277, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Odriozola-González, P.; Planchuelo-Gómez, A.; Irurtia, M.J.; de Luis-García, R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020, 290, 113108. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Wang, Q.; Xu, R.; Volkow, N.D. Increased risk of COVID-19 infection and mortality in people with mental disorders: Analysis from electronic health records in the United States. World Psychiatry 2021, 20, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Yao, H.; Chen, J.H.; Xu, Y.F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry 2020, 7, e21. [Google Scholar] [CrossRef]
- Shinn, A.K.; Viron, M. Perspectives on the COVID-19 Pandemic and Individuals with Serious Mental Illness. J. Clin. Psychiatry 2020, 81, 14205. [Google Scholar] [CrossRef]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Chen, H.; Phillips; Cheng, H.; Chen, Q.; Chen, X.; Fralick, D.; Zhang, Y.; Liu, M.; Huang, J.; Bueber, M. Mental health law of the People’s Republic of China (English translation with annotations): Translated and annotated version of China’s new mental health law. Shanghai Arch. Psychiatry 2012, 24, 305–321. [Google Scholar] [CrossRef]
- Liu, X.; Lin, H.; Jiang, H.; Li, R.; Zhong, N.; Su, H.; Li, Y.; Zhao, M. Clinical characteristics of hospitalised patients with schizophrenia who were suspected to have coronavirus disease (COVID-19) in Hubei Province, China. Gen. Psychiatry 2020, 33, e100222. [Google Scholar] [CrossRef]
- Ma, J.; Hua, T.; Zeng, K.; Zhong, B.; Wang, G.; Liu, X. Influence of social isolation caused by coronavirus disease 2019 (COVID-19) on the psychological characteristics of hospitalized schizophrenia patients: A case-control study. Transl. Psychiatry 2020, 10, 411. [Google Scholar] [CrossRef]
- Yamada, A.-M.; Lee, K.K.; Dinh, T.Q.; Barrio, C.; Brekke, J.S. Intrinsic Motivation as a Mediator of Relationships between Symptoms and Functioning Among Individuals with Schizophrenia Spectrum Disorders in a Diverse Urban Community. J. Nerv. Ment. Dis. 2010, 198, 28–34. [Google Scholar] [CrossRef]
- Tomotake, M. Quality of life and its predictors in people with schizophrenia. J. Med. Investig. 2011, 58, 167–174. [Google Scholar] [CrossRef]
- Haro, J.M.; Novick, D.; Bertsch, J.; Karagianis, J.; Dossenbach, M.; Jones, P.B. Cross-national clinical and functional remission rates: Worldwide Schizophrenia Outpatient Health Outcomes (W-SOHO) study. Br. J. Psychiatry 2011, 199, 194–201. [Google Scholar] [CrossRef] [PubMed]
- Solé, B.; Verdolini, N.; Amoretti, S.; Montejo, L.; Rosa, A.R.; Hogg, B.; Garcia-Rizo, C.; Mezquida, G.; Bernardo, M.; Martinez-Aran, A.; et al. Effects of the COVID-19 pandemic and lockdown in Spain: Comparison between community controls and patients with a psychiatric disorder. Preliminary results from the BRIS-MHC STUDY. J. Affect. Disord. 2020, 281, 13–23. [Google Scholar] [CrossRef]
- Rosa-Alcázar, Á.; Parada-Navas, J.L.; García-Hernández, M.D.; Martínez-Murillo, S.; Olivares-Olivares, P.J.; Rosa-Alcázar, A.I. Coping Strategies, Anxiety and Depression in OCD and Schizophrenia: Changes during COVID-19. Brain Sci. 2021, 11, 926. [Google Scholar] [CrossRef]
- Hosgelen, E.I.; Alptekin, K. The Impact of The COVID-19 Pandemic on Schizophrenia Patients. Turk. Psikiyatr. Derg. 2021, 32, 219–221. [Google Scholar] [CrossRef]
- Ferrarelli, F. Sleep Abnormalities in Schizophrenia (SCZ): State of the Art and Next Steps. Am. J. Psychiatry 2021, 178, 903–913. [Google Scholar] [CrossRef] [PubMed]
- Nyer, M.; Farabaugh, A.; Fehling, K.; Soskin, D.; Holt, D.; Papakostas, G.I.; Pedrelli, P.; Fava, M.; Pisoni, A.; Vitolo, O.; et al. Relationship between sleep disturbance and depression, anxiety, and functioning in college students. Depress. Anxiety 2013, 30, 873–880. [Google Scholar] [CrossRef]
- Vollrath, M.; Wicki, W.; Angst, J. The Zurich study. VIII. Insomnia: Association with depression, anxiety, somatic syndromes, and course of insomnia. Eur. Arch. Psychiatry Neurol. Sci. 1989, 239, 113–124. [Google Scholar] [CrossRef] [PubMed]
- Suvisaari, J.; Keinanen, J.; Eskelinen, S.; Mantere, O. Diabetes and Schizophrenia. Curr. Diabetes Rep. 2016, 16, 16. [Google Scholar] [CrossRef]
- Ayerbe, L.; Forgnone, I.; Addo, J.; Siguero, A.; Gelati, S.; Ayis, S. Hypertension risk and clinical care in patients with bipolar disorder or schizophrenia; A systematic review and meta-analysis. J. Affect. Disord. 2018, 225, 665–670. [Google Scholar] [CrossRef]
- Pan, A.; Keum, N.; Okereke, O.I.; Sun, Q.; Kivimaki, M.; Rubin, R.R.; Hu, F.B. Bidirectional association between depression and metabolic syndrome: A systematic review and meta-analysis of epidemiological studies. Diabetes Care 2012, 35, 1171–1180. [Google Scholar] [CrossRef] [PubMed]
- Lotfaliany, M.; Bowe, S.J.; Kowal, P.; Orellana, L.; Berk, M.; Mohebbi, M. Depression and chronic diseases: Co-occurrence and communality of risk factors. J. Affect. Disord. 2018, 241, 461–468. [Google Scholar] [CrossRef]
- Wang, Z.; Yang, H.; Guo, Z.; Liu, B.; Geng, S. Socio-demographic characteristics and co-occurrence of depressive symptoms with chronic diseases among older adults in China: The China longitudinal ageing social survey. BMC Psychiatry 2019, 19, 310. [Google Scholar] [CrossRef] [PubMed]
- Garfin, D.; Holman, E.; Silver, R. Cumulative exposure to prior collective trauma and acute stress responses to the Boston marathon bombings. Psychol. Sci. 2015, 26, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Roby, D.D.; Lyons, D.E.; Craig, D.P.; Collis, K.; Visser, G.H. Quantifying the effect of predators on endangered species using a bioenergetics approach: Caspian terns and juvenile salmonids in the Columbia River estuary. Can. J. Zool. 2003, 81, 250–265. [Google Scholar] [CrossRef]
- Rasool, S.F.; Chin, T.; Wang, M.; Asghar, A.; Khan, A.; Zhou, L. Exploring the role of organizational support, and critical success factors on renewable energy projects of Pakistan. Energy 2022, 243, 122765. [Google Scholar] [CrossRef]
- Borgogna, N.C.; Brenner, R.E.; McDermott, R.C. Sexuality and gender invariance of the PHQ-9 and GAD-7: Implications for 16 identity groups. J. Affect. Disord. 2021, 278, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Rasool, S.; Ma, D. The Relationship between Workplace Violence and Innovative Work Behavior: The Mediating Roles of Employee Wellbeing. Healthcare 2020, 8, 332. [Google Scholar] [CrossRef]
- Plummer, F.; Manea, L.; Trepel, D.; McMillan, D. Screening for anxiety disorders with the GAD-7 and GAD-2: A systematic review and diagnostic metaanalysis. Gen. Hosp. Psychiatry 2016, 39, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A brief measure for assessing generalized anxiety disorder—The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Bian, Q.; Zhao, Y.; Li, X.; Wang, W.; Du, J.; Zhang, G.; Zhou, Q.; Zhao, M. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry 2014, 36, 539–544. [Google Scholar] [CrossRef]
- Upthegrove, R.; Marwaha, S.; Birchwood, M. Depression and Schizophrenia: Cause, Consequence, or Trans-diagnostic Issue? Schizophr. Bull. 2017, 43, 240–244. [Google Scholar] [CrossRef] [PubMed]
- Kelleher, I.; Corcoran, P.; Keeley, H.; Wigman, J.; Devlin, N.; Ramsay, H.; Wasserman, C.; Carli, V.; Sarchiapone, M.; Hoven, C.; et al. Psychotic symptoms and population risk for suicide attempt: A prospective cohort study. JAMA Psychiatry 2013, 70, 940–948. [Google Scholar] [CrossRef] [PubMed]
- Dutta, R.; Murray, R.M.; Allardyce, J.; Jones, P.B.; Boydell, J. Early risk factors for suicide in an epidemiological first episode psychosis cohort. Schizophr. Res. 2011, 126, 11–19. [Google Scholar] [CrossRef]
- Nyhuis, A.W.; Faries, D.; Ascher-Svanum, H.; Stauffer, V.L.; Kinon, B.J. Predictors of switching antipsychotic medications in the treatment of schizophrenia. BMC Psychiatry 2010, 10, 75. [Google Scholar] [CrossRef]
- Zhong, B.-L.; Luo, W.; Li, H.-M.; Zhang, Q.-Q.; Liu, X.-G.; Li, W.-T.; Li, Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. Int. J. Biol. Sci. 2020, 16, 1745–1752. [Google Scholar] [CrossRef]
- Mueser, K.T.; Deavers, F.; Penn, D.L.; Cassisi, J.E. Psychosocial treatments for schizophrenia. Annu. Rev. Clin. Psychol. 2013, 9, 465–497. [Google Scholar] [CrossRef]
- Fiorillo, A.; Gorwood, P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry 2020, 63, e32. [Google Scholar] [CrossRef] [PubMed]
- Hien, D.; Haas, G.; Cook, H. Gender differences in premorbid social adjustment and intimacy motivation in schizophrenia. J. Clin. Psychol. 1998, 54, 35–48. [Google Scholar] [CrossRef]
- Agerbo, E.; Byrne, M.; Eaton, W.W.; Mortensen, P.B. Marital and Labor Market Status in the Long Run in Schizophrenia. Arch. Gen. Psychiatry 2004, 61, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Eaton, W. Marital status and schizophrenia. Acta Psychiatr. Scand. 1975, 52, 320–329. [Google Scholar] [CrossRef]
- Tien, A.Y. Psychopathologic precursors and sociodemographic risk factors for the schizophrenia syndrome. Arch. Gen. Psychiatry 1992, 49, 37–46. [Google Scholar] [CrossRef]
- Thara, R.; Srinivasan, T.N. Outcome of marriage in schizophrenia. Soc. Psychiatry Psychiatr. Epidemiol. 1997, 32, 416–420. [Google Scholar] [CrossRef] [PubMed]
- Nyer, M.; Kasckow, J.; Fellows, I.; Lawrence, E.C.; Golshan, S.; Solorzano, E.; Zisook, S. The relationship of marital status and clinical characteristics in middle-aged and older patients with schizophrenia and depressive symptoms. Ann. Clin. Psychiatry 2010, 22, 172–179. [Google Scholar]
- Prime, H.; Wade, M.; Browne, D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. 2020, 75, 631–643. [Google Scholar] [CrossRef]
- Walker, E.; Bettes, B.A.; Kain, E.; Harvey, P. Relationship of gender and marital status with symptomatology in psychotic patients. J. Abnorm. Psychol. 1985, 94, 42–50. [Google Scholar] [CrossRef]
- Okun, M.L.; Mancuso, R.A.; Hobel, C.J.; Schetter, C.D.; Coussons-Read, M. Poor sleep quality increases symptoms of depression and anxiety in postpartum women. J. Behav. Med. 2018, 41, 703–710. [Google Scholar] [CrossRef]
- Tsuno, N.; Besset, A.; Ritchie, K. Sleep and depression. J. Clin. Psychiatry 2005, 66, 1254–1269. [Google Scholar] [CrossRef]
- Alvaro, P.K.; Roberts, R.; Harris, J.K. A Systematic Review Assessing Bidirectionality between Sleep Disturbances, Anxiety, and Depression. Sleep 2013, 36, 1059–1068. [Google Scholar] [CrossRef] [PubMed]
- Ford, D.E.; Cooper-Patrick, L. Sleep disturbances and mood disorders: An epidemiologic perspective. Depress. Anxiety 2001, 14, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Breslau, N.; Roth, T.; Rosenthal, L.; Andreski, P. Sleep disturbance and psychiatric disorders: A longitudinal epidemiological study of young Adults. Biol. Psychiatry 1996, 39, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef] [PubMed]
- Özdin, S.; Bayrak Özdin, Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int. J. Soc. Psychiatry 2020, 66, 504–511. [Google Scholar] [CrossRef]
- Bakshi, A.J.; Deshmukh, J.; Kumar, S. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. Br. J. Guid. Couns. 2021, 49, 633–636. [Google Scholar] [CrossRef]
- Seghi, F.; Barbini, B.; Franchini, L.; Colombo, C. The challenge of mental health during COVID-19 outbreak: Experience from metropolitan area of Milan. Eur. Arch. Psychiatry Clin. Neurosci. 2021, 271, 401–402. [Google Scholar] [CrossRef]
| Severity | GAD-7 | Severity | PHQ-9 | ||
|---|---|---|---|---|---|
| n | (%) | n | (%) | ||
| Mild | 12,612 | 83.2 | Mild | 9867 | 65.1 |
| Moderate | 2377 | 15.7 | Moderate | 3902 | 25.7 |
| Severe | 176 | 1.2 | Severe | 1249 | 8.2 |
| Extremely serious | 147 | 1.0 | |||
| Total | 15,165 | 100 | 15,165 | 100 | |
| Characteristic | n (%) | GAD-7 (Mean ± SD) | F/t/χ2 | p | PHQ-9 (Mean ± SD) | F/t/χ2 | p |
|---|---|---|---|---|---|---|---|
| Sex | −2.03 | 0.042 | −3.27 | 0.001 | |||
| Male (%) | 7010 (46.2) | 8.1 ± 2.1 | 10.3 ± 2.5 | ||||
| Female (%) | 8155 (53.8) | 8.2 ± 2.2 | 10.5 ± 2.8 | ||||
| Age (years) | 2.84 | 0.014 | 1.79 | 0.111 | |||
| ≤18 | 24 (0.2) | 8.1 ± 1.9 | 10.2 ± 2.3 | ||||
| 19~29 | 508 (3.3) | 8.0 ± 2.2 | 10.3 ± 2.9 | ||||
| 30~39 | 1647 (10.9) | 8.3 ± 2.3 | 10.6 ± 3.0 | ||||
| 40~49 | 2642 (17.4) | 8.2 ± 2.1 | 10.4 ± 2.6 | ||||
| 50~59 | 4433 (29.2) | 8.1 ± 2.1 | 10.4 ± 2.6 | ||||
| ≥60 | 5911 (39.0) | 8.1 ± 2.1 | 10.4 ± 2.7 | ||||
| Marital status | 1.69 | 0.092 | 0.90 | 0.368 | |||
| With partner | 8607 (56.8) | 8.2 ± 2.2 | 10.4 ± 2.7 | ||||
| Without partner | 6558 (43.2) | 8.1 ± 2.1 | 10.4 ± 2.6 | ||||
| Education (years) | 4.08 | 0.007 | 0.38 | 0.769 | |||
| Illiteracy | 2528 (16.7) | 8.1 ± 2.2 | 10.4 ± 2.8 | ||||
| Primary school | 4786 (31.6) | 8.1 ± 2.1 | 10.4 ± 2.7 | ||||
| Junior high school | 7069 (46.6) | 8.2 ± 2.1 | 10.4 ± 2.6 | ||||
| University and above | 782 (5.2) | 8.3 ± 2.2 | 10.4 ± 2.5 | ||||
| Sleep status | 158.87 | <0.001 | 284.00 | <0.001 | |||
| Better | 4256 (28.1) | 7.8 ± 1.6 | 9.8 ± 1.8 | ||||
| Normal | 10,243 (67.5) | 8.2 ± 2.2 | 10.6 ± 2.7 | ||||
| Poor | 666 (4.4) | 9.1 ± 3.2 | 12.0 ± 4.4 | ||||
| Accompanying other long-standing disease | 4.18 | <0.001 | 6.86 | <0.001 | |||
| Yes | 2648 (17.5) | 8.3 ± 2.3 | 10.7 ± 3.0 | ||||
| No | 12,517 (82.5) | 8.1 ± 2.1 | 10.3 ± 2.6 |
| n (%) | GAD-7 (Mean ± SD) | F/t | p | PHQ-9 (Mean ± SD) | F/t | p | |
|---|---|---|---|---|---|---|---|
| Concern about COVID-19 | 8.17 | <0.001 | 2.29 | 0.022 | |||
| Yes | 12,722 (83.9) | 8.2 ± 2.1 | 10.4 ± 2.6 | ||||
| No | 2443 (16.1) | 7.8 ± 2.0 | 10.3 ± 2.9 | ||||
| Total | 15,165 (100) | ||||||
| The degree of concern about COVID-19 | 93.19 | <0.001 | 95.30 | <0.001 | |||
| Less | 12,055 (79.5) | 8.0 ± 2.0 | 10.2 ± 2.5 | ||||
| General | 2803 (18.5) | 8.6 ± 2.5 | 11.0 ± 3.1 | ||||
| More | 307 (2.0) | 8.4 ± 2.8 | 10.5 ± 3.2 | ||||
| Total | 15,615 (100) |
| Anxiety a | Depression b | ||||
|---|---|---|---|---|---|
| OR(95% CI) | p | OR(95% CI) | p | ||
| Age | ≤18 | 1.14 (0.39–3.4) | 0.811 | 0.86 (0.35–2.09) | 0.734 |
| 19~29 | 0.94 (0.72–1.21) | 0.620 | 0.92 (0.75–1.12) | 0.387 | |
| 30~39 | 1.26 (1.09–1.46) | 0.002 | 1.23 (1.09–1.38) | 0.001 | |
| 40~49 | 1.16 (1.03–1.32) | 0.018 | 1.04 (0.94–1.15) | 0.488 | |
| 50~59 | 1.03 (0.92–1.15) | 0.614 | 1.01 (0.93–1.10) | 0.786 | |
| ≥60 | 1.00 | 1.00 | |||
| Sleep status | Better | 0.23 (0.19–0.28) | <0.001 | 0.26 (0.22–0.31) | <0.001 |
| Normal | 0.47 (0.40–0.56) | <0.001 | 0.54 (0.46–0.63) | <0.001 | |
| Poor | 1.00 | 1.00 | |||
| Accompanying other long-standing diseases | Yes | 1.15 (1.03–1.29) | 0.013 | 1.29 (1.18–1.42) | <0.001 |
| No | 1.00 | 1.00 | |||
| Concerning about COVID-19 | Yes | 1.44 (1.26–1.65) | <0.001 | 1.49 (1.34–1.64) | <0.001 |
| No | 1.00 | 1.00 | |||
| The degree of concern about COVID-19 | Less | 0.78 (0.57–1.05) | 0.095 | 0.85 (0.67–1.08) | 0.188 |
| General | 1.38 (1.01–1.87) | 0.041 | 1.54 (1.20–1.99) | 0.001 | |
| More | 1.00 | 1.00 | |||
| Anxiety a | Depression b | ||||
|---|---|---|---|---|---|
| OR(95% CI) | p | OR(95% CI) | p | ||
| Male (n = 7010) | |||||
| Marital status | With partner | / | / | 0.88 (0.79–0.97) | 0.013 |
| Without partner | / | / | 1.00 | ||
| Sleep status | Better | 0.30 (0.22–0.41) | <0.001 | 0.31 (0.23–0.40) | <0.001 |
| Normal | 0.54 (0.41–0.72) | <0.001 | 0.61 (0.47–0.79) | <0.001 | |
| Poor | 1.00 | 1.00 | |||
| Accompanying other long-standing diseases | Yes | / | / | 1.37 (1.20–1.57) | <0.001 |
| No | / | / | 1.00 | ||
| Concerning about COVID-19 | Yes | 1.36 (1.12–1.65) | 0.002 | 1.48 (1.28–1.72) | <0.001 |
| No | 1.00 | 1.00 | |||
| The degree of concern about COVID-19 | Less | 0.66 (0.44–1.01) | 0.055 | 0.69 (0.49–0.97) | 0.032 |
| General | 1.18 (0.77–1.82) | 0.443 | 1.33 (0.94–1.90) | 0.112 | |
| More | 1.00 | 1.00 | |||
| Female (n = 8155) | |||||
| Sleep status | Better | 0.20 (0.16–0.26) | <0.001 | 0.24 (0.19–0.30) | <0.001 |
| Normal | 0.44 (0.35–0.55) | <0.001 | 0.50 (0.41–0.61) | <0.001 | |
| Poor | 1.00 | 1.00 | |||
| Accompanying other long-standing diseases | Yes | 1.16 (1.00–1.34) | 0.046 | 1.21 (1.07–1.36) | 0.002 |
| No | 1.00 | 1.00 | |||
| Concerning about COVID-19 | Yes | 1.55 (1.29–1.86) | <0.001 | 1.53 (1.33–1.75) | <0.001 |
| No | 1.00 | 1.00 | |||
| The degree of concern about COVID-19 | Less | 0.85 (0.55–1.30) | 0.454 | 1.00 (0.71–1.41) | 0.997 |
| General | 1.55 (1.00–2.40) | 0.050 | 1.75 (1.23–2.50) | 0.002 | |
| More | 1.00 | 1.00 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, S.; Sun, X.; Zhu, Q.; Zhao, Y.; Tang, J.; Song, H. Factors Influencing the Level of Depression and Anxiety of Community-Dwelling Patients with Schizophrenia in China during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 4376. https://doi.org/10.3390/ijerph20054376
Chen S, Sun X, Zhu Q, Zhao Y, Tang J, Song H. Factors Influencing the Level of Depression and Anxiety of Community-Dwelling Patients with Schizophrenia in China during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2023; 20(5):4376. https://doi.org/10.3390/ijerph20054376
Chicago/Turabian StyleChen, Shanshan, Xiaohua Sun, Qisha Zhu, Yuan Zhao, Jinsong Tang, and Haidong Song. 2023. "Factors Influencing the Level of Depression and Anxiety of Community-Dwelling Patients with Schizophrenia in China during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 20, no. 5: 4376. https://doi.org/10.3390/ijerph20054376
APA StyleChen, S., Sun, X., Zhu, Q., Zhao, Y., Tang, J., & Song, H. (2023). Factors Influencing the Level of Depression and Anxiety of Community-Dwelling Patients with Schizophrenia in China during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 20(5), 4376. https://doi.org/10.3390/ijerph20054376







