Protective Role of Social Networks for the Well-Being of Persons with Disabilities: Results from a State-Wide Cross-Sectional Survey in Kerala, India
Abstract
1. Introduction
1.1. People with Disabilities in Kerala, India
1.2. Social Networks of People with Disabilities
2. Materials and Methods
2.1. Design
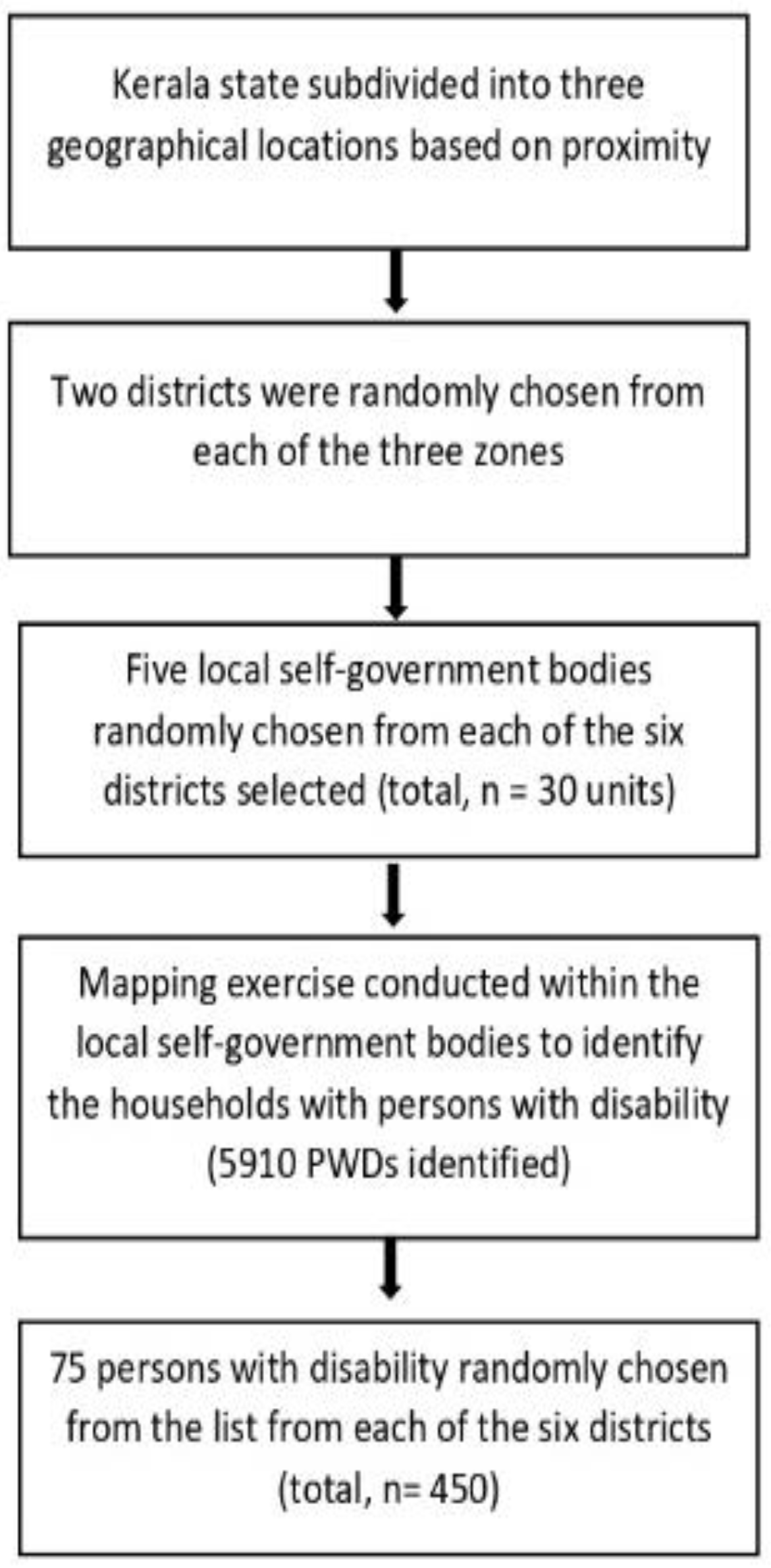
2.2. Participant Recruitment
2.3. Measurements
2.3.1. Outcome Variable
2.3.2. Exposure Variables
2.4. Data Analysis
2.5. Ethical Considerations
3. Results
3.1. Demographic Characteristics
3.2. Service Accessibility
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. World Report on Disability 2011. Available online: https://apps.who.int/iris/handle/10665/44575 (accessed on 12 August 2022).
- Kerala Social Security Mission. Kerala Disability Census Report 2015. Available online: https://drive.google.com/file/d/1Iy-59Xe9xiX0QGZM2uVFxnVbnwnlF0Cm/view?pli=1 (accessed on 18 February 2023).
- Persons with Disabilities (Divyangjan) in India—A Statistical Profile: 2021. Available online: http://www.nhfdc.nic.in/upload/nhfdc/Persons_Disabilities_31mar21.pdf (accessed on 18 February 2023).
- Das Prasad, S.A.; Nundy, S. Rationing medical resources fairly during the COVID-19 crisis: Is this possible in India (or America)? Curr. Med. Res. Pract. 2020, 10, 127–129. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.G.; Roy, G.; Kar, S.S. Disability and rehabilitation services in India: Issues and challenges. J. Fam. Med. Prim. Care 2012, 1, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Senjam, S.S.; Singh, A. Addressing the health needs of people with disabilities in India. Indian J. Public Health 2020, 64, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Shandra, C.L. Disability and social participation: The case of formal and informal volunteering. Soc. Sci. Res. 2017, 68, 195–213. [Google Scholar] [CrossRef]
- Henderson, C.; Noblett, J.; Parke, H.; Clement, S.; Caffrey, A.; Gale-Grant, O.; Schulze, B.; Druss, B.; Thornicroft, G. Mental health-related stigma in health care and mental health-care settings. Lancet Psychiatry 2014, 1, 467–482. [Google Scholar] [CrossRef] [PubMed]
- Vásquez, E.; Murillo, R.; Echeverria, S. Neighborhood Social Cohesion and Walking Limitations in Ethnically Diverse Older Latinos in the United States. Ethn. Dis. 2019, 29, 247–252. [Google Scholar] [CrossRef]
- Trani, J.F.; Moodley, J.; Anand, P.; Graham, L.; Thu Maw, M.T. Stigma of persons with disabilities in South Africa: Uncovering pathways from discrimination to depression and low self-esteem. Soc. Sci. Med. 2020, 265, 113449. [Google Scholar] [CrossRef]
- Liu, S.; Xie, W.; Han, S.; Mou, Z.; Zhang, X.; Zhang, L. Social Interaction Patterns of the Disabled People in Asymmetric Social Dilemmas. Front. Psychol. 2018, 9, 1683. [Google Scholar] [CrossRef]
- Zapfel, S.; Reims, N.; Niehaus, M. Social Networks and Disability: Access to and Stabilization of Integration into the Primary Labor Market. In Social Networks and Health Inequalities: A New Perspective for Research; Klärner, A., Gamper, M., Keim-Klärner, S., Moor, I., von der Lippe, H., Vonneilich, N., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2022; pp. 273–290. [Google Scholar]
- Devassy, S.M.; Scaria, L.; Cheguvera, N.; Thampi, K. Association of Depression and Anxiety with Social Network Types: Results from a Community Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 6120. [Google Scholar] [CrossRef]
- Emerson, E.; Fortune, N.; Llewellyn, G.; Stancliffe, R. Loneliness, social support, social isolation and wellbeing among working age adults with and without disability: Cross-sectional study. Disabil. Health J. 2021, 14, 100965. [Google Scholar] [CrossRef]
- Ipsen, C.; Repke, M. Reaching people with disabilities to learn about their experiences of social connection and loneliness. Disabil. Health J. 2022, 15, 101220. [Google Scholar] [CrossRef] [PubMed]
- Saju, M.D.; Benny, A.M.; Preet Allagh, K.; Joseph, B.; Amuthavalli Thiyagarajan, J. Relationship between neighbourhood cohesion and disability: Findings from SWADES population-based survey, Kerala, India. F1000Research 2020, 9, 700. [Google Scholar] [CrossRef] [PubMed]
- Chakrabarti, S. Research on family caregiving for mental illness in India and its impact on clinical practice: Are we doing enough to help families? Indian J. Soc. Psychiatry 2016, 32, 19–24. [Google Scholar] [CrossRef]
- Song, L.; Chang, T.-Y. Do resources of network members help in help seeking? Social capital and health information search. Soc. Netw. 2012, 34, 658–669. [Google Scholar] [CrossRef]
- Tournier, T.; Hendriks, A.H.C.; Jahoda, A.; Hastings, R.P.; Giesbers, S.A.H.; Vermulst, A.A.; Embregts, P.J.C.M. Family network typologies of adults with intellectual disability: Associations with psychological outcomes. J. Appl. Res. Intellect. Disabil. 2021, 34, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Giesbers, S.A.H.; Hendriks, A.H.C.; Hastings, R.P.; Jahoda, A.; Tournier, T.; Embregts, P.J.C.M. Social Capital and the Reciprocal Nature of Family Relationships: The Perspective of Individuals With Mild Intellectual Disability. Am. J. Intellect. Dev. Disabil. 2020, 125, 170–185. [Google Scholar] [CrossRef] [PubMed]
- Araya, R.; Dunstan, F.; Playle, R.; Thomas, H.; Palmer, S.; Lewis, G. Perceptions of social capital and the built environment and mental health. Soc. Sci. Med. 2006, 62, 3072–3083. [Google Scholar] [CrossRef]
- Gordon-Larsen, P.; Nelson, M.C.; Page, P.; Popkin, B.M. Inequality in the Built Environment Underlies Key Health Disparities in Physical Activity and Obesity. Pediatrics 2006, 117, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Chola, L.; Alaba, O. Association of neighbourhood and individual social capital, neighbourhood economic deprivation and self-rated health in South Africa—A multi-level analysis. PLoS ONE 2013, 8, e71085. [Google Scholar] [CrossRef] [PubMed]
- Song, M.-S. Convergence Models of Evaluation Systems for Social Welfare Facilities. Je Korea Converg. Soc. 2015, 6, 115–122. [Google Scholar] [CrossRef]
- Leu, J.; Yen, I.H.; Gansky, S.A.; Walton, E.; Adler, N.E.; Takeuchi, D.T. The association between subjective social status and mental health among Asian immigrants: Investigating the influence of age at immigration. Soc. Sci. Med. 2008, 66, 1152–1164. [Google Scholar] [CrossRef] [PubMed]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A Systematic Review of the Literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Junnarkar, M.; Sharma, S. Anxiety, stress, depression, and psychosocial functioning of Indian adolescents. Indian J. Psychiatry 2015, 57, 367–374. [Google Scholar] [CrossRef]
- Srivastava, K. Urbanization and mental health. Ind. Psychiatry J. 2009, 18, 75–76. [Google Scholar] [CrossRef] [PubMed]
- Lakshmana, G.; Sangeetha, V.; Pandey, V. Community perception of accessibility and barriers to utilizing mental health services. J. Educ. Health Promot. 2022, 11, 56. [Google Scholar] [CrossRef]
- Lindsay, S. Spaces of well-being among young adults with physical disabilities transitioning from pediatric to adult healthcare. Disabil. Health J. 2018, 11, 149–154. [Google Scholar] [CrossRef]
- Kingsbury, M.; Clayborne, Z.; Colman, I.; Kirkbride, J.B. The protective effect of neighbourhood social cohesion on adolescent mental health following stressful life events. Psychol. Med. 2020, 50, 1292–1299. [Google Scholar] [CrossRef]
- Holt-Lunstad, J.; Smith, T.B.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and Social Isolation as Risk Factors for Mortality: A Meta-Analytic Review. Perspect. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef]
- Attree, P.; French, B.; Milton, B.; Povall, S.; Whitehead, M.; Popay, J. The experience of community engagement for individuals: A rapid review of evidence. Health Soc. Care Community 2011, 19, 250–260. [Google Scholar] [CrossRef]
- Rathod, S.; Pinninti, N.; Irfan, M.; Gorczynski, P.; Rathod, P.; Gega, L.; Naeem, F. Mental Health Service Provision in Low- and Middle-Income Countries. Health Serv. Insights 2017, 10, 1178632917694350. [Google Scholar] [CrossRef] [PubMed]
- Hunt, X.; Bradshaw, M.; Vogel, S.L.; Encalada, A.V.; Eksteen, S.; Schneider, M.; Chunga, K.; Swartz, L. Community Support for Persons with Disabilities in Low- and Middle-Income Countries: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 8269. [Google Scholar] [CrossRef] [PubMed]
- Butel, J.; Braun, K.L. The Role of Collective Efficacy in Reducing Health Disparities: A Systematic Review. Fam. Community Health 2019, 42, 8–19. [Google Scholar] [CrossRef] [PubMed]
- Duggan, A. Understanding Interpersonal Communication Processes Across Health Contexts: Advances in the Last Decade and Challenges for the Next Decade. J. Health Commun. 2006, 11, 93–108. [Google Scholar] [CrossRef] [PubMed]
- Lochner, K.A.; Kawachi, I.; Brennan, R.T.; Buka, S.L. Social capital and neighborhood mortality rates in Chicago. Soc. Sci. Med. 2003, 56, 1797–1805. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.C.; Zhu, Z.Y. Improving Social Inclusion for People with Physical Disabilities: The Roles of Mobile Social Networking Applications (MSNA) by Disability Support Organizations in China. Int. J. Environ. Res. Public Health 2020, 17, 2333. [Google Scholar] [CrossRef] [PubMed]
| Variables | Category | Overall | Northern Zone | Central Zone | Southern Zone |
|---|---|---|---|---|---|
| Age | Children (0–18 years) | 93 (20.7%) | 28 (18.6%) | 29 (19.3%) | 36 (24%) |
| Young adults (19–39 years) | 151 (33.6%) | 55 (36.7%) | 54 (36%) | 42 (28%) | |
| Middle adulthood (40–59 years) | 148 (32.9%) | 49 (32.7%) | 57 (38%) | 42 (28%) | |
| Late adulthood (>60 years) | 58 (12.9%) | 18 (12%) | 10 (6.7%) | 30 (20%) | |
| Gender | Male | 279 (62%) | 91 (60.7%) | 100 (66.7%) | 88 (58.7%) |
| Female | 171 (38%) | 59 (39.3%) | 50 (33.3%) | 62 (41.3%) | |
| Education | Illiterate | 74 (16.4%) | 30 (20%) | 22 (14.7%) | 22 (14.7%) |
| literate but did not complete primary education | 14 (3.1%) | 10 (6.7%) | 1 (0.7%) | 3 (2%) | |
| Completed primary education | 324 (72%) | 100 (66.7%) | 114 (76%) | 110 (73.3%) | |
| Completed secondary education | 33 (7.3%) | 9 (6%) | 11 (7.3%) | 13 (8.7%) | |
| Completed tertiary education | 5 (1.1%) | 1 (0.7%) | 2 (1.3%) | 2 (1.3%) | |
| Marital status | Currently married | 147 (32.7%) | 52 (34.7%) | 45 (30%) | 50 (33.3%) |
| Never married | 284 (63.1%) | 9 1(60.7%) | 100 (66.7%) | 93 (62%) | |
| Widowed | 10 (2.2%) | 4 (2.7%) | 1 (0.7%) | 5 (3.3%) | |
| Separated/Divorced | 9 (2%) | 3 (2%) | 4 (2.7%) | 2 (1.3%) | |
| Employment | Employed | 98 (21.8%) | 32 (21.3%) | 44 (29.3%) | 22 (14.7%) |
| Unemployed | 96 (21.3%) | 20 (13.3%) | 10 (6.7%) | 66 (44%) | |
| Student | 109 (24.2%) | 38 (25.3%) | 41 (27.3%) | 30 (20%) | |
| Dependent | 147 (32.7%) | 60 (40%) | 55 (36.7%) | 32 (21.3%) | |
| Type of ration card | Yellow | 64 (14.2%) | 17 (11.3%) | 20 (13.3%) | 27 (18%) |
| Pink | 260 (57.7%) | 94 (62.7%) | 83 (55.3%) | 19 (12.7%) | |
| Blue | 58 (12.9%) | 16 (10.7%) | 23 (15.3%) | 19 (12.7%) | |
| White | 68 (15.1%) | 23 (15.3%) | 24 (16%) | 21 (14%) | |
| Type of disability | Physical disability | 244 (54.2%) | 69 (46%) | 83 (55.3%) | 92 (61.3%) |
| Intellectual disability | 107 (23.8%) | 37 (24.7%) | 33 (22%) | 37 (24.7%) | |
| Multiple disabilities | 69 (15.3%) | 32 (21.3%) | 23 (15.3%) | 14 (9.3%) | |
| Other disabilities* | 30 (6.7%) | 12 (8%) | 11 (7.3%) | 7 (4.7%) | |
| Level of disability | Below 40% | 33 (7.3%) | 9 (6%) | 6 (4%) | 18 (12%) |
| Between 40–79% | 314 (69.8%) | 94 (62.7%) | 116 (77.3%) | 104 (69.3%) | |
| 80% above | 103 (22.9%) | 47 (31.3%) | 28 (18.7%) | 28 (18.7%) | |
| Well-being | Total mean score | 12.94 (4.9) | 13 (4.9) | 11.7 (4.9) | 14.2 (4.7) |
| Depression | Total mean score | 6.6 (6.3) | 6.9 (6.9) | 8.1 (6.2) | 4.8 (5.2) |
| Anxiety | Total mean score | 9.3 (8.7) | 9.2 (8.6) | 11.2 (8.9) | 7.4 (8.2) |
| Stress | Total mean score | 8.2 (7.7) | 8.2 (7.7) | 10.1 (8.1) | 6.2 (6.8) |
| Social Support | Poor support networks | 216 (48%) | 71 (47.3%) | 85 (56.7%) | 60 (40%) |
| Adequate support networks | 234 (52%) | 79 (52.7%) | 65 (43.3%) | 90 (60%) |
| Service Type | with Access | Gender | Zone | |||
|---|---|---|---|---|---|---|
| Male | Female | North | Central | South | ||
| Income/Employment | 271 (60.2%) | 160 (59%) | 111 (41%) | 85 (31.4%) | 69 (25.5%) | 117 (43.1%) |
| Access to food/other daily services | 421 (93.6%) | 258 (61.3%) | 163 (38.7%) | 142 (33.7%) | 133 (31.6%) | 146 (34.7%) |
| Access to medical health care | 336 (74.7%) | 210 (62.5%) | 126 (37.5%) | 123 (36.6%) | 108 (32.1%) | 105 (31.3%) |
| Access to mental health care treatment. | 386 (85.8%) | 244 (63.2%) | 142 (36.8%) | 139 (36%) | 127 (32.9%) | 120 (31.1%) |
| Accessibility Variables | Overall | Social Support Networks | p-Value | |
|---|---|---|---|---|
| Poor Support Networks | Support Networks Available | |||
| General Services | ||||
| Employment access—adequate | 271 (60.22%) | 105 (38.75%) | 166 (61.25%) | p < 0.001 |
| Employment access—Inadequate | 179 (39.78%) | 111 (62.1%) | 68 (37.9%) | |
| Food/basic services—adequate | 421 (93.56%) | 199 (47.27%) | 222 (52.73%) | p = 0.238 |
| Food/basic services—Inadequate | 29 (6.44%) | 17 (58.6%) | 12 (41.4%) | |
| Medical health care—adequate | 336 (74.67%) | 156 (46.43%) | 180 (53.57%) | p = 0.252 |
| Medical health care—Inadequate | 114 (25.33%) | 60 (52.6%) | 54 (47.4%) | |
| Mental health care—adequate | 386 (85.78%) | 181 (46.89%) | 205 (53.11%) | p = 0.248 |
| Mental health care—Inadequate | 64 (14.22%) | 35 (54.7%) | 29 (45.3%) | |
| Associative Factors | Categories | Crude Regression Coefficient (CI), p-Value |
|---|---|---|
| Social Support Networks | Poor support networks (reference) | |
| Support networks available | 2.30 (1.40–3.19), p < 0.001 | |
| Education | (1-unit increase) | 0.71 (0.18–1.24), p = 0.008 |
| Service Accessibility | (no accessibility issues as reference) | |
| Inability to access one of the services | −1.50 (−2.52 to −0.49), p = 0.004 | |
| Inability to access two of the services | −2.08 (−3.42 to −0.73), p = 0.003 | |
| Inability to access three of the services | −4.50 (−6.43 to −2.58), p < 0.001 | |
| Inability to access all four services | −5.52 (−9.13 to −1.91), p = 0.003 | |
| Presence of depressive symptoms | (1-unit increase) | −0.65 (−0.69 to −0.61), p < 0.001 |
| Presence of anxiety symptoms | (1-unit increase) | −0.49 (−0.52 to −0.47), p < 0.001 |
| Presence of stress symptoms | (1-unit increase) | −0.55 (−0.58 to −0.52), p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Devassy, S.M.; Scaria, L.; Yohannan, S.V.; Pathrose, S.I. Protective Role of Social Networks for the Well-Being of Persons with Disabilities: Results from a State-Wide Cross-Sectional Survey in Kerala, India. Int. J. Environ. Res. Public Health 2023, 20, 4213. https://doi.org/10.3390/ijerph20054213
Devassy SM, Scaria L, Yohannan SV, Pathrose SI. Protective Role of Social Networks for the Well-Being of Persons with Disabilities: Results from a State-Wide Cross-Sectional Survey in Kerala, India. International Journal of Environmental Research and Public Health. 2023; 20(5):4213. https://doi.org/10.3390/ijerph20054213
Chicago/Turabian StyleDevassy, Saju Madavanakadu, Lorane Scaria, Shilpa V. Yohannan, and Sunirose Ishnassery Pathrose. 2023. "Protective Role of Social Networks for the Well-Being of Persons with Disabilities: Results from a State-Wide Cross-Sectional Survey in Kerala, India" International Journal of Environmental Research and Public Health 20, no. 5: 4213. https://doi.org/10.3390/ijerph20054213
APA StyleDevassy, S. M., Scaria, L., Yohannan, S. V., & Pathrose, S. I. (2023). Protective Role of Social Networks for the Well-Being of Persons with Disabilities: Results from a State-Wide Cross-Sectional Survey in Kerala, India. International Journal of Environmental Research and Public Health, 20(5), 4213. https://doi.org/10.3390/ijerph20054213






