Abstract
Timely arrival at a hospital capable of percutaneous coronary intervention (PCI) is critical in treating acute myocardial infarction (AMI). We examined the association between driving time to the nearest PCI-capable hospital and case fatality among AMI patients. A total of 142,474 AMI events during 2013–2019 from the Beijing Cardiovascular Disease Surveillance System were included in this cross-sectional study. The driving time from the residential address to the nearest PCI-capable hospital was calculated. Logistic regression was used to estimate the risk of AMI death associated with driving time. In 2019, 54.5% of patients lived within a 15-min drive to a PCI-capable hospital, with a higher proportion in urban than peri-urban areas (71.2% vs. 31.8%, p < 0.001). Compared with patients who had driving times ≤15 min, the adjusted odds ratios (95% CI, p value) for AMI fatality risk associated with driving times 16–30, 31–45, and >45 min were 1.068 (95% CI 1.033–1.104, p < 0.001), 1.189 (95% CI 1.127–1.255, p < 0.001), and 1.436 (95% CI 1.334–1.544, p < 0.001), respectively. Despite the high accessibility to PCI-capable hospitals for AMI patients in Beijing, inequality between urban and peri-urban areas exists. A longer driving time is associated with an elevated AMI fatality risk. These findings may help guide the allocation of health resources.
1. Introduction
Ischemic heart disease is a leading cause of death worldwide [1]. Acute myocardial infarction (AMI) is a serious, often-fatal manifestation of ischemic heart disease. Timely arrival to hospitals with percutaneous coronary intervention (PCI) capability after the onset of AMI is critical to lowering the risk of death [2,3]. It has been reported that 70.7% of patients hospitalized with AMI arrived at the hospital ≥2 h after symptom onset in China [4], while the obstacles for timely hospital arrival are yet to be elucidated. Geographic accessibility to hospitals has been thought to be associated with prolonged pre-hospital delay [5]. However, to what extent geographic accessibility may affect pre-hospital delay and prognosis for patients with AMI is poorly understood.
Several studies have investigated the association between geographic accessibility to PCI-capable hospitals and death among patients with AMI at the patient level or neighborhood level [6,7,8,9,10]. Three studies conducted at the patient level have assessed the association of straight-line distance and driving time to PCI-capable hospitals with the risk of in-hospital death [6,7,8]. However, half of all AMI deaths occur out of the hospital [11], and patients affected most by geographic accessibility may be more likely to die before reaching a PCI-capable hospital. Two published studies focused on AMI mortality rates (including both pre-hospital death and in-hospital death) at the neighborhood level but not the patient level [9,10]. Additionally, existing studies have failed to consider the impact of traffic conditions on driving time [8,10] or the impact of road networks on travel distance [6,7,9]. Therefore, the association between driving time to the nearest PCI-capable hospital and the risk of AMI death at the patient level is yet to be elucidated. Such investigations could guide the emergency care of AMI and affect decision-making on health resource allocations.
Using AMI events extracted from the Beijing Cardiovascular Disease Surveillance System (BCDSS), we aimed to quantify the driving time from the residential address to the nearest PCI-capable hospital considering traffic congestion during 2013–2019 in Beijing, and to further assess its association with the risk of AMI case fatality including both pre-hospital and in-hospital fatality.
2. Materials and Methods
2.1. Data Sources
Beijing, China’s capital city, comprises six districts as urban areas and ten districts as peri-urban areas [12]. We identified patients with AMI in Beijing using the BCDSS, which links routinely collected records in the Beijing Hospital Discharge Information System and the Beijing Vital Registration Monitoring System using personal identification information (Figure S1) [13]. The Beijing Hospital Discharge Information System covers admissions to all secondary- and tertiary-level hospitals in Beijing that are authorized to admit patients and provide comprehensive in-hospital medical, prevention, rehabilitation, and health care services. AMI admissions were identified on the basis of principal discharge diagnoses with International Classification of Diseases, Tenth Revision (ICD-10) codes I21–I22 (acute myocardial infarction and subsequent myocardial infarction) [14]. The Beijing Vital Registration Monitoring System covers all deaths in Beijing [15]. Deaths from AMI including both pre-hospital and in-hospital deaths were identified on the basis of the underlying cause of death using ICD-10 codes I21–I22 [14]. The diagnosis of AMI in the BCDSS has been validated as described in Supplementary Method S1. The study was approved by the ethics review committee at Beijing An Zhen Hospital, Capital Medical University, with a waiver of informed consent (2021139X).
2.2. Study Population
The system identified 179,866 AMI records among the permanent Beijing residents aged ≥35 years between 2013 and 2019. We took multiple steps to avoid double-counting AMI events. Patients who were discharged and then readmitted (including transferred patients) or died on the same day were deemed as single continuous care episodes (n = 5169). Patients discharged alive with a total length of stay of ≤1 day and without readmission or death on the same day were excluded (n = 2428) because these were unlikely to be AMI cases [16]. For patients with multiple events during the study period, we included a randomly selected single event and excluded other events for the same patient (n = 17,093) [17]. Information on the residential address for each patient was obtained from the BCDSS. To protect patient privacy, the number of the smallest unit for the address such as the apartment number was masked in the database. Patient addresses were geocoded to latitude and longitude coordinates, of which the 12,700 addresses that could not be geocoded to the patient level were excluded. After excluding patients with missing demographic information (n = 2), 142,474 AMI events were included in this analysis (Figure S2).
2.3. Study Outcomes
The primary outcome was AMI death and secondary outcomes were pre-hospital and in-hospital AMI deaths. AMI deaths were identified on the basis of the underlying cause of death on the death certificate. We defined hospitalized patients with a primary diagnosis of AMI and died during hospitalization as in-hospital AMI death and the remainder as pre-hospital AMI death.
2.4. Driving Time to the Nearest PCI-Capable Hospital
Hospitals in the BCDSS that reported performing PCI in patients were considered PCI-capable hospitals [18]. The addresses of PCI-capable hospitals were geocoded to the latitude and longitude coordinates. The road network system in Beijing has basically been stable in recent years. We considered the road network in 2021 and the impact of traffic conditions such as road congestion on driving time in a real setting [19]. We identified the nearest PCI-capable hospital for patients by computing the vehicle driving time along the road network between each patient–hospital pair using a web mapping application program interface [20] on the basis of the pair’s geographical coordinates. Because AMI most frequently occurs during the morning [21], we estimated the driving time during the morning peak traffic hours in 2021 and used the driving time during the evening peak traffic hours as a sensitivity analysis. Then, the driving time was adjusted using the Beijing Transport Development Annual Report to obtain the PCI-capable hospital accessibility in the year of the patient’s onset [22].
2.5. Covariates
Age, sex, marital status, comorbidities, day of the week (weekday or weekend), and year of the event were obtained from the BCDSS. Comorbidities were defined as any concomitant diagnosis including heart failure (ICD-10 code I50) and stroke (ICD-10 codes I60, I61, I63, and I64). The average year of education at the township level was extracted from the 2010 national population census [23]. Socioeconomic status included average per-capita disposable income at the district level from 2015 to 2019 derived from the statistical yearbook [24] and the proportion of unemployed derived at the district level from the 2010 national population census [23]. Cardiovascular risk factors at the district level included the average prevalence of hypertension, diabetes, hypercholesterolemia, and smoking in 2014 and 2017.
2.6. Statistical Analysis
Continuous variables were presented as means and standard deviations (SD), and differences between groups were compared using the one-way analysis of variance. Categorical variables were reported as numbers (percentages) and compared using the chi-squared test.
A multilevel logistic regression model was used to evaluate the risk of AMI death associated with driving time, which allowed the patients (level-1) to be nested within districts (level-2). The odds ratio (OR) and corresponding 95% confidence intervals (CI) were calculated. We stratified the driving time into four categories (≤15 min, 16–30 min, 31–45 min, and >45 min). Model 1 was univariate. Model 2 was adjusted for age and sex. Model 3 was further adjusted for marital status, years of education, day of the week, year of the event, per-capita disposable income (district level), and the proportion of unemployed (district level). Model 4 was additionally adjusted for heart failure, stroke, and the prevalence rate (district level) of hypertension, diabetes, hypercholesterolemia, and smoking. To assess possible effect modification, we conducted analyses stratified by age group (<65 and ≥65 years) and sex. Product terms between the driving time categories and dichotomized age and sex were additionally included in model 4, and a Wald test was used to calculate the p value for multiplicative interactions.
We further explored the association between driving time and the risk of pre-hospital and in-hospital death. In the analysis of the association between driving time and in-hospital death, patients who died pre-hospital were excluded. To adjust for potential selection bias in excluding pre-hospital deaths, we applied the inverse probability of selection weights (i.e., proportional to the reciprocal probability of having died before hospital admission) in a weighted regression in which an individual was assigned their selection weight [25]. Restricted cubic splines were used to flexibly model the concentration–response association between the driving time and the risk of pre-hospital death and in-hospital death. The number of knots was selected using the Akaike information criterion.
Three sensitivity analyses were performed to check the robustness of the results. First, we included the first event or the last event instead of a randomly selected single event for patients who had multiple AMI events during the study period. Second, we used the driving time during the evening peak traffic hours to assess the risk of AMI death associated with driving time. Third, we determined the driving distance along the road network from the patients’ residential address to the nearest PCI-capable hospital using the web mapping application program interface [20]. We then applied the driving distance as an alternative accessibility measurement to assess the association with AMI death.
All statistical analyses were performed using Stata software, version 17 (StataCorp., College Station, TX, USA). A 2-sided p < 0.05 was considered statistically significant.
3. Results
3.1. Characteristics of the Study Population
A total of 142,474 AMI events in Beijing between 2013 and 2019 were identified. The mean (SD) age was 69.3 (13.6) years, and 65.1% were male. Overall, 81.9% of patients were married, and 55.0% lived in urban areas. The numbers and proportions of patients within the driving time categories of ≤15, 16–30, 31–45, and >45 min were 67,821 (47.6%), 49,688 (34.9%), 18,038 (12.7%), and 6927 (4.8%), respectively. Patients with driving times ≤15 min were more likely to be male and had a higher proportion of heart failure and stroke. In addition, these patients were more likely to live in urban areas and in districts with higher per-capita disposable income and a lower proportion of unemployment (Table 1).

Table 1.
Characteristics of patients with acute myocardial infarction in Beijing between 2013 and 2019.
3.2. Driving Time to the Nearest PCI-Capable Hospital
During the study period, the median driving time to the nearest PCI-capable hospital for patients decreased gradually in Beijing from 16.6 to 13.9 min (Figure 1). In 2019, 54.5% (11,010/20,192) and 86.5% (17,471/20,192) of patients lived within a 15-min and 30-min drive to a PCI-capable hospital, respectively. Stratified analyses showed that the median driving time for urban patients decreased from 13.2 to 11.8 min over the study period, while that for peri-urban patients decreased from 25.7 to 21.4 min (Figure 1). In 2019, 71.2% (8284/11,628) and 99.1% (11,528/11,628) of patients in urban areas lived within a 15-min and 30-min drive to a PCI-capable hospital, respectively. In comparison, 31.8% (2726/8564) and 69.4% (5943/8564) of patients in peri-urban areas lived within a 15-min and 30-min drive to a PCI-capable hospital, respectively. In 2019, the proportion of patients living within a 15-min and 30-min drive to a PCI-capable hospital in urban areas was significantly higher than that in peri-urban areas (both p < 0.001).
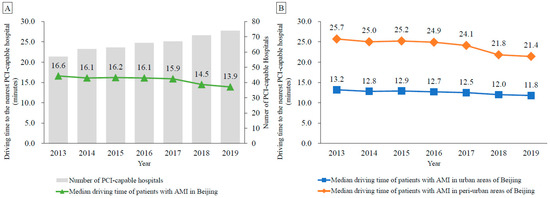
Figure 1.
Median driving time to the nearest percutaneous coronary intervention-capable hospital in Beijing among patients with acute myocardial infarction, 2013–2019. (A) Median driving time of all patients in Beijing; (B) Median driving time of patients in urban and peri-urban areas of Beijing. Abbreviations: AMI, acute myocardial infarction; PCI, percutaneous coronary intervention.
3.3. Association between Driving Time and the Risk of AMI Fatality
Among all AMI events, 33.5% (47,756/142,474) were fatal. The case fatality rates were 30.2% (20,509/67,821), 33.6% (16,710/49,688), 39.6% (7148/18,038), and 48.9% (3389/6927) among patients with driving times ≤15, 16–30, 31–45, and >45 min, respectively. Compared with patients who had driving times ≤15 min, the adjusted ORs (95% CI, p value) for the risk of AMI fatality among those with driving times of 16–30, 31–45, and >45 min were 1.068 (95% CI 1.033–1.104, p < 0.001), 1.189 (95% CI 1.127–1.255, p < 0.001), and 1.436 (95% CI 1.334–1.544, p < 0.001), respectively (Table 2). The association was stronger among younger patients (35–64 years) and male patients than among older patients (≥65 years) and female patients, respectively (both Pinteraction < 0.001) (Figure 2).

Table 2.
Association between driving time to the nearest percutaneous coronary intervention-capable hospital and the risk of case fatality among patients with acute myocardial infarction.
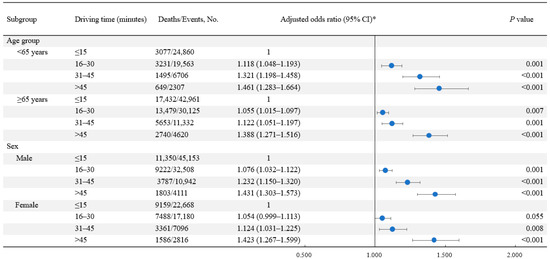
Figure 2.
Subgroup analyses for the association between driving time to the nearest percutaneous coronary intervention-capable hospital and the risk of case fatality among patients with acute myocardial infarction. * Model adjusted for age, sex, marital status, day of the week, year of the event, heart failure, stroke, years of education, per-capita disposable income at the district level, proportion of unemployed at the district level, prevalence of hypertension at the district level, prevalence of diabetes at the district level, prevalence of hypercholesterolemia at the district level, and prevalence of smoking at the district level. Abbreviations: CI, confidence interval.
3.4. Association between Driving Time and the Risk of Pre-Hospital and In-Hospital AMI Fatality
A total of 21,312 pre-hospital fatal events and 26,444 in-hospital fatal events among patients with AMI during the study period were identified. Compared with patients who had driving times ≤15 min, those with driving times of 16–30 min (adjusted OR 1.243, 95% CI 1.174–1.316, p < 0.001), 31–45 min (adjusted OR 1.460, 95% CI 1.347–1.581, p < 0.001), and >45 min (adjusted OR 1.656, 95% CI 1.495–1.836, p < 0.001) had higher risks of pre-hospital fatality in the fully adjusted model. The adjusted ORs (95% CI, p value) for driving times of 16–30, 31–45, and >45 min associated with the risk of in-hospital fatality were 1.028 (0.979–1.080, p = 0.260), 0.851 (0.753–0.962, p = 0.010), and 0.833 (0.675–1.029, p = 0.091), respectively, adjusting for selection bias. Associations between driving time and the risks of both pre-hospital fatality and in-hospital fatality were nonlinear (Pnonlinearity < 0.001 for pre-hospital fatality; Pnonlinearity = 0.030 for in-hospital fatality). The risk of pre-hospital fatality increased with driving time and remained relatively flat when the driving time was more than approximately 40 min, while the risk of in-hospital fatality slightly decreased when the driving time was more than approximately 20 min (Figure 3).
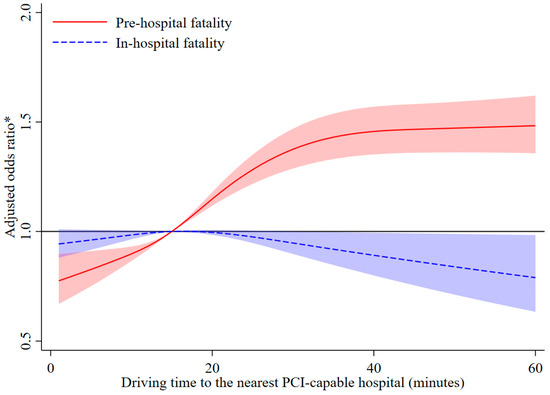
Figure 3.
Restricted cubic spline analysis for the association between driving time to the nearest percutaneous coronary intervention-capable hospital and the risk of pre-hospital fatality and in-hospital fatality among patients with acute myocardial infarction. * Model adjusted for age, sex, marital status, day of the week, year of the event, heart failure, stroke, years of education, per-capita disposable income at the district level, proportion of unemployed at the district level, prevalence of hypertension at the district level, prevalence of diabetes at the district level, prevalence of hypercholesterolemia at the district level, and prevalence of smoking at the district level. In the analysis of the association between driving time and in-hospital death, the model additionally adjusted for potential selection bias.
3.5. Sensitivity Analyses
The results were similar to the main analyses when using the first event (Table S1) or the last event (Table S2) instead of a randomly selected single event for patients with multiple AMI events. The results did not change substantially when using the driving time during the evening peak traffic hours (Table S3) or the driving distance (Table S4) as surrogate measures of driving time during the morning peak traffic hours.
4. Discussion
Using city-wide data from Beijing, we found that the median driving time to the nearest PCI-capable hospital among patients with AMI decreased gradually from 2013 to 2019, and more than half of these patients lived within a 15-min drive to a PCI-capable hospital in 2019. However, a substantial disparity in driving time was found between patients living in urban areas and peri-urban areas. A longer driving time was associated with an increased risk of AMI fatality, especially pre-hospital AMI fatality. These findings reveal considerable inequality in the accessibility to PCI-capable hospitals within a city and highlight a need to improve the allocation of health resources for AMI acute treatment.
There is inconsistent evidence concerning the association of accessibility to PCI-capable hospitals with AMI mortality that includes both pre-hospital death and in-hospital death at the neighborhood level [9,10]. One study reported the adverse effects of a longer driving time to the nearest PCI-capable hospital on AMI mortality at the block group level in the United States [10]. However, another study conducted at the county level in the United States reported no significant association between distance to PCI-capable hospitals and AMI mortality, possibly because there is less variance at the larger scale (county level) than at the smaller scale (block group level) [9].
Our findings indicate the association between a longer driving time and an increased risk for AMI fatality at the patient level. A longer driving time to PCI-capable hospitals among patients with AMI is related to increased total ischemic time, which is associated with an increased risk of death [26]. Regarding the potential biological mechanism for this association, patients who have longer ischemic times may have less myocardium for salvage [26]. Previous studies conducted at the patient level have focused on the association between accessibility to PCI-capable hospitals and the risk of in-hospital death [6,7,8]. We further assessed the effect of driving time on the risk of AMI death stratified by pre-hospital and in-hospital death. Consistent with the results of prior studies [6,7,8], we did not find that increased driving time was associated with a higher risk of in-hospital death. A potential explanation is that patients with AMI who were most affected by accessibility might have died before reaching a PCI-capable hospital and were not included in those studies [6,7,8]. Therefore, it is likely that the increase in mortality risk associated with longer driving times may be underestimated among in-hospital deaths.
In our study, the association between driving time to the nearest PCI-capable hospital and the risk of AMI death differed by age and sex. The following reason may explain the stronger associations among younger patients than among older individuals. Compared with younger patients, older patients with AMI are more likely to use emergency medical services [27], which is associated with substantial reductions in ischemic time and treatment delay [27]. The discrepancy in associations between males and females may be because higher odds of not being aware of any AMI symptoms were associated with the male sex compared with the female sex [28].
Our study using city-wide data can help guide policy deliberations and the allocation of health resources. Although more than 70% of patients in urban areas lived within a 15-min drive to a PCI hospital in 2019, approximately 70% of peri-urban patients had a drive time of more than 15 min. Additionally, our previous work showed that rapid increases in AMI incidence were particularly evident in Beijing’s peri-urban areas [29]. These findings allow for the identification of within-city health care disparities to inform policy-making and cost-effective allocation of health resources. Our results also support Beijing’s recent health policy of providing high-quality medical resources in peri-urban areas [30], which may help reduce urban–rural inequality regarding access to health facilities and effectively reduce AMI deaths.
To our knowledge, this is the first study to estimate the driving time of patients with AMI to the nearest PCI-capable hospital in China using city-wide data and considering traffic congestion. Our system covered both hospitalized cases and pre-hospital deaths from AMI. Therefore, this is the most representative study providing data on the accessibility to PCI-capable hospitals in Beijing. Additionally, most previous studies have used straight-line distance [6,7,9] or speed limits to measure the driving time [10], which may lead to the underestimation of the driving time or distance, especially in megacities. In our study, the driving time based on the road network was estimated by taking the real traffic conditions into account, and the driving distance was estimated by considering the road network, thus providing a more accurate driving time and distance. Finally, this study included both pre-hospital and in-hospital deaths and comprehensively assessed the impact of driving time to the nearest PCI-capable hospital on the risk of death after the onset of AMI.
This study had several limitations. First, the driving time was calculated based on the residential address in our study, while the location where each patient experienced a heart attack was unavailable. However, the mean age of patients was 69.3 years in the current study. Previous research has reported that older adults spent 85% of their time at home [31], and a study conducted in China found that the daily activities of older adults were within a 15-min walking distance, especially a 5–10-min walking distance [32]. Therefore, we assumed that most AMI events occurred at or near the patients’ homes in our study. Second, the exact time of AMI onset was also unavailable. However, given that AMI onset is more common in the morning than at any other time of the day [21], we calculated the driving time during the morning peak traffic hours. The results in the sensitivity analyses when using the driving time during the evening peak traffic hours and driving distance as the accessibility indicators also support our main findings. Finally, whether patients were transported by ambulance was unavailable in our study. However, as found in our previous nationwide registry, only 11.6% of AMI patients in China were transported by ambulance [4]. Therefore, we estimated the driving time for non-ambulance transport. The pre-hospital survival rates could be higher due to the use of defibrillators and cardio-pulmonary resuscitation for AMI patients who reached the hospital by ambulance, although the proportion was low.
5. Conclusions
There is substantial disparity in accessibility to PCI-capable hospitals between urban and peri-urban areas in Beijing. A longer driving time to the nearest PCI-capable hospital is associated with a higher risk of AMI fatality. Considering the uneven distribution of PCI-capable hospital resources in Beijing, our study provides important information for further allocation of medical resources in megacities and may aid in improving the prognosis for AMI patients.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20043166/s1, Method S1: Validation of the diagnosis of acute myocardial infarction in the Beijing Cardiovascular Disease Surveillance System. Table S1: Association between driving time to the nearest percutaneous coronary intervention-capable hospital and the risk of case fatality among patients with the first acute myocardial infarction event, 2013–2019. Table S2: Association between driving time to the nearest percutaneous coronary intervention-capable hospital and the risk of case fatality among patients with the last acute myocardial infarction event, 2013–2019. Table S3: Association between driving time to the nearest percutaneous coronary intervention-capable hospital during evening peak traffic hours and the risk of case fatality among patients with acute myocardial infarction. Table S4: Association between driving distance to the nearest percutaneous coronary intervention-capable hospital and the risk of case fatality among patients with acute myocardial infarction. Figure S1: Data source and linkage of the Beijing Cardiovascular Disease Surveillance System. Figure S2: Flowchart of the study population. Reference [33] is cited in the Supplementary Materials.
Author Contributions
Conceptualization, J.L.; Data Curation, J.C., Q.D., P.H., Z.Y., M.G., F.L., Y.S., J.S., Y.Q., Y.L. and J.L.; Formal Analysis, J.C.; Investigation, M.G. and F.L.; Methodology, J.C., Q.D., Z.Y., Y.S., Y.Q., Y.L. and J.L.; Project Administration, Q.D. and J.L.; Visualization, J.C.; Supervision, Y.L. and J.L.; Validation, P.H.; Writing—Original Draft, J.C.; Writing—Review and Editing, J.C., Q.D., P.H., Z.Y., M.G., F.L., Y.S., J.S., Y.Q., Y.L. and J.L.; Funding Acquisition, Q.D. and J.L. All authors contributed to the interpretation of the results and drafting of this manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grants from the National Natural Science Foundation of China (grant numbers 82073635 and 82103962); the Beijing Nova Program Interdisciplinary Cooperation Project (grant number Z191100001119017); the Capital’s Funds for Health Improvement and Research (grant number 2020-1-1051); and the Beijing Municipal Commission of Health (grant number 2021-7). This work was also supported by the Pathways to Equitable Healthy Cities grant from the Wellcome Trust [209376/Z/17/Z]. For the purpose of Open Access, the author has applied a CC BY public copyright license to any Author Accepted Manuscript version arising from this submission. The funders had no role in the study design, collection, analysis, interpretation of data, writing of the manuscript.
Institutional Review Board Statement
The study was approved by the ethics review committee at Beijing An Zhen Hospital, Capital Medical University, with a waiver of informed consent (2021139X).
Informed Consent Statement
The study was approved by the ethics review committee at Beijing An Zhen Hospital, Capital Medical University, with a waiver of informed consent (2021139X). The data were anonymized prior to analysis.
Data Availability Statement
The data used for this study were obtained from the Beijing Municipal Health Big Data and Policy Research Center and cannot be shared publicly given the institutional regulations and the data confidentiality agreement. Similar data may be requested by researchers from the above data holder authorities for research purposes. The analytical methods can be reproduced based on the details provided in this article, and the statistical code is available upon request.
Acknowledgments
We are grateful for the data from the 2014 and 2017 Beijing Chronic Disease and Risk Factors Surveillance, and we thank the data collection teams for their support and contribution to this study.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
PCI: percutaneous coronary intervention; AMI: acute myocardial infarction; BCDSS: Beijing Cardiovascular Disease Surveillance System; ICD-10: International Classification of Diseases, Tenth Revision; SD: standard deviation; OR: odds ratio; CI: confidence interval.
References
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Lawton, J.S.; Tamis-Holland, J.E.; Bangalore, S.; Bates, E.R.; Beckie, T.M.; Bischoff, J.M.; Bittl, J.A.; Cohen, M.G.; DiMaio, J.M.; Don, C.W.; et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: A report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation 2022, 145, e18–e114. [Google Scholar] [CrossRef]
- De Luca, G.; Suryapranata, H.; Ottervanger, J.P.; Antman, E.M. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: Every minute of delay counts. Circulation 2004, 109, 1223–1225. [Google Scholar] [CrossRef] [PubMed]
- Hu, D.Q.; Hao, Y.C.; Liu, J.; Yang, N.; Yang, Y.Q.; Sun, Z.Q.; Zhao, D.; Liu, J. Pre-hospital delay in patients with acute myocardial infarction in China: Findings from the Improving Care for Cardiovascular Disease in China-Acute Coronary Syndrome (CCC-ACS) project. J. Geriatr. Cardiol. 2022, 19, 276–283. [Google Scholar] [PubMed]
- Nilsson, G.; Mooe, T.; Söderström, L.; Samuelsson, E. Pre-hospital delay in patients with first time myocardial infarction: An observational study in a northern Swedish population. BMC Cardiovasc. Disord. 2016, 16, 93. [Google Scholar] [CrossRef]
- Alexandrescu, R.; Bottle, A.; Jarman, B.; Aylin, P. Impact of transfer for angioplasty and distance on AMI in-hospital mortality. Acute Card Care 2012, 14, 5–12. [Google Scholar] [CrossRef]
- Gregory, P.M.; Malka, E.S.; Kostis, J.B.; Wilson, A.C.; Arora, J.K.; Rhoads, G.G. Impact of geographic proximity to cardiac revascularization services on service utilization. Med. Care 2000, 38, 45–57. [Google Scholar] [CrossRef]
- Rhudy JPJr Alexandrov, A.W.; Hyrkäs, K.E.; Jablonski-Jaudon, R.A.; Pryor, E.R.; Wang, H.E.; Bakitas, M.A. Geographic access to interventional cardiology services in one rural state. Heart Lung 2016, 45, 434–440. [Google Scholar] [CrossRef]
- Graves, B.A. Access to cardiac interventional services in Alabama and Mississippi: A geographical information system analysis. Perspect. Health Inf. Manag. 2010, 7, 1b. [Google Scholar]
- Balamurugan, A.; Delongchamp, R.; Im, L.; Bates, J.; Mehta, J.L. Neighborhood and acute myocardial infarction mortality as related to the driving time to percutaneous coronary intervention-capable hospital. J. Am. Heart Assoc. 2016, 5, e002378. [Google Scholar] [CrossRef]
- Grey, C.; Jackson, R.; Schmidt, M.; Ezzati, M.; Asaria, P.; Exeter, D.J.; Kerr, A.J. One in four major ischaemic heart disease events are fatal and 60% are pre-hospital deaths: A national data-linkage study (ANZACS-QI 8). Eur. Heart J. 2017, 38, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Beijing Municipal Science & Technology Commission, Administration Commission of Zhongguancun Science Park. Beijing Technology Market Statistical Annual Report in 2019. Available online: http://kw.beijing.gov.cn/art/2020/12/8/art_6656_578808.html (accessed on 21 November 2022).
- Xie, W.; Li, G.; Zhao, D.; Xie, X.; Wei, Z.; Wang, W.; Wang, M.; Li, G.; Liu, W.; Sun, J.; et al. Relationship between fine particulate air pollution and is chaemic heart disease morbidity and mortality. Heart 2015, 101, 257–263. [Google Scholar] [CrossRef]
- Asaria, P.; Bennett, J.E.; Elliott, P.; Rashid, T.; Iyathooray Daby, H.; Douglass, M.; Francis, D.P.; Fecht, D.; Ezzati, M. Contributions of event rates, pre-hospital deaths, and deaths following hospitalisation to variations in myocardial infarction mortality in 326 districts in England: A spatial analysis of linked hospitalisation and mortality data. Lancet Public Health 2022, 7, e813–e824. [Google Scholar] [CrossRef]
- Liu, R.; Liu, X.; Yang, P.; Du, X.; He, L.; Chen, T.; Li, X.; Xie, G.; Wu, S.; Su, J.; et al. Influenza-associated cardiovascular mortality in older adults in Beijing, China: A population-based time-series study. BMJ Open 2020, 10, e042487. [Google Scholar] [CrossRef]
- Chen, J.; Normand, S.L.; Wang, Y.; Drye, E.E.; Schreiner, G.C.; Krumholz, H.M. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: Progress and continuing challenges. Circulation 2010, 121, 1322–1328. [Google Scholar] [CrossRef]
- Kulkarni, V.T.; Ross, J.S.; Wang, Y.; Nallamothu, B.K.; Spertus, J.A.; Normand, S.L.; Masoudi, F.A.; Krumholz, H.M. Regional density of cardiologists and rates of mortality for acute myocardial infarction and heart failure. Circ. Cardiovasc. Qual. Outcomes 2013, 6, 352–359. [Google Scholar] [CrossRef]
- Nallamothu, B.K.; Bates, E.R.; Wang, Y.; Bradley, E.H.; Krumholz, H.M. Driving times and distances to hospitals with percutaneous coronary intervention in the United States: Implications for prehospital triage of patients with ST-elevation myocardial infarction. Circulation 2006, 113, 1189–1195. [Google Scholar] [CrossRef]
- Niu, Q.; Wang, Y.; Xia, Y.; Wu, H.; Tang, X. Detailed assessment of the spatial distribution of urban parks according to day and travel mode based on Web Mapping API: A case study of main parks in Wuhan. Int. J. Environ. Res. Public Health 2018, 15, 1725. [Google Scholar] [CrossRef]
- Amap. WebService API. Available online: https://lbs.amap.com/api/webservice/guide/api/georegeo#geo (accessed on 21 November 2022).
- Fabbian, F.; Bhatia, S.; De Giorgi, A.; Maietti, E.; Bhatia, S.; Shanbhag, A.; Deshmukh, A. Circadian periodicity of ischemic heart disease: A systematic review of the literature. Heart Fail. Clin. 2017, 13, 673–680. [Google Scholar] [CrossRef]
- Beijing Transport Institute. Beijing Transport Development Annual Report in 2021. Available online: https://www.bjtrc.org.cn/List/index/cid/7.html (accessed on 21 November 2022).
- Beijing Municipal Bureau of Statistics. Tabulation on the 2010 Population Census of Beijing Municipality. Available online: http://tjj.beijing.gov.cn/tjsj_31433/tjsk_31457/202003/t20200327_1740183.html (accessed on 21 November 2022).
- Beijing Municipal Bureau of Statistics. Beijing Regional Statistical Yearbook. Available online: http://nj.tjj.beijing.gov.cn/nj/qxnj/2021/zk/indexch.htm (accessed on 21 November 2022).
- Sun, J.W.; Wang, R.; Li, D.; Toh, S. Use of linked databases for improved confounding control: Considerations for potential selection bias. Am. J. Epidemiol. 2022, 191, 711–723. [Google Scholar] [CrossRef]
- Denktas, A.E.; Anderson, H.V.; McCarthy, J.; Smalling, R.W. Total ischemic time: The correct focus of attention for optimal ST-segment elevation myocardial infarction care. JACC Cardiovasc. Interv. 2011, 4, 599–604. [Google Scholar] [CrossRef] [PubMed]
- Mathews, R.; Peterson, E.D.; Li, S.; Roe, M.T.; Glickman, S.W.; Wiviott, S.D.; Saucedo, J.F.; Antman, E.M.; Jacobs, A.K.; Wang, T.Y. Use of emergency medical service transport among patients with ST-segment-elevation myocardial infarction: Findings from the National Cardiovascular Data Registry Acute Coronary Treatment Intervention Outcomes Network Registry-Get with The Guidelines. Circulation 2011, 124, 154–163. [Google Scholar] [CrossRef]
- Mahajan, S.; Valero-Elizondo, J.; Khera, R.; Desai, N.R.; Blankstein, R.; Blaha, M.J.; Virani, S.S.; Kash, B.A.; Zoghbi, W.A.; Krumholz, H.M.; et al. Variation and disparities in awareness of myocardial infarction symptoms among adults in the United States. JAMA Netw. Open 2019, 2, e1917885. [Google Scholar] [CrossRef]
- Chang, J.; Deng, Q.; Guo, M.; Ezzati, M.; Baumgartner, J.; Bixby, H.; Chan, Q.; Zhao, D.; Lu, F.; Hu, P.; et al. Trends and inequalities in the incidence of acute myocardial infarction among Beijing townships, 2007–2018. Int. J. Environ. Res. Public Health 2021, 18, 12276. [Google Scholar] [CrossRef]
- Beijing Municipal Health Commission. Beijing Health Facilities Special Plan (2020–2035). Available online: http://wjw.beijing.gov.cn/zwgk_20040/ghjh1/202109/t20210910_2490429.html (accessed on 21 November 2022).
- Mckenna, K.; Broome, K.; Liddle, J. What older people do: Time use and exploring the link between role participation and life satisfaction in people aged 65 years and over. Aust. Occup. Ther. J. 2007, 54, 273–284. [Google Scholar] [CrossRef]
- Bu, J.; Yin, J.; Yu, Y.; Zhan, Y. Identifying the daily activity spaces of older adults living in a high-density urban area: A study using the smartphone-based Global Positioning System trajectory in Shanghai. Sustainability 2021, 13, 5003. [Google Scholar] [CrossRef]
- Zhang, Q.; Zhao, D.; Xie, W.; Xie, X.; Guo, M.; Wang, M.; Wang, W.; Liu, W.; Liu, J. Recent trends in hospitalization for acute myocardial infarction in Beijing: Increasing overall burden and a transition from ST-segment elevation to non-ST-segment elevation myocardial infarction in a population-based study. Medicine 2016, 95, e2677. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).