The Influence of the COVID-19 Pandemic on Emergency Medical Services to Out-of-Hospital Cardiac Arrests in a Low-Incidence Urban City: An Observational Epidemiological Analysis
Abstract
:1. Introduction
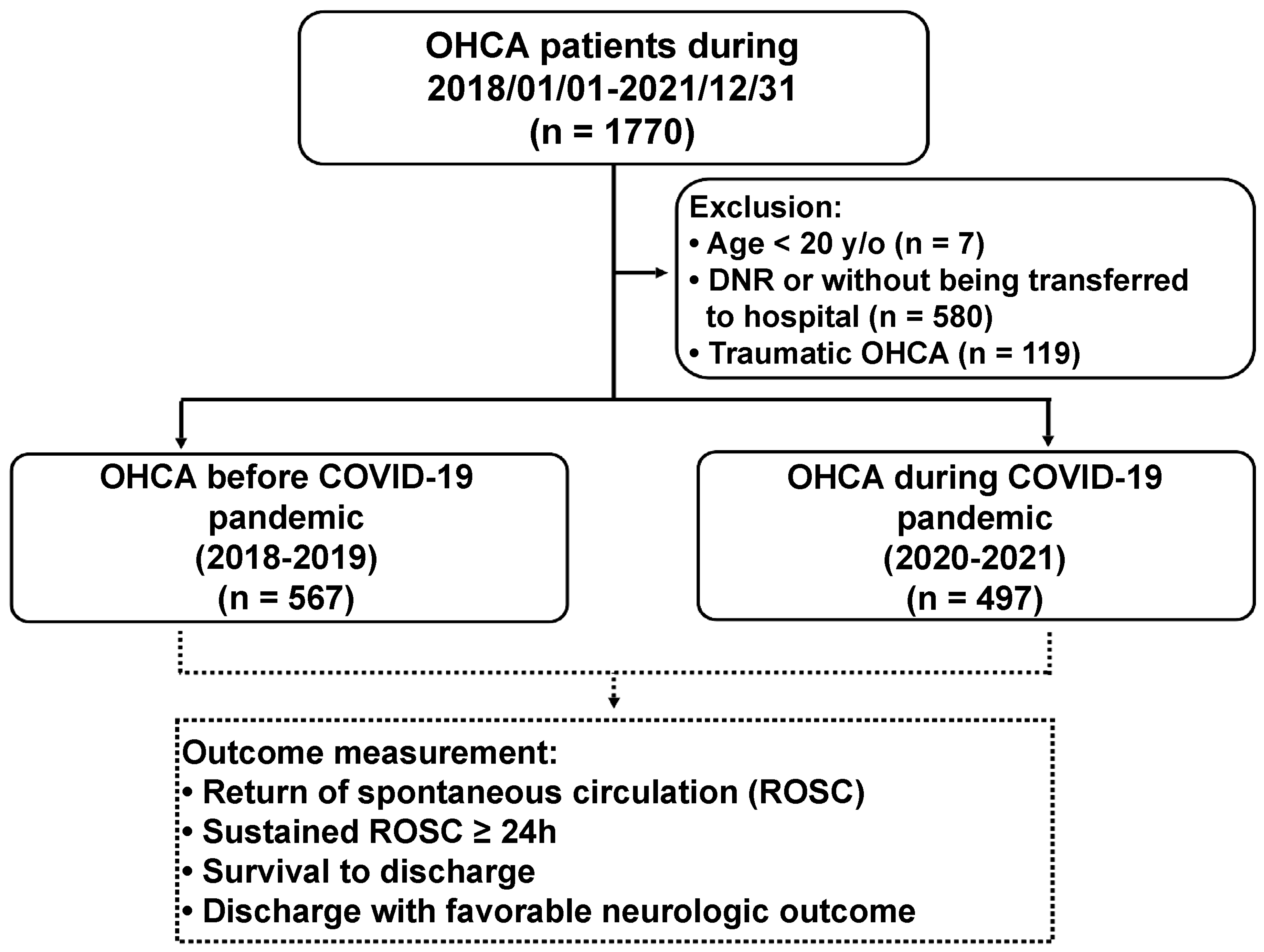
2. Materials and Methods
2.1. Background and Settings of Study
2.2. Healthcare Facilities, Pre-Hospital Rescue and OHCA Registry of the City
2.3. Adjustment of EMS Protocol during the COVID-19 Pandemic
2.4. Data Collection and Outcome Measurement
2.5. Statistical Methods
3. Results
3.1. Demographics and Characteristics of OHCA Patients
3.2. Influence of COVID-19 on the Primary Outcomes
3.3. Influence of COVID-19 on the Secondary Outcomes
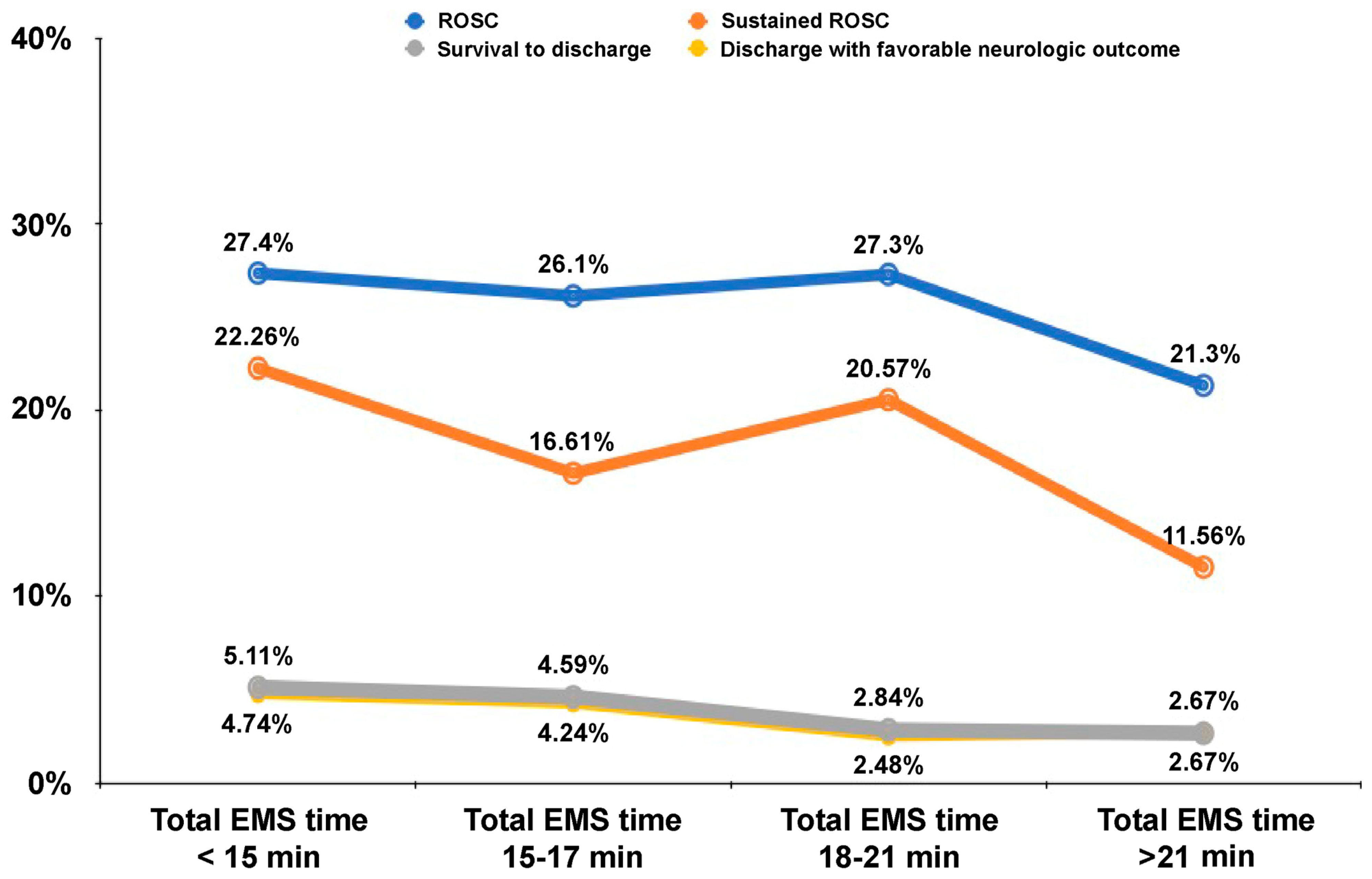
3.4. Influence of the EMS Time on the Primary and Secondary Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Myat, A.; Song, K.J.; Rea, T. Out-of-hospital cardiac arrest: Current concepts. Lancet 2018, 391, 970–979. [Google Scholar] [CrossRef] [PubMed]
- Merchant, R.M.; Topjian, A.A.; Panchal, A.R.; Cheng, A.; Aziz, K.; Berg, K.M. Part 1: Executive summary: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2020, 142 (Suppl. 2), S337–S357. [Google Scholar] [CrossRef] [PubMed]
- Howard, I.; Cameron, P.; Wallis, L.; Castren, M.; Lindstrom, V. Quality Indicators for Evaluating Prehospital Emergency Care: A Scoping Review. Prehosp. Disaster Med. 2018, 33, 43–52. [Google Scholar] [CrossRef]
- Amiry, A.A.I.; Maguire, B.J. Emergency Medical Services (EMS) Calls During COVID-19: Early Lessons Learned for Systems Planning (A Narrative Review). Open Access Emerg. Med. 2021, 13, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Scquizzato, T.; D’Amico, F.; Rocchi, M.; Saracino, M.; Stella, F.; Landoni, G.; Zangrillo, A. Impact of COVID-19 pandemic on out-of-hospital cardiac arrest system-of-care: A systematic review and meta-analysis. Prehosp. Emerg. Care 2022, 26, 30–41. [Google Scholar] [CrossRef] [PubMed]
- Lim, Z.J.; Reddy, M.P.; Afroz, A.; Billah, B.; Shekar, K.; Subramaniam, A. Incidence and outcome of out-of-hospital cardiac arrests in the COVID-19 era: A systematic review and meta-analysis. Resuscitation 2020, 157, 248–258. [Google Scholar] [CrossRef]
- Bielski, K.; Szarpak, A.; Jaguszewski, M.J.; Kopiec, T.; Smereka, J.; Gasecka, A.; Wolak, P.; Nowak-Starz, G.; Chmielewski, J.; Rafique, Z.; et al. The Influence of COVID-19 on Out-Hospital Cardiac Arrest Survival Outcomes: An Updated Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 5573. [Google Scholar] [CrossRef]
- Teoh, S.E.; Masuda, Y.; Tan, D.J.H.; Liu, N.; Morrison, L.J.; Ong, M.E.H.; Blewer, A.L.; Ho, A.F.W. Impact of the COVID-19 pandemic on the epidemiology of out-of-hospital cardiac arrest: A systematic review and meta-analysis. Ann. Intensive Care 2021, 11, 169. [Google Scholar] [CrossRef]
- Yu, J.H.; Liu, C.Y.; Chen, W.K.; Yu, S.H.; Huang, F.W.; Yang, M.T.; Shih, H.M. Impact of the COVID-19 pandemic on emergency medical service response to out-of-hospital cardiac arrests in Taiwan: A retrospective observational study. Emerg. Med. J. 2021, 38, 679–684. [Google Scholar] [CrossRef]
- Ortiz, F.R.; Del Valle, P.F.; Knox, E.C.; Fábrega, X.J.; Pascual, J.M.N.; Rodríguez, I.M.; Teja-Ruiz, B.; Ruiz-Azpiazu, J.I.; Iglesias-Vázquez, J.A.; Echarri-Sucunza, A.; et al. Influence of the COVID-19 pandemic on out-of-hospital cardiac arrest. A Spanish nationwide prospective cohort study. Resuscitation 2020, 157, 230–240. [Google Scholar] [CrossRef]
- Chan, P.S.; Girotra, S.; Tang, Y.; Al-Araji, R.; Nallamothu, B.K.; McNally, B. Outcomes for out-of-hospital cardiac arrest in the United States during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2021, 6, 296–303. [Google Scholar] [CrossRef]
- Talikowska, M.; Ball, S.; Tohira, H.; Bailey, P.; Rose, D.; Brink, D.; Bray, J.; Finn, J. No apparent effect of the COVID-19 pandemic on out-of-hospital cardiac arrest incidence and outcome in Western Australia. Resusc. Plus 2021, 8, 100183. [Google Scholar] [CrossRef] [PubMed]
- Nishiyama, C.; Kiyohara, K.; Iwami, T.; Hayashida, S.; Kiguchi, T.; Matsuyama, T.; Katayama, Y.; Shimazu, T.; Kitamura, T. Influence of COVID-19 pandemic on bystander interventions, emergency medical service activities, and patient outcomes in out-of-hospital cardiac arrest in Osaka City, Japan. Resusc. Plus 2021, 5, 100088. [Google Scholar] [CrossRef] [PubMed]
- Summers, J.; Cheng, H.Y.; Lin, H.H.; Barnard, L.T.; Kvalsvig, A.; Wilson, N.; Baker, M.G. Potential lessons from the Taiwan and New Zealand health responses to the COVID-19 pandemic. Lancet Reg. Health-West. Pac. 2020, 4, 100044. [Google Scholar] [CrossRef] [PubMed]
- Taiwan Center of Disease Control Statistics. Available online: https://nidss.cdc.gov.tw/nndss/Cdcwnh07?id=19CoV (accessed on 12 October 2022).
- Chiayi City Household Registration Service. Available online: https://household.chiayi.gov.tw/popul05/index.aspx?Parser=99,7,43 (accessed on 20 September 2022).
- Recommendations for Pre-Hospital Respiratory Treatment during the COVID-19 Pandemic. Taiwan Emerg. Med. Bull. 2020, 3, e2020030213. Available online: https://www.sem.org.tw/EJournal/Detail/200 (accessed on 20 September 2022).
- Hagihara, A.; Onozuka, D.; Ono, J.; Nagata, T.; Hasegawa, M. Age Gender Interaction Effect on Resuscitation Outcomes in Patients with Out-of-Hospital Cardiac Arrest. Am. J. Cardiol. 2017, 120, 387–392. [Google Scholar] [CrossRef]
- Andersen, L.W.; Bivens, M.J.; Giberson, T.; Giberson, B.; Mottley, J.L.; Gautam, S.; Salciccioli, J.D.; Cocchi, M.N.; McNally, B.; Donnino, M.W. The relationship between age and outcome in out-of-hospital cardiac arrest patients. Resuscitation 2015, 94, 49–54. [Google Scholar] [CrossRef]
- Nichol, G.; Cobb, L.A.; Yin, L.; Maynard, C.; Olsufka, M.; Larsen, J.; McCoy, A.M.; Sayre, M.R. Briefer activation time is associated with better outcomes after out-of-hospital cardiac arrest. Resuscitation 2016, 107, 139–144. [Google Scholar] [CrossRef]
- Park, H.A.; Ahn, K.O.; Lee, E.J.; Park, J.O.; On Behalf of the Korean Cardiac Arrest Research Consortium (Ko CI). Association between survival and on-scene resuscitation time in refractory out-of-hospital cardiac arrest: A cross-sectional Retrospective Study. Int. J. Environ. Res. Public Health 2021, 18, 496. [Google Scholar] [CrossRef]
- Riva, G.; Jonsson, M.; Ringh, M.; Claesson, A.; Djärv, T.; Forsberg, S.; Nordberg, P.; Rubertsson, S.; Rawshani, A.; Nord, A.; et al. Survival after dispatcher-assisted cardiopulmonary resuscitation in out-of-hospital cardiac arrest. Resuscitation 2020, 157, 195–201. [Google Scholar] [CrossRef]
- Lee, Y.J.; Song, K.J.; Shin, S.D.; Lee, S.C.; Lee, E.J.; Ro, Y.S.; Ahn, K.O. Dispatcher-Assisted Cardiopulmonary Resuscitation Program and Outcomes after Pediatric Out-of-Hospital Cardiac Arrest. Pediatr. Emerg. Care 2019, 35, 561–567. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Hong, K.J.; Shin, S.D.; Ro, Y.S.; Song, K.J.; Park, J.H.; Kong, S.Y.; Kim, T.H.; Lee, S.C. The effect of dispatcher-assisted cardiopulmonary resuscitation on early defibrillation and return of spontaneous circulation with survival. Resuscitation 2019, 135, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Siman-Tov, M.; Strugo, R.; Podolsky, T.; Rosenblat, I.; Blushtein, O. Impact of dispatcher assisted CPR on ROSC rates: A National Cohort Study. Am. J. Emerg. Med. 2020, 44, 333–338. [Google Scholar] [CrossRef]
- Czapla, M.; Zielińska, M.; Kubica-Cielińska, A.; Diakowska, D.; Quinn, T.; Karniej, P. Factors associated with return of spontaneous circulation after out-of-hospital cardiac arrest in Poland: A one-year retrospective study. BMC Cardiovasc. Disord. 2020, 20, 288. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, Y.J.; Han, S.; Choi, H.J.; Moon, H.; Kim, G. Effect of Prehospital Epinephrine on Outcomes of Out-of-Hospital Cardiac Arrest: A Bayesian Network Approach. Emerg. Med. Int. 2020, 2020, 8057106. [Google Scholar] [CrossRef]
- Chen, Y.R.; Liao, C.J.; Huang, H.C.; Tsai, C.H.; Su, Y.S.; Liu, C.H.; Hsu, C.F.; Tsai, M.J. The Effect of Implementing Mechanical Cardiopulmonary Resuscitation Devices on Out-of-Hospital Cardiac Arrest Patients in an Urban City of Taiwan. Int. J. Environ. Res. Public Health 2021, 18, 3636. [Google Scholar] [CrossRef]
- Uy-Evanado, A.; Chugh, H.S.; Sargsyan, A.; Nakamura, K.; Mariani, R.; Hadduck, K.; Reinier, K. Out-of-hospital cardiac arrest response and outcomes during the COVID-19 pandemic. Clin. Electrophysiol. 2021, 7, 6–11. [Google Scholar] [CrossRef]
- Ball, J.; Nehme, Z.; Bernard, S.; Stub, D.; Stephenson, M.; Smith, K. Collateral damage: Hidden impact of the COVID-19 pandemic on the out-of-hospital cardiac arrest system-of-care. Resuscitation 2020, 156, 157–163. [Google Scholar] [CrossRef]
- Lee, D.W.; Moon, H.J.; Heo, N.H.; KoCARC. Association between ambulance response time and neurologic outcome in patients with cardiac arrest. Am. J. Emerg. Med. 2019, 37, 1999–2003. [Google Scholar] [CrossRef]
- Sato, N.; Matsuyama, T.; Akazawa, K.; Nakazawa, K.; Hirose, Y. Benefits of adding a physician-staffed ambulance to bystander-witnessed out-of-hospital cardiac arrest: A community-based, observational study in Niigata, Japan. BMJ Open 2019, 9, e032967. [Google Scholar] [CrossRef]
- Bujak, K.; Nadolny, K.; Trzeciak, P.; Gałązkowski, R.; Ładny, J.R.; Gąsior, M. Does the presence of physician-staffed emergency medical services improve the prognosis in out-of-hospital cardiac arrest? A propensity score matching analysis. Kardiol. Pol. 2022, 80, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Paoli, A.; Brischigliaro, L.; Scquizzato, T.; Favaretto, A.; Spagna, A. Out-of-hospital cardiac arrest during the COVID-19 pandemic in the Province of Padua, Northeast Italy. Resuscitation 2020, 154, 47. [Google Scholar] [CrossRef] [PubMed]
- Semeraro, F.; Gamberini, L.; Tartaglione, M.; Iarussi, B.; Descovich, C.; Picoco, C.; Gordini, G. Out-of-hospital cardiac arrest during the COVID-19 era in Bologna: System response to preserve performances. Resuscitation 2020, 157, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.H.; Su, H.Y.; Tsai, I.T. Impact of COVID-19 Pandemic on Emergency Department Volume and Acuity in Low Incidence Area: Taiwan’s Experience in Three Hospitals. J. Acute Med. 2022, 12, 105–112. [Google Scholar] [CrossRef]
- DeFilippis, E.M.; Ranard, L.S.; Berg, D.D. Cardiopulmonary resuscitation during the COVID-19 pandemic: A view from trainees on the front line. Circulation 2020, 141, 1833–1835. [Google Scholar] [CrossRef]
- Cheng, K.Y.; Tu, Y.C.; Lu, J.J.; Tsai, M.J.; Hsu, C.F. Simulation Based Ambulance and Crew Decontamination Advise During COVID-19 Pandemic. J. Acute Med. 2021, 11, 63–67. [Google Scholar] [CrossRef]
| Before COVID-19 Pandemic (n = 567) | During COVID-19 Pandemic (n = 497) | p Value | |
|---|---|---|---|
| Demographics | |||
| Age | 76.0 (64–85) | 78 (65–85) | 0.545 |
| Older adults (≥65 years) | 409.0 (72.65) | 367.0 (75.98) | 0.219 |
| Male gender | 313 (55.40) | 292 (59.00) | 0.239 |
| Time period of emergent call reception | |||
| Day (8 AM–4 PM) | 247 (43.56) | 220 (44.27) | 0.779 |
| Evening (4 PM–12 PM) | 168 (29.63) | 153 (30.78) | |
| Night (12 PM–8 AM) | 152 (26.81) | 124 (24.95) | |
| Time interval of the rescue | |||
| Reaction time (min) | 4 (3–5) | 5 (3–6) | <0.001 |
| On site time (min) | 9 (7–12) | 10 (8–13) | <0.001 |
| Traffic time (min) | 3 (2–4) | 3 (2–5) | <0.001 |
| Total rescue time (min) | 16 (14–20) | 19 (15–22) | <0.001 |
| EMS Dispatcher related | |||
| DACPR or BSCPR | 300 (53.19) | 299 (60.16) | 0.022 |
| OHCA verification time (s) | 55 (28–109) (n = 403) | 62 (29–115) (n = 392) | 0.247 |
| DACPR beginning time (s) | 172 (132–233) (n = 270) | 175(131–229) (n = 291) | 0.608 |
| Numbers of EMT (Median (IQR)) | 3 (3–3) | 3 (2–3) (n = 495) | <0.001 |
| EMTP dispatch | 133 (23.46) | 152 (30.58) | 0.009 |
| Characteristics of OHCA | |||
| Cardiac arrest witnessed | 292 (51.50) | 237 (47.69) | 0.215 |
| Shockable arrhythmia by AED | 102 (18.25) | 95 (19.55) | 0.592 |
| OHCA locations | |||
| Home | 427 (75.31) | 384 (77.73) | 0.012 |
| Public place | 42 (7.41) | 35 (7.09) | |
| Institution | 65 (11.46) | 44 (8.91) | |
| Others | 16 (2.82) | 27 (5.47) | |
| On the ambulance | 17 (3.00) | 4 (0.81) | |
| Prehospital treatment | |||
| Use of Public Access Defibrillation (PAD) | 12 (2.12) | 17 (3.42) | 0.192 |
| Number of PAD defibrillations | 0 (0–0) | 0 (0–0) | 0.191 |
| Laryngeal mask airway | 478 (84.30) | 358 (72.18) | <0.001 |
| Mechanical CPR device | 168 (29.63) | 387 (78.02) | <0.001 |
| Intravenous epinephrine | 16 (2.82) | 47 (9.46) | <0.001 |
| Level of transferred hospital | |||
| Primary | 80 (14.11) | 66 (13.66) | 0.588 |
| Secondary | 301 (53.09) | 244 (50.52) | |
| Tertiary | 186 (32.80) | 173 (35.82) | |
| Outcomes | |||
| Any ROSC | 135 (23.81) | 139 (27.97) | 0.122 |
| Continued ROSC (≥24 h) | 93 (16.40) | 99 (19.92) | 0.137 |
| Survival to discharge | 30 (5.29) | 11 (2.21) | 0.009 |
| Discharge with favorable neurologic outcome | 29 (5.11) | 9 (1.81) | 0.004 |
| Factors | OR (95% CI) | p Value | aOR (95% CI) | p Value |
|---|---|---|---|---|
| Age (per additional year) | 0.99 (0.98–0.99) | 0.002 | - | |
| Total rescue time (per minute) | 0.98 (0.96–1.00) | 0.112 | - | |
| Number of dispatched EMT (per person) | 0.81 (0.60–1.10) | 0.174 | - | |
| Dispatch of EMTP | 1.07 (0.78–1.45) | 0.680 | - | |
| BSCPR or DACPR | 0.80 (0.61–1.06) | 0.115 | - | |
| OHCA locations | ||||
| Home | reference | reference | ||
| Public place | 3.71 (2.30–5.97) | <0.001 | 3.59 (2.22–5.83) | <0.001 |
| Institution | 0.77 (0.46–1.29) | 0.320 | 0.81 (0.48–1.35) | 0.418 |
| Others | 2.47 (1.32–4.63) | 0.005 | 2.28 (1.20–4.33) | 0.011 |
| On the ambulance | 4.58 (1.90–11.03) | <0.001 | 4.09 (1.63–10.28) | 0.003 |
| Laryngeal mask airway | 0.96 (0.69–1.34) | 0.799 | - | |
| Mechanical CPR device | 1.10 (0.84–1.45) | 0.488 | - | |
| Intravenous epinephrine | 1.37 (0.79–2.37) | 0.264 | - | |
| COVID-19 pandemic | 1.24 (0.94–1.64) | 0.122 | 1.25 (0.94–1.67) | 0.129 |
| Factors | OR (95% CI) | p Value | aOR (95% CI) | p Value |
|---|---|---|---|---|
| Age (per additional year) | 0.99 (0.98–0.99) | 0.002 | - | |
| Total rescue time (per minute) | 0.96 (0.93–0.99) | 0.016 | - | |
| Number of dispatched EMT (per person) | 0.93 (0.66–1.03) | 0.663 | - | |
| Dispatch of EMTP | 1.02 (0.72–1.45) | 0.918 | - | |
| BSCPR or DACPR | 0.88 (0.64–1.21) | 0.436 | - | |
| OHCA locations | ||||
| Home | reference | reference | ||
| Public place | 4.40 (2.69–7.20) | <0.001 | 4.22 (2.55–6.97) | <0.001 |
| Institution | 1.01 (0.57–1.78) | 0.971 | 1.06 (0.60–1.87) | 0.843 |
| Others | 3.48 (1.82–6.66) | <0.001 | 3.51 (1.82–6.76) | <0.001 |
| On the ambulance | 4.40 (1.82–10.68) | 0.001 | 3.72 (1.43–9.71) | 0.007 |
| Laryngeal mask airway | 0.89 (0.62–1.30) | 0.560 | - | |
| Mechanical CPR device | 1.10 (0.80–1.51) | 0.549 | - | |
| Intravenous epinephrine | 0.96 (0.49–1.87) | 0.901 | - | |
| COVID-19 pandemic | 1.27 (0.93–1.73) | 0.137 | 1.32 (0.95–1.83) | 0.102 |
| Factors | OR (95% CI) | p Value | aOR (95% CI) | p Value |
|---|---|---|---|---|
| Age (per additional year) | 0.97 (0.96–0.99) | <0.001 | 0.98 (0.96–0.99) | 0.022 |
| Total rescue time (per minute) | 0.93 (0.87–0.99) | 0.034 | - | |
| Number of dispatched EMT (per person) | 1.81 (0.84–3.90) | 0.129 | - | |
| Dispatch of EMTP | 0.76 (0.36–1.62) | 0.477 | - | |
| BSCPR or DACPR | 0.98 (0.53–1.85) | 0.962 | - | |
| OHCA locations | ||||
| Home | reference | reference | ||
| Public place | 7.28 (3.51–15.14) | <0.001 | 5.67 (2.63–12.25) | <0.001 |
| Institution | 0.33 (0.04–2.49) | 0.283 | 0.35 (0.05–2.63) | 0.308 |
| Others | 1.75 (0.40–7.69) | 0.459 | 1.55 (0.34–7.05) | 0.574 |
| On the ambulance | 5.98 (1.64–21.79) | 0.007 | 3.48 (0.74–16.25) | 0.113 |
| Laryngeal mask airway | 0.73 (0.36–1.48) | 0.385 | - | |
| Mechanical CPR device | 0.71 (0.38–1.33) | 0.280 | - | |
| Intravenous epinephrine | 0.81 (0.19–3.43) | 0.773 | - | |
| COVID-19 pandemic | 0.41 (0.20–0.82) | 0.012 | 0.43 (0.21–0.89) | 0.002 |
| Factors | OR (95% CI) | p Value | aOR (95% CI) | p Value |
|---|---|---|---|---|
| Age (per additional year) | 0.97 (0.95–0.99) | <0.001 | 0.98 (0.96–0.99) | 0.018 |
| Total rescue time (per minute) | 0.93 (0.87–1.00) | 0.055 | - | |
| Number of dispatched EMT (per person) | 1.70 (0.78–3.74) | 0.184 | - | |
| Dispatch of EMTP | 0.84 (0.39–1.80) | 0.661 | - | |
| BSCPR or DACPR | 1.06 (0.55–2.05) | 0.855 | - | |
| OHCA locations | ||||
| Home | reference | reference | ||
| Public place | 8.03 (3.82–16.89) | <0.001 | 6.20 (2.83–13.59) | <0.001 |
| Institution | 0.37 (0.05–2.76) | 0.329 | 0.39 (0.05–2.02) | 0.356 |
| Others | 1.93 (0.44–8.54) | 0.386 | 1.73 (0.38–7.97) | 0.482 |
| On the ambulance | 4.16 (0.91–19.04) | 0.066 | 1.74 (0.22–13.91) | 0.599 |
| Laryngeal mask airway | 0.87 (0.41–1.87) | 0.721 | - | |
| Mechanical CPR device | 0.73 (0.38–1.41) | 0.349 | - | |
| Intravenous epinephrine | 0.88 (0.21–3.74) | 0.861 | - | |
| COVID-19 pandemic | 0.34 (0.16–0.73) | 0.006 | 0.35 (0.16–0.77) | 0.009 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, C.-H.; Tsai, M.-J.; Hsu, C.-F.; Tsai, C.-H.; Su, Y.-S.; Cai, D.-C. The Influence of the COVID-19 Pandemic on Emergency Medical Services to Out-of-Hospital Cardiac Arrests in a Low-Incidence Urban City: An Observational Epidemiological Analysis. Int. J. Environ. Res. Public Health 2023, 20, 2713. https://doi.org/10.3390/ijerph20032713
Liu C-H, Tsai M-J, Hsu C-F, Tsai C-H, Su Y-S, Cai D-C. The Influence of the COVID-19 Pandemic on Emergency Medical Services to Out-of-Hospital Cardiac Arrests in a Low-Incidence Urban City: An Observational Epidemiological Analysis. International Journal of Environmental Research and Public Health. 2023; 20(3):2713. https://doi.org/10.3390/ijerph20032713
Chicago/Turabian StyleLiu, Chung-Hsien, Ming-Jen Tsai, Chi-Feng Hsu, Cheng-Han Tsai, Yao-Sing Su, and Deng-Chuan Cai. 2023. "The Influence of the COVID-19 Pandemic on Emergency Medical Services to Out-of-Hospital Cardiac Arrests in a Low-Incidence Urban City: An Observational Epidemiological Analysis" International Journal of Environmental Research and Public Health 20, no. 3: 2713. https://doi.org/10.3390/ijerph20032713
APA StyleLiu, C.-H., Tsai, M.-J., Hsu, C.-F., Tsai, C.-H., Su, Y.-S., & Cai, D.-C. (2023). The Influence of the COVID-19 Pandemic on Emergency Medical Services to Out-of-Hospital Cardiac Arrests in a Low-Incidence Urban City: An Observational Epidemiological Analysis. International Journal of Environmental Research and Public Health, 20(3), 2713. https://doi.org/10.3390/ijerph20032713








