The Time Course of Cardiorespiratory Adaptations to Rowing Indoor Training in Post-Menopausal Women
Abstract
1. Introduction
2. Materials and Methods
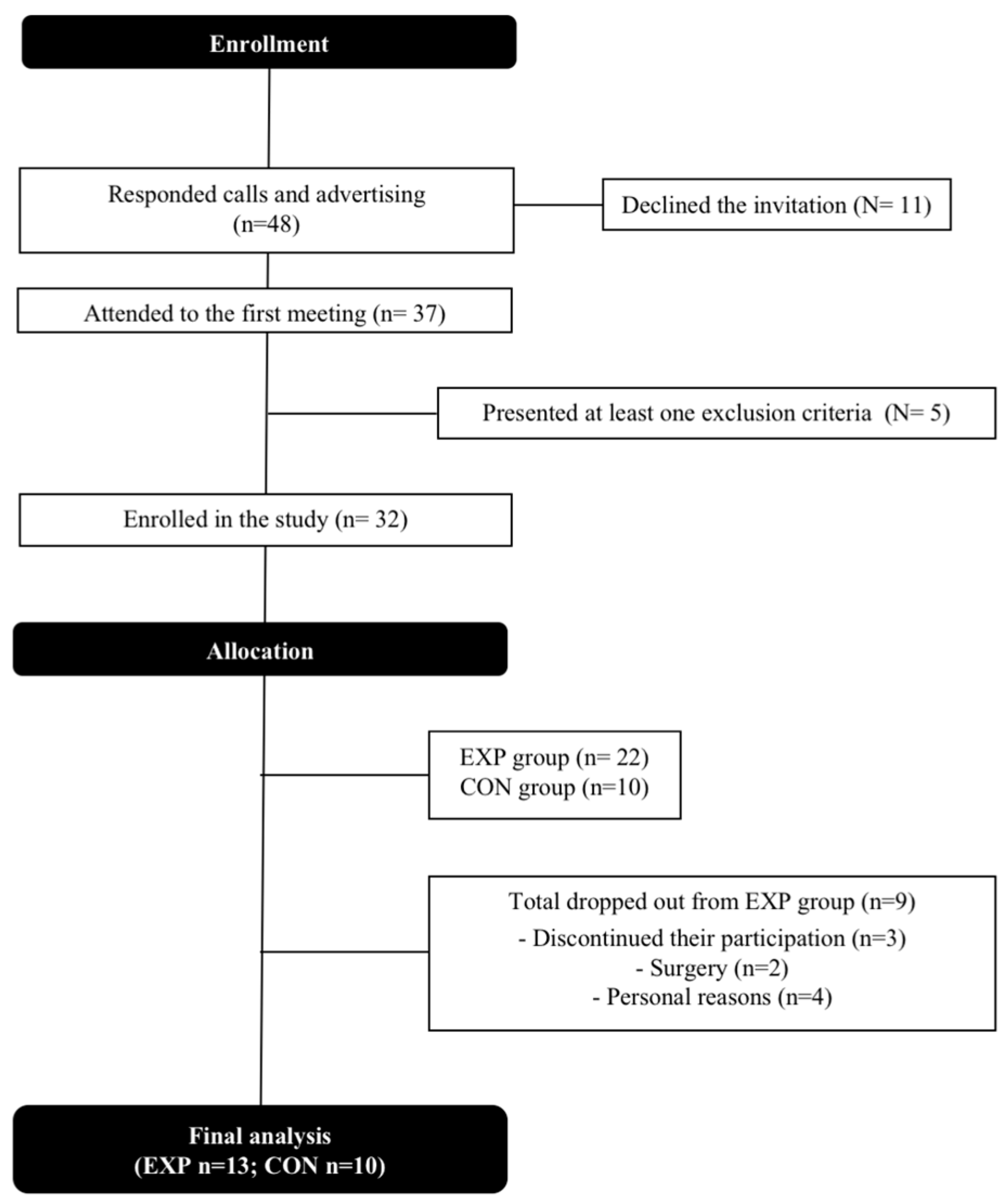
2.1. Sample
2.2. Experimental Protocol
2.3. Cardiopulmonary Exercise Test (CET)
2.4. Rowing Stepwise Exercise
2.5. Rowing Exercise Training Protocol
2.6. Statistical Analysis
3. Results
3.1. Sample
3.2. Maximal Cardiorespiratory Fitness following Rowing Training
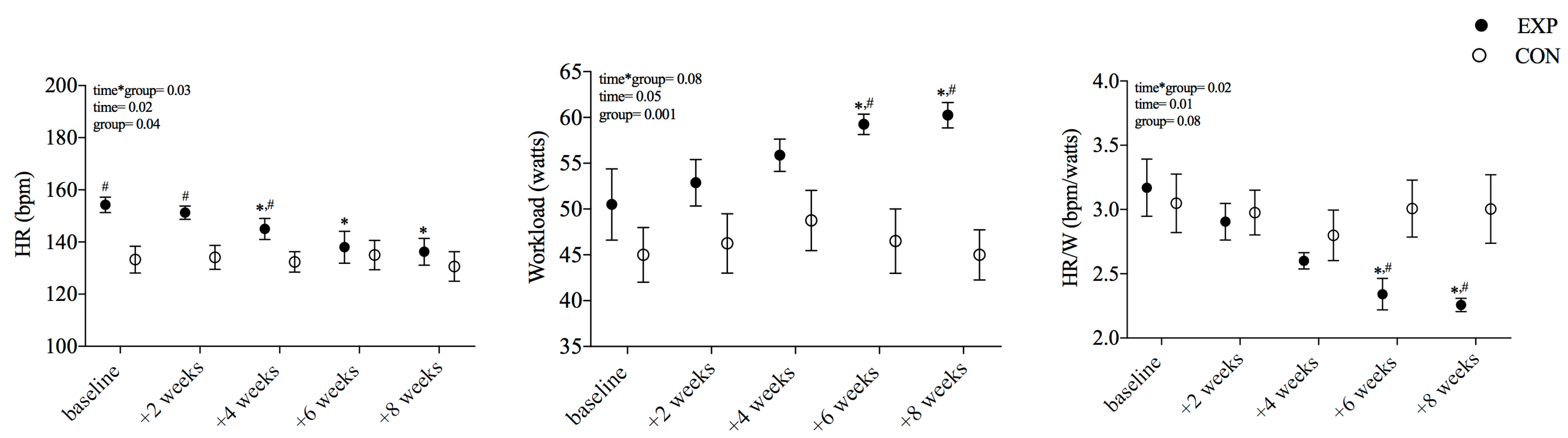
3.3. Heart Rate and Workload Responses to Rowing Stepwise Exercise after Training
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Harridge, S.D.; Lazarus, N.R. Physical activity, aging, and physiological function. Physiology 2017, 32, 152–161. [Google Scholar] [CrossRef] [PubMed]
- Lucini, D.; Cerchiello, M.; Pagani, M. Selective reductions of cardiac autonomic responses to light bicycle exercise with aging in healthy humans. Auton. Neurosci. 2004, 110, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Rodeheffer, R.J.; Gerstenblith, G.; Becker, L.C.; Fleg, J.L.; Weisfeldt, M.L.; Lakatta, E.G. Exercise cardiac output is maintained with advancing age in healthy human subjects: Cardiac dilatation and increased stroke volume compensate for a diminished heart rate. Circulation 1984, 69, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Lakkata, E.G. Cardiovascular regulatory mechanisms in advanced age. Physiol. Rev. 1993, 73, 413–469. [Google Scholar] [CrossRef]
- Katzel, L.I.; Sorkin, J.D.; Fleg, J.L. A comparison of longitudinal changes in aerobic fitness in older endurance athletes and sedentary men. J. Am. Geriatr. Soc. 2001, 49, 1657–1664. [Google Scholar] [CrossRef]
- Mazzeo, R.S.P.; Cavanagh, P.P.; Evans, W.J.P.; Fiatarone, M.; Hagberg, J.P.; McAuley, E.; Startzell, J. ACSM Position Stand: Exercise and Physical Activity for Older Adults. Med. Sci. Sports Exerc. 1998, 30, 992–1008. [Google Scholar] [CrossRef]
- Alkhatib, A.; Klonizakis, M. Effects of exercise training and Mediterranean diet on vascular risk reduction in post-menopausal women. Clin. Hemorheol. Microcirc. 2014, 57, 33–47. [Google Scholar] [CrossRef]
- Volianitis, S.; Yoshiga, C.C.; Secher, N.H. The physiology of rowing with perspective on training and health. Eur. J. Appl. Physiol. 2020, 120, 1943–1963. [Google Scholar] [CrossRef]
- Antero-Jacquemin, J.; Desgorces, F.D.; Dor, F.; Sedeaud, A.; Haïda, A.; LeVan, P.; Toussaint, J.F. Row for your life: A century of mortality follow- p of French Olympic rowers. PLoS ONE 2014, 9, 113362. [Google Scholar] [CrossRef]
- Pedersen, B.K.; Saltin, B. Evidence for prescribing exercise as therapy in chronic disease. Scand. J. Med. Sci. Sports 2006, 16, S3–S63. [Google Scholar] [CrossRef]
- Kawano, H.; Iemitsu, M.; Gando, Y.; Ishijima, T.; Asaka, M.; Aoyama, T.; Ando, T.; Tokizawa, K.; Miyachi, M.; Sakamoto, S.; et al. Habitual rowing exercise is associated with high physical fitness without affecting arterial stiffness in older men. J. Sports Sci. 2012, 30, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Yoshiga, C.C.; Higuchi, M.; Oka, J. Rowing prevents muscle wasting in older men. Eur. J. Appl. Physiol. 2002, 88, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Olsen, D.B.; Scheede-Bergdahl, C.; Reving, D.; Boushel, R.; Dela, F. The effect of rowing on endothelial function and insulin action in healthy controls and in patients with type 2 diabetes. Scand. J. Med. Sci. Sports 2010, 21, 420–430. [Google Scholar] [CrossRef]
- Krainski, F.; Hastings, J.L.; Heinicke, K.; Romain, N.; Pacini, E.L.; Snell, P.G.; Wyrick, P.; Palmer, M.D.; Haller, R.G.; Levine, B.D. The effect of rowing ergometry and resistive exercise on skeletal muscle structure and function during bed rest. J. Appl. Physiol. 2014, 116, 1569–1581. [Google Scholar] [CrossRef]
- Liwicka, E.; Nowak, A.; Zep, W.; Leszczyński, P.; Pilaczyńska-Szcześniak, Ł. Bone mass and bone metabolic indices in male master rowers. J. Bone Miner. Metab. 2015, 33, 540–546. [Google Scholar] [CrossRef]
- Shibata, S.; Fu, Q.; Bivens, T.B.; Hastings, J.L.; Wang, W.; Levine, B.D. Short-term exercise training improves the cardiovascular response to exercise in the postural orthostatic tachycardia syndrome. J. Physiol. 2012, 590, 3495–3505. [Google Scholar] [CrossRef] [PubMed]
- Seifert, T.; Brassard, P.; Wissenberg, M.; Rasmussen, P.; Nordby, P.; Stallknecht, B.; Adser, H.; Jakobsen, A.H.; Pilegaard, H.; Nielsen, H.B.; et al. Endurance training enhances BDNF release from the human brain. Am. J. Physiol. Integr. Comp. Physiol. 2010, 298, R372–R377. [Google Scholar] [CrossRef]
- Belman, M.J.; Gaesser, G.A. Exercise training below and above the lactate threshold in the elderly. Med. Sci. Sports Exerc. 1991, 23, 562–568. [Google Scholar] [CrossRef]
- De Vito, G.; Hernandez, R.; Gonzalez, V.; Felici, F.; Figura, F. Low intensity physical training in older subjects. J. Sports Med. Phys. Fitness. 1997, 37, 72–77. [Google Scholar]
- Meijer, E.P.; Westerterp, K.R.; Verstappen, F.T.J. Effect of exercise training on total daily physical activity in elderly humans. Eur. J. Appl. Physiol. 1999, 80, 16–21. [Google Scholar] [CrossRef]
- Gulli, G.; Cevese, A.; Cappelletto, P.; Gasparini, G.; Schena, F. Moderate aerobic training improves autonomic cardiovascular control in older women. Clin. Auton. Res. 2003, 13, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Braz, N.F.; Carneiro, M.V.; Oliveira-Ferreira, F.; Arrieiro, A.N.; Amorim, F.T.; Lima, M.M.; Avelar, N.C.; Lacerda, A.C.; Peixoto, M.F. Influence of aerobic training on cardiovascular and metabolic parameters in elderly hypertensive women. Int. J. Prev. Med. 2012, 3, 652–659. [Google Scholar] [PubMed]
- Ferreira, L.F.; Rodrigues, G.D.; Soares, P.P.D. Quantity of aerobic exercise training for the improvement of heart rate vari-ability in older adults. Int. J. Cardiovasc. Sci. 2017, 30, 157. [Google Scholar]
- Meneghelo, R.S.; Araújo, C.G.; Stein, R.; Mastrocolla, L.E.; Albuquerque, P.F.; Serra, S.M. Sociedade Brasileira de Cardiologia. III Diretrizes da Sociedade Brasileira de Cardiologia sobre teste ergométrico. Arq. Bras. Cardiol. 2010, 95 (Suppl. S1), 1–26. [Google Scholar]
- Cole, C.R.; Blackstone, E.H.; Pashkow, F.J.; Snader, C.E.; Lauer, M.S. Heart-rate recovery immediately after exercise as a pre-dictor of mortality. N Engl. J. Med. 1999, 341, 1351–1357. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A fexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 2009, 41, 3–13. [Google Scholar] [CrossRef]
- Basset, D.R.; Howley, E.T. Limiting factors for maximum oxygen uptake and determinants of endurance performance. Med. Sci. Sports Exerc. 2000, 32, 70–84. [Google Scholar] [CrossRef]
- Blair, S.N.; Kampert, J.B.; Kohl, H.W., III; Barlow, C.E.; Macera, C.A.; Paffenbarger, R.S., Jr.; Gibbons, L.W. Influences of cardi-orespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA 1996, 276, 205–210. [Google Scholar] [CrossRef]
- Coudert, J.; Van Praagh, E. Endurance exercise training in the elderly: Effects on cardiovascular function. Curr. Opin. Clin. Nutr. Metab. Care. 2000, 3, 479–483. [Google Scholar] [CrossRef]
- Spina, R.J.; Ogawa, T.; Kohrt, W.M.; Martin, W.H., 3rd; Holloszy, J.O.; Ehsani, A.A. Differences in cardiovascular adaptations to endurance exercise training between older men and women. J. Appl. Physiol. 1993, 75, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Spina, R.J. 10 Cardiovascular Adaptations to Endurance Exercise Training in Older Men and Women. Exerc. Sport Sci. Rev. 1999, 27, 317–332. [Google Scholar] [CrossRef] [PubMed]
- Hejazi, K.; Askari, R.; Hofmeister, M. Effects of physical exercise on bone mineral density in older postmenopausal women: A systematic review and meta-analysis of randomized controlled trials. Arch. Osteoporos. 2022, 17, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Klonizakis, M.; Moss, J.; Gilbert, S.; Broom, D.; Foster, J.; Tew, G. Low-volume high-intensity interval training rapidly improves cardiopulmonary function in postmenopausal women. Menopause 2014, 21, 1099–1105. [Google Scholar] [CrossRef] [PubMed]
- Lyall, G.K.; Birk, G.K.; Harris, E.; Ferguson, C.; Riches-Suman, K.; Kearney, M.T.; Porter, K.E.; Birch, K.M. Efficacy of interval exercise training to improve vascular health in sedentary postmenopausal females. Physiol. Rep. 2022, 10, e15441. [Google Scholar] [CrossRef]
- Duarte, A.; Soares, P.P.; Pescatello, L.; Farinatti, P. Aerobic Training Improves Vagal Reactivation Regardless of Resting Vagal Control. Med. Sci. Sports Exerc. 2015, 47, 1159–1167. [Google Scholar] [CrossRef]
- MacMillan, J.S.; Davis, L.L.; Durham, C.F.; Matteson, E.S. Exercise and heart rate recovery. Heart Lung J. Acute Crit. Care. 2006, 35, 383–390. [Google Scholar] [CrossRef]
- Imai, K.; Sato, H.; Hori, M.; Kusuoka, H.; Ozaki, H.; Yokoyama, H.; Takeda, H.; Inoue, M.; Kamada, T. Vagally mediated heart rate recovery after exercise is accelerated in athletes but blunted in patients with chronic heart failure. J. Am. Coll. Cardiol. 1994, 24, 1529–1535. [Google Scholar] [CrossRef]
- Buchheit, M.; Papelier, Y.; Laursen, P.B.; Ahmaidi, S. Noninvasive assessment of cardiac parasympathetic function: Postexercise heart rate recovery or heart rate variability? Am. J. Physiol. Heart Circ. Physiol. 2007, 293, H8–H10. [Google Scholar] [CrossRef]
- Darr, K.C.; Bassett, D.R.; Morgan, B.J.; Thomas, D.P. Effects of age and training status on heart rate recovery after peak exercise. Am. J. Physiol. Circ. Physiol. 1988, 254, H340–H343. [Google Scholar] [CrossRef]
- Lind, L.; Andren, B. Heart rate recovery after exercise is related to the insulin resistance syndrome and heart rate varia-bility in elderly men. Am. Heart J. 2002, 144, 666–672. [Google Scholar] [PubMed]
- Njemanze, H.; Warren, C.; Eggett, C.; MacGowan, G.A.; Bates, M.G.; Siervo, M.; Ivkovic, S.; Trenell, M.I.; Jakovljevic, D.G. Age-related decline in cardiac autonomic function is not attenuated with increased physical activity. Oncotarget 2016, 7, 76390–76397. [Google Scholar] [CrossRef] [PubMed]
- Fleg, J.L.; O’Connor, F.; Gerstenblith, G.; Becker, L.C.; Clulow, J.; Schulman, S.P.; Lakatta, E. Impact of age on the cardiovascular response to dynamic upright exercise in healthy men and women. J. Appl. Physiol. 1995, 78, 890–900. [Google Scholar] [CrossRef] [PubMed]
| CON (n = 10) | EXP (n = 13) | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Baseline | Post-Intervention | Baseline | Post-Intervention | Int. | Time | Group | |
| Total body mass (kg) | 64.86 ± 8.95 | 64.88 ± 9.06 | 60.37 ± 11.75 | 60.40 ± 11.95 | 0.98 | 0.92 | 0.33 |
| SBP (mmHg) | 121 ± 14 | 121 ± 15 | 124 ± 10 | 116 ± 10 | 0.03 | 0.04 | 0.61 |
| DBP (mmHg) | 77 ± 11 | 77 ± 12 | 76 ± 8 | 74 ± 8 | 0.48 | 0.48 | 0.33 |
| HR (bpm) | 82 ± 10 | 78 ± 10 | 76 ± 11 | 79 ± 10 | 0.20 | 0.77 | 0.38 |
| CON (n = 10) | EXP (n = 13) | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Baseline | Post-Intervention | Baseline | Post-Intervention | Int. | Time | Group | |
| VO2peak (mL·kg−1·min−1) | 18.2 ± 3.69 | 18.28 ± 3.41 | 18.06 ± 2.66 | 21.76 ± 3.22 *,#,d | 0.01 | 0.01 | 0.22 |
| VEpeak (L/min) | 36.90 ± 4.65 | 37.66 ± 5.03 | 33.76 ± 6.76 | 35.40 ± 8.45 a | 0.07 | 0.34 | 0.47 |
| RQpeak | 1.06 ± 0.08 | 1.09 ± 0.12 | 1.08 ± 0.07 | 1.07 ± 0.07 a | 0.59 | 0.28 | 0.74 |
| SVpeak (mL) | 93.34 ± 16.96 | 87.72 ± 18.85 | 92.1 ± 18.08 | 103.84 ± 22.09 *,#,c | 0.01 | 0.01 | 0.29 |
| COpeak (L/min) | 12.50 ± 2.21 | 12.21 ± 2.07 | 14.87 ± 3.07 | 17.26 ± 4.14 *,#,d | 0.01 | 0.01 | 0.01 |
| HRpeak (bpm) | 150 ± 10 | 153 ± 10 | 163 ± 15 | 164 ± 14 b | 0.67 | 0.03 | 0.13 |
| HRR (bpm) | 20 ± 2 | 20 ± 4 | 21 ± 1 | 27 ± 1 *,c | 0.01 | 0.01 | 0.16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Araujo, R.C.; Rodrigues, G.D.; Ferreira, L.F.; Soares, P.P.d.S. The Time Course of Cardiorespiratory Adaptations to Rowing Indoor Training in Post-Menopausal Women. Int. J. Environ. Res. Public Health 2023, 20, 3238. https://doi.org/10.3390/ijerph20043238
Araujo RC, Rodrigues GD, Ferreira LF, Soares PPdS. The Time Course of Cardiorespiratory Adaptations to Rowing Indoor Training in Post-Menopausal Women. International Journal of Environmental Research and Public Health. 2023; 20(4):3238. https://doi.org/10.3390/ijerph20043238
Chicago/Turabian StyleAraujo, Renata Cardoso, Gabriel Dias Rodrigues, Luana Farinazzo Ferreira, and Pedro Paulo da Silva Soares. 2023. "The Time Course of Cardiorespiratory Adaptations to Rowing Indoor Training in Post-Menopausal Women" International Journal of Environmental Research and Public Health 20, no. 4: 3238. https://doi.org/10.3390/ijerph20043238
APA StyleAraujo, R. C., Rodrigues, G. D., Ferreira, L. F., & Soares, P. P. d. S. (2023). The Time Course of Cardiorespiratory Adaptations to Rowing Indoor Training in Post-Menopausal Women. International Journal of Environmental Research and Public Health, 20(4), 3238. https://doi.org/10.3390/ijerph20043238







