Contribution of Live Video to Physicians’ Remote Assessment of Suspected COVID-19 Patients in an Emergency Medical Communication Centre: A Retrospective Study and Web-Based Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
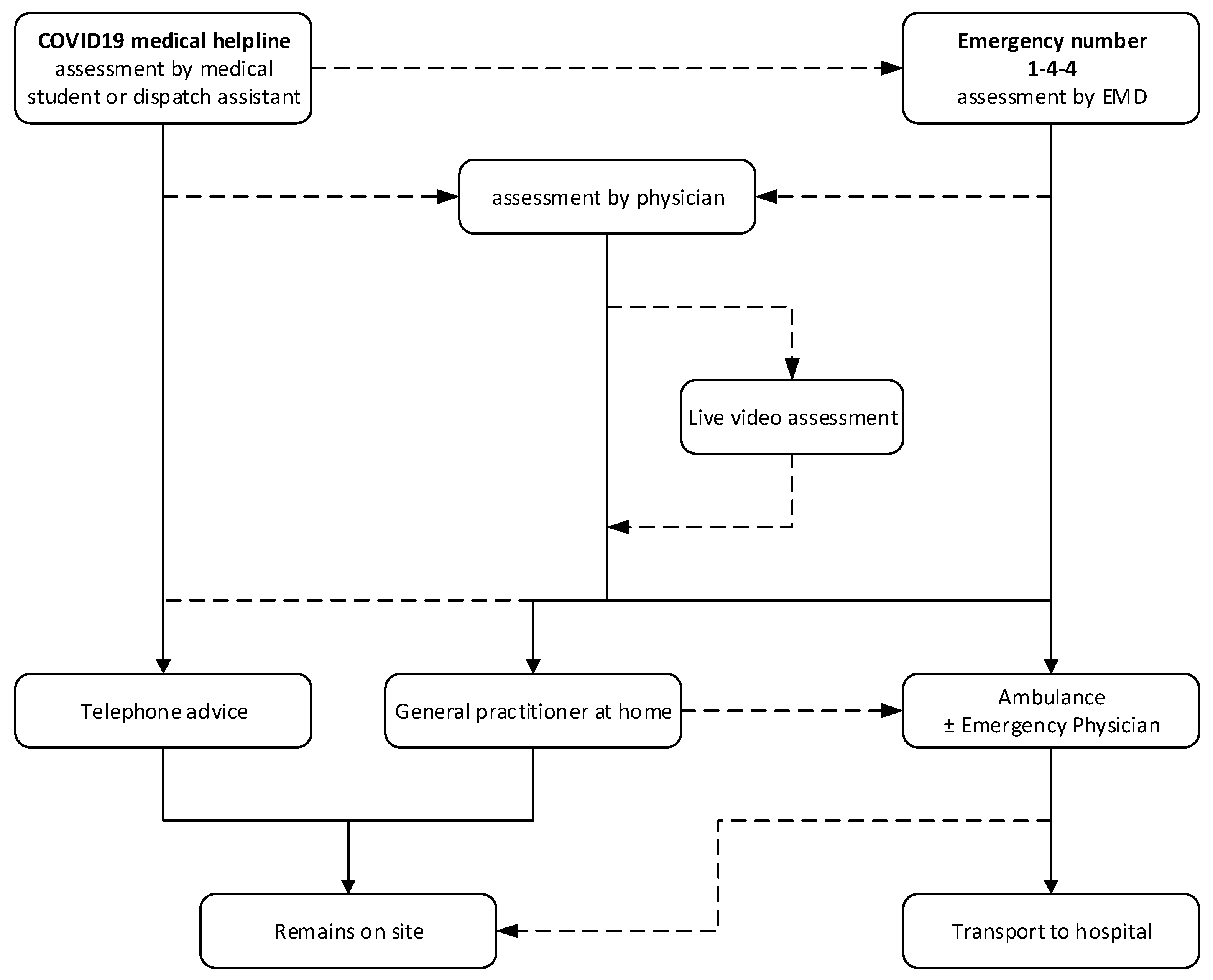
2.2. Geneva’s Typical EMCC and Emergency Medical System (EMS)
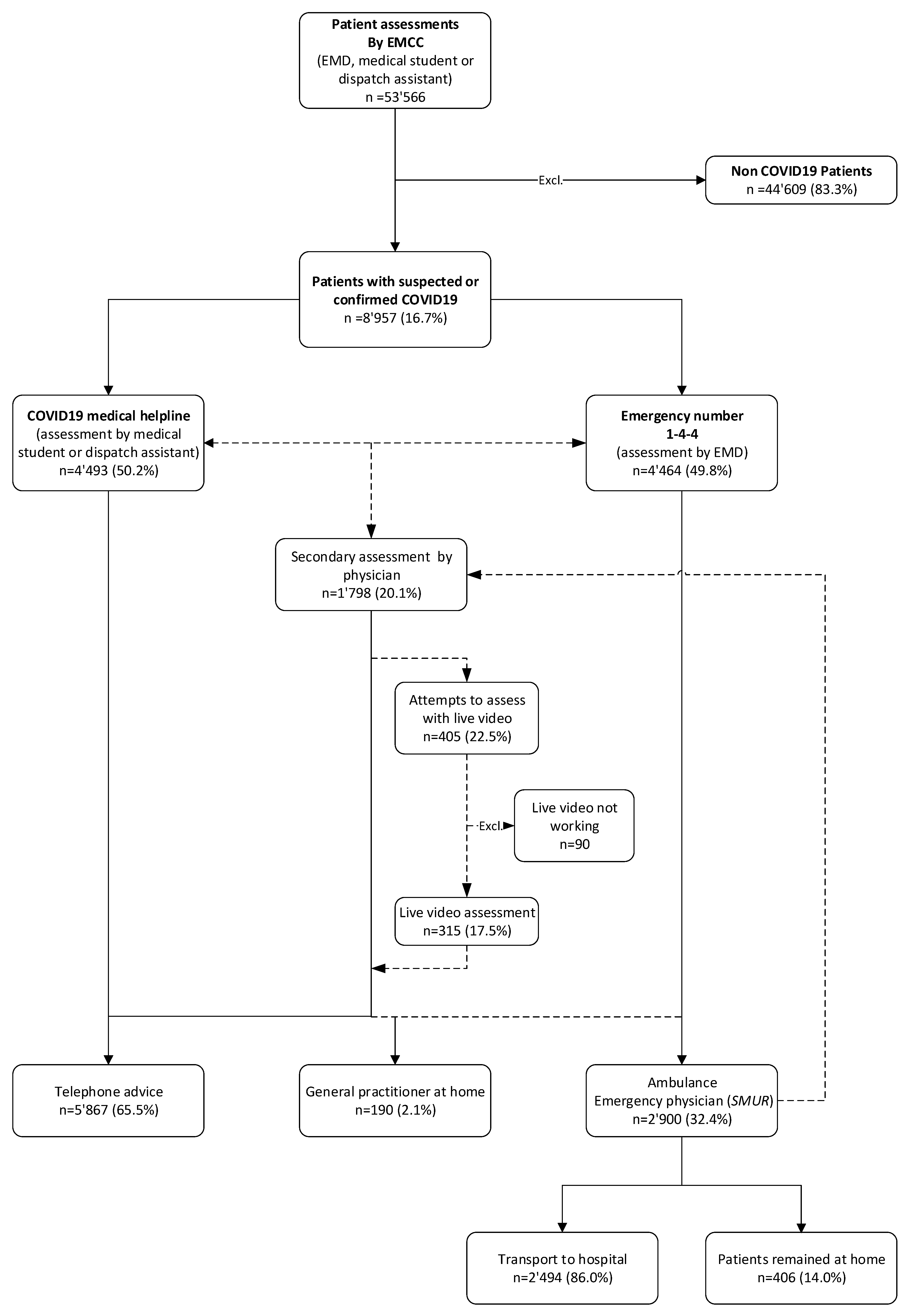
2.3. Re-Organization of Geneva’s EMCC during the COVID-19 Pandemic
2.4. Live Video Facilities
2.5. Web-Based Survey
2.6. Study Design
2.6.1. Data
2.6.2. Inclusion and Exclusion Criteria
2.6.3. Outcomes
2.6.4. Measures
2.6.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kristal, R.; Rowell, M.; Kress, M.; Keeley, C.; Jackson, H.; Piwnica-Worms, K.; Hendricks, L.; Long, T.G.; Wallach, A.B. A Phone Call Away: New York’s Hotline And Public Health In The Rapidly Changing COVID-19 Pandemic. Health Aff. (Proj. Hope) 2020, 39, 1431–1436. [Google Scholar] [CrossRef]
- Marrazzo, F.; Spina, S.; Pepe, P.E.; D’Ambrosio, A.; Bernasconi, F.; Manzoni, P.; Graci, C.; Frigerio, C.; Sacchi, M.; Stucchi, R.; et al. Rapid reorganization of the Milan metropolitan public safety answering point operations during the initial phase of the COVID-19 outbreak in Italy. J. Am. Coll. Emerg. Physicians Open 2020, 1, 1240–1249. [Google Scholar] [CrossRef]
- Saberian, P.; Conovaloff, J.L.; Vahidi, E.; Hasani-Sharamin, P.; Kolivand, P.H. How the COVID-19 Epidemic Affected Prehospital Emergency Medical Services in Tehran, Iran. West. J. Emerg. Med. 2020, 21, 110–116. [Google Scholar] [CrossRef]
- Prezant, D.J.; Lancet, E.A.; Zeig-Owens, R.; Lai, P.H.; Appel, D.; Webber, M.P.; Braun, J.; Hall, C.B.; Asaeda, G.; Kaufman, B.; et al. System impacts of the COVID-19 pandemic on New York City’s emergency medical services. J. Am. Coll. Emerg. Physicians Open 2020, 1, 1205–1213. [Google Scholar] [CrossRef]
- Lapostolle, F.; Schneider, E.; Vianu, I.; Dollet, G.; Roche, B.; Berdah, J.; Michel, J.; Goix, L.; Chanzy, E.; Petrovic, T.; et al. Clinical features of 1487 COVID-19 patients with outpatient management in the Greater Paris: The COVID-call study. Intern. Emerg. Med. 2020, 15, 813–817. [Google Scholar] [CrossRef] [PubMed]
- Dami, F.; Berthoz, V. Lausanne medical dispatch centre’s response to COVID-19. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 37. [Google Scholar] [CrossRef]
- Hautz, W.E.; Exadaktylos, A.; Sauter, T.C. Online forward triage during the COVID-19 outbreak. Emerg. Med. J. EMJ 2021, 38, 106–108. [Google Scholar] [CrossRef]
- Galmiche, S.; Rahbe, E.; Fontanet, A.; Dinh, A.; Bénézit, F.; Lescure, F.X.; Denis, F. Implementation of a Self-Triage Web Application for Suspected COVID-19 and Its Impact on Emergency Call Centers: Observational Study. J. Med. Internet Res. 2020, 22, e22924. [Google Scholar] [CrossRef]
- Vuilleumier, S.; Spichiger, T.; Dénéréaz, S.; Fiorentino, A. Not only COVID-19 disease impacts ambulance emergency demands but also lockdowns and quarantines. BMC Emerg. Med. 2023, 23, 4. [Google Scholar] [CrossRef]
- Jaffe, E.; Sonkin, R. The Role of Israel’s Emergency Medical Services during a Pandemic in the Pre-Exposure Period. Disaster Med. Public Health Prep. 2022, 16, 477–481. [Google Scholar] [CrossRef]
- Jaffe, E.; Sonkin, R.; Alpert, E.A.; Magid, A.; Knobler, H.Y. Flattening the COVID-19 Curve: The Unique Role of Emergency Medical Services in Containing a Global Pandemic. Isr. Med. Assoc. J. IMAJ 2020, 22, 476–482. [Google Scholar]
- Johansson, A.; Esbjörnsson, M.; Nordqvist, P.; Wiinberg, S.; Andersson, R.; Ivarsson, B.; Möller, S. Technical feasibility and ambulance nurses’ view of a digital telemedicine system in pre-hospital stroke care—A pilot study. Int. Emerg. Nurs. 2019, 44, 35–40. [Google Scholar] [CrossRef]
- Ter Avest, E.; Lambert, E.; de Coverly, R.; Tucker, H.; Griggs, J.; Wilson, M.H.; Ghorbangholi, A.; Williams, J.; Lyon, R.M. Live video footage from scene to aid helicopter emergency medical service dispatch: A feasibility study. Scand. J. Trauma Resusc. Emerg. Med. 2019, 27, 55. [Google Scholar] [CrossRef]
- Felzen, M.; Beckers, S.K.; Kork, F.; Hirsch, F.; Bergrath, S.; Sommer, A.; Brokmann, J.C.; Czaplik, M.; Rossaint, R. Utilization, Safety, and Technical Performance of a Telemedicine System for Prehospital Emergency Care: Observational Study. J. Med. Internet Res. 2019, 21, e14907. [Google Scholar] [CrossRef]
- Vicente, V.; Johansson, A.; Ivarsson, B.; Todorova, L.; Möller, S. The Experience of Using Video Support in Ambulance Care: An Interview Study with Physicians in the Role of Regional Medical Support. Healthcare 2020, 8, 106. [Google Scholar] [CrossRef]
- Linderoth, G.; Lippert, F.; Østergaard, D.; Ersbøll, A.K.; Meyhoff, C.S.; Folke, F.; Christensen, H.C. Live video from bystanders’ smartphones to medical dispatchers in real emergencies. Resuscitation 2021, 21, 101. [Google Scholar] [CrossRef]
- Linderoth, G.; Rosenkrantz, O.; Lippert, F.; Østergaard, D.; Ersbøll, A.K.; Meyhoff, C.S.; Folke, F.; Christensen, H.C. Live video from bystanders’ smartphones to improve cardiopulmonary resuscitation. Resuscitation 2021, 168, 35–43. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Wherton, J.; Shaw, S.; Morrison, C. Video consultations for COVID-19. BMJ 2020, 368, m998. [Google Scholar] [CrossRef]
- Monaghesh, E.; Hajizadeh, A. The role of telehealth during COVID-19 outbreak: A systematic review based on current evidence. BMC Public Health 2020, 20, 1193. [Google Scholar] [CrossRef]
- Ponnapalli, A.; Khare, Y.; Dominic, C.; Ganesh, S.; Bhalla, G.; Gokani, S.A. Remote risk-stratification of dyspnoea in acute respiratory disorders: A systematic review of the literature. J. R. Coll. Physicians Edinb. 2021, 51, 221–229. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- OCSTAT. Etat et Évolution de la Population. Available online: https://statistique.ge.ch/domaines/apercu.asp?dom=01_01 (accessed on 1 January 2023).
- Larribau, R.; Chappuis, V.N.; Cottet, P.; Regard, S.; Deham, H.; Guiche, F.; Sarasin, F.P.; Niquille, M. Symptom-Based Dispatching in an Emergency Medical Communication Centre: Sensitivity, Specificity, and the Area under the ROC Curve. Int. J. Environ. Res. Public Health 2020, 17, 8254. [Google Scholar] [CrossRef]
- Genecand, C.; Mongin, D.; Koegler, F.; Lebowitz, D.; Regard, S.; Falcone, J.L.; Nehme, M.; Braillard, O.; Grira, M.; Joubert, D.; et al. Cohort profile: Actionable Register of Geneva Outpatients and inpatients with SARS-CoV-2 (ARGOS). BMJ Open 2021, 11, e048946. [Google Scholar] [CrossRef]
- Midez, R.; Fehlmann, C.A.; Marti, C.; Larribau, R.; Rouyer, F.; Boroli, F.; Suppan, L.; Gartner, B.A. Association between Prehospital Hypoxemia and Admission to Intensive Care Unit during the COVID-19 Pandemic: A Retrospective Cohort Study. Medicina 2021, 57, 1362. [Google Scholar] [CrossRef]
- Bell, F.; Pilbery, R.; Connell, R.; Fletcher, D.; Leatherland, T.; Cottrell, L.; Webster, P. The acceptability and safety of video triage for ambulance service patients and clinicians during the COVID-19 pandemic. Br. Paramed. J. 2021, 6, 49–58. [Google Scholar] [CrossRef]
- Sykora, R.; Renza, M.; Ruzicka, J.; Bakurova, P.; Kukacka, M.; Smetana, J.; Duska, F. Audiovisual Consults by Paramedics to Reduce Hospital Transport After Low-Urgency Calls: Randomized Controlled Trial. Prehosp. Disaster Med. 2020, 35, 656–662. [Google Scholar] [CrossRef]
- Breeman, W.; Poublon, N.A.; Verhofstad, M.H.J.; Van Lieshout, E.M.M. Safety of on-scene medical care by EMS nurses in non-transported patients: A prospective, observational study. Scand. J. Trauma Resusc. Emerg. Med. 2018, 26, 79. [Google Scholar] [CrossRef]
- Sýkora, R.; Peřan, D.; Renza, M.; Bradna, J.; Smetana, J.; Duška, F. Video Emergency Calls in Medical Dispatching: A Scoping Review. Prehospital Disaster Med. 2022, 37, 819–826. [Google Scholar] [CrossRef]
- Jaffe, E.; Sonkin, R.; Strugo, R.; Zerath, E. Evolution of emergency medical calls during a pandemic—An emergency medical service during the COVID-19 outbreak. Am. J. Emerg. Med. 2020, 43, 260–266. [Google Scholar] [CrossRef]
- Gattu, R.; Scollan, J.; DeSouza, A.; Devereaux, D.; Weaver, H.; Agthe, A.G. Telemedicine: A Reliable Tool to Assess the Severity of Respiratory Distress in Children. Hosp. Pediatr. 2016, 6, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Siew, L.; Hsiao, A.; McCarthy, P.; Agarwal, A.; Lee, E.; Chen, L. Reliability of Telemedicine in the Assessment of Seriously Ill Children. Pediatrics 2016, 137, e20150712. [Google Scholar] [CrossRef] [PubMed]
- Boggan, J.C.; Shoup, J.P.; Whited, J.D.; Van Voorhees, E.; Gordon, A.M.; Rushton, S.; Lewinski, A.A.; Tabriz, A.A.; Adam, S.; Fulton, J.; et al. Effectiveness of Acute Care Remote Triage Systems: A Systematic Review. J. Gen. Intern. Med. 2020, 35, 2136–2145. [Google Scholar] [CrossRef]
- Hollander, J.E.; Carr, B.G. Virtually Perfect? Telemedicine for COVID-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef] [PubMed]
- Savioli, G.; Ceresa, I.F.; Gri, N.; Bavestrello Piccini, G.; Longhitano, Y.; Zanza, C.; Piccioni, A.; Esposito, C.; Ricevuti, G.; Bressan, M.A. Emergency Department Overcrowding: Understanding the Factors to Find Corresponding Solutions. J. Pers. Med. 2022, 12, 279. [Google Scholar] [CrossRef]
- Deana, C.; Rovida, S.; Orso, D.; Bove, T.; Bassi, F.; De Monte, A.; Vetrugno, L. Learning from the Italian experience during COVID-19 pandemic waves: Be prepared and mind some crucial aspects. Acta Biomed. 2021, 92, e2021097. [Google Scholar] [CrossRef]
| Total | Number | COVID-19 Medical Helpline | p Value | |
|---|---|---|---|---|
| Assessment | 1.4.4. | |||
| Patient assessments (n) | 8957 | 4493 | 4464 | |
| Patient’s sex | ||||
| Male, n (% *) | 3800 (42.4) | 2187 (48.7) | 1613 (36.1) | <0.001 |
| Female, n (% *) | 4486 (50.1) | 2201 (49.0) | 2285 (51.2) | |
| Patient’s age (years, mean ± SD) | 49.1 [±21.9] | 57.6 [±22.7] | 39.8 [±16.6] | <0.001 |
| Level of medical dispatch priority, n (% *) | ||||
| Level 1-A (immediate life-threatening emergency, requiring an EP) | 305 (3.4) | 302 (6.7) | 3 (0.1) | <0.001 |
| Level 1-B (life-threatening emergency) | 1030 (11.5) | 1018 (22.7) | 12 (0.3) | <0.001 |
| Level 2 (potential emergency) | 1181 (13.2) | 1158 (25.8) | 23 (0.5) | <0.001 |
| Level 3 (non-urgent situation, but requiring an ambulance in general) | 951 (10.6) | 848 (18.9) | 103 (2.3) | <0.001 |
| Level 4 (non-urgent situation) | 5388 (60.2) | 1100 (24.5) | 4288 (96.1) | <0.001 |
| Unknown | 102 (1.1) | 67 (1.5) | 35 (0.8) | |
| Main symptom at time of emergency call, n (% *) | ||||
| COVID-19 symptoms (rhinorrhoea, throat pain, dry cough, anosmia, agueusia) | 4824 (53.9) | 779 (17,3) | 4045 (90.6) | <0.001 |
| Dyspnoea | 2225 (24.8) | 2157 (48.0) | 68 (1.5) | <0.001 |
| Fever | 810 (9.0) | 561 (12.5) | 249 (5.6) | <0.001 |
| Nausea, vomiting, abdominal pain | 129 (1.4) | 128 (2.9) | 1 (0.0) | <0.001 |
| Other symptoms | 969 (10.8) | 868 (19.3) | 101 (2.3) | <0.001 |
| Medical dispatch decision, n (% *) | ||||
| Ambulance ± SMUR | 2900 (32.4) | 2859 (63.6) | 41 (0.9) | <0.001 |
| General Practitioner at home | 190 (2.1) | 186 (4.1) | 4 (0.1) | <0.001 |
| Telephone Advice | 5867 (65.5) | 1448 (32.2) | 4419 (99.0) | <0.001 |
| NACA ** scale in the field, transmitted by paramedics, n (% *) | ||||
| >4 (Injuries/diseases with acute threat of life) | 86 (1.0) | 86 (1.9) | 0 (0.0) | <0.001 |
| 4 (injuries/diseases which can possibly lead to deterioration of vital signs) | 654 (7.3) | 649 (14.4) | 5 (0.1) | <0.001 |
| 3 (injuries/diseases without threat of life but requiring hospital admission) | 1447 (16.2) | 1432 (31.9) | 15 (0.3) | <0.001 |
| <3 (injuries/diseases requiring examination in ambulatory or no examination) | 661 (7.4) | 645 (14.4) | 16 (0.4) | <0.001 |
| Not transmitted (no ambulance) | 6109 (68.2) | 1681 (37.4) | 4428 (99.2) | <0.001 |
| Ambulance dispatched | 2900 | 2859 | 41 | |
| Ambulance sent but leaves patient on site (no transport), n (% *) | 406 (14.0) | 391 (13.7) | 15 (36.7) |
| Failed Call Attempts with Live Video | |
|---|---|
| 90 | |
| Reasons for failure of live video related to patients or callers, n (% *) | 48 (53.3) |
| URL link not selected in the SMS | 33 (36.7) |
| Denial of access to the smartphone camera | 10 (11.1) |
| Patient/caller uncomfortable (embarrassed) to be seen on video | 5 (5.6) |
| Reasons for the failure of live video due to technical problems, n (% *) | 28 (31.1) |
| No camera detected on the phone | 12 (13.3) |
| Poor internet connection (Wi-Fi or 4G) | 8 (8.9) |
| SMS message not received on the smartphone | 5 (5.6) |
| Telephone number error | 2 (2.2) |
| IPhone® incompatible | 1 (1.1) |
| Reasons for the failure of live video not determined, n (% *) | 14 (15.6) |
| URL: uniform resource locator | |
| SMS: short message system |
| Calls with Live Video | |
|---|---|
| 107 | |
| Patient/caller acceptance of live video, n (% *) | |
| Poor acceptance | 5 (4.7) |
| Acceptable or good acceptance | 7 (6.5) |
| Very good or excellent acceptance | 95 (88.8) |
| Ease of use by the physician, n (% *) | |
| Poor usability | 2 (1.9) |
| Acceptable or good usability | 6 (5.6) |
| Very good or excellent usability | 99 (92.5) |
| Patient’s sex | |
| Male, n (% *) | 41 (38.3) |
| Female, n (% *) | 63 (58.9) |
| Video call context, n (% *) | |
| Patient alone at home | 28 (26.2) |
| Patient not alone at home (presence of a close relative) | 63 (58.9) |
| Paramedics on site | 16 (15.0) |
| Indication for the use of live video, n (% *) | |
| Assessment of breathing | 87 (81.3) |
| Assessment of the patient’s general condition | 84 (78.5) |
| Assessment of patient’s vital signs (other than breathing rate) | 17 (15.9) |
| Other reasons (communication difficulties, difficult psycho-social context) | 14 (13.1) |
| Single indication | 37 (34.6) |
| Multiple indications | 70 (65.4) |
| Calls with Live Video | |
|---|---|
| Paramedics not on site, n (% *): | 91 |
| Urgent ambulance dispatched (Dispatch Priority Level 1) | 7 (7.7) |
| Non-urgent ambulance dispatched (Dispatch Priority Level 2 or 3) | 8 (8.8) |
| General Practitioner home visit organised | 5 (5.5) |
| Follow-up required (patient to organise) | 13 (14.3) |
| Patient remained at home with advice, no current indication for follow-up | 57 (62.6) |
| Not documented | 1 (1.1) |
| Paramedics on site, n (% *): | 16 |
| Re-orientated ambulance to a specific, specialist site | 10 (62.5) |
| Patient remained at home with advice | 6 (37.5) |
| Physician’s evaluation of the live video call contribution to the outcome of the decision, n (% *) | 107 |
| Contribution to outcome of the medical decision | 81 (75.7) |
| No Contribution to outcome of the medical decision | 1 (0.93) |
| Insufficient quality of video | 17 (15.89) |
| Not documented | 8 (7.48) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Larribau, R.; Healey, B.; Chappuis, V.N.; Boussard, D.; Guiche, F.; Herren, T.; Gartner, B.A.; Suppan, L. Contribution of Live Video to Physicians’ Remote Assessment of Suspected COVID-19 Patients in an Emergency Medical Communication Centre: A Retrospective Study and Web-Based Survey. Int. J. Environ. Res. Public Health 2023, 20, 3307. https://doi.org/10.3390/ijerph20043307
Larribau R, Healey B, Chappuis VN, Boussard D, Guiche F, Herren T, Gartner BA, Suppan L. Contribution of Live Video to Physicians’ Remote Assessment of Suspected COVID-19 Patients in an Emergency Medical Communication Centre: A Retrospective Study and Web-Based Survey. International Journal of Environmental Research and Public Health. 2023; 20(4):3307. https://doi.org/10.3390/ijerph20043307
Chicago/Turabian StyleLarribau, Robert, Beth Healey, Victor Nathan Chappuis, Dominique Boussard, Florent Guiche, Tara Herren, Birgit Andrea Gartner, and Laurent Suppan. 2023. "Contribution of Live Video to Physicians’ Remote Assessment of Suspected COVID-19 Patients in an Emergency Medical Communication Centre: A Retrospective Study and Web-Based Survey" International Journal of Environmental Research and Public Health 20, no. 4: 3307. https://doi.org/10.3390/ijerph20043307
APA StyleLarribau, R., Healey, B., Chappuis, V. N., Boussard, D., Guiche, F., Herren, T., Gartner, B. A., & Suppan, L. (2023). Contribution of Live Video to Physicians’ Remote Assessment of Suspected COVID-19 Patients in an Emergency Medical Communication Centre: A Retrospective Study and Web-Based Survey. International Journal of Environmental Research and Public Health, 20(4), 3307. https://doi.org/10.3390/ijerph20043307









