Changes of Oral and Physical Functions in Older Japanese Who Participated in Keyboard Harmonica and Exercise Classes during COVID-19-Related Movement Restrictions
Abstract
1. Introduction
2. Materials and Methods
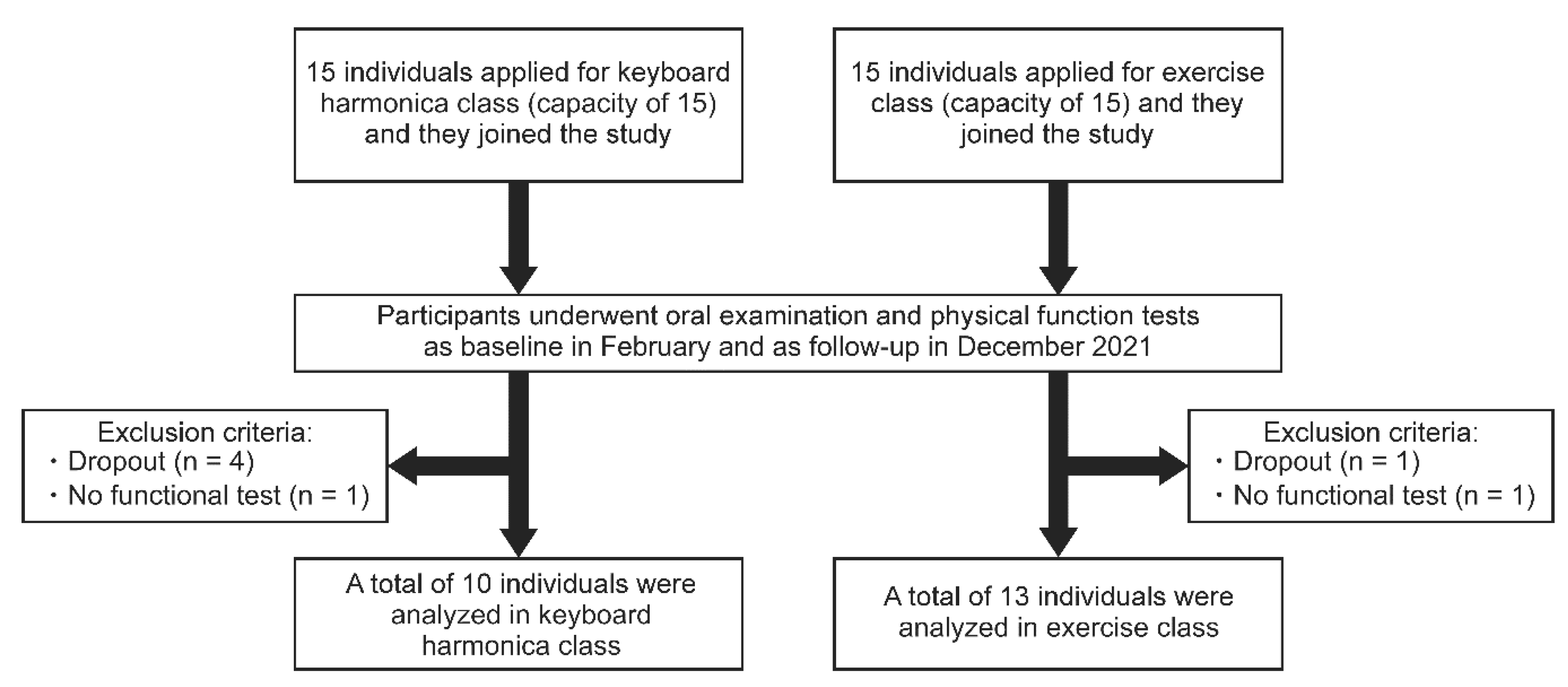
2.1. Participants and Study Design
2.2. Contents of Each Frailty-Prevention Class
2.3. Oral Function
2.3.1. Number of Remaining Teeth
2.3.2. Occlusal Force
2.3.3. Oral Diadochokinesis (ODK)
2.3.4. Tongue Strength
2.3.5. Masticatory Performance
2.4. Physical Function
2.4.1. Grip Strength
2.4.2. Open-Eyed One-Leg Standing Time
2.4.3. Five Times Sit-to-Stand Test
2.4.4. 5 m Gait Speed
2.4.5. 3 m Timed up & Go Test (TUG)
2.5. Body Composition
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Maalouf, A.; Maalouf, H. Impact of COVID-19 pandemic on medical waste management in Lebanon. Waste Manag. Res. 2021, 39, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Cabinet Secretariat Measures to be Taken Based on the Basic Response Policy. Available online: https://corona.go.jp/en/emergency/ (accessed on 28 December 2022).
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Otobe, Y.; Suzuki, M.; Koyama, S.; Kikuchi, T.; Kusumi, H.; Arai, H. The influence of the COVID-19 pandemic on physical activity and new incidence of frailty among initially non-frail older adults in Japan: A follow-up online survey. J. Nutr. Health Aging 2021, 25, 751–756. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Imaoka, M.; Nakao, H.; Hida, M.; Imai, R.; Tazaki, F.; Takeda, M. Increased anxiety about falls and walking ability among community-dwelling Japanese older adults during the COVID-19 pandemic. Psychogeriatrics 2021, 21, 826–831. [Google Scholar] [CrossRef] [PubMed]
- Krendl, A.C.; Perry, B.L. The impact of sheltering in place during the COVID-19 pandemic on older adults’ social and mental well-being. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021, 76, e53–e58. [Google Scholar] [CrossRef] [PubMed]
- Akita, M.; Otaki, N.; Yokoro, M.; Yano, M.; Tanino, N.; Fukuo, K. Relationship between social activity and frailty in Japanese older women during restriction on outings due to COVID-19. Can. Geriatr. J. 2021, 24, 320–324. [Google Scholar] [CrossRef] [PubMed]
- Son, B.K.; Imoto, T.; Inoue, T.; Nishimura, T.; Tanaka, T.; Iijima, K. Social detachment influenced muscle mass and strength during the COVID-19 pandemic in Japanese community-dwelling older women. J. Frailty Aging 2022, 11, 231–235. [Google Scholar] [CrossRef] [PubMed]
- López, J.; Perez-Rojo, G.; Noriega, C.; Carretero, I.; Velasco, C.; Martinez-Huertas, J.A.; López-Frutos, P.; Galarraga, L. Psychological well-being among older adults during the COVID-19 outbreak: A comparative study of the young-old and the old-old adults. Int. Psychogeriatr. 2020, 32, 1365–1370. [Google Scholar] [CrossRef] [PubMed]
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Otobe, Y.; Suzuki, M.; Koyama, S.; Kikuchi, T.; Kusumi, H.; Arai, H. Effect of the COVID-19 epidemic on physical activity in community-dwelling older adults in Japan: A cross-sectional online survey. J. Nutr. Health Aging 2020, 24, 948–950. [Google Scholar] [CrossRef]
- Chen, K. Use of gerontechnology to assist older adults to cope with the COVID-19 pandemic. J. Am. Med. Dir. Assoc. 2020, 21, 983–984. [Google Scholar] [CrossRef] [PubMed]
- Valenzuela, P.L.; Santos-Lozano, A.; Lista, S.; Serra-Rexach, J.A.; Emanuele, E.; Lucia, A. Coronavirus lockdown: Forced inactivity for the oldest old? J. Am. Med. Dir. Assoc. 2020, 21, 988–989. [Google Scholar] [CrossRef]
- Kojima, M.; Satake, S.; Osawa, A.; Arai, H. Management of frailty under COVID-19 pandemic in Japan. Glob. Health Med. 2021, 3, 196–202. [Google Scholar] [CrossRef]
- Liao, M.Y.; Yeh, C.J.; Liao, C.C.; Lee, S.H.; Yang, S.F.; Lee, M.C. Effects of receiving and providing family support on mortality in non-frail, pre-frail and frail older adults in Taiwan: A 12-year follow-up longitudinal study. Eur. Geriatr. Med. 2018, 9, 679–685. [Google Scholar] [CrossRef]
- Hybels, C.F.; Blazer, D.G.; Pieper, C.F. Toward a threshold for subthreshold depression: An analysis of correlates of depression by severity of symptoms using data from an elderly community sample. Gerontologist 2001, 41, 357–365. [Google Scholar] [CrossRef]
- Dent, E.; Morley, J.E.; Cruz-Jentoft, A.J.; Woodhouse, L.; Rodríguez-Mañas, L.; Fried, L.P.; Woo, J.; Aprahamian, I.; Sanford, A.; Lundy, J.; et al. Physical frailty: ICFSR international clinical practice guidelines for identification and management. J. Nutr. Health Aging 2019, 23, 771–787. [Google Scholar] [CrossRef]
- Miller, P.D. Miller classification of marginal tissue recession revisited after 35 years. Compend. Contin. Educ. Dent. 2018, 39, 514–520. [Google Scholar] [PubMed]
- Mizutani, S.; Egashira, R.; Yamaguchi, M.; Tamai, K.; Yoshida, M.; Kato, T.; Umezaki, Y.; Aoki, H.; Naito, T. Changes in oral and cognitive functions among older Japanese dental outpatients: A 2-year follow-up study. J. Oral Rehabil. 2021, 48, 1150–1159. [Google Scholar] [CrossRef] [PubMed]
- Iyota, K.; Mizutani, S.; Oku, S.; Asao, M.; Futatsuki, T.; Inoue, R.; Imai, Y.; Kashiwazaki, H. A cross-sectional study of age-related changes in oral function in healthy Japanese individuals. Int. J. Environ. Res. Public Health 2020, 17, 1376. [Google Scholar] [CrossRef]
- Minakuchi, S.; Tsuga, K.; Ikebe, K.; Ueda, T.; Tamura, F.; Nagao, K.; Furuya, J.; Matsuo, K.; Yamamoto, K.; Kanazawa, M.; et al. Oral hypofunction in the older population: Position paper of the Japanese Society of Gerodontology in 2016. Gerodontology 2018, 35, 317–324. [Google Scholar] [CrossRef]
- Komagamine, Y.; Kanazawa, M.; Minakuchi, S.; Uchida, T.; Sasaki, Y. Association between masticatory performance using a colour-changeable chewing gum and jaw movement. J. Oral Rehabil. 2011, 38, 555–563. [Google Scholar] [CrossRef] [PubMed]
- Shinkai, S.; Watanabe, S.; Kumagai, S.; Fujiwara, Y.; Amano, H.; Yoshida, H.; Ishizaki, T.; Yukawa, H.; Suzuki, T.; Shibata, H. Walking speed as a good predictor for the onset of functional dependence in a Japanese rural community population. Age Ageing 2000, 29, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef] [PubMed]
- Podsiadlo, D.; Richardson, S. The timed “up & go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Bott, J.; Blumenthal, S.; Buxton, M.; Ellum, S.; Falconer, C.; Garrod, R.; Harvey, A.; Hughes, T.; Lincoln, M.; Mikelsons, C.; et al. British Thoracic Society Physiotherapy Guideline Development Group guidelines for the physiotherapy management of the adult, medical, spontaneously breathing patient. Thorax 2009, 64, i1–i51. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, J.; Furukawa, Y.; Kobinata, N.; Yoshikawa, H.; Araki, F.; Yagyu, A.; Iwasaka, Y. Combined effect of pulmonary rehabilitation and music therapy in patients with chronic obstructive pulmonary disease. J. Phys. Ther. Sci. 2021, 33, 779–783. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.R.; Sudati, I.P.; Konzen, V.M.; de Campos, A.C.; Wibelinger, L.M.; Correa, C.; Miguel, F.M.; Silva, R.N.; Borghi-Silva, A. COVID-19 and the impact on the physical activity level of elderly people: A systematic review. Exp. Gerontol. 2022, 159, 111675. [Google Scholar] [CrossRef]
- Hirose, T.; Sawaya, Y.; Ishizaka, M.; Hashimoto, N.; Ito, A.; Endo, Y.; Kobayashi, K.; Yakabi, A.; Onoda, K.; Hara, T.; et al. Characteristics of Japanese older adults whose trunk muscle mass decreased during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2022, 19, 11438. [Google Scholar] [CrossRef]
- Klempel, N.; Blackburn, N.E.; McMullan, I.L.; Wilson, J.J.; Smith, L.; Cunningham, C.; O’Sullivan, R.; Caserotti, P.; Tully, M.A. The effect of chair-based exercise on physical function in older adults: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2021, 18, 1902. [Google Scholar] [CrossRef]
- Runacres, A.; Mackintosh, K.A.; Knight, R.L.; Sheeran, L.; Thatcher, R.; Shelley, J.; McNarry, M.A. Impact of the COVID-19 pandemic on sedentary time and behaviour in children and adults: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2021, 18, 11286. [Google Scholar] [CrossRef]
- Marconcin, P.; Werneck, A.O.; Peralta, M.; Ihle, A.; Gouveia, É.R.; Ferrari, G.; Sarmento, H.; Marques, A. The association between physical activity and mental health during the first year of the COVID-19 pandemic: A systematic review. BMC Public Health 2022, 22, 209. [Google Scholar] [CrossRef]
- O’Brien, W.J.; Badenhorst, C.E.; Draper, N.; Basu, A.; Elliot, C.A.; Hamlin, M.J.; Batten, J.; Lambrick, D.; Faulkner, J. Physical activity, mental health and wellbeing during the first COVID-19 containment in New Zealand: A cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 12036. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Beltrán-Velasco, A.I.; Ramos-Campo, D.J.; Mielgo-Ayuso, J.; Nikolaidis, P.A.; Belando, N.; Tornero-Aguilera, J.F. Physical activity and COVID-19. The basis for an efficient intervention in times of COVID-19 pandemic. Physiol. Behav. 2022, 244, 113667. [Google Scholar] [CrossRef]
- Smith, B.J.; Lim, M.H. How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Res. Pract. 2020, 30, 3022008. [Google Scholar] [CrossRef]
- Banerjee, D.; Rai, M. Social isolation in COVID-19: The impact of loneliness. Int. J. Soc. Psychiatry 2020, 66, 525–527. [Google Scholar] [CrossRef]
- Williams, C.Y.K.; Townson, A.T.; Kapur, M.; Ferreira, A.F.; Nunn, R.; Galante, J.; Phillips, V.; Gentry, S.; Usher-Smith, J.A. Interventions to reduce social isolation and loneliness during COVID-19 physical distancing measures: A rapid systematic review. PLoS ONE 2021, 16, e0247139. [Google Scholar] [CrossRef]
- Pérez, L.M.; Castellano-Tejedor, C.; Cesari, M.; Soto-Bagaria, L.; Ars, J.; Zambom-Ferraresi, F.; Baró, S.; Díaz-Gallego, F.; Vilaró, J.; Enfedaque, M.B.; et al. Depressive symptoms, fatigue and social relationships influenced physical activity in frail older community-dwellers during the Spanish lockdown due to the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 808. [Google Scholar] [CrossRef]
- Ciardo, A.; Simon, M.M.; Sonnenschein, S.K.; Büsch, C.; Kim, T.S. Impact of the COVID-19 pandemic on oral health and psychosocial factors. Sci. Rep. 2022, 12, 4477. [Google Scholar] [CrossRef]
| Variables | Total (n = 23) | Keyboard Harmonica (n = 10) | Exercise (n = 13) | p-Value | |
|---|---|---|---|---|---|
| Sex | Male | 5 (22) | 2 (20) | 3 (23) | 1.000 * |
| Female | 18 (78) | 8 (80) | 10 (77) | ||
| Age | 72 (68.0, 74.0) | 72 (69.0, 75.0) | 70 (65.5, 73.0) | 0.284 † | |
| Class participation (times) | 14.0 (14.0, 15.0) | 14.5 (14.0, 15.0) | 14.0 (13.0, 15.0) | 0.446 † | |
| Number of remaining teeth | 25.0 (22.0, 28.0) | 25.0 (19.8, 25.8) | 28.0 (24.0, 28.0) | 0.101 † | |
| Occlusal force (N) | 771 (617, 1117) | 720 (544, 870) | 884 (583, 1222) | 0.208 † | |
| ODK/pa/(times/s) | 6.6 (6.2, 7.0) | 6.6 (5.5, 7.0) | 6.6 (6.2, 7.1) | 0.648 † | |
| ODK/ta/(times/s) | 6.8 (6.4, 7.4) | 6.8 (5.7, 7.3) | 7.0 (6.4, 7.5) | 0.284 † | |
| ODK/ka/(times/s) | 6.4 (6.2, 6.6) | 6.6 (5.6, 6.7) | 6.2 (6.2, 6.7) | 0.738 † | |
| Tongue pressure (kPa) | 35.3 (31.7, 40.0) | 31.6 (23.9, 34.7) | 37.3 (35.1, 43.0) | 0.002 † | |
| Masticatory performance | 8.0 (8.0, 9.0) | 8.0 (8.0, 8.3) | 8.0 (8.0, 9.0) | 0.483 † | |
| Grip strength (kg) | 28.0 (23.5, 32.5) | 27.0 (23.0, 34.6) | 29.0 (24.5, 32.5) | 0.648 † | |
| Open-eyed one-leg standing time (s) | 120 (58, 120) | 107 (62, 120) | 120 (42, 120) | 0.784 † | |
| Five times sit-to-stand test (s) | 6.97 (5.85, 9.22) | 6.38 (5.46, 8.30) | 7.29 (6.02, 9.36) | 0.284 † | |
| 5 m gait speed (s) | 3.26 (2.79, 3.82) | 3.27 (2.79, 3.72) | 3.17 (2.80, 3.84) | 0.987 † | |
| 3 m TUG (s) | 5.40 (4.60, 6.95) | 5.28 (4.73, 6.87) | 5.40 (4.60, 7.01) | 0.976 † | |
| Total skeletal muscle mass (kg) | 35.3 (33.4, 39.0) | 35.6 (32.6, 40.4) | 35.2 (33.0, 42.0) | 0.948 † | |
| Total body fat (kg) | 15.0 (11.2, 17.1) | 14.8 (10.7, 18.2) | 15.1 (11.5, 17.0) | 0.744 † | |
| BMI | 21.4 (20.5, 23.2) | 21.2 (20.1, 25.3) | 21.4 (19.9, 22.4) | 0.784 † |
| Keyboard Harmonica (n = 10) | Exercise (n = 13) | Main Effect | Interactions (Time × Between Groups) | ||||
|---|---|---|---|---|---|---|---|
| Time | Between Groups | ||||||
| Variables | Baseline | Follow-Up | Baseline | Follow-Up | p-Value * | p-Value * | p-Value * |
| Occlusal force (N) | 696 ± 293 | 643 ± 343 | 899 ± 319 | 910 ± 318 | 0.680 | 0.072 | 0.528 |
| ODK/pa/(times/s) | 6.3 ± 1.1 | 6.8 ± 0.4 | 6.7 ± 0.4 | 6.7 ± 0.5 | 0.040 | 0.597 | 0.040 |
| ODK/ta/(times/s) | 6.5 ± 0.9 | 6.7 ± 0.6 | 7.0 ± 0.6 | 6.7 ± 0.7 | 0.633 | 0.351 | 0.074 |
| ODK/ka/(times/s) | 6.2 ± 0.7 | 6.2 ± 0.6 | 6.5 ± 0.5 | 6.3 ± 0.5 | 0.527 | 0.385 | 0.320 |
| Tongue pressure (kPa) | 30.9 ± 6.7 | 32.1 ± 6.6 | 39.2 ± 5.2 | 35.9 ± 5.1 | 0.441 | 0.008 | 0.114 |
| Masticatory performance | 8.1 ± 0.6 | 7.8 ± 1.2 | 8.2 ± 0.8 | 8.2 ± 0.6 | 0.394 | 0.368 | 0.394 |
| Grip strength (kg) | 29.7 ± 8.6 | 27.3 ± 7.9 | 31.1 ± 9.8 | 28.9 ± 9.5 | <0.001 | 0.694 | 0.890 |
| Open-eyed one-leg standing time (s) | 96 ± 28 | 101 ± 28 | 85 ± 47 | 96 ± 40 | 0.134 | 0.572 | 0.544 |
| Five times sit-to-stand test (s) | 6.83 ± 1.70 | 7.69 ± 2.24 | 7.59 ± 1.69 | 6.79 ± 1.71 | 0.915 | 0.915 | 0.010 |
| 5 m gait speed (s) | 3.40 ± 0.76 | 3.85 ± 1.59 | 3.33 ± 0.56 | 3.26 ± 0.27 | 0.465 | 0.241 | 0.321 |
| 3 m TUG (s) | 5.72 ± 1.14 | 6.00 ± 0.86 | 5.77 ± 1.37 | 5.76 ± 1.11 | 0.280 | 0.844 | 0.230 |
| Total skeletal muscle mass (kg) | 37.1 ± 6.6 | 36.6 ± 6.2 | 37.3 ± 6.4 | 37.3 ± 6.7 | 0.226 | 0.877 | 0.201 |
| Total body fat (kg) | 15.2 ± 5.9 | 15.7 ± 5.9 | 14.5 ± 4.7 | 13.7 ± 3.8 | 0.706 | 0.525 | 0.115 |
| Variables | Baseline | Follow-Up | p-Value * |
|---|---|---|---|
| BMI | 21.2 (20.1, 25.3) | 21.2 (19.4, 24.9) | 0.798 |
| Occlusal force (N) | 720 (544, 870) | 630 (327, 969) | 0.799 |
| ODK/pa/(times/s) | 6.6 (5.5, 7.0) | 6.8 (6.6, 7.1) | 0.046 |
| ODK/ta/(times/s) | 6.8 (5.7, 7.3) | 6.6 (6.6, 7.1) | 0.491 |
| ODK/ka/(times/s) | 6.6 (5.6, 6.7) | 6.2 (5.8, 6.7) | 0.856 |
| Tongue pressure (kPa) | 31.6 (23.9, 34.7) | 30.8 (27.4, 36.6) | 0.374 |
| Masticatory performance | 8.0 (8.0, 8.3) | 8.0 (7.0, 9.0) | 0.414 |
| Grip strength (kg) | 27.0 (23.0, 34.6) | 24.5 (21.4, 33.2) | 0.005 |
| Open-eyed one-leg standing time (s) | 107 (62, 120) | 120 (69, 120) | 0.500 |
| Five times sit-to-stand test (s) | 6.38 (5.46, 8.30) | 7.26 (5.79, 10.22) | 0.139 |
| 5 m gait speed (s) | 3.27 (2.79, 3.72) | 3.25 (2.76, 4.52) | 0.959 |
| 3 m TUG (s) | 5.28 (4.73, 6.87) | 5.60 (5.26, 6.86) | 0.203 |
| Total skeletal muscle mass (kg) | 35.6 (32.6, 40.4) | 35.0 (32.4, 39.5) | 0.017 |
| Total body fat (kg) | 14.8 (10.7, 18.2) | 14.8 (11.5, 19.1) | 0.214 |
| Variables | Baseline | Follow-Up | p-Value * |
|---|---|---|---|
| BMI | 21.4 (19.9, 22.4) | 21.4 (20.0, 22.2) | 0.123 |
| Occlusal force (N) | 884 (583, 1222) | 909 (657, 1086) | 0.753 |
| ODK/pa/(times/s) | 6.6 (6.2, 7.1) | 6.6 (6.1, 7.3) | 0.713 |
| ODK/ta/(times/s) | 7.0 (6.4, 7.5) | 6.4 (6.2, 7.4) | 0.070 |
| ODK/ka/(times/s) | 6.2 (6.2, 6.7) | 6.2 (5.9, 6.7) | 0.141 |
| Tongue pressure (kPa) | 37.3 (35.1, 43.0) | 36.2 (31.6, 39.0) | 0.055 |
| Masticatory performance | 8.0 (8.0, 9.0) | 8.0 (8.0, 9.0) | 1.000 |
| Grip strength (kg) | 29.0 (24.5, 32.5) | 24.7 (23.5, 32.1) | 0.003 |
| Open-eyed one-leg standing time (s) | 120 (42, 120) | 120 (59, 120) | 0.173 |
| Five times sit-to-stand test (s) | 7.29 (6.02, 9.36) | 6.29 (5.41, 8.13) | 0.100 |
| 5 m gait speed (s) | 3.17 (2.80, 3.84) | 3.26 (3.07, 3.51) | 0.700 |
| 3 m TUG (s) | 5.40 (4.60, 7.01) | 5.22 (4.96, 6.97) | 0.753 |
| Total skeletal muscle mass (kg) | 35.2 (33.0, 42.0) | 34.9 (32.4, 42.8) | 0.807 |
| Total body fat (kg) | 15.1 (11.5, 17.0) | 14.2 (10.8, 17.2) | 0.308 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mizutani, S.; Matsuzaki, H.; Iyota, K.; Tani, A.; Oku, S.; Tabuchi, H.; Fujiwara, A.; Hase-Tamaru, S.; Kishimoto, H.; Narazaki, K. Changes of Oral and Physical Functions in Older Japanese Who Participated in Keyboard Harmonica and Exercise Classes during COVID-19-Related Movement Restrictions. Int. J. Environ. Res. Public Health 2023, 20, 3700. https://doi.org/10.3390/ijerph20043700
Mizutani S, Matsuzaki H, Iyota K, Tani A, Oku S, Tabuchi H, Fujiwara A, Hase-Tamaru S, Kishimoto H, Narazaki K. Changes of Oral and Physical Functions in Older Japanese Who Participated in Keyboard Harmonica and Exercise Classes during COVID-19-Related Movement Restrictions. International Journal of Environmental Research and Public Health. 2023; 20(4):3700. https://doi.org/10.3390/ijerph20043700
Chicago/Turabian StyleMizutani, Shinsuke, Hideaki Matsuzaki, Kiyomi Iyota, Asuka Tani, Saori Oku, Hiroaki Tabuchi, Akiko Fujiwara, Shizuka Hase-Tamaru, Hiro Kishimoto, and Kenji Narazaki. 2023. "Changes of Oral and Physical Functions in Older Japanese Who Participated in Keyboard Harmonica and Exercise Classes during COVID-19-Related Movement Restrictions" International Journal of Environmental Research and Public Health 20, no. 4: 3700. https://doi.org/10.3390/ijerph20043700
APA StyleMizutani, S., Matsuzaki, H., Iyota, K., Tani, A., Oku, S., Tabuchi, H., Fujiwara, A., Hase-Tamaru, S., Kishimoto, H., & Narazaki, K. (2023). Changes of Oral and Physical Functions in Older Japanese Who Participated in Keyboard Harmonica and Exercise Classes during COVID-19-Related Movement Restrictions. International Journal of Environmental Research and Public Health, 20(4), 3700. https://doi.org/10.3390/ijerph20043700









