Knowledge of Medical Imaging Professionals on Healthcare-Associated Infections: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
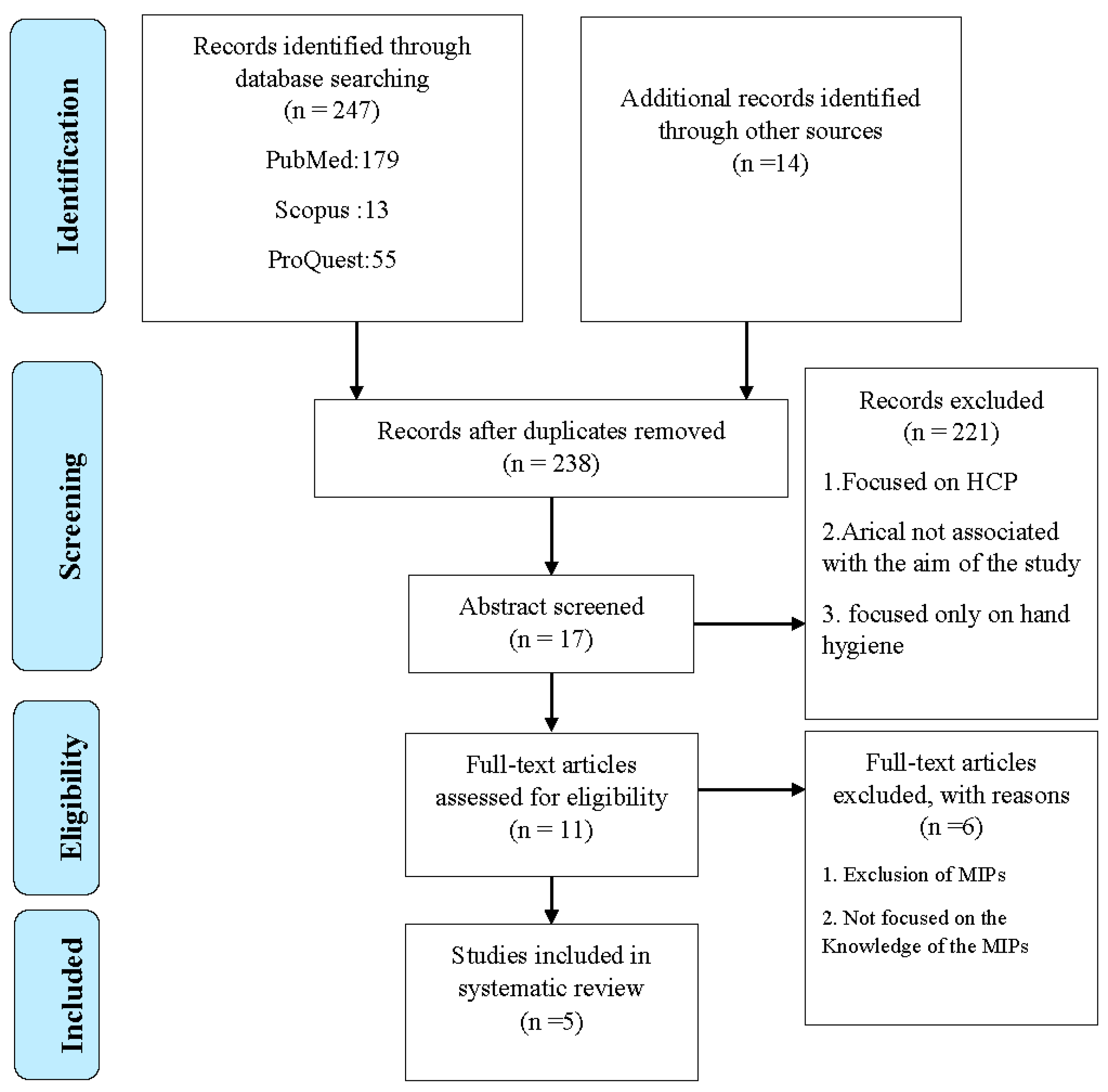
2. Materials and Methods
2.1. Search Strategy
2.2. Selection Criteria
2.2.1. Selection of the Studies
2.2.2. Data Extraction
2.2.3. Risk of Bias
2.2.4. Criteria for Inclusion and Exclusion
2.2.5. Data Analysis
3. Results
3.1. Characteristics of the Included Studies
3.2. Methodological Quality
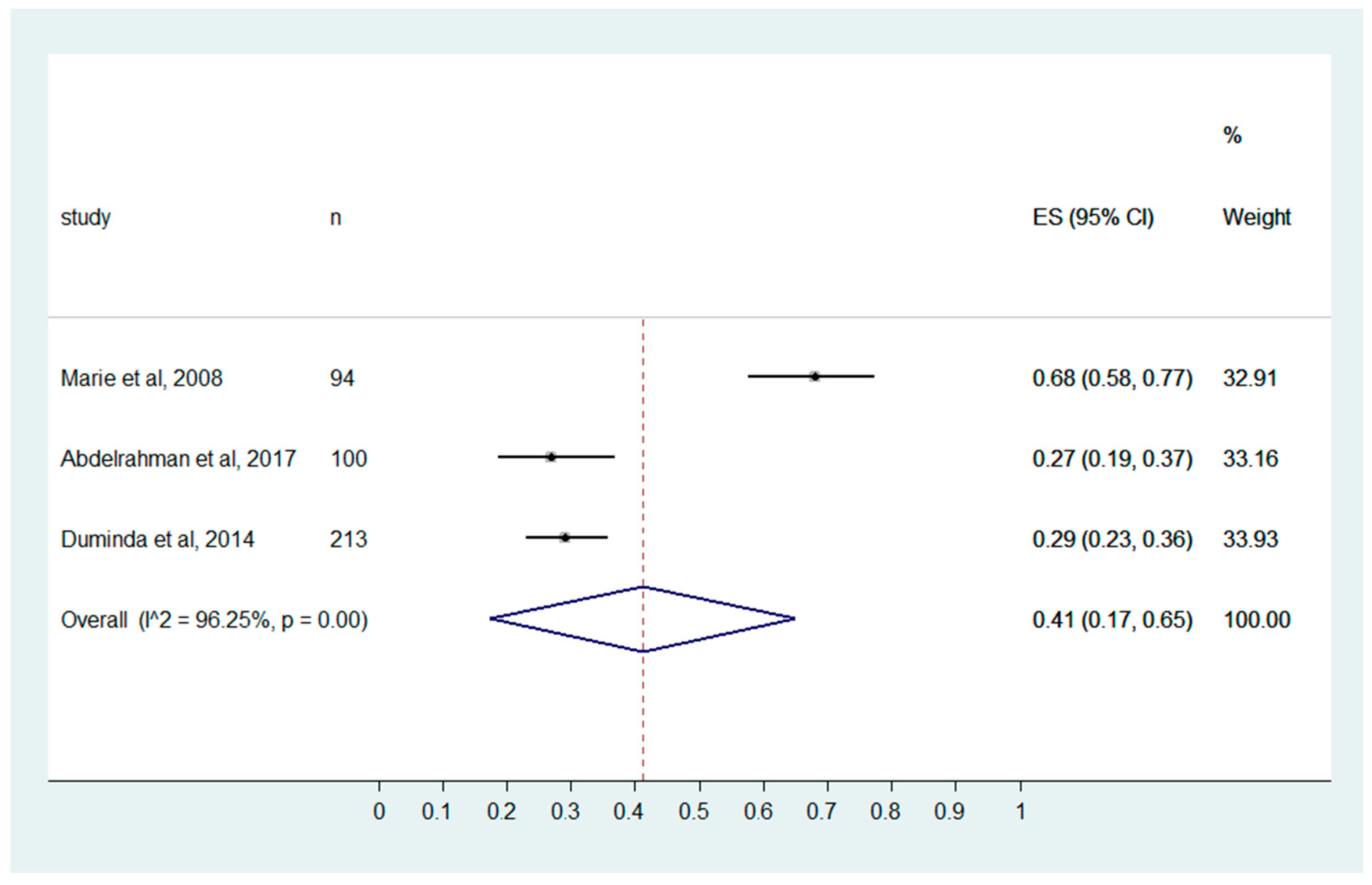
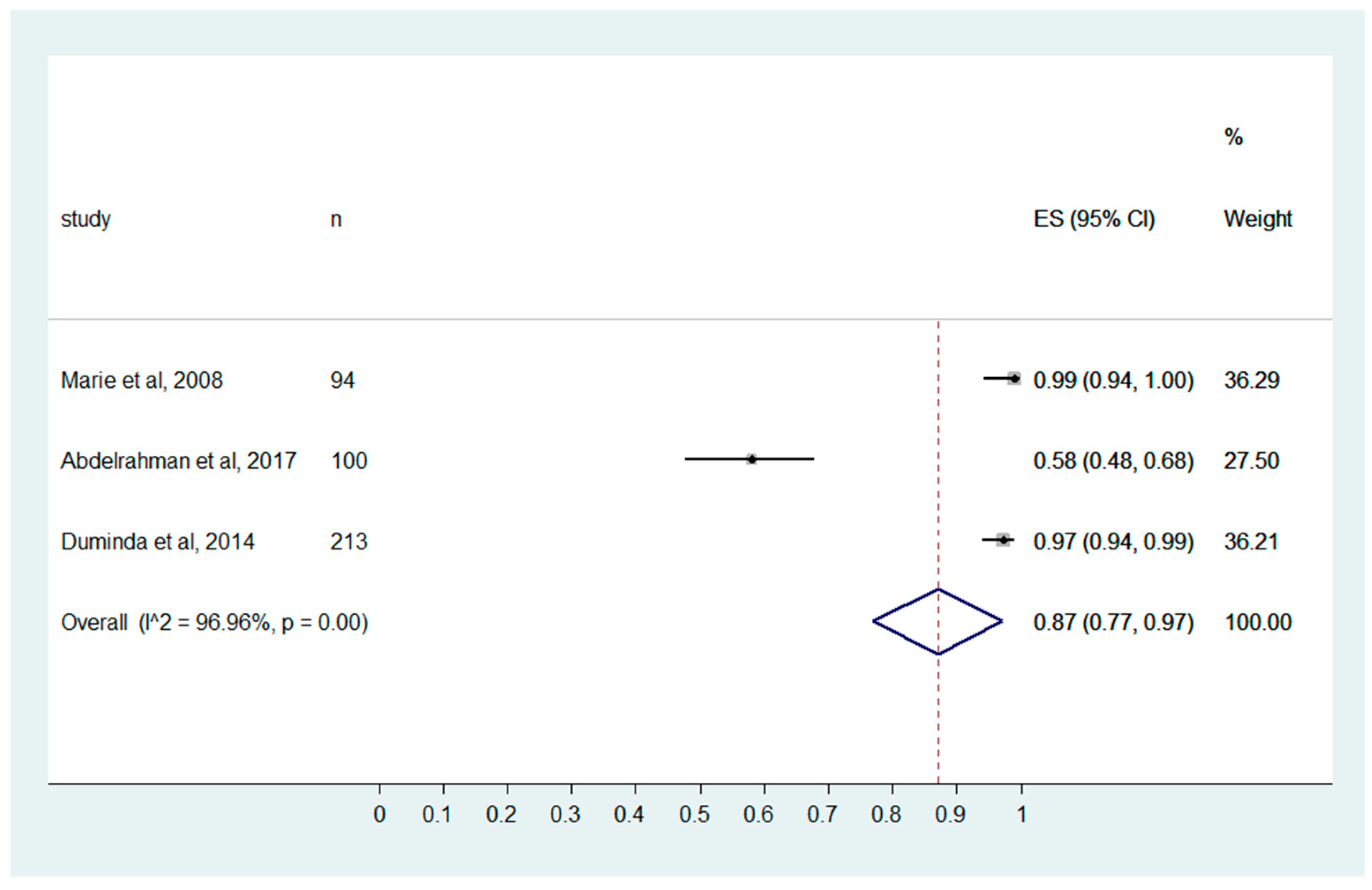
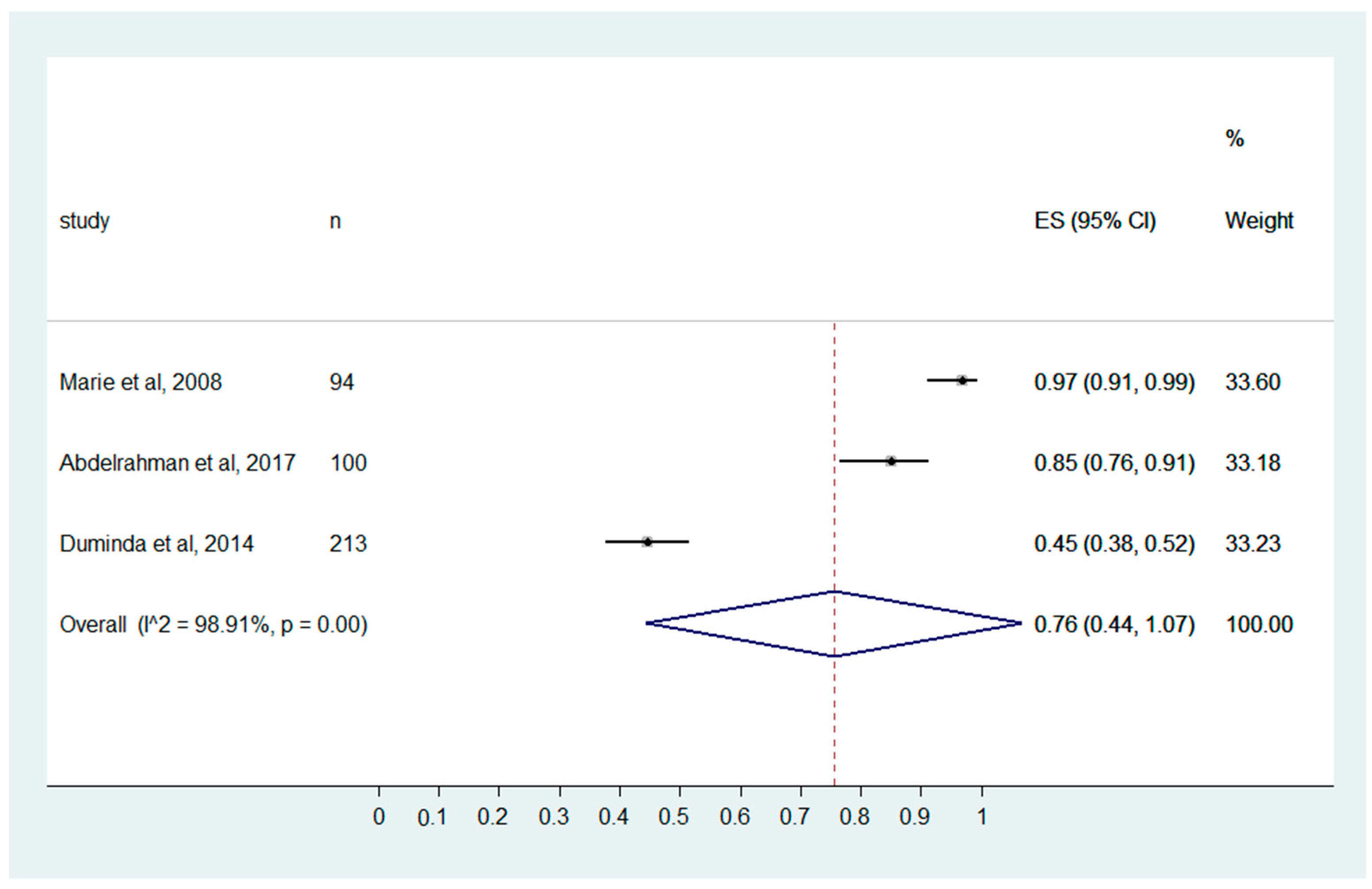
3.3. Meta-Analysis
3.4. Environment and HCIAs
3.5. Gloves Recommendation during the Procedure
3.6. Precaution Standards
4. Discussion
4.1. The Spread of Infection
4.2. Knowledge of Hand and Machine Hygiene in RD
4.3. Recommendations of Precaution Standards to Protect the Patients and HCP
4.4. Invasive Procedures and HCIAs
4.5. Limitations of the Included Studies
4.6. Limitation of the Present Review
4.7. Future Recommendations from the Present Review
4.8. Future Scopes
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kumar, B.; Manuja, A.; Gulati, B.; Virmani, N.; Tripathi, B.N. Zoonotic Viral Diseases of Equines and Their Impact on Human and Animal Health. Open Virol. J. 2018, 12, 80–98. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. N. Eng. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef]
- Paules, C.I.; Marston, H.D.; Fauci, A.S. Coronavirus Infections—More Than Just the Common Cold. JAMA 2020, 323, 707. [Google Scholar] [CrossRef] [PubMed]
- Qu, J.; Yang, W.; Yang, Y.; Qin, L.; Yan, F. Infection Control for CT Equipment and Radiographers’ Personal Protection During the Coronavirus Disease (COVID-19) Outbreak in China. Am. J. Roentgenol. 2020, 215, 940–944. [Google Scholar] [CrossRef] [PubMed]
- van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef]
- Hietala, S.K.; Hullinger, P.J.; Crossley, B.M.; Kinde, H.; Ardans, A.A. Environmental Air Sampling to Detect Exotic Newcastle Disease Virus in Two California Commercial Poultry Flocks. J. Vet. Diagn. Investig. 2005, 17, 198–200. [Google Scholar] [CrossRef]
- Li, Y.; Huang, X.; Yu, I.T.S.; Wong, T.W.; Qian, H. Role of Air Distribution in SARS Transmission during the Largest Nosocomial Outbreak in Hong Kong. Indoor Air 2005, 15, 83–95. [Google Scholar] [CrossRef]
- Hefzy, E.M.; Wegdan, A.A.; Abdel Wahed, W.Y. Hospital Outpatient Clinics as a Potential Hazard for Healthcare Associated Infections. J. Infect. Public Health 2016, 9, 88–97. [Google Scholar] [CrossRef]
- Marcel, J.-P.; Alfa, M.; Baquero, F.; Etienne, J.; Goossens, H.; Harbarth, S.; Hryniewicz, W.; Jarvis, W.; Kaku, M.; Leclercq, R.; et al. Healthcare-Associated Infections: Think Globally, Act Locally. Clin. Microbiol. Infect. 2008, 14, 895–907. [Google Scholar] [CrossRef]
- Ilyas, F.; Burbridge, B.; Babyn, P. Health Care-Associated Infections and the Radiology Department. J. Med. Imaging Radiat. Sci. 2019, 50, 596–606.e1. [Google Scholar] [CrossRef] [PubMed]
- Levin, P.D.; Shatz, O.; Sviri, S.; Moriah, D.; Or-Barbash, A.; Sprung, C.L.; Moses, A.E.; Block, C. Contamination of Portable Radiograph Equipment with Resistant Bacteria in the ICU. Chest 2009, 136, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Ustünsöz, B. Hospital Infections in Radiology Clinics. Diagn. Interv. Radiol. 2005, 11, 5–9. [Google Scholar] [PubMed]
- Lawson, S.R.; Sauer, R.; Loritsch, M.B. Bacterial Survival on Radiographic Cassettes. Radiol. Technol. 2002, 73, 507–510. [Google Scholar]
- Busi Rizzi, E.; Puro, V.; Schinina’, V.; Nicastri, E.; Petrosillo, N.; Ippolito, G. Radiographic Imaging in Ebola Virus Disease: Protocol to Acquire Chest Radiographs. Eur. Radiol. 2015, 25, 3368–3371. [Google Scholar] [CrossRef]
- Buerke, B.; Mellmann, A.; Stehling, C.; Wessling, J.; Heindel, W.; Juergens, K.U. Microbiologic Contamination of Automatic Injectors at MDCT: Experimental and Clinical Investigations. AJR Am. J. Roentgenol. 2008, 191, W283–W287. [Google Scholar] [CrossRef]
- Wooltorton, E. Medical Gels and the Risk of Serious Infection. CMAJ 2004, 171, 1348. [Google Scholar] [CrossRef]
- Buerke, B.; Puesken, M.; Mellmann, A.; Schuelke, C.; Knauer, A.; Heindel, W.; Wessling, J. Automatic MDCT Injectors: Hygiene and Efficiency of Disposable, Prefilled, and Multidosing Roller Pump Systems in Clinical Routine. AJR Am. J. Roentgenol. 2011, 197, W226–W232. [Google Scholar] [CrossRef]
- Epidemiology Working Group for NCIP Epidemic Response, C.C. for D.C. and P. [The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) in China]. Zhonghua Liu Xing Bing Xue Za Zhi 2020, 41, 145–151. [Google Scholar] [CrossRef]
- Nienhaus, A.; Kesavachandran, C.; Wendeler, D.; Haamann, F.; Dulon, M. Infectious Diseases in Healthcare Workers-an Analysis of the Standardised Data Set of a German Compensation Board. J. Occup. Med. Toxicol. 2012, 7, 8. [Google Scholar] [CrossRef]
- Schmidt, J.M. Stopping the Chain of Infection in the Radiology Suite. Radiol. Technol. 2012, 84, 31–48; qiuz 49–51. Available online: https://pubmed.ncbi.nlm.nih.gov/22988261/ (accessed on 11 January 2023). [PubMed]
- Schmidt, J.M. Stopping the Chain of Infection in the Radiology Suite. Radiol. Technol. 2020, 91, 489–493. Available online: https://pubmed.ncbi.nlm.nih.gov/32381669/ (accessed on 11 January 2023).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- El-Gilany, A.H.; Badawy, K.; Sarraf, B. Knowledge of Health Care Providers Os Standard Precautions and Infection Controla t Studentshospital, Mansoura University, Egypt. TAF Prev. Med. Bull. 2012, 11, 23–28. [Google Scholar] [CrossRef]
- Abdelrahman, M.A.; Alhasan, M.; Alewaidat, H.; Rawashdeh, M.A.; al Mousa, D.S.; Almhdawi, K.A. Knowledge of Nosocomial Infection Control Practices among Radiographers in Jordan. Radiography 2017, 23, 298–304. [Google Scholar] [CrossRef]
- Baird, M.; Zito, N.; Howden, L. The Awareness and Implementation of Infection Control Procedures among Radiographers. Radiogr. Off. J. Aust. Inst. Radiogr. 2002, 49, 61–65. [Google Scholar]
- Cobb, A.; Lazar, B. Mobile Device Usage Contributes to Nosocomial Infections. Radiol. Technol. 2020, 91, 303–307. [Google Scholar]
- Crofton, C.C.; Foley, S.J. An Investigation of Radiographers’ Mobile Phone Use and the Success of an Awareness Campaign at Reducing the Nosocomial Infection Risks. Radiography 2018, 24, 57–63. [Google Scholar] [CrossRef]
- Jayasinghe, R.D.; Weerakoon, B.S. Prevention of Nosocomial Infections and Standard Precautions: Knowledge and Practice among Radiographers in Sri Lanka -. J. Med. Allied Sci. 2014, 4, 9–16. [Google Scholar]
- Nyirenda, D.; ten Ham-Baloyi, W.; Williams, R.; Venter, D. Knowledge and Practices of Radiographers Regarding Infection Control in Radiology Departments in Malawi. Radiography 2018, 24, e56–e60. [Google Scholar] [CrossRef]
- Smith, A.; Lodge, T.D. Can Radiographic Equipment Be Contaminated by Micro-Organisms to Become a Reservoir for Cross Infection? Synergy 2004, 12–17. Available online: https://www.proquest.com/docview/212420127?pq-origsite=gscholar&fromopenview=true (accessed on 11 January 2023).
- Tavolacci, M.-P.; Ladner, J.; Bailly, L.; Merle, V.; Pitrou, I.; Czernichow, P. Prevention of Nosocomial Infection and Standard Precautions: Knowledge and Source of Information among Healthcare Students. Infect. Control Hosp. Epidemiol. 2008, 29, 642–647. [Google Scholar] [CrossRef] [PubMed]
- Temesgen, C.; Demissie, M. Knowledge and Practice of Tuberculosis Infection Control among Health Professionals in Northwest Ethiopia; 2011. BMC Health Serv. Res. 2014, 14, 593. [Google Scholar] [CrossRef] [PubMed]
- Tvedt, C.; Bukholm, G. Healthcare Workers’ Self-Reported Effect of an Interventional Programme on Knowledge and Behaviour Related to Infection Control. Qual. Saf. Health Care 2010, 19, e7. [Google Scholar] [CrossRef] [PubMed]
- Aso, M.; Kato, K.; Yasuda, M.; Takahashi, T.; Say, S.; Fujimura, K.; Kuroki, K.; Nakazawa, Y. [Hand Hygiene during Mobile X-Ray Imaging in the Emergency Room]. Nihon Hoshasen Gijutsu Gakkai Zasshi 2011, 67, 793–799. [Google Scholar] [CrossRef] [PubMed]
- Giacometti, M.; Gualano, M.R.; Bert, F.; Minniti, D.; Bistrot, F.; Grosso, M.; Siliquini, R. Microbiological Contamination of Radiological Equipment. Acta Radiol. 2014, 55, 1099–1103. [Google Scholar] [CrossRef] [PubMed]
- Olu, O.; Kargbo, B.; Kamara, S.; Wurie, A.H.; Amone, J.; Ganda, L.; Ntsama, B.; Poy, A.; Kuti-George, F.; Engedashet, E.; et al. Epidemiology of Ebola Virus Disease Transmission among Health Care Workers in Sierra Leone, May to December 2014: A Retrospective Descriptive Study. BMC Infect. Dis. 2015, 15, 416. [Google Scholar] [CrossRef] [PubMed]
- Picton-Barnes, D.; Pillay, M.; Lyall, D. A Systematic Review of Healthcare-Associated Infectious Organisms in Medical Radiation Science Departments. Healthcare 2020, 8, 80. [Google Scholar] [CrossRef]
- Carling, P.C.; Parry, M.F.; von Beheren, S.M. Healthcare Environmental Hygiene Study Group Identifying Opportunities to Enhance Environmental Cleaning in 23 Acute Care Hospitals. Infect. Control Hosp. Epidemiol. 2008, 29, 1–7. [Google Scholar] [CrossRef]
- Kim, J.-S.; Kim, H.-S.; Park, J.-Y.; Koo, H.-S.; Choi, C.-S.; Song, W.; Cho, H.C.; Lee, K.M. Contamination of X-Ray Cassettes with Methicillin-Resistant Staphylococcus Aureus and Methicillin-Resistant Staphylococcus Haemolyticus in a Radiology Department. Ann. Lab. Med. 2012, 32, 206–209. [Google Scholar] [CrossRef]
- Shelly, M.J.; Scanlon, T.G.; Ruddy, R.; Hannan, M.M.; Murray, J.G. Meticillin-Resistant Staphylococcus Aureus (MRSA) Environmental Contamination in a Radiology Department. Clin. Radiol. 2011, 66, 861–864. [Google Scholar] [CrossRef]
- Tugwell, J.; Maddison, A. Radiographic Markers–A Reservoir for Bacteria? Radiography 2011, 17, 115–120. [Google Scholar] [CrossRef]
- Bello, A.I.; Asiedu, E.N.; Adegoke, B.O.A.; Quartey, J.N.A.; Appiah-Kubi, K.O.; Owusu-Ansah, B. Nosocomial Infections: Knowledge and Source of Information among Clinical Health Care Students in Ghana. Int. J. Gen. Med. 2011, 4, 571–574. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.Y.; Philip, A.; Richter, M.D.; Gupta, S.; Lessne, M.L.; Kim, C.Y. Prevention and Management of Infectious Complications of Percutaneous Interventions. Semin. Intervent. Radiol. 2015, 32, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Boyle, H.; Strudwick, R.M. Do Lead Rubber Aprons Pose an Infection Risk? Radiography 2010, 16, 297–303. [Google Scholar] [CrossRef]
- Khan, W.; Sullivan, K.L.; McCann, J.W.; Gonsalves, C.F.; Sato, T.; Eschelman, D.J.; Brown, D.B. Moxifloxacin Prophylaxis for Chemoembolization or Embolization in Patients with Previous Biliary Interventions: A Pilot Study. AJR Am. J. Roentgenol. 2011, 197, W343–W345. [Google Scholar] [CrossRef]
- Paul, M.; Leibovici, L. Observational Studies Examining Patient Management in Infectious Diseases. Clin. Microbiol. Infect. 2017, 23, 127–128. [Google Scholar] [CrossRef][Green Version]
- Concato, J. Observational versus Experimental Studies: What’s the Evidence for a Hierarchy? NeuroRx 2004, 1, 341–347. [Google Scholar] [CrossRef]

| Sl. No. | Search |
|---|---|
| 1 | “(nosocomial infections or hospital-acquired infections or healthcare-associated infections)” |
| 2 | “(knowledge or education or understanding or awareness)” |
| 3 | “ (radiographer or radiologist technologist).” |
| 1 AND 3 | |
| 1 AND 2 AND 3 | |
| 4 | “ (nosocomial Infections)” |
| 5 | “(knowledge) “ |
| 6 | “ (radiographer)” |
| 4 AND 5 AND 6 |
| Criteria’s | Score |
|---|---|
| Clarity of the questioners | +/− |
| Details of the study methodology | +/− |
| Details of data collection | +/− |
| Research content | +/− |
| Data analysis | +/− |
| Result revenant to the study’s objective | +/− |
| Ethics approval | +/− |
| Overall | ++/+/− |
| Author | |||||
|---|---|---|---|---|---|
| M.A. Abdelrahman et al. [25] | El-Gilany et al. [24] | Jayasinghe et al. [29] | Marie-Pierre et al. [32] | Nyirenda, D. et al. [30] | |
| Year | 2017 | 2012 | 2014 | 2008 | 2018 |
| Country | Jordan | Egypt | Sri Lanka | France | Malawi |
| Samples | 128 | 14 | 213 | 94 | 62 |
| Study design | CS | CS | CS | CS | CS |
| No of items | 41 | 50 | 18 | 25 | 36 |
| Ethical approval | Yes | Yes | Yes | Yes | Yes |
| Mode of data collection | SA | SA | SA | SA | SA |
| Validation | Yes | Yes | Yes | Yes | Yes |
| Items specific to radiology | Yes | No | No | No | No |
| Environment and HCAIs | Poor | * | Poor | poor | Good |
| Intervention and HCAIs | Good | * | Moderate | Good | * |
| Standard precaution and HCAIs | Good | Moderate | Good | Good | Moderate |
| Gloves recommend and HCAIs | Poor | * | Poor | Moderate | * |
| Study | Items | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | Overall | |
| M.A. Abdelrahman et al. [25] | + | + | + | + | + | + | + | ++ |
| El-Gilany et al. [24] | + | + | + | + | + | + | + | ++ |
| Jayasingheet al. [29] | + | + | + | + | - | + | + | ++ |
| Marie-Pierre et al. [32] | + | + | + | + | + | + | + | ++ |
| Nyirenda, D. et al. [30] | + | + | + | + | - | + | + | ++ |
| Outcome Measure | Effect Size (95% CI) |
|---|---|
| “The environment (air, water, inert surfaces) is the major source of bacteria responsible for nosocomial infection.” | 0.18 (0.08, 0.28) |
| “Invasive procedures increase the risk of nosocomial infection.” | 0.76 (0.44, 1.07) |
| “Medical Imaging Professionals knowledge on standard precautions recommend the use of gloves.” | 0.41 (0.17, 0.65) |
| “Precaution standards to protect the patients and the healthcare workers.” | 0.87 (0.77, 0.97) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sukumar, S.; Saha, S.; Dkhar, W.; Panakkal, N.C.; Nair, V.T.; Bommasamudram, T.; Vaishali, K.; Nagaraja, R.; Ravichandran, S.; Kadavigere, R. Knowledge of Medical Imaging Professionals on Healthcare-Associated Infections: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 4326. https://doi.org/10.3390/ijerph20054326
Sukumar S, Saha S, Dkhar W, Panakkal NC, Nair VT, Bommasamudram T, Vaishali K, Nagaraja R, Ravichandran S, Kadavigere R. Knowledge of Medical Imaging Professionals on Healthcare-Associated Infections: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2023; 20(5):4326. https://doi.org/10.3390/ijerph20054326
Chicago/Turabian StyleSukumar, Suresh, Shovan Saha, Winniecia Dkhar, Nitika C. Panakkal, Visakh Thrivikraman Nair, Tulasiram Bommasamudram, K Vaishali, Ravishankar Nagaraja, Sneha Ravichandran, and Rajagopal Kadavigere. 2023. "Knowledge of Medical Imaging Professionals on Healthcare-Associated Infections: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 20, no. 5: 4326. https://doi.org/10.3390/ijerph20054326
APA StyleSukumar, S., Saha, S., Dkhar, W., Panakkal, N. C., Nair, V. T., Bommasamudram, T., Vaishali, K., Nagaraja, R., Ravichandran, S., & Kadavigere, R. (2023). Knowledge of Medical Imaging Professionals on Healthcare-Associated Infections: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 20(5), 4326. https://doi.org/10.3390/ijerph20054326







