Evaluating the Effectiveness of Letter and Telephone Reminders in Promoting the Use of Specific Health Guidance in an At-Risk Population for Metabolic Syndrome in Japan: A Randomized Controlled Trial
Abstract
1. Introduction
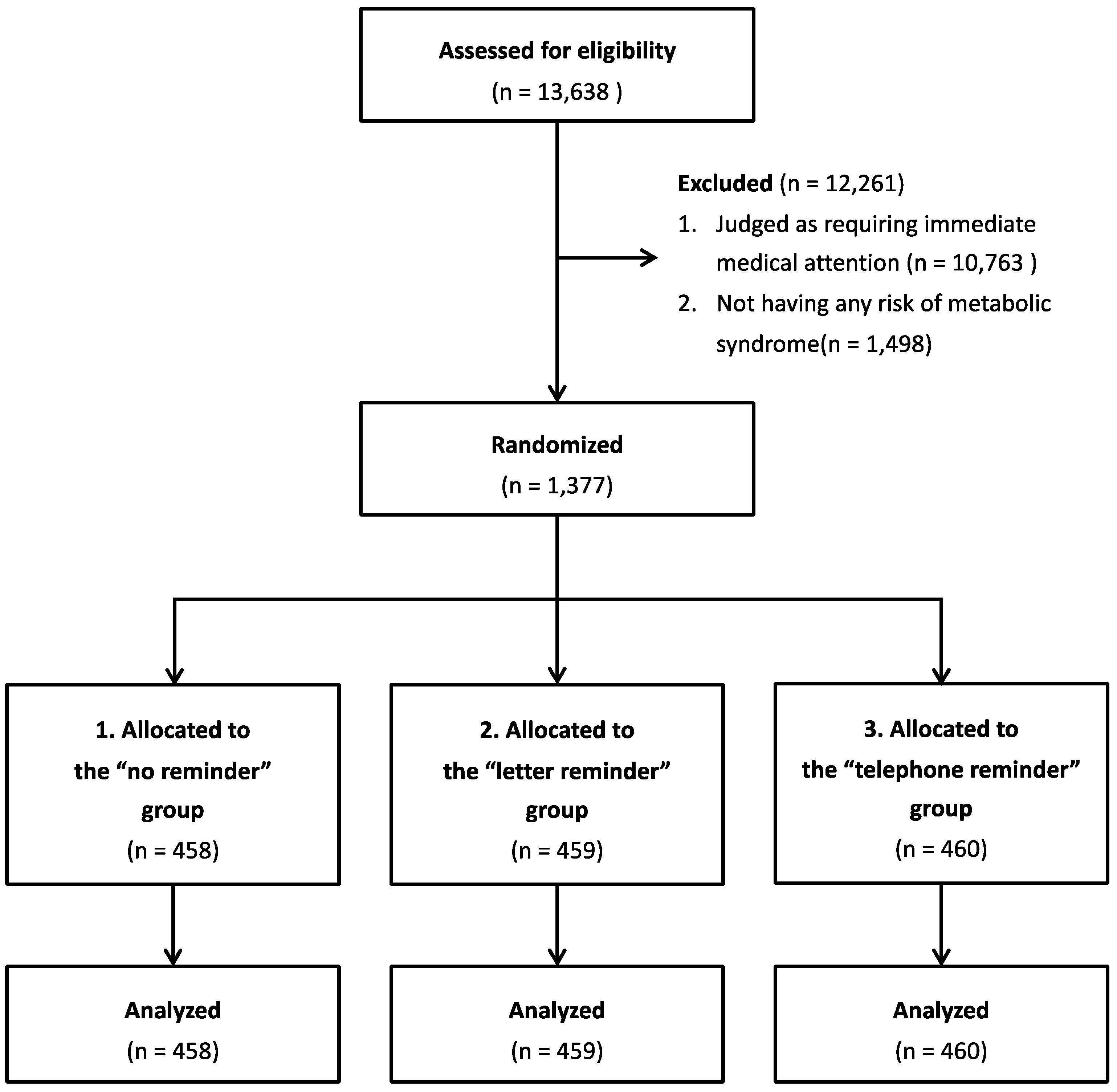
2. Materials and Methods
2.1. Sample and Procedures
2.2. Intervention
2.2.1. Letter Reminder
2.2.2. Telephone Reminder
2.3. Measures
2.3.1. Outcomes
2.3.2. Participants’ Characteristics
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- GBD. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- Park, Y.W.; Zhu, S.; Palaniappan, L.; Heshka, S.; Carnethon, M.R.; Heymsfield, S.B. The metabolic syndrome: Prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988–1994. Arch. Intern. Med. 2003, 163, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health. 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Tsushita, K.; Hosler, A.S.S.; Miura, K.; Ito, Y.; Fukuda, T.; Kitamura, A.; Tatara, K. Rationale and descriptive analysis of specific health guidance: The nationwide lifestyle intervention program targeting metabolic syndrome in Japan. J. Atheroscler. Thromb. 2018, 25, 308–322. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare. Data on Specific Health Checkups and Health Guidance. Available online: https://www.mhlw.go.jp/bunya/shakaihosho/iryouseido01/info02a-2.html (accessed on 1 December 2022).
- Khatlani, K.; Njike, V.; Costales, V.C. Effect of lifestyle intervention on cardiometabolic risk factors in overweight and obese women with polycystic ovary syndrome: A systematic review and meta-analysis. Metab. Syndr. Relat. Disord. 2019, 17, 473–485. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Stewart, R.A.H.; Benatar, J.R. Intensity and duration of lifestyle interventions for long-term weight loss and association with mortality: A meta-analysis of randomised trials. BMJ Open 2019, 9, e029966. [Google Scholar] [CrossRef] [PubMed]
- Sequi-Dominguez, I.; Alvarez-Bueno, C.; Martinez-Vizcaino, V.; Fernandez-Rodriguez, R.; Del Saz Lara, A.; Cavero-Redondo, I. Effectiveness of mobile health interventions promoting physical activity and lifestyle interventions to reduce cardiovascular risk among individuals with metabolic syndrome: Systematic review and meta-analysis. J. Med. Internet Res. 2020, 22, e17790. [Google Scholar] [CrossRef]
- Nieste, I.; Franssen, W.M.A.; Spaas, J.; Bruckers, L.; Savelberg, H.H.C.M.; Eijnde, B.O. Lifestyle interventions to reduce sedentary behaviour in clinical populations: A systematic review and meta-analysis of different strategies and effects on cardiometabolic health. Prev. Med. 2021, 148, 106593. [Google Scholar] [CrossRef]
- Jørgensen, T.; Jacobsen, R.K.; Toft, U.; Aadahl, M.; Glümer, C.; Pisinger, C. Effect of screening and lifestyle counselling on incidence of ischaemic heart disease in general population: Inter99 randomised trial. BMJ 2014, 348, g3617. [Google Scholar] [CrossRef]
- Fukuma, S.; Iizuka, T.; Ikenoue, T.; Tsugawa, Y. Association of the national health guidance intervention for obesity and cardiovascular risks with health outcomes among Japanese men. JAMA Intern. Med. 2020, 180, 1630–1637. [Google Scholar] [CrossRef] [PubMed]
- Baron, R.C.; Melillo, S.; Rimer, B.K.; Coates, R.J.; Kerner, J.; Habarta, N.; Chattopadhyay, S.; Sabatino, S.A.; Elder, R.; Leeks, K.J.; et al. Intervention to increase recommendation and delivery of screening for breast, cervical, and colorectal cancers by healthcare providers a systematic review of provider reminders. Am. J. Prev. Med. 2010, 38, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Sallis, A.; Sherlock, J.; Bonus, A.; Saei, A.; Gold, N.; Vlaev, I.; Chadborn, T. Pre-notification and reminder SMS text messages with behaviourally informed invitation letters to improve uptake of NHS Health Checks: A factorial randomised controlled trial. BMC Public Health 2019, 19, 1162. [Google Scholar] [CrossRef] [PubMed]
- Gidlow, C.J.; Ellis, N.J.; Riley, V.; Chadborn, T.; Bunten, A.; Iqbal, Z.; Ahmed, A.; Fisher, A.; Sugden, D.; Clark-Carter, D. Randomised controlled trial comparing uptake of NHS Health Check in response to standard letters, risk-personalised letters and telephone invitations. BMC Public Health 2019, 19, 224. [Google Scholar] [CrossRef] [PubMed]
- Cook, E.J.; Sharp, C.; Randhawa, G.; Guppy, A.; Gangotra, R.; Cox, J. Who uses NHS health checks? Investigating the impact of ethnicity and gender and method of invitation on uptake of NHS health checks. Int. J. Equity Health 2016, 15, 13. [Google Scholar] [CrossRef] [PubMed]
- Stone, T.J.; Brangan, E.; Chappell, A.; Harrison, V.; Horwood, J. Telephone outreach by community workers to improve uptake of NHS Health Checks in more deprived localities and minority ethnic groups: A qualitative investigation of implementation. J. Public Health 2020, 42, e198–e206. [Google Scholar] [CrossRef]
- Gidlow, C.; Ellis, N.; Randall, J.; Cowap, L.; Smith, G.; Iqbal, Z.; Kumar, J. Method of invitation and geographical proximity as predictors of NHS Health Check uptake. J. Public Health 2015, 37, 195–201. [Google Scholar] [CrossRef]
- Ellis, N.; Gidlow, C.; Cowap, L.; Randall, J.; Iqbal, Z.; Kumar, J. A qualitative investigation of non-response in NHS health checks. Arch. Public Health 2015, 73, 14. [Google Scholar] [CrossRef] [PubMed]
- Albada, A.; Ausems, M.G.E.M.; Bensing, J.M.; van Dulmen, S. Tailored information about cancer risk and screening: A systematic review. Patient Educ. Couns. 2009, 77, 155–171. [Google Scholar] [CrossRef]
- Edwards, A.G.K.; Naik, G.; Ahmed, H.; Elwyn, G.J.; Pickles, T.; Hood, K.; Playle, R. Personalised risk communication for informed decision making about taking screening tests. Cochrane Database Syst. Rev. 2013, 2013, CD001865. [Google Scholar] [CrossRef] [PubMed]
- Brangan, E.; Stone, T.J.; Chappell, A.; Harrison, V.; Horwood, J. Patient experiences of telephone outreach to enhance uptake of NHS Health Checks in more deprived communities and minority ethnic groups: A qualitative interview study. Health Expect. 2019, 22, 364–372. [Google Scholar] [CrossRef] [PubMed]
| Variable | Category | Total n = 1377 | 1. No Reminder n = 458 | 2. Letter Reminder n = 459 | 3. Telephone Reminder n = 460 | p |
|---|---|---|---|---|---|---|
| Sex | Men | 1073 (77.9) | 357 (77.9) | 357 (77.8) | 359 (78.0) | 0.995 a |
| Age (years old) | 63.1 ± 10.0 | 63.3 ± 9.8 | 63.0 ± 10.0 | 62.9 ± 10.1 | 0.857 c | |
| Waist circumference (cm) | 92.3 ± 6.0 | 92.3 ± 5.8 | 92.1 ± 5.6 | 92.6 ± 6.5 | 0.841 c | |
| Body mass index (kg/m2) | 25.5 ± 2.8 | 25.5 ± 2.6 | 25.4 ± 2.7 | 25.6 ± 2.9 | 0.721 c | |
| Diastolic blood pressure (mmHg) | 126.7 ± 9.8 | 126.5 ± 10.1 | 127.4 ± 9.2 | 126.3 ± 10.1 | 0.549 c | |
| Systolic blood pressure (mmHg) | 76.5 ± 8.3 | 75.9 ± 9.1 | 76.8 ± 7.9 | 76.7 ± 7.9 | 0.473 c | |
| HbA1c (%) | 5.5 ± 0.3 | 5.5 ± 0.3 | 5.5 ± 0.4 | 5.5 ± 0.3 | 0.409 c | |
| Fasting blood glucose (mg/dl) | 97.7 ± 10.7 | 97.4 ± 10.3 | 98.2 ± 11.2 | 97.4 ± 10.6 | 0.753 c | |
| Triglyceride (mg/dl) | 134.5 ± 62.1 | 136.6 ± 62.0 | 131.0 ± 63.2 | 135.8 ± 61.2 | 0.290 c | |
| High-density lipoprotein cholesterol (mg/dl) | 57.7 ± 15.9 | 57.9 ± 15.8 | 58.0 ± 16.5 | 57.1 ± 15.3 | 0.766 c | |
| History of diseases | Cerebrovascular diseases | 14 (1.0) | 2 (0.4) | 7 (1.5) | 5 (1.1) | 0.103 b |
| Cardiovascular diseases | 51 (3.7) | 17 (3.7) | 12 (2.6) | 22 (4.8) | 0.220 a | |
| Chronic kidney failure or under dialysis therapy | 2 (0.1) | 1 (0.2) | 0 (0.0) | 1 (0.2) | 0.606 b | |
| Smoking habits | Having | 267 (19.4) | 82 (17.9) | 82 (17.9) | 103 (22.4) | 0.137 a |
| Exercise habits | Having | 584 (42.4) | 207 (45.2) | 179 (39.0) | 198 (43.0) | 0.156 a |
| Frequency of drinking | Every day | 448 (32.5) | 154 (33.5) | 154 (33.6) | 140 (30.4) | 0.390 c |
| Sometimes | 394 (28.6) | 132 (28.8) | 118 (25.7) | 144 (31.3) | ||
| Rarely/never | 535 (38.9) | 172 (37.6) | 187 (40.7) | 176 (38.3) |
| Variable | Category | 1. No Reminder n = 458 | 2. Letter Reminder n = 459 | 3. Telephone Reminder n = 460 | p | |
|---|---|---|---|---|---|---|
| Among Three Groups | Multiple Comparison a | |||||
| Utilization of specific health guidance | Yes | 48 (10.5) | 70 (15.3) | 63 (13.7) | 0.093 (χ2 = 4.753) | 1 vs. 2: 0.038 1 vs. 3: 0.156 2 vs. 3: 0.513 |
| No | 410 (89.5) | 389 (84.7) | 397 (86.3) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murayama, H.; Shimada, S.; Morito, K.; Maeda, H.; Takahashi, Y. Evaluating the Effectiveness of Letter and Telephone Reminders in Promoting the Use of Specific Health Guidance in an At-Risk Population for Metabolic Syndrome in Japan: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2023, 20, 3784. https://doi.org/10.3390/ijerph20053784
Murayama H, Shimada S, Morito K, Maeda H, Takahashi Y. Evaluating the Effectiveness of Letter and Telephone Reminders in Promoting the Use of Specific Health Guidance in an At-Risk Population for Metabolic Syndrome in Japan: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2023; 20(5):3784. https://doi.org/10.3390/ijerph20053784
Chicago/Turabian StyleMurayama, Hiroshi, Setaro Shimada, Kosuke Morito, Haruna Maeda, and Yuta Takahashi. 2023. "Evaluating the Effectiveness of Letter and Telephone Reminders in Promoting the Use of Specific Health Guidance in an At-Risk Population for Metabolic Syndrome in Japan: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 20, no. 5: 3784. https://doi.org/10.3390/ijerph20053784
APA StyleMurayama, H., Shimada, S., Morito, K., Maeda, H., & Takahashi, Y. (2023). Evaluating the Effectiveness of Letter and Telephone Reminders in Promoting the Use of Specific Health Guidance in an At-Risk Population for Metabolic Syndrome in Japan: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 20(5), 3784. https://doi.org/10.3390/ijerph20053784







