Psychosocial and Health-Related Behavioral Outcomes of a Work Readiness HIV Peer Worker Training Program
Abstract
1. Introduction
1.1. HIV Peer Intervention and Peer Worker Training
1.2. Employment as a Social Determinant of Health
1.3. Vocational Development and Intervention for People Living with HIV
2. Methods
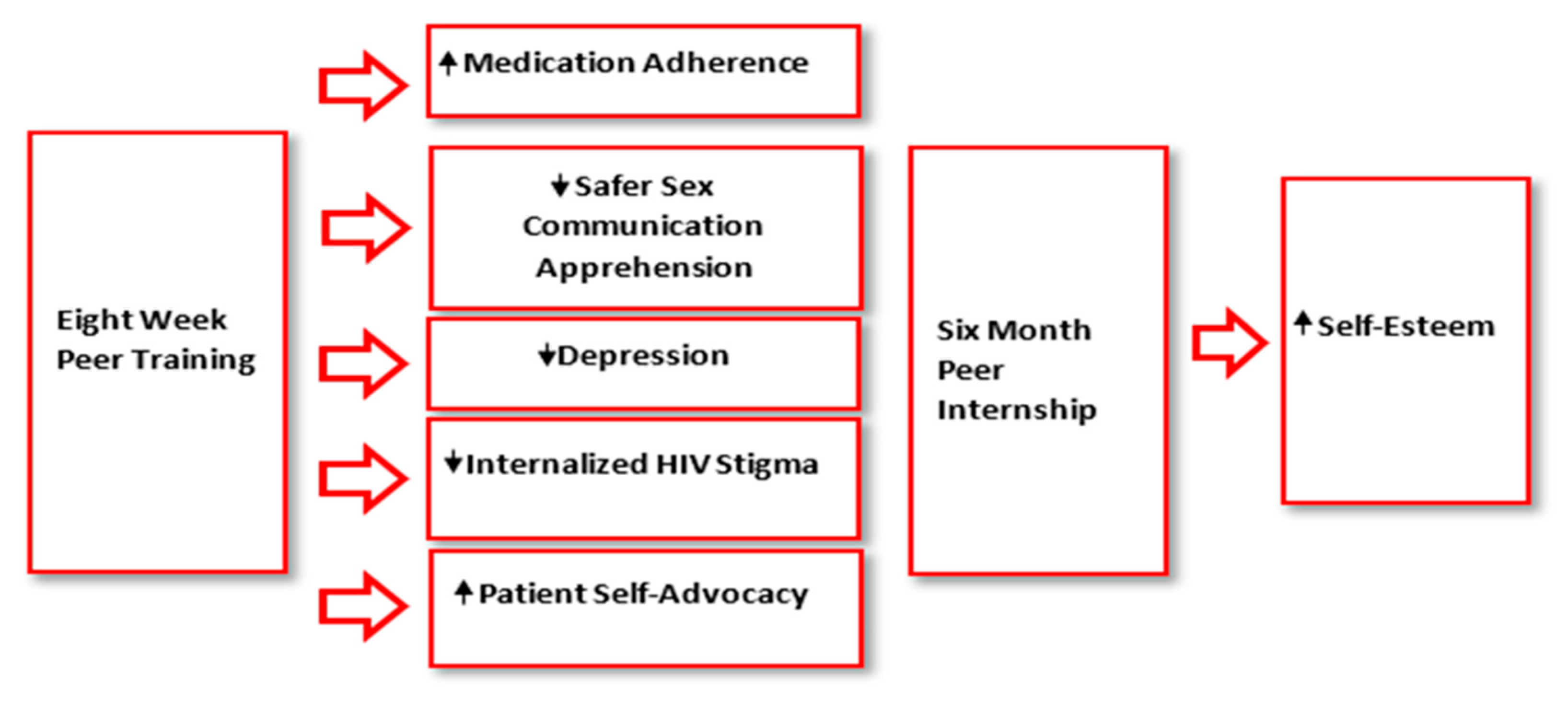
2.1. Peer Worker Training Program
2.2. Peer Internship Program
2.3. Procedures
2.4. Participants
2.5. Measures
2.6. Statistical Analysis
3. Results
3.1. Sociodemographic, Health, and Job History of Program Participants
3.2. Psychosocial Inventories at Baseline
3.3. Psychosocial and Health-Related Behavioral Outcome Inventories at Training Completion
3.4. Psychosocial Inventories for Peer Internship Participants
4. Discussion
4.1. Psychosocial Outcomes of Peer Worker Training
4.2. Health-Related Behavioral Outcomes of Peer Worker Training
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, K.; Lekas, H.-M. AIDS as a chronic illness: Psychosocial implications. Aids 2002, 16, S69–S76. [Google Scholar] [CrossRef] [PubMed]
- Conyers, L.M. Expanding Understanding of HIV/AIDS and Employment: Perspectives of Focus Groups. Rehabil. Couns. Bull. 2004, 48, 5–18. [Google Scholar] [CrossRef]
- Work Health Organization (WHO). Social Determinants of Health. Available online: https://www.who.int/health-topics/social-determinants-of-health (accessed on 10 October 2022).
- National Prevention Information Network. Establishing a Holistic Framework to Reduce Inequities in HIV, Viral Hepatitis, STDs, and Tuberculosis in the United States—Connecting Public Health Professionals with Trusted Information and Each Other. Available online: https://npin.cdc.gov/publication/establishing-holistic-framework-reduce-inequities-hiv-viral-hepatitis-stds-and (accessed on 14 November 2022).
- Center for Disease Control and Prevention (CDC). Behavioral and Clinical Characteristics—Persons Living with Diagnosed HIV Infection-Medical Monitoring Project. Available online: https://www.cdc.gov/hiv/library/reports/hiv-surveillance-special-reports/no-28/index.html (accessed on 14 November 2022).
- Bruyère, S.M. Labor and Employment Relations Association Series. Employment and Disability: Issues, Innovations, and Opportunities. Available online: www.leraweb.org (accessed on 28 March 2021).
- Substance Abuse and Mental Health Services Administration. Peer Support Workers for Those in Recovery. Available online: https://www.samhsa.gov/brss-tacs/recovery-support-tools/peers (accessed on 10 November 2022).
- Medley, A.; Kennedy, C.; O’Reilly, K.; Sweat, M. Effectiveness of Peer Education Interventions for HIV Prevention in Developing Countries: A Systematic Review and Meta-Analysis. AIDS Educ. Prev. 2009, 21, 181–206. [Google Scholar] [CrossRef] [PubMed]
- Shiner, M. Defining peer education. J. Adolesc. 1999, 22, 555–566. [Google Scholar] [CrossRef]
- Simoni, J.M.; Nelson, K.M.; Franks, J.C.; Yard, S.S.; Lehavot, K. Are Peer Interventions for HIV Efficacious? A Systematic Review. AIDS Behav. 2011, 15, 1589–1595. [Google Scholar] [CrossRef]
- Simoni, J.M.; Franks, J.C.; Lehavot, K.; Yard, S.S. Peer interventions to promote health: Conceptual considerations. Am. J. Orthopsychiatry 2011, 81, 351–359. [Google Scholar] [CrossRef]
- Genberg, B.L.; Shangani, S.; Sabatino, K.; Rachlis, B.; Wachira, J.; Braitstein, P.; Operario, D. Improving Engagement in the HIV Care Cascade: A Systematic Review of Interventions Involving People Living with HIV/AIDS as Peers. AIDS Behav. 2016, 20, 2452–2463. [Google Scholar] [CrossRef]
- Berg, R.C.; Page, S.; Øgård-Repål, A. The effectiveness of peer-support for people living with HIV: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0252623. [Google Scholar] [CrossRef]
- Han, H.-R.; Kim, K.; Murphy, J.; Cudjoe, J.; Wilson, P.; Sharps, P.; Farley, J.E. Community health worker interventions to promote psychosocial outcomes among people living with HIV—A systematic review. PLoS ONE 2018, 13, e0194928. [Google Scholar] [CrossRef]
- Yocom, C. Medicaid Coverage of Peer Support Services for Adults; United States Government Accountability Office: Washington, DC, USA, 2020; pp. 1–19. Available online: https://www.gao.gov/assets/gao-20-616.pdf (accessed on 14 November 2022).
- New York State Department of Health. NYSDOH 2015 Blueprint on Ending the AIDS Epidemic. Available online: https://www.health.ny.gov/diseases/aids/ending_the_epidemic/docs/blueprint.pdf (accessed on 14 November 2022).
- New York State Department of Health AIDS Institute. Peer Worker Course Catalogue. Available online: https://www.hivtrainingny.org/FAQDocs/PeerCertificationCourseCatalogue.pdf (accessed on 14 November 2022).
- Lambert, S.M.; Debattista, J.; Bodiroza, A.; Martin, J.; Staunton, S.; Walker, R. Effective peer education in HIV: Defining factors that maximise success. Sex. Health 2013, 10, 325–331. [Google Scholar] [CrossRef]
- Maulsby, C.H.; Ratnayake, A.; Hesson, D.; Mugavero, M.J.; Latkin, C.A. A Scoping Review of Employment and HIV. AIDS Behav. 2020, 24, 2942–2955. [Google Scholar] [CrossRef] [PubMed]
- Blalock, A.C.; Mcdaniel, J.S.; Farber, E.W. Effect of Employment on Quality of Life and Psychological Functioning in Patients With HIV/AIDS. Psychosomatics 2002, 43, 400–404. [Google Scholar] [CrossRef] [PubMed]
- Rueda, S.; Raboud, J.; Mustard, C.; Bayoumi, A.; Lavis, J.; Rourke, S.B. Employment status is associated with both physical and mental health quality of life in people living with HIV. AIDS Care 2011, 23, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Worthington, C.; Krentz, H.B. Socio-economic factors and health-related quality of life in adults living with HIV. Int. J. STD AIDS 2005, 16, 608–614. [Google Scholar] [CrossRef] [PubMed]
- Cherrick, R.; Skarupski, K. Concerns regarding workforce participation for people living with HIV/AIDS. J. Forensics Vocat. Anal. 2000, 3, 23–30. [Google Scholar]
- Woods, S.P.; HIV Neurobehavioral Research Programs Group; Weber, E.; Weisz, B.M.; Twamley, E.W.; Grant, I. Prospective memory deficits are associated with unemployment in persons living with HIV infection. Rehabil. Psychol. 2011, 56, 77–84. [Google Scholar] [CrossRef]
- Conover, C.J.; Arno, P.; Weaver, M.; Ang, A.; Ettner, S.L. Income and employment of people living with combined HIV/AIDS, chronic mental illness, and substance abuse disorders. SSRN Electron. J. 2006, 9, 71–86. [Google Scholar]
- Razzano, L.A.; Hamilton, M.M. Health-related barriers to employment among people with HIV/AIDS. J. Vocat. Rehabil. 2005, 22, 179–188. [Google Scholar]
- Torres-Madriz, G.; Lerner, D.; Ruthazer, R.; Rogers, W.H.; Wilson, I.B. Work-related Barriers and Facilitators to Antiretroviral Therapy Adherence in Persons Living with HIV Infection. AIDS Behav. 2010, 15, 1475–1482. [Google Scholar] [CrossRef]
- Chiu, Y.-C.J.; Boomer, K.; Conyers, L.; Wang, Y.; Misrok, M. Examining the Relationships Between Social Determinants of Health and Health-Related Quality of Life Among Individuals Living With HIV. Rehabil. Res. Policy Educ. 2021, 35, 168–184. [Google Scholar] [CrossRef]
- Rueda, S.; Raboud, J.; Rourke, S.B.; Bekele, T.; Bayoumi, A.; Lavis, J.; Cairney, J.; Mustard, C. Influence of employment and job security on physical and mental health in adults living with HIV: Cross-sectional analysis. Open Med. Chem. J. 2012, 6, e118–e126. [Google Scholar]
- Rueda, S.; Smith, P.; Bekele, T.; O’Brien, K.; Husbands, W.; Liza, C.; Jose-Boerbridge, M.; Mittmann, N.; Rachlis, A.; Conyers, L.; et al. Is any job better than no job? Labor market experiences and depressive symptoms in people living with HIV. AIDS Care 2015, 27, 907–915. [Google Scholar] [CrossRef] [PubMed]
- Oliva, J. Labour participation of people living with HIV/AIDS in Spain. Health Econ. 2009, 19, 491–500. [Google Scholar] [CrossRef] [PubMed]
- Brooks, R.A.; Martin, D.J.; Ortiz, D.J.; Veniegas, R.C. Perceived barriers to employment among persons living with HIV/AIDS. AIDS Care 2004, 16, 756–766. [Google Scholar] [CrossRef] [PubMed]
- Maguire, C.P.; McNally, C.J.; Britton, P.J.; Werth, J.L.; Borges, N.J. Challenges of Work. Couns. Psychol. 2008, 36, 42–89. [Google Scholar] [CrossRef]
- Hergenrather, K.C.; Rhodes, S.D.; Clark, G. The Employment Perspectives Study: Identifying Factors Influencing the Job–Seeking Behavior of Persons Living with HIV/AIDS. AIDS Educ. Prev. 2005, 17, 131–142. [Google Scholar] [CrossRef]
- Goldblum, P.; Kohlenberg, B. Vocational counseling for people with HIV: The client-focused considering work model. J. Vocat. Rehabil. 2005, 22, 115–124. [Google Scholar]
- Conyers, L.M. A client-focused considering work model for people with emerging or episodic illnesses. J. Vocat. Rehabil. 2018, 48, 331–343. [Google Scholar] [CrossRef]
- DiClemente, C.C.; Prochaska, J.O. Toward a Comprehensive, Transtheoretical Model of Change: Stages of change and addictive behaviors. In Treating Addictive Behaviors, 2nd ed.; Applied Clinical Psychology; Miller, W., Heather, N., Eds.; Plenum Press: New York, NY, USA, 1998; pp. 3–24. [Google Scholar]
- Conyers, L.; Boomer, K.B. Examining the role of vocational rehabilitation on access to care and public health outcomes for people living with HIV/AIDS. Disabil. Rehabil. 2013, 36, 1203–1210. [Google Scholar] [CrossRef]
- Datti, P.A.; Conyers, L.M. Application of the behavioral model of service utilization to predicting factors associated with vocational rehabilitation use among a sample of Latino men with HIV/AIDS in New York State. J. Vocat. Rehabil. 2010, 33, 15–25. [Google Scholar] [CrossRef]
- Jung, Y.; Bellini, J. Rates of Access to the State/Federal Vocational Rehabilitation Program, Service Provision, Successful Closure, and Reasons for Closure for Persons Living with HIV/AIDS; Center on Human Policy, Law, and Disability Studies: Syracuse, NY, USA, 2009. Available online: https://eric.ed.gov/?id=ED507321 (accessed on 14 November 2022).
- Conyers, L.; Datti, P. The unmet vocational rehabilitation needs of women with HIV/AIDS. Work 2008, 31, 277–290. Available online: https://content.iospress.com/articles/work/wor00782 (accessed on 20 September 2022). [PubMed]
- Conyers, L.M. The impact of vocational services and employment on people with HIV/AIDS. Work 2004, 23, 205–214. [Google Scholar] [PubMed]
- Gómez, W.; Flentje, A.; Schustack, A.; Ramirez-Forcier, J.; Andrews, B.; Dilworth, S.E.; Riley, E.D.; Curotto, A.; Carrico, A.W. Navigating Barriers to Vocational Rehabilitation for HIV-Positive Persons. AIDS Behav. 2015, 20, 1132–1142. [Google Scholar] [CrossRef]
- Martin, D.J.; Arns, P.; Batterham, P.; Afifi, A.; Steckart, J. Workforce reentry for people with HIV/AIDS: Intervention effects and predictors of success. Work 2006, 27, 221–233. [Google Scholar] [PubMed]
- Martin, D.J.; Chernoff, R.A.; Buitron, M.; Comulada, W.S.; Liang, L.-J.; Wong, F.L. Helping people with HIV/AIDS return to work: A randomized clinical trial. Rehabil. Psychol. 2012, 57, 280–289. [Google Scholar] [CrossRef]
- Kohlenberg, B.; Watts, M.W. Considering work for people living with HIV/AIDS: Evaluation of a group employment counseling program. J. Rehabil. 2003, 69, 22–29. [Google Scholar]
- Hergenrather, K.C.; Geishecker, S.; Clark, G.; Rhodes, S.D. A Pilot Test of the HOPE Intervention to Explore Employment and Mental Health Among African American Gay Men Living With HIV/AIDS: Results From a CBPR Study. AIDS Educ. Prev. 2013, 25, 405–422. [Google Scholar] [CrossRef]
- Kielhofner, G.; Braveman, B.; Fogg, L.; Levin, M. A Controlled Study of Services to Enhance Productive Participation Among People With HIV/AIDS. Am. J. Occup. Ther. 2008, 62, 36–45. [Google Scholar] [CrossRef]
- Bedell, G. Balancing health, work, and daily life: Design and evaluation of a pilot intervention for persons with HIV/AIDS. Work 2008, 31, 131–144. [Google Scholar]
- Kielhofner, G.; Braveman, B.; Finlayson, M.; Paul-Ward, A.; Goldbaum, L.; Goldstein, K. Outcomes of a Vocational Program for Persons With AIDS. Am. J. Occup. Ther. 2004, 58, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Escovitz, K.; Donegan, K. Providing effective employment supports for persons living with HIV: The KEEP project. J. Vocat. Rehabil. 2005, 22, 105–114. [Google Scholar]
- Breuer, N.L. Teaching the HIV-positive client how to manage the workplace. J. Vocat. Rehabil. 2005, 22, 163–169. [Google Scholar]
- Conyers, L.M.; Richardson, L.A.; Datti, P.A.; Koch, L.C.; Misrok, M. A Critical Review of Health, Social, and Prevention Outcomes Associated With Employment for People Living With HIV. AIDS Educ. Prev. 2017, 29, 475–490. [Google Scholar] [CrossRef] [PubMed]
- Braveman, B. Development of a community-based return to work program for people with AIDS. Occup. Ther. Health Care 2001, 13, 113–131. [Google Scholar] [CrossRef]
- Martin, D.J.; Chernoff, R.A.; Buitron, M. Tailoring a vocational rehabilitation program to the needs of people with HIV/AIDS: The Harbor-UCLA experience. J. Vocat. Rehabil. 2005, 22, 95–103. [Google Scholar]
- Egan, B.E.; Hoagland, J. In-house work opportunities: Implications for housing organizations serving persons living With HIV/AIDS. Work 2006, 27, 247–253. [Google Scholar]
- Fairchild, A.J.; MacKinnon, D.P. A General Model for Testing Mediation and Moderation Effects. Prev. Sci. 2008, 10, 87–99. [Google Scholar] [CrossRef]
- Selig, J.; Preacher, K.J. Mediation Models for Longitudinal Data in Developmental Research. Res. Hum. Dev. 2009, 6, 144–164. [Google Scholar] [CrossRef]
- Wu, A.D.; Zumbo, B.D. Understanding and Using Mediators and Moderators. Soc. Indic. Res. 2007, 87, 367–392. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2011, 16, 606–613. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Carbin, M.G. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 1988, 8, 77–100. [Google Scholar] [CrossRef]
- Turan, B.; Budhwani, H.; Fazeli, P.L.; Browning, W.R.; Raper, J.L.; Mugavero, M.J.; Turan, J.M. How Does Stigma Affect People Living with HIV? The Mediating Roles of Internalized and Anticipated HIV Stigma in the Effects of Perceived Community Stigma on Health and Psychosocial Outcomes. AIDS Behav. 2016, 21, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Phillips, K.D.; Moneyham, L.; Tavakoli, A. Development of an Instrument to Measure Internalized Stigma in Those with HIV/AIDS. Issues Ment. Health Nurs. 2011, 32, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, M. Society and the Adolescent Self-Image; Princeton University Press: London, UK, 1965. [Google Scholar]
- Reynolds, N.R.; Sun, J.; Nagaraja, H.N.; Gifford, A.L.; Wu, A.W.; A Chesney, M. Optimizing Measurement of Self-Reported Adherence With the ACTG Adherence Questionnaire: A Cross-Protocol Analysis. Am. J. Ther. 2007, 46, 402–409. [Google Scholar] [CrossRef]
- Babin, E.A. An examination of predictors of nonverbal and verbal communication of pleasure during sex and sexual satisfaction. J. Soc. Pers. Relatsh. 2012, 30, 270–292. [Google Scholar] [CrossRef]
- Brashers, D.E.; Haas, S.M.; Neidig, J.L. The Patient Self-Advocacy Scale: Measuring Patient Involvement in Health Care Decision-Making Interactions. Health Commun. 1999, 11, 97–121. [Google Scholar] [CrossRef]
- O’Brien, K.K.; Bayoumi, A.M.; Strike, C.; Young, N.L.; Davis, A.M. Exploring disability from the perspective of adults living with HIV/AIDS: Development of a conceptual framework. Health Qual. Life Outcomes 2008, 6, 76. [Google Scholar] [CrossRef]
- Braveman, B.; Levin, M.; Kielhofner, G.; Finlayson, M. HIV/AIDS and return to work: A literature review one-decade post-introduction of combination therapy (HAART). Work 2006, 27, 295–303. [Google Scholar]
- Burns, S.M.; Young, L.R.L.; Maniss, S. Predictors of employment and disability among people living with HIV/AIDS. Rehabil. Psychol. 2006, 51, 127–134. [Google Scholar] [CrossRef]
- Titov, N.; Dear, B.F.; McMillan, D.; Anderson, T.; Zou, J.; Sunderland, M. Psychometric Comparison of the PHQ-9 and BDI-II for Measuring Response during Treatment of Depression. Cogn. Behav. Ther. 2011, 40, 126–136. [Google Scholar] [CrossRef]
- Ware, D.; Rueda, S.; Plankey, M.; Surkan, P.; Okafor, C.N.; Teplin, L.; Friedman, M.R. The longitudinal impact of employment, retirement and disability status on depressive symptoms among men living with HIV in the Multicenter AIDS Cohort Study. PLoS ONE 2020, 15, e0239291. [Google Scholar] [CrossRef] [PubMed]
- Remien, R.H.; Patel, V.; Chibanda, D.; Abas, M.A. Integrating mental health into HIV prevention and care: A call to action. J. Int. AIDS Soc. 2021, 24, e25748. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Canada, K.; Shi, K.; Corrigan, P. HIV-related stigma acting as predictors of unemployment of people living with HIV/AIDS. AIDS Care 2011, 24, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Lightner, J.S.; Rajabiun, S.; Cabral, H.J.; Flaherty, J.; Shank, J.; Brooks, R. Associations of internalized and anticipated HIV stigma with returning to work for persons living with HIV. PLoS ONE 2021, 16, e0252783. [Google Scholar] [CrossRef]
- Barrington, C.; Acevedo, R.; Donastorg, Y.; Perez, M.; Kerrigan, D. ‘HIV and work don’t go together’: Employment as a social determinant of HIV outcomes among men who have sex with men and transgender women in the Dominican Republic. Glob. Public Health 2016, 12, 1506–1521. [Google Scholar] [CrossRef]
- Rosenberg, M.; Schooler, C.; Schoenbach, C.; Rosenberg, F. Global Self-Esteem and Specific Self-Esteem: Different Concepts, Different Outcomes. Am. Sociol. Rev. 1995, 60, 141. [Google Scholar] [CrossRef]
- Silván-Ferrero, P.; Holgado, P.F.; Jiménez, J.; Pérez-Garín, D. Benefits of employment in people with mental illness: Differential mediating effects of internalized stigma on self-esteem. J. Community Appl. Soc. Psychol. 2021, 32, 119–134. [Google Scholar] [CrossRef]
- Nachega, J.B.; A Uthman, O.; Peltzer, K.; A Richardson, L.; Mills, E.J.; Amekudzi, K.; Ouédraogo, A. Association between antiretroviral therapy adherence and employment status: Systematic review and meta-analysis. Bull. World Health Organ. 2014, 93, 29–41. [Google Scholar] [CrossRef]
- Semvua, S.K.; Orrell, C.; Mmbaga, B.T.; Semvua, H.H.; Bartlett, J.A.; Boulle, A.A. Predictors of non-adherence to antiretroviral therapy among HIV infected patients in northern Tanzania. PLoS ONE 2017, 12, e0189460. [Google Scholar] [CrossRef]
- Daniels, J.; Struthers, H.; Soler, J.; Ricco, E.; Blackmon, J.; Teklehaimanot, S.; McIntyre, J.; Coates, T. Building self-advocacy in HIV care: The use of role-play to examine healthcare access for HIV-positive MSM in rural South Africa. Glob. Health Promot. 2020, 28, 32–40. [Google Scholar] [CrossRef]
- Mutchler, M.G.; Wagner, G.; Cowgill, B.O.; McKay, T.; Risley, B.; Bogart, L.M. Improving HIV/AIDS care through treatment advocacy: Going beyond client education to empowerment by facilitating client–provider relationships. AIDS Care 2011, 23, 79–90. [Google Scholar] [CrossRef] [PubMed]
- Bond, K.T.; Frye, V.; Cupid, M.; Lucy, D.; Koblin, B.A. HIV-Related Communication and Safe Sex Practices among Heterosexual Black Men: A Qualitative Report. J. Black Sex. Relatsh. 2018, 4, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Dawson-Rose, C.; Gutin, S.A.; Mudender, F.; Hunguana, E.; Kevany, S. Effects of a peer educator program for HIV status disclosure and health system strengthening: Findings from a clinic-based disclosure support program in Mozambique. PLoS ONE 2020, 15, e0232347. [Google Scholar] [CrossRef] [PubMed]
- Buot, M.-L.G.; Docena, J.P.; Ratemo, B.K.; Bittner, M.J.; Burlew, J.T.; Nuritdinov, A.R.; Robbins, J.R. Beyond Race and Place: Distal Sociological Determinants of HIV Disparities. PLoS ONE 2014, 9, e91711. [Google Scholar] [CrossRef]
- Oldenburg, C.E.; Perez-Brumer, A.G.; Reisner, S.L. Poverty matters: Contextualizing the syndemic condition of psychological factors and newly diagnosed HIV infection in the United States. Aids 2014, 28, 2763–2769. [Google Scholar] [CrossRef]
- Arns, P.G.; Martin, D.J.; Chernoff, R.A. Psychosocial needs of HIV-positive individuals seeking workforce re-entry. AIDS Care 2004, 16, 377–386. [Google Scholar] [CrossRef]
- Topping, K.J. Peer Education and Peer Counselling for Health and Well-Being: A Review of Reviews. Int. J. Environ. Res. Public Health 2022, 19, 6064. [Google Scholar] [CrossRef]
- Hergenrather, K.C.; Zeglin, R.J.; Conyers, L.; Misrok, M.; Rhodes, S.D. Persons Living With HIV/AIDS: Employment as a Social Determinant of Health. Rehabil. Res. Policy Educ. 2016, 30, 4–31. [Google Scholar] [CrossRef]
- New York State Office of Temporary Disability Assistance. 1994 INF-41 HIV Peer Educator Stipends. Available online: https://otda.ny.gov/policy/directives/1994/INF/94_INF-41.pdf (accessed on 14 November 2022).
| Number of Participants Who Completed Surveys during Program Milestones | ||||||
|---|---|---|---|---|---|---|
| Baseline Only Participants | Training Completion Participants | Training and Internship Participants | ||||
| (N = 67) | (N = 137) | (N = 55) | ||||
| Survey Timeframe | n | Survey Timeframe | n | Survey Timeframe | n | |
| Cohort One | September 2014 | 13 | November 2014 | 9 | June 2015 | 9 |
| Cohort Two | March 2015 | 6 | May 2015 | 8 | December 2015 | 9 |
| Cohort Three | September 2015 | 8 | November 2015 | 12 | June 2016 | 11 |
| Cohort Four | March 2016 | 6 | May 2016 | 20 | December 2016 | 5 |
| Cohort Five | September 2016 | 7 | November 2016 | 16 | June 2017 | 4 |
| Cohort Six | March 2017 | 7 | May 2017 | 18 | December 2017 | 4 |
| Cohort Seven | September 2017 | 6 | November 2017 | 21 | June 2018 | 4 |
| Cohort Eight | March 2018 | 7 | May 2018 | 15 | December 2018 | 9 |
| Cohort Nine | September 2018 | 7 | November 2018 | 18 | - | - |
| Total | 67 | 137 | 55 | |||
| Measures | Cronbach’s α Time 1 | Cronbach’s α Time 2 | Cronbach’s α Time 3 |
|---|---|---|---|
| Patient Health Questionnaire (PHQ-9) | 0.86 | 0.89 | 0.85 |
| Beck’s Depression Inventory (BDI) | 0.93 | 0.96 | NA |
| The Internalized Stigma of HIV/AIDS Tool (ISAT) | 0.88 | 0.88 | 0.89 |
| Rosenberg’s Self-Esteem Scale | 0.83 | 0.81 | 0.84 |
| General Sexual Communication Apprehension scale | 0.73 | 0.68 | 0.67 |
| The Patient Self-advocacy Scale | 0.76 | 0.70 | 0.68 |
| Baseline Participants | |||||
|---|---|---|---|---|---|
| (N = 259) | |||||
| Category | n | % | Category | n | % |
| Baseline Demographics | |||||
| Gender | Age | ||||
| Male | 146 | 56.37 | 18–34 | 54 | 21.26 |
| Female | 97 | 37.45 | 35–44 | 65 | 25.59 |
| Transgender | 16 | 6.18 | 45–54 | 83 | 32.68 |
| Education Level | 55–64 | 52 | 20.47 | ||
| <High School | 43 | 16.86 | Race/Ethnicity | ||
| HS Graduate or GED | 170 | 66.67 | Black | 157 | 61.57 |
| College | 42 | 16.47 | Hispanic | 55 | 21.57 |
| Sexual Identity | White | 14 | 5.49 | ||
| Straight | 129 | 51.8 | Mixed | 29 | 11.37 |
| LGBTQ | 120 | 48.19 | |||
| Baseline health characteristics | |||||
| AIDS Diagnosis | Viral Load | ||||
| Yes | 90 | 35.43 | Undetectable | 207 | 83.81 |
| No | 164 | 64.57 | Detectable | 40 | 16.19 |
| Years Living with HIV | Self-Rated General Health in the Past Year | ||||
| 0–5 Years | 49 | 19.68 | Excellent | 46 | 20.44 |
| 6–10 Years | 32 | 12.85 | Very Good | 90 | 40 |
| 11–15 Years | 42 | 16.87 | Good | 67 | 29.78 |
| 16–25 Years | 82 | 32.93 | Fair or Poor | 22 | 9.78 |
| > 25 Years | 44 | 17.67 | Alcohol and/or Drug Addiction History | ||
| Number of Chronic Conditions Other than HIV | Yes | 141 | 54.86 | ||
| None | 81 | 31.52 | No | 116 | 45.14 |
| One | 79 | 30.74 | Mental Health Diagnosis | ||
| More than Two | 97 | 37.74 | Yes | 119 | 46.12 |
| No | 139 | 45.14 | |||
| Baseline work history and benefits received | |||||
| Years since last part-time or full-time employment | Public Benefits Received | ||||
| Past 2 Years | 99 | 41.08 | Medical * | 220 | 85.27 |
| Past 5 Years | 45 | 18.67 | Housing ** | 184 | 71.32 |
| Past 5–10 Years | 43 | 17.84 | Cash *** | 204 | 78.76 |
| Over 10 Years | 35 | 14.52 | SSI or SSD | 30 | 14.02 |
| Never | 19 | 7.88 | |||
| Participants by Program Completion Type | ||||||||
|---|---|---|---|---|---|---|---|---|
| Baseline Only Participants | Training Completion Participants | Training and Internship Participants | ANOVA | |||||
| Mean (SD) | Valid n | Mean (SD) | Valid n | Mean (SD) | Valid n | f-Value | p-Value | |
| Safer Sex Com. Apprehension | 12.59 (6.55) | 60 | 11.83 (5.74) | 131 | 12.06 (5.57) | 54 | 0.34 | 0.71 |
| Patient Self-Advocacy | 41.25 (8.25) | 57 | 43.3 (5.84) | 118 | 42.07 (6.79) | 50 | 1.93 | 0.15 |
| HIV Medication Adh. | 92.34 (11.98) | 54 | 88.2 (18.6) | 110 | 92.34 (11.98) | 48 | 1.37 | 0.26 |
| Beck’s Depression Inv. | 14.74 (12.20) | 17 | 12.95 (11.64) | 17 | 11.75 (9.06) | 18 | 0.32 | 0.72 |
| PHQ-9 Depression Inv. | 5.28 (5.72) | 46 | 4.68 (4.72) | 118 | 5.38 (4.85) | 37 | 0.43 | 0.65 |
| HIV Intern. Stigma | 24.59 (9.92) | 65 | 24.02 (8.49) | 134 | 26.93 (9.10) | 55 | 2.05 | 0.13 |
| Self-Esteem | 21.92 (5.35) | 65 | 21.49 (5.0) | 136 | 20.81 (4.62) | 55 | 0.73 | 0.48 |
| Survey Period | ||||
|---|---|---|---|---|
| Time 1 | Time 2 | Paired t-Test | ||
| Psychosocial Inventory (Valid N) | Mean (SD) | Mean (SD) | t-value | p-value |
| Safer Sex Communication Apprehension (176) | 11.95 (5.72) | 11.18 (5.54) | −1.66 | 0.1 |
| Patient Self-Advocacy (153) | 42.84 (8.25) | 43.94 (6.79) | 2.08 | 0.04 |
| HIV Medication Adherence (149) | 88.01 (11.98) | 90.88 (11.98) | 2.2 | 0.03 |
| Beck’s Depression Inventory (35) | 11.75 (10.25) | 10.80 (11.58) | −0.9 | 0.38 |
| PHQ-9 Depression Inventory (150) | 4.82 (4.70) | 3.04 (4.19) | −4.49 | <0.001 |
| HIV Internalized Stigma (185) | 25.06 (8.74) | 23.02 (8.79) | −3.79 | <0.001 |
| Self-Esteem (186) | 21.33 (4.87) | 22.49 (4.88) | 4.03 | <0.001 |
| Participants by Program Completion Type | ||||||||
|---|---|---|---|---|---|---|---|---|
| Training Completion Only Participants | Training and Internship Participants | |||||||
| Time 1 | Time 2 | Paired t-Test | Time 1 | Time 2 | Paired t-Test | |||
| Inventory | Valid n | Mean (SD) | Mean (SD) | p-value | Valid n | Mean (SD) | Mean (SD) | p-value |
| Safer Sex Com. Apprehen. | 123 | 11.95 (5.8) | 11.84 (5.69) | 0.83 | 52 | 12.2 (5.53) | 9.66 (5.74) | 0.001 |
| Patient Self-Advoc. | 108 | 43.07 (6.0) | 43.47 (6.74) | 0.5 | 48 | 41.95 (6.8) | 44.65 (5.19) | 2 |
| HIV Med. Adh. | 103 | 88.44 (15.8) | 89.51 (13.92) | 0.77 | 53 | 88.81 (17.0) | 93.94 (13.98) | 0.02 |
| Beck’s Depression | 17 | 12.94 (12.99) | 12.73 (11.64) | 0.94 | 18 | 11.75 (9.06) | 8.86 (10.00) | 0.26 |
| PHQ-9 Depression | 86 | 4.86 (5.10) | 3.00 (3.82) | 0.001 | 35 | 5.21 (4.9) | 2.77 (3.42) | <0.001 |
| HIV Intern. Stigma | 131 | 24.23 (8.46) | 22.45 (8.82) | 0.001 | 53 | 27.15 (9.05) | 24.67 (8.48) | 0.003 |
| Self-Esteem | 132 | 21.36 (4.98) | 22.70 (4.93) | 0.001 | 53 | 20.7 (4.58) | 21.85 (4.69) | 0.07 |
| Survey Period | Paired t-Test | |||||
|---|---|---|---|---|---|---|
| Baseline | Training Completion | Internship | Time 1–2 | Time 2–3 | Time 1–3 | |
| Psychosocial Inventory (Valid N) | Mean (SD) | Mean (SD) | Mean (SD) | p-value | p-value | p-value |
| Safer Sex Communication Apprehension (N = 52) | 12.2 (5.53) | 9.66 (5.74) | 10.22 (5.03) | 0.001 | 0.21 | 0.02 |
| Patient Self-Advocacy (N = 48) | 41.95 (6.8) | 44.65 (5.19) | 45.17 (4.82) | 0.02 | 0.58 | <0.001 |
| HIV Medication Adherence (N = 53) | 88.81 (17.0) | 93.94 (13.98) | 92.83 (12.87) | 0.02 | 0.33 | 0.37 |
| Beck’s Depression Inventory (N = 18) | 11.75 (9.06) | 8.86 (10.00) | 0.26 | |||
| PHQ-9 Depression Inventory (N = 35) | 5.21 (4.9) | 2.77 (3.42) | 2.63 (3.03) | <0.001 | 0.78 | 0.003 |
| HIV Internalized Stigma (N = 53) | 27.15 (9.05) | 24.67 (8.48) | 23.06 (8.02) | 0.003 | 0.18 | <0.001 |
| Self-Esteem (N = 53) | 20.7 (4.58) | 21.85 (4.69) | 22.74 (4.64) | 0.07 | 0.23 | 0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McKinney-Prupis, E.; Chiu, Y.-C.J.; Grov, C.; Tsui, E.K.; Duke, S.I. Psychosocial and Health-Related Behavioral Outcomes of a Work Readiness HIV Peer Worker Training Program. Int. J. Environ. Res. Public Health 2023, 20, 4322. https://doi.org/10.3390/ijerph20054322
McKinney-Prupis E, Chiu Y-CJ, Grov C, Tsui EK, Duke SI. Psychosocial and Health-Related Behavioral Outcomes of a Work Readiness HIV Peer Worker Training Program. International Journal of Environmental Research and Public Health. 2023; 20(5):4322. https://doi.org/10.3390/ijerph20054322
Chicago/Turabian StyleMcKinney-Prupis, Erin, Yung-Chen Jen Chiu, Christian Grov, Emma K. Tsui, and Sharen I. Duke. 2023. "Psychosocial and Health-Related Behavioral Outcomes of a Work Readiness HIV Peer Worker Training Program" International Journal of Environmental Research and Public Health 20, no. 5: 4322. https://doi.org/10.3390/ijerph20054322
APA StyleMcKinney-Prupis, E., Chiu, Y.-C. J., Grov, C., Tsui, E. K., & Duke, S. I. (2023). Psychosocial and Health-Related Behavioral Outcomes of a Work Readiness HIV Peer Worker Training Program. International Journal of Environmental Research and Public Health, 20(5), 4322. https://doi.org/10.3390/ijerph20054322






