Incidental Pathologic Findings from Orthodontic Pretreatment Panoramic Radiographs
Abstract
1. Background
2. Methods
2.1. Data Collection
2.2. Statistical Analysis
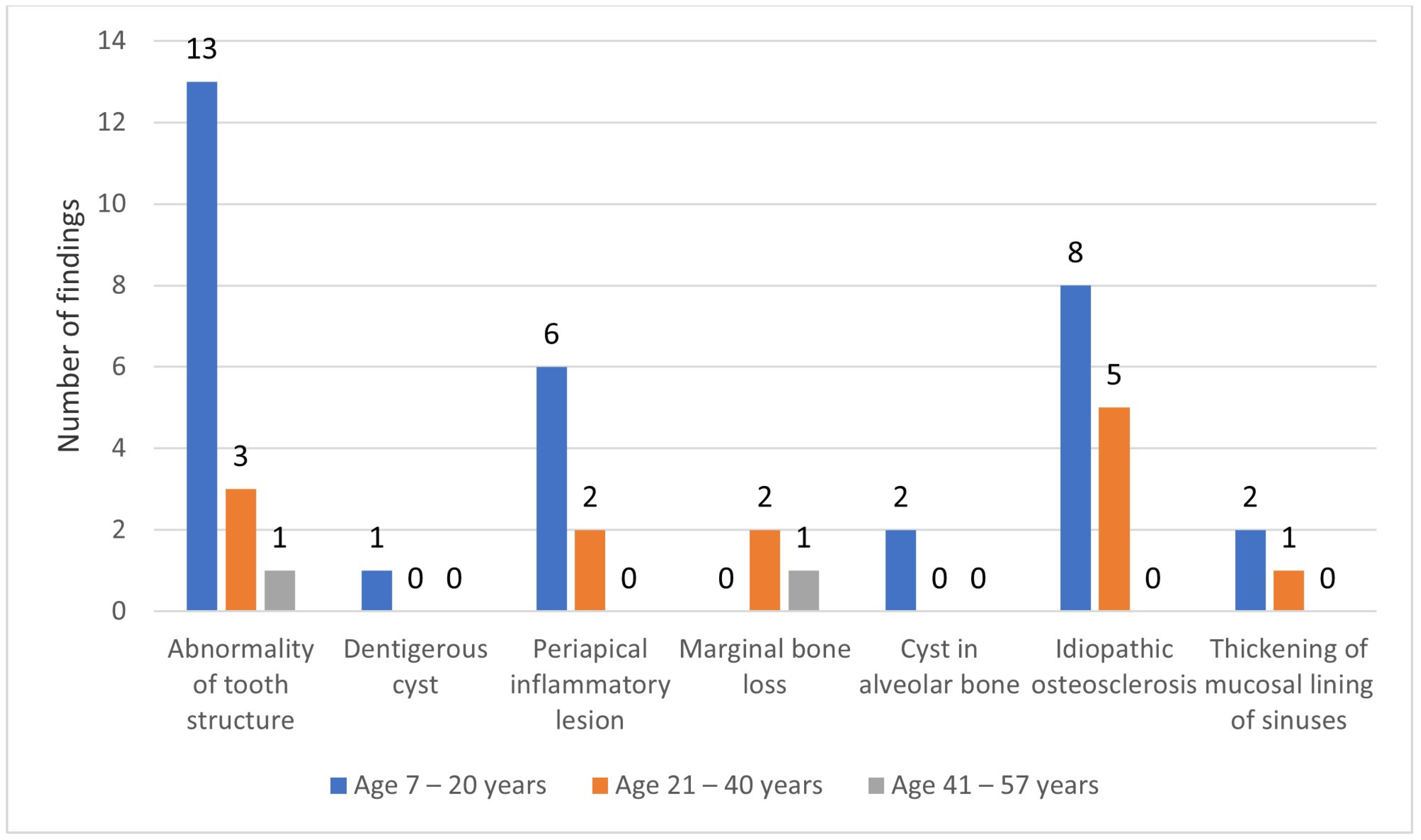
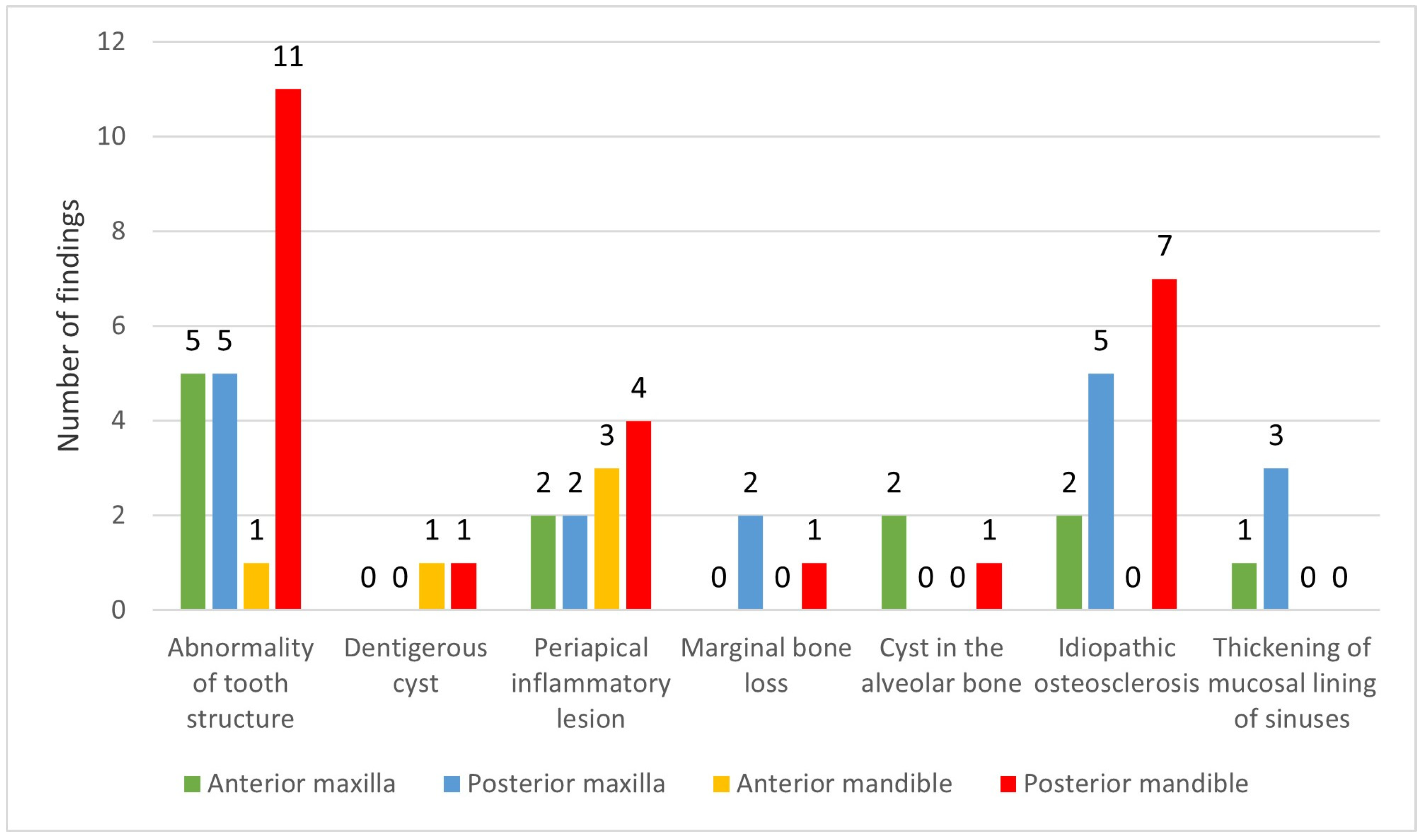
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 2D | Two-dimensional |
| IPFs | Incidental pathologic findings |
| IQR | Interquartile range |
| SPSS | Statistical Package for the Social Sciences |
References
- Stramotas, S.; Geenty, J.P.; Petocz, P.; Darendeliler, M.A. Accuracy of linear and angular measurements on panoramic radiographs taken at various positions in vitro. Eur. J. Orthod. 2002, 24, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Granlund, C.M.; Lith, A.; Molander, B.; Gröndahl, K.; Hansen, K.; Ekestubbe, A. Frequency of errors and pathology in panoramic images of young orthodontic patients. Eur. J. Orthod. 2012, 34, 452–457. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.-Y.; Oh, S.H.; Kim, S.-H.; Ahn, H.-W.; Kang, Y.-G.; Choi, Y.-S.; Kook, Y.-A.; Nelson, G. Effectiveness of 2D radiographs in detecting CBCT-based incidental findings in orthodontic patients. Sci. Rep. 2021, 11, 9280. [Google Scholar] [CrossRef] [PubMed]
- Akarslan, Z.Z.; Erten, H.; Güngör, K.; Celik, I. Common errors on panoramic radiographs taken in a dental school. J. Contemp. Dent. Pract. 2003, 4, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Okşayan, R.; Aktan, A.M.; Sökücü, O.; Haştar, E.; Ciftci, M.E. Does the panoramic radiography have the power to identify the gonial angle in orthodontics? Sci. World J. 2012, 2012, 219708. [Google Scholar] [CrossRef] [PubMed]
- Langlais, R.P.; Langland, O.E.; Nortjé, C.J. Diagnostic Imaging of the Jaws; Williams & Wilkinsons: Baltimore, MD, USA, 1995. [Google Scholar]
- Sameshima, G.T.; Asgarifar, K.O. Assessment of root resorption and root shape: Periapical vs panoramic films. Angle Orthod. 2001, 71, 185–189. [Google Scholar] [PubMed]
- Kuhlberg, A.J.; Norton, L.A. Pathologic findings in orthodontic radiographic images. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 182–184. [Google Scholar] [CrossRef]
- Thanyakarn, C.; Hansen, K.; Rohlin, M.; Akesson, L. Measurements of tooth length in panoramic radiographs. 1. The use of indicators. Dentomaxillofac. Radiol. 1992, 21, 26–30. [Google Scholar] [CrossRef]
- Soni, P.; Sharma, V.; Sengupta, J. Cervical vertebrae anomalies—Incidental findings on lateral cephalograms. Angle Orthod. 2008, 78, 176–180. [Google Scholar] [CrossRef]
- Rathi, M.; Fida, M. Pattern of dental anomalies in orthodontic patients at a tertiary care hospital. J. Pak. Dent. Assoc. 2013, 22, 232–235. [Google Scholar]
- Tetradis, S.; Kantor, M.L. Prevalence of skeletal and dental anomalies and normal variants seen in cephalometric and other radiographs of orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 572–577. [Google Scholar] [CrossRef]
- Bondemark, L.; Jeppsson, M.; Lindh-Ingildsen, L.; Rangne, K. Incidental findings of pathology and abnormality in pretreatment orthodontic panoramic radiographs. Angle Orthod. 2006, 76, 98–102. [Google Scholar]
- Bahaziq, A.; Jadu, F.M.; Jan, A.M.; Baghdady, M.; Feteih, R.M. A comparative study of the examination pattern of panoramic radiographs using Eye-tracking software. J. Contemp. Dent. Pract. 2019, 20, 1436–1441. [Google Scholar] [PubMed]
- Jose, M.; Varghese, J. Panoramic radiograph a valuable diagnostic tool in dental practice-Report of three cases. Int. J. Dent. Clin. 2011, 3, 47–49. [Google Scholar]
- Dobson, A.J.; Gebski, V.J. Sample Sizes for Comparing Two Independent Proportions Using the Continuity-Corrected Arc Sine Transformation. J. R. Stat. Soc. Ser. D Stat. Soc. 1986, 35, 51–53. [Google Scholar] [CrossRef]
- Ardakani, F.; Sheikhha, M.; Ahmadi, H. Prevalence of dental developmental anomalies: A radiographic study. Community Dent. Health 2007, 24, 140–144. [Google Scholar]
- Jadu, F.; Jan, A. Incidental findings on panoramic radiographs for pre-extraction assessment of third molars. Asian J. Sci. Technol. 2015, 6, 1539–1543. [Google Scholar]
- Yoga, S.; Vishwanath, R.; Sitra, G.; Vandana; John, B.; Kayalvizhi. Occult pathologies disclosed in panoramic radiographs: A retrospective study. Int. J. Curr. Res. 2017, 9, 49330–49333. [Google Scholar]
- Goncalves Filho, A.J.; Moda, L.B.; Oliveira, R.P.; Ribeiro, A.L.R.; Pinheiro, J.J.; Alver-Junior, S.M. Prevalence of dental anomalies on panoramic radiographs in a population of the state of Pará, Brazil. Indian J. Dent. Res. 2014, 25, 648–653. [Google Scholar]
- Cral, W.G.; Silveira, M.Q.; Rubira-Bullen, I.R.F.; Capelozza, A.L.A. Incidental findings in pretreatment and post-treatment orthodontic panoramic radiographs. Int. J. Radiol. Radiat. Ther. 2018, 5, 46–50. [Google Scholar]
- Hernández, G.; Plaza, S.P.; Cifuentes, D.; Villalobos, L.M.; Ruiz, L.M. Incidental findings in pre-orthodontic treatment radiographs. Int. Dent. J. 2018, 68, 320–326. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, D.; Yu, W. Incidental findings in a consecutive series of digital panoramic radiographs. Imaging Sci. Dent. 2020, 50, 53–64. [Google Scholar] [CrossRef] [PubMed]
- MacDonald-Jankowski, D. Idiopathic osteosclerosis in the jaws of Britons and of the Hong Kong Chinese: Radiology and systematic review. Dentomaxillofac. Radiol. 1999, 28, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Peltola, J.S. A panoramatomographic study of the teeth and jaws of Finnish university students. Community Dent. Oral Epidemiol. 1993, 21, 36–39. [Google Scholar] [CrossRef]
- Cederhag, J.; Lundegren, N.; Alstergren, P.; Shi, X.-Q.; Hellén-Halme, K. Evaluation of panoramic radiographs in relation to the mandibular third molar and to incidental findings in an adult population. Eur. J. Dent. 2021, 15, 266–272. [Google Scholar] [CrossRef]
- Vaseemuddin, S. Incidental findings on panoramic radiograph: A clinical study. J. Adv. Med. Dent. Sci. Res. 2016, 4, 223–226. [Google Scholar]
- Vallo, J.; Suominen-Taipale, L.; Huumonen, S.; Soikkonen, K.; Norblad, A. Prevalence of mucosal abnormalities of the maxillary sinus and their relationship to dental disease in panoramic radiography: Results from the Health 2000 Health Examination Survey. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, e80–e87. [Google Scholar] [CrossRef]
- Sanchez Trocino, B.; De la Fuente Hernandez, J.; Diaz Acevedo, J.; Vilar Pineda, G. Alterations and pathologies prevalence in panoramic radiographs in patients attending the university dental clinic. Int. J. Odontostomatol. 2013, 7, 47–52. [Google Scholar] [CrossRef]
- Abdel-Kader, H.M. Medicolegal perspective: Interpretation of pretreatment orthodontic radiographs. World J. Orthod. 2008, 9, 14–20. [Google Scholar]
- Ghassemzadeh, S.; Sbricoli, L.; Frigo, A.C.; Bacci, C. Incidental findings detected with panoramic radiography: Prevalence calculated on a sample of 2017 cases treated at a major Italian trauma and cancer centre. Oral Radiol. 2021, 37, 507–517. [Google Scholar] [CrossRef]
- Indra, G.; Maragathavalli, G. Incidental findings in orthodontic patients studied using two dimensional images. J. Res. Med. Dent. Sci. 2021, 9, 330–335. [Google Scholar]
- Kang, H. The prevention and handling of the missing data. Korean J. Anesthesiol. 2013, 64, 402–406. [Google Scholar] [CrossRef] [PubMed]

| Location | Finding | Criteria |
|---|---|---|
| Tooth/tooth associated | Altered morphology | Radiographically unusual shape or size of the tooth |
| Dentigerous cyst | Radiolucent zone of more than 3 mm with well-defined borders around the crown of an unerupted tooth, epicenter just above the crown, and the cyst attaches at the cemento-enamel junction | |
| Periapical inflammatory lesion | Radiolucent or radiopaque change in association with a tooth apex with radiographically interrupted lamina dura | |
| Marginal bone loss | Distance between the cementoenamel junction and the alveolar bone crest larger than 2 mm | |
| Alveolar bone | Cyst | Centrally located radiolucency within the bone, round or oval and with well-defined borders and corticated thin radiopaque line |
| Idiopathic osteosclerosis | Radiopaque change, i.e., dense trabeculae calcifications with well- or ill-defined borders in the surrounding bone | |
| Sinuses | Thickening of mucosal lining | Density along the sinus floor or generalized density of the maxillary sinus or cystic (oval, well defined) density in any area of the sinus |
| Findings | Male | Female | Total | |
|---|---|---|---|---|
| Abnormality of tooth structure | Altered tooth morphology | 8 (17%) | 9 (19.1%) | 17 (36.1%) |
| IPF | Dentigerous cyst | 0 (-) | 1 (2.1%) | 1 (2.1%) |
| Periapical inflammatory lesion | 5 (10.6%) | 3 (6.4%) | 8 (17%) | |
| Marginal bone loss | 3 (6.4%) | 0 (-) | 3 (6.4%) | |
| Cyst in the alveolar bone | 0 (-) | 2 (4.3%) | 2 (4.3%) | |
| Idiopathic osteosclerosis | 8 (17%) | 5 (10.7%) | 13 (27.7%) | |
| Thickening of mucosal lining of sinuses | 2 (4.3%) | 1 (2.1%) | 3 (6.4%) | |
| Total | 26 (55.3%) | 21 (44.7) | 47 (100%) |
| Other Findings | Male | Females | Total |
|---|---|---|---|
| Impacted teeth | 18 (13.43%) | 31 (23.13%) | 49 (36.6%) |
| Widening of periodontal ligament | 6 (4.47%) | 10 (7.46%) | 16 (11.9%) |
| Pulp stones | 3 (2.2%) | 5 (3.7%) | 8 (5.9%) |
| Rotated teeth | 3 (2.2%) | 2 (1.5%) | 5 (3.7%) |
| Missing teeth | 11 (8.2%) | 12 (9%) | 23 (17.2%) |
| Unerupted potential impaction | 10 (7.5%) | 9 (6.7%) | 19 (14.2%) |
| Crowding | 2 (1.5%) | 6 (4.5%) | 8 (6%) |
| Spacing | 3 (2.2%) | 1 (0.7%) | 4 (3%) |
| Supernumerary teeth | 1 (0.7%) | 0 (-) | 1 (0.7%) |
| Retained deciduous teeth | 0 (-) | 1 (0.7%) | 1 (0.7%) |
| Total | 57 (42.5%) | 77 (57.5%) | 134 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hlongwa, P.; Moshaoa, M.A.L.; Musemwa, C.; Khammissa, R.A.G. Incidental Pathologic Findings from Orthodontic Pretreatment Panoramic Radiographs. Int. J. Environ. Res. Public Health 2023, 20, 3479. https://doi.org/10.3390/ijerph20043479
Hlongwa P, Moshaoa MAL, Musemwa C, Khammissa RAG. Incidental Pathologic Findings from Orthodontic Pretreatment Panoramic Radiographs. International Journal of Environmental Research and Public Health. 2023; 20(4):3479. https://doi.org/10.3390/ijerph20043479
Chicago/Turabian StyleHlongwa, Phumzile, Mpule Annah Lerato Moshaoa, Charity Musemwa, and Razia Abdool Gafaar Khammissa. 2023. "Incidental Pathologic Findings from Orthodontic Pretreatment Panoramic Radiographs" International Journal of Environmental Research and Public Health 20, no. 4: 3479. https://doi.org/10.3390/ijerph20043479
APA StyleHlongwa, P., Moshaoa, M. A. L., Musemwa, C., & Khammissa, R. A. G. (2023). Incidental Pathologic Findings from Orthodontic Pretreatment Panoramic Radiographs. International Journal of Environmental Research and Public Health, 20(4), 3479. https://doi.org/10.3390/ijerph20043479






