Epidemiological Characteristics of Notifiable Respiratory Infectious Diseases in Mainland China from 2010 to 2018
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Classification of RIDs and Studied Regions
2.3. Data Analysis
2.4. Joinpoint Regression Model
2.5. Seasonal Decomposition
2.6. Spatiotemporal Clustering Analysis
3. Results
3.1. Overall Epidemic Situation of RIDs
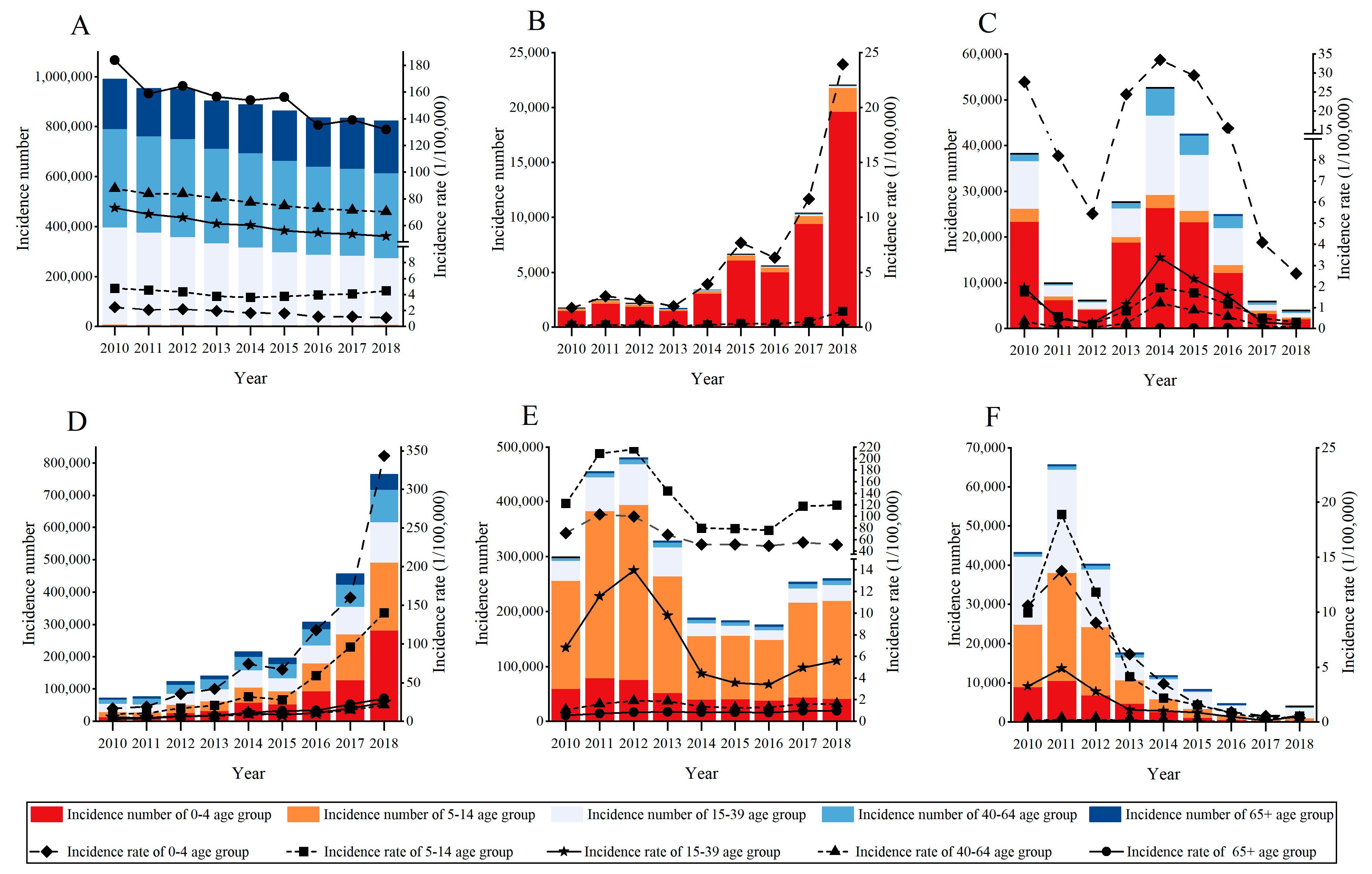
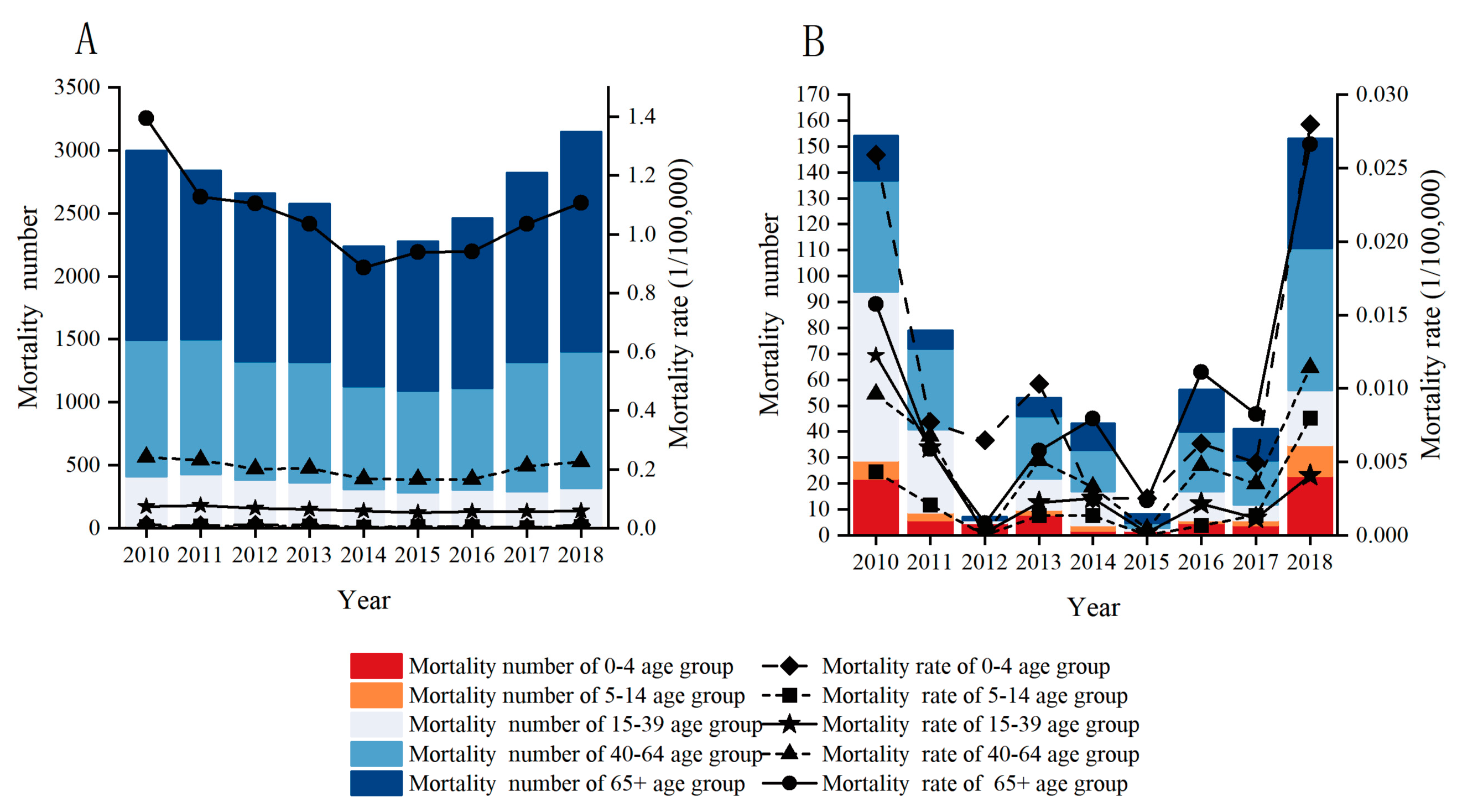
3.2. Age-Specific Incidence Rates and Mortalities for the Six Selected RIDs
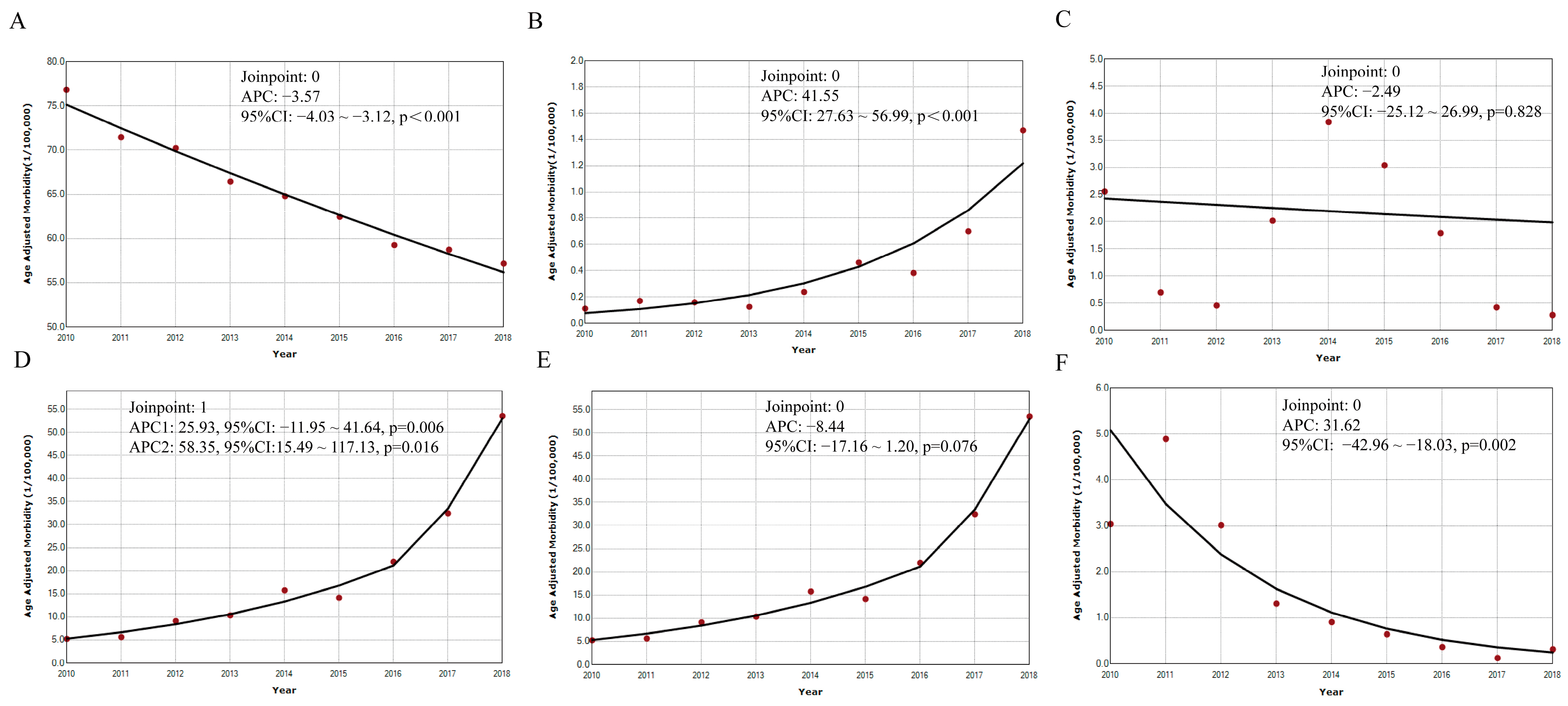
3.3. Temporal Trends of Incidence Rates and Mortalities of the Six Selected RIDs
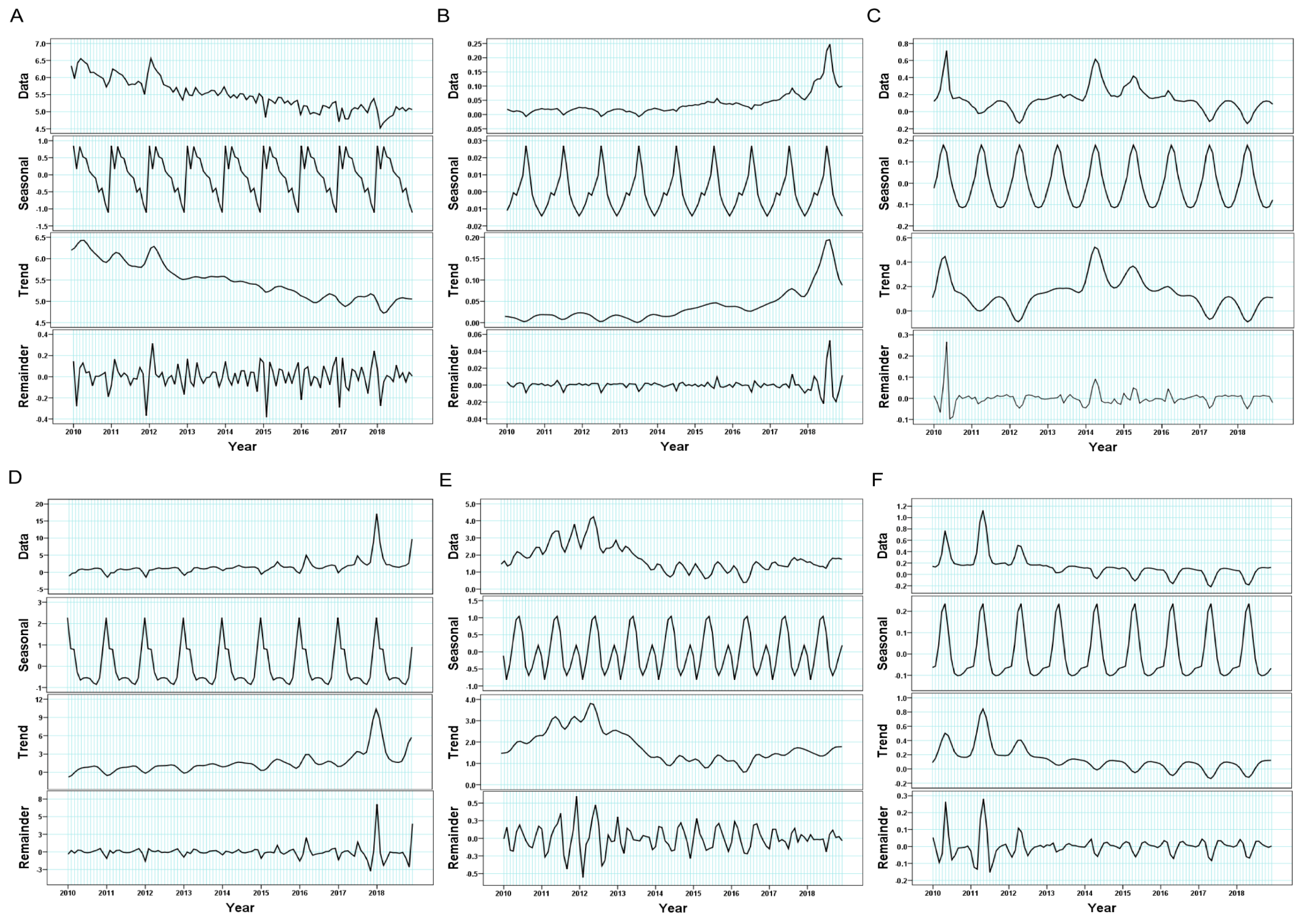
3.4. Seasonal Distributions of Incidence Rates of the Six Selected RIDs
3.5. Spatial Distribution of Incidence Rates for the Six Selected RIDs
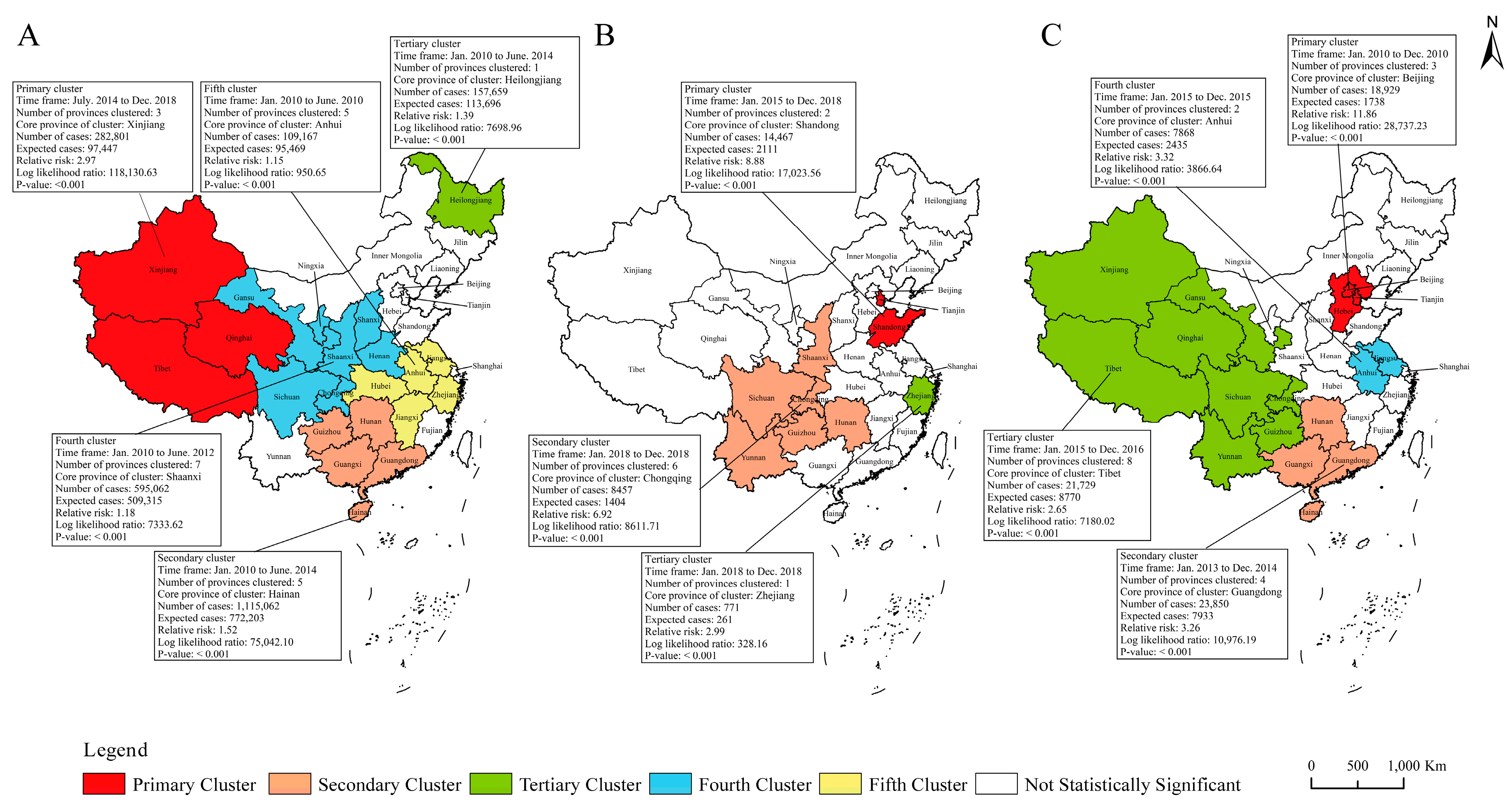
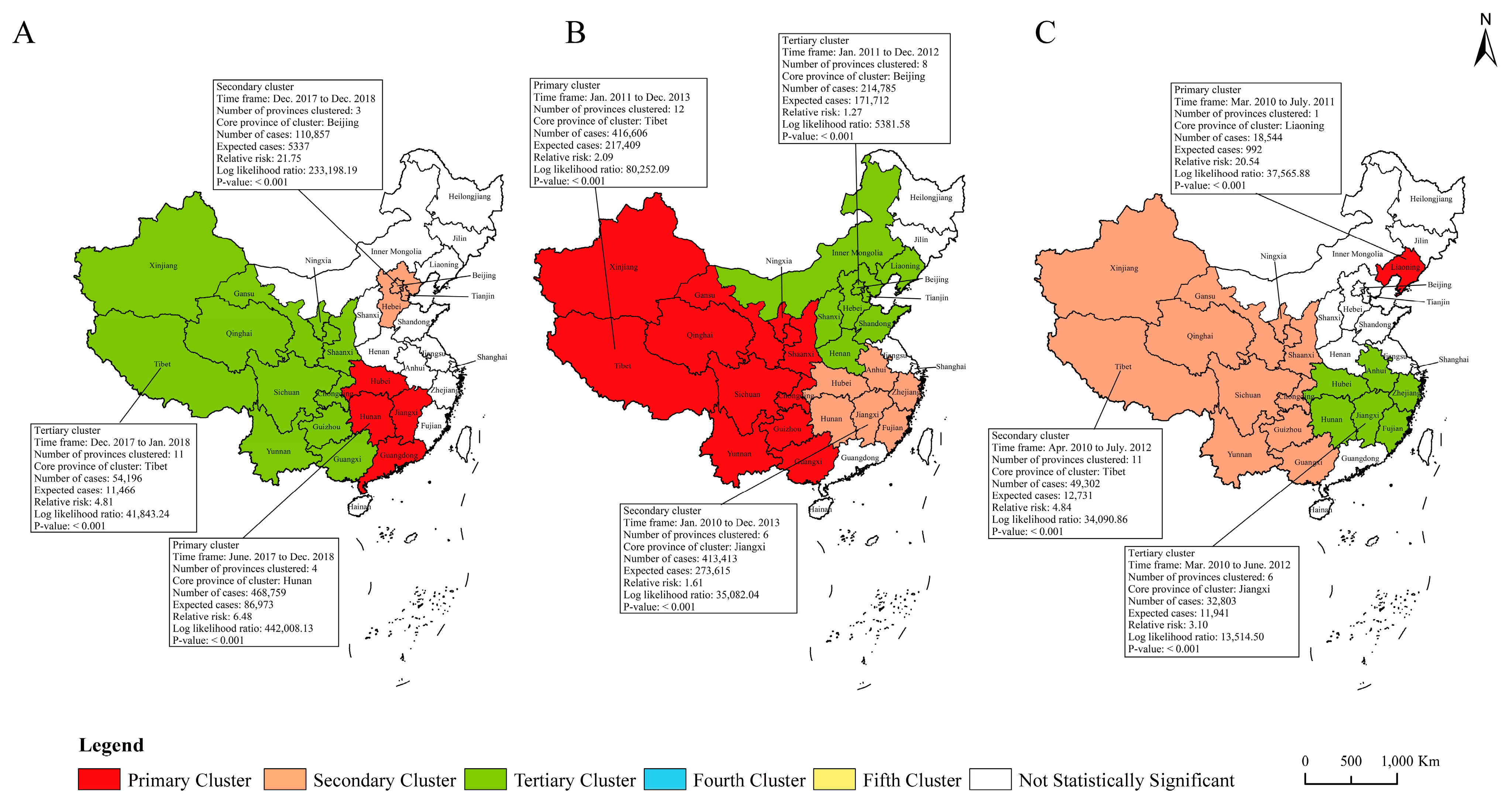
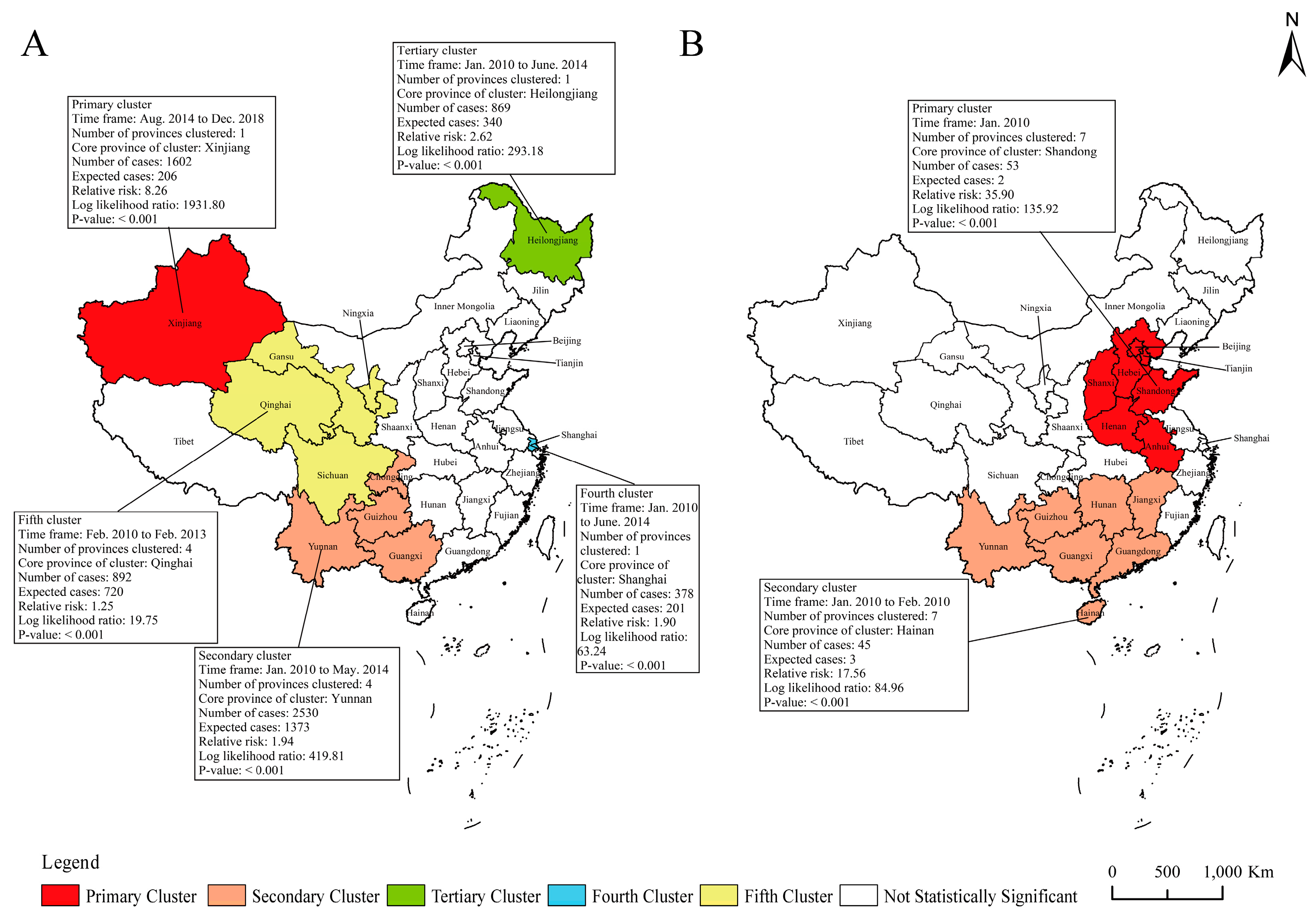
3.6. Spatiotemporal Clustering Analysis of Incidence Rates and Mortalities for the Six Selected RIDs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mao, Y.; He, R.X.; Zhu, B.; Liu, J.L.; Zhang, N. Notifiable respiratory infectious diseases in China: A spatial-temporal epidemiology analysis. Int. J. Environ. Res. Public Health 2020, 17, 2301. [Google Scholar] [CrossRef]
- Iuliano, A.D.; Roguski, K.M.; Chang, H.H.; Muscatello, D.J.; Palekar, R.; Tempia, S.; Cohen, C.; Gran, J.M.; Schanzer, D.; Cowling, B.J.; et al. Estimates of global seasonal influenza-associated respiratory mortality: A modelling study. Lancet 2018, 391, 1285–1300. [Google Scholar] [CrossRef]
- World Health Organization. Global Tuberculosis Report 2020. Available online: https://www.who.int/publications/i/item/9789240013131 (accessed on 15 March 2022).
- Jiang, Y.; Dou, X.; Yan, C.; Wan, L.; Liu, H.; Li, M.; Wang, R.; Li, G.; Zhao, L.; Liu, Z.; et al. Epidemiological characteristics and trends of notifiable infectious diseases in China from 1986 to 2016. J. Glob. Health 2020, 10, 020803. [Google Scholar] [CrossRef]
- Dong, Y.; Wang, L.; Burgner, D.P.; Miller, J.E.; Song, Y.; Ren, X.; Li, Z.; Yi, X.; Ma, J.; Susan, M.S.; et al. Infectious diseases in children and adolescents in China: Analysis of national surveillance data from 2008 to 2017. BMJ 2020, 369, m1043. [Google Scholar] [CrossRef]
- Wang, L.Q.; Wang, W.B. Temporal trends in notification and mortality of tuberculosis in China, 2004-2019: A joinpoint and age-period-cohort analysis. Int. J. Environ. Res. Public Health 2021, 18, 5607. [Google Scholar] [CrossRef]
- Zeng, L.; Zang, F.; Song, N.H.; Li, Z.J. Analysis of influenza trend and impact of COVID-19 in Kezhou, Xinjiang for 8 consecutive years. J. Med. Virol. 2022, 94, 3081–3086. [Google Scholar] [CrossRef]
- Public Health Data Center. Available online: https://www.phsciencedata.cn/Share/index.jsp (accessed on 23 February 2022).
- National Bureau of Statistics of China. Chinese Population Census in 2010. Available online: http://www.stats.gov.cn (accessed on 23 February 2022).
- National Health Commission of the People’s Republic of China. Notice on Adjusting the Management of Some Legal Infectious Diseases. Available online: http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=f6ee56b5508a4295a8d552ca5f0f5edd (accessed on 23 February 2022).
- Kim, H.J.; Fay, M.P.; Feuer, E.J.; Midthune, D.N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 2000, 19, 335–351. [Google Scholar] [CrossRef]
- Mao, Y.; Zhang, N.; Zhu, B.; Liu, J.L.; He, R.X. A descriptive analysis of the spatio-temporal distribution of intestinal infectious diseases in China. BMC Infect. Dis. 2019, 19, 766. [Google Scholar] [CrossRef]
- Kulldorff, M. Prospective time periodic geographical disease surveillance using a scan statistic. J. R. Stat. Soc. 2001, 164, 61–72. [Google Scholar] [CrossRef]
- Kiani, B.; Raouf Rahmati, A.; Bergquist, R.; Hashtarkhani, S.; Firouraghi, N.; Bagheri, N.; Moghaddas, E.; Mohammadi, A. Spatio-temporal epidemiology of the tuberculosis incidence rate in Iran 2008 to 2018. BMC Public Health 2021, 21, 1093. [Google Scholar] [CrossRef]
- Zhao, Z.X.; Zhao, J.; Ma, J.Q. Concept of an integrated information system for notifiable disease communicable surveillance in China. Disease Surveillence 2018, 33, 423–427. [Google Scholar]
- Uplekar, M.; Weil, D.; Lonnroth, K.; Jaramillo, E.; Lienhardt, C.; Dias, H.M.; Falzon, D.; Floyd, K.; Gargioni, G.; Getahun, H.; et al. WHO’s new end TB strategy. Lancet 2015, 385, 1799–1801. [Google Scholar] [CrossRef]
- Jiang, H.; Liu, M.Y.; Zhang, Y.J.; Yin, J.F.; Li, Z.W.; Zhu, C.; Li, Q.H.; Luo, X.Y.; Ji, T.T.; Zhang, J.J.; et al. Changes in incidence and epidemiological characteristics of pulmonary tuberculosis in mainland China, 2005-2016. JAMA Netw. Open 2021, 4, e215302. [Google Scholar] [CrossRef]
- Zou, X.; Zhou, L.; Wu, H.Z.; Chen, L.; Zhou, F.J.; Gong, C.; Ye, J.L.; Ling, L. The role of tuberculosis control institutes in delivering tuberculosis information to domestic migrants in China: A multi-level analysis of a nationwide cross-sectional survey. Int. J. Infect. Dis. 2019, 86, 94–101. [Google Scholar] [CrossRef]
- Cheng, J.; Sun, Y.N.; Zhang, C.Y.; Yu, Y.L.; Tang, L.H.; Peng, H.; Peng, Y.; Yao, Y.X.; Hou, S.Y.; Li, J.W.; et al. Incidence and risk factors of tuberculosis among the elderly population in China. a prospective cohort study. Infect. Dis. Poverty 2020, 9, 13. [Google Scholar] [CrossRef]
- World Health Organization. China Country Assessment Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2016; Available online: https.//www.who.int/ageing/publications/china-country-assessment/zh/ (accessed on 15 December 2022).
- Wang, R.P.; Jiang, Y.G.; Guo, X.Q.; Wu, Y.L.; Zhao, G.M. Influence of infectious disease seasonality on the performance of the outbreak detection algorithm in the China Infectious Disease Automated-alert and Response System. J. Int. Med. Res. 2018, 46, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Atkins, K.E.; Feng, L.Z.; Pang, M.; Zheng, Y.M.; Liu, X.X.; Cowling, B.J.; Yu, H.J. Seasonal influenza vaccination in China: Landscape of diverse regional reimbursement policy, and budget impact analysis. Vaccine 2016, 34, 5724–5735. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.J.; Yang, J.; Zhu, F.; Wang, L.J.; Guo, Q.; Tang, J.; Fang, Q.Q.; Wang, D.Y.; Chen, T. Influenza-like illness outbreaks in China during 2017-2018 surveillance season. Chin. J. Prev. Med. 2019, 53, 982–986. [Google Scholar]
- Zeng, X.X.; Xie, Y.R.; Chen, T.; Huang, W.J.; Tang, J.; Li, X.Y.; Wang, D.Y. Analysis of influenza outbreak characteristics in China from 2019 to 2020. Int. J. Virol. 2021, 5, 359–363. [Google Scholar]
- Dave, K.; Lee, P.C. Global Geographical and Temporal Patterns of Seasonal Influenza and Associated Climatic Factors. Epidemiol. Rev. 2019, 41, 51–68. [Google Scholar] [CrossRef]
- Diamond, C.; Gong, H.; Sun, F.Y.; Liu, Y.; Quilty, B.J.; Jit, M.; Yang, J.; Yu, H.J.; Edmunds, W.J.; Baguelinet, M. Regional-based within-year seasonal variations in influenza-related health outcomes across mainland China: A systematic review and spatio-temporal analysis. BMC Med. 2022, 20, 58. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Chen, Y.; Wang, X.; Yu, H. Influenza-associated disease burden in mainland China: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 2886. [Google Scholar] [CrossRef] [PubMed]
- National Health Commission of the People’s Republic of China. The Implementation of the Expanded National Immunization Plan. Available online: http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=37097 (accessed on 10 March 2022).
- Tan, H.Y.; Li, C.Y.; Xiao, L.; Liu, F.Q.; Wu, C.Q. Epidemiological characteristics and trend prediction of pertussis in Hunan Province from 2009 to 2018. Chin. J. Dis. Control Prev. 2020, 24, 1263–1268. [Google Scholar]
- Liu, Y.; You, X.L.; Han, Z.M. Epidemiological characteristics of pertussis and influencing factors in Chongqing. Mod. Prev. Med. 2021, 48, 1372–1374. [Google Scholar]
- Sealey, K.L.; Belcher, T.; Preston, A. Bordetella pertussis epidemiology and evolution in the light of pertussis resurgence. Infect. Genet. Evol. 2016, 40, 136–143. [Google Scholar] [CrossRef]
- Kim, C.; Yi, S.; Cho, S.I. Recent increase in pertussis incidence in Korea: An age-period-cohort analysis. Epidemiol. Health 2021, 43, e2021053. [Google Scholar] [CrossRef]
- Ma, C.; Rodewald, L.; Hao, L.; Su, Q.; Zhang, Y.; Wen, N.; Fan, C.X.; Yang, H.; Luo, H.M.; Wang, H.Q.; et al. Progress toward measles elimination—China, January 2013–June 2019. MMWR Morb. Mortal Wkly. Rep. 2019, 68, 1112–1116. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Zhang, Y.; Wang, H.; Zhu, Z.; Mao, N.; Mulders, M.N.; Rota, P.A. Global and national laboratory networks support high quality surveillance for measles and rubella. Int. Health 2017, 9, 184–189. [Google Scholar] [CrossRef]
- Geng, M.J.; Zhang, H.Y.; Yu, L.J.; Lv, C.L.; Wang, T.; Che, T.L.; Xu, Q.; Jiang, B.G.; Chen, J.J.; Hay, S.I.; et al. Changes in notifiable infectious disease incidence in China during the COVID-19 pandemic. Nat Commun. 2021, 12, 6923. [Google Scholar] [CrossRef]
- National Health Commission of the People’s Republic of China. Diagnostic Criteria for Mump. Available online: http://www.nhc.gov.cn/wjw/s9491/200704/38797.shtml (accessed on 21 March 2022).
- Borysiak, M.D.; Thompson, M.J.; Posner, J.D. Translating diagnostic assays from the laboratory to the clinic: Analytical and clinical metrics for device development and evaluation. Lab Chip. 2016, 16, 1293–1313. [Google Scholar] [CrossRef]
- World Health Organization. Global Influenza Strategy 2019–2030. Available online: https://www.who.int/publications/i/item/9789241515320 (accessed on 10 March 2022).

| Year | Pulmonary Tuberculosis | Pertussis | Measles | Seasonal Influenza | Mumps | Rubella | Others | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case (n) | Rate (1/100,000) | Case (n) | Rate (1/100,000) | Case (n) | Rate (1/100,000) | Case (n) | Rate (1/100,000) | Case (n) | Rate (1/100,000) | Case (n) | Rate (1/100,000) | Case (n) | Rate (1/100,000) | Case (n) | Rate (1/100,000) | |
| 2010 | 991,350 | 74.27 | 1764 | 0.13 | 38,159 | 2.86 | 71,625 | 5.37 | 298,932 | 22.40 | 43,117 | 3.23 | 21,202 | 1.59 | 1,466,149 | 109.85 |
| 2011 | 953,275 | 71.09 | 2517 | 0.19 | 9943 | 0.74 | 75,493 | 5.63 | 454,385 | 33.89 | 65,549 | 4.89 | 64,107 | 4.78 | 1,625,269 | 121.21 |
| 2012 | 951,508 | 70.62 | 2183 | 0.16 | 6183 | 0.46 | 123,212 | 9.15 | 479,518 | 35.59 | 40,156 | 2.98 | 46,655 | 3.46 | 1,649,415 | 122.42 |
| 2013 | 904,434 | 66.80 | 1712 | 0.13 | 27,646 | 2.04 | 140,714 | 10.39 | 327,759 | 24.21 | 17,580 | 1.30 | 34,430 | 2.54 | 1,454,275 | 107.40 |
| 2014 | 889,381 | 65.63 | 3408 | 0.25 | 52,628 | 3.88 | 215,533 | 15.91 | 187,500 | 13.84 | 11,793 | 0.87 | 54,745 | 4.04 | 1,414,988 | 104.41 |
| 2015 | 864,015 | 63.42 | 6658 | 0.49 | 42,361 | 3.11 | 195,723 | 14.37 | 182,833 | 13.42 | 8133 | 0.60 | 68,557 | 5.03 | 1,368,280 | 100.43 |
| 2016 | 836,236 | 61.00 | 5584 | 0.41 | 24,820 | 1.81 | 306,682 | 22.37 | 175,001 | 12.77 | 4535 | 0.33 | 59,647 | 4.35 | 1,412,505 | 103.04 |
| 2017 | 835,193 | 60.53 | 10,390 | 0.75 | 5941 | 0.43 | 456,718 | 33.10 | 252,740 | 18.32 | 1605 | 0.12 | 75,076 | 5.44 | 1,637,663 | 118.69 |
| 2018 | 823,342 | 59.27 | 22,057 | 1.59 | 3940 | 0.28 | 765,186 | 55.09 | 259,071 | 18.65 | 3930 | 0.28 | 78,970 | 5.69 | 1,956,496 | 140.85 |
| Provinces and Regions | Pulmonary Tuberculosis | Pertussis | Measles | Seasonal Influenza | Mumps | Rubella | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2010 (1/10,000) | 2018 (1/10,000) | Percentage Change (%) | 2010 (1/10,000) | 2018 (1/10,000) | Percentage Change (%) | 2010 (1/10,000) | 2018 (1/10,000) | Percentage Change (%) | 2010 (1/10,000) | 2018 (1/10,000) | Percentage Change (%) | 2010 (1/10,000) | 2018 (1/10,000) | Percentage Change (%) | 2010 (1/10,000) | 2018 (1/10,000) | Percentage Change (%) | |
| Beijing | 45.70 | 30.43 | −33.41 | 0.08 | 0.87 | 985.69 | 14.13 | 0.47 | −96.64 | 6.37 | 381.84 | 5894.07 | 16.56 | 9.04 | −45.41 | 6.21 | 0.27 | −95.69 |
| Tianjin | 25.54 | 21.39 | −16.26 | 0.99 | 5.27 | 430.87 | 16.22 | 0.42 | −97.39 | 4.69 | 18.02 | 284.16 | 17.44 | 7.07 | −59.49 | 6.71 | 0.12 | −98.18 |
| Hebei | 59.08 | 39.31 | −33.47 | 0.55 | 1.20 | 117.40 | 20.55 | 0.32 | −98.44 | 19.63 | 74.21 | 278.10 | 16.17 | 18.60 | 15.00 | 4.87 | 0.04 | −99.18 |
| Shanxi | 69.58 | 35.03 | −49.66 | 0.18 | 0.49 | 182.35 | 0.70 | 0.08 | −88.48 | 2.45 | 21.18 | 765.26 | 14.70 | 16.76 | 14.03 | 0.76 | 0.07 | −90.35 |
| Inner Mongolia | 74.07 | 54.09 | −26.98 | 0.02 | 0.19 | 819.52 | 2.83 | 0.27 | −90.51 | 1.44 | 12.57 | 772.48 | 7.75 | 9.31 | 20.11 | 3.84 | 0.06 | −98.46 |
| Liaoning | 60.10 | 55.81 | −7.14 | 0.01 | 0.01 | −20.91 | 0.96 | 0.05 | −94.75 | 2.97 | 6.41 | 115.82 | 25.64 | 7.04 | −72.54 | 19.64 | 0.04 | −99.81 |
| Jilin | 83.79 | 47.43 | −43.39 | 0.06 | 0.10 | 54.19 | 1.15 | 0.13 | −89.08 | 2.76 | 9.79 | 255.19 | 16.29 | 5.84 | −64.15 | 2.59 | 0.03 | −98.72 |
| Heilongjiang | 95.84 | 65.23 | −31.94 | 0.15 | 0.11 | −26.87 | 16.46 | 0.25 | −98.49 | 1.48 | 5.26 | 256.04 | 9.53 | 4.81 | −49.51 | 1.16 | 0.02 | −97.96 |
| Shanghai | 34.33 | 26.14 | −23.87 | 0.00 | 0.47 | - | 1.34 | 0.24 | −82.45 | 15.72 | 16.95 | 7.79 | 18.57 | 9.37 | −49.56 | 1.45 | 0.09 | −94.02 |
| Jiangsu | 53.93 | 31.02 | −42.49 | 0.05 | 0.17 | 227.11 | 0.95 | 0.12 | −86.89 | 3.56 | 14.67 | 311.75 | 7.19 | 9.81 | 36.38 | 1.23 | 0.05 | −95.55 |
| Zhejiang | 63.89 | 45.26 | −29.16 | 0.08 | 1.36 | 1621.93 | 2.22 | 0.35 | −84.29 | 7.84 | 166.33 | 2020.53 | 40.70 | 10.00 | −75.43 | 5.44 | 0.21 | −96.23 |
| Anhui | 64.49 | 51.08 | −20.80 | 0.06 | 0.34 | 446.85 | 0.72 | 0.22 | −68.96 | 4.63 | 43.55 | 840.10 | 20.11 | 25.54 | 27.00 | 2.92 | 0.16 | −94.52 |
| Fujian | 58.93 | 45.24 | −23.24 | 0.01 | 0.37 | 6669.91 | 0.06 | 0.15 | 129.83 | 7.93 | 51.61 | 550.88 | 23.67 | 7.76 | −67.21 | 4.70 | 0.93 | −80.19 |
| Jiangxi | 85.08 | 70.83 | −16.75 | 0.02 | 0.56 | 3447.95 | 0.31 | 0.06 | −79.99 | 6.09 | 37.97 | 523.13 | 20.58 | 14.40 | −30.05 | 1.69 | 0.05 | −96.92 |
| Shandong | 42.48 | 28.12 | −33.82 | 0.25 | 5.77 | 2223.91 | 1.88 | 0.10 | −94.68 | 3.48 | 14.97 | 329.73 | 6.72 | 6.92 | 2.94 | 0.55 | 0.03 | −93.82 |
| Henan | 73.11 | 55.16 | −24.56 | 0.08 | 0.32 | 281.91 | 2.37 | 0.64 | −72.83 | 4.30 | 36.70 | 752.95 | 16.17 | 20.95 | 29.61 | 1.52 | 0.02 | −98.62 |
| Hubei | 84.75 | 63.49 | −25.09 | 0.03 | 0.46 | 1553.63 | 0.93 | 0.60 | −35.57 | 3.71 | 92.56 | 2392.72 | 39.65 | 26.31 | −33.65 | 2.69 | 0.07 | −97.48 |
| Hunan | 88.59 | 78.75 | −11.11 | 0.04 | 2.90 | 7032.87 | 0.34 | 0.16 | −53.31 | 7.10 | 88.19 | 1141.66 | 30.31 | 44.36 | 46.36 | 3.35 | 0.29 | −91.42 |
| Guangdong | 99.51 | 64.81 | −34.87 | 0.02 | 2.22 | 12,488.53 | 0.67 | 0.29 | −56.25 | 7.37 | 165.08 | 2139.33 | 30.60 | 20.68 | −32.43 | 1.20 | 0.71 | −40.59 |
| Guangxi | 97.01 | 82.82 | −14.63 | 0.01 | 0.36 | 4273.88 | 0.05 | 0.05 | −4.42 | 3.63 | 44.03 | 1114.21 | 41.24 | 32.73 | −20.62 | 2.08 | 2.28 | 9.95 |
| Hainan | 109.66 | 85.05 | −22.43 | 0.00 | 0.27 | - | 0.03 | 0.10 | 187.40 | 4.07 | 31.82 | 681.12 | 72.81 | 80.06 | 9.96 | 0.32 | 1.38 | 324.94 |
| Chongqing | 89.90 | 73.37 | −18.39 | 0.05 | 7.05 | 13,343.58 | 0.30 | 0.18 | −39.46 | 3.54 | 18.89 | 433.23 | 50.98 | 21.51 | −57.80 | 2.13 | 0.18 | −91.77 |
| Sichuan | 81.74 | 57.34 | −29.85 | 0.24 | 1.56 | 537.39 | 0.71 | 0.17 | −76.91 | 1.98 | 10.28 | 419.82 | 16.76 | 18.21 | 8.68 | 2.57 | 0.23 | −90.99 |
| Guizhou | 129.14 | 114.06 | −11.68 | 0.06 | 1.51 | 2390.79 | 0.22 | 0.03 | −85.94 | 3.45 | 9.70 | 181.39 | 22.48 | 27.26 | 21.26 | 1.42 | 0.33 | −76.93 |
| Yunnan | 55.60 | 59.61 | 7.21 | 0.07 | 0.19 | 162.57 | 0.22 | 1.40 | 537.97 | 2.45 | 14.51 | 492.15 | 30.30 | 22.90 | −24.42 | 2.07 | 0.49 | −76.30 |
| Tibet | 118.34 | 166.66 | 40.84 | 0.00 | 0.03 | - | 1.31 | 0.53 | −59.25 | 2.24 | 0.86 | −61.62 | 15.27 | 31.68 | 107.38 | 60.00 | 0.24 | −99.60 |
| Shaanxi | 67.91 | 55.90 | −17.68 | 0.15 | 6.20 | 4076.18 | 2.20 | 0.19 | −91.22 | 2.10 | 37.64 | 1690.19 | 21.77 | 21.83 | 0.30 | 3.40 | 0.16 | −95.32 |
| Gansu | 90.64 | 38.71 | −57.30 | 0.30 | 1.11 | 269.72 | 2.53 | 0.21 | −91.74 | 8.83 | 30.94 | 250.46 | 20.49 | 20.92 | 2.14 | 5.27 | 0.09 | −98.34 |
| Qinghai | 87.35 | 140.33 | 60.65 | 0.05 | 0.08 | 55.23 | 5.42 | 0.50 | −90.75 | 1.99 | 18.43 | 825.48 | 23.83 | 34.93 | 46.58 | 12.79 | 0.22 | −98.30 |
| Ningxia | 57.39 | 36.73 | −36.00 | 0.21 | 0.25 | 19.92 | 1.38 | 0.34 | −75.48 | 22.90 | 18.95 | −17.26 | 86.84 | 17.94 | −79.34 | 10.51 | 0.04 | −99.58 |
| Xinjiang | 164.46 | 304.94 | 85.42 | 0.77 | 1.65 | 113.08 | 1.43 | 0.36 | −74.48 | 4.73 | 25.54 | 440.53 | 23.46 | 19.45 | −17.09 | 3.95 | 0.12 | −96.99 |
| Whole mainland China | 74.27 | 59.27 | −20.20 | 0.13 | 1.59 | 1123.08 | 2.86 | 0.28 | −90.21 | 5.37 | 55.09 | 925.88 | 22.40 | 18.65 | 16.74 | 3.23 | 0.28 | 91.33 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deng, L.; Han, Y.; Wang, J.; Liu, H.; Li, G.; Wang, D.; He, G. Epidemiological Characteristics of Notifiable Respiratory Infectious Diseases in Mainland China from 2010 to 2018. Int. J. Environ. Res. Public Health 2023, 20, 3946. https://doi.org/10.3390/ijerph20053946
Deng L, Han Y, Wang J, Liu H, Li G, Wang D, He G. Epidemiological Characteristics of Notifiable Respiratory Infectious Diseases in Mainland China from 2010 to 2018. International Journal of Environmental Research and Public Health. 2023; 20(5):3946. https://doi.org/10.3390/ijerph20053946
Chicago/Turabian StyleDeng, Lele, Yajun Han, Jinlong Wang, Haican Liu, Guilian Li, Dayan Wang, and Guangxue He. 2023. "Epidemiological Characteristics of Notifiable Respiratory Infectious Diseases in Mainland China from 2010 to 2018" International Journal of Environmental Research and Public Health 20, no. 5: 3946. https://doi.org/10.3390/ijerph20053946
APA StyleDeng, L., Han, Y., Wang, J., Liu, H., Li, G., Wang, D., & He, G. (2023). Epidemiological Characteristics of Notifiable Respiratory Infectious Diseases in Mainland China from 2010 to 2018. International Journal of Environmental Research and Public Health, 20(5), 3946. https://doi.org/10.3390/ijerph20053946






