The Dermatologic Care Needs of a Rural Community in South Florida
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Patient Demographics
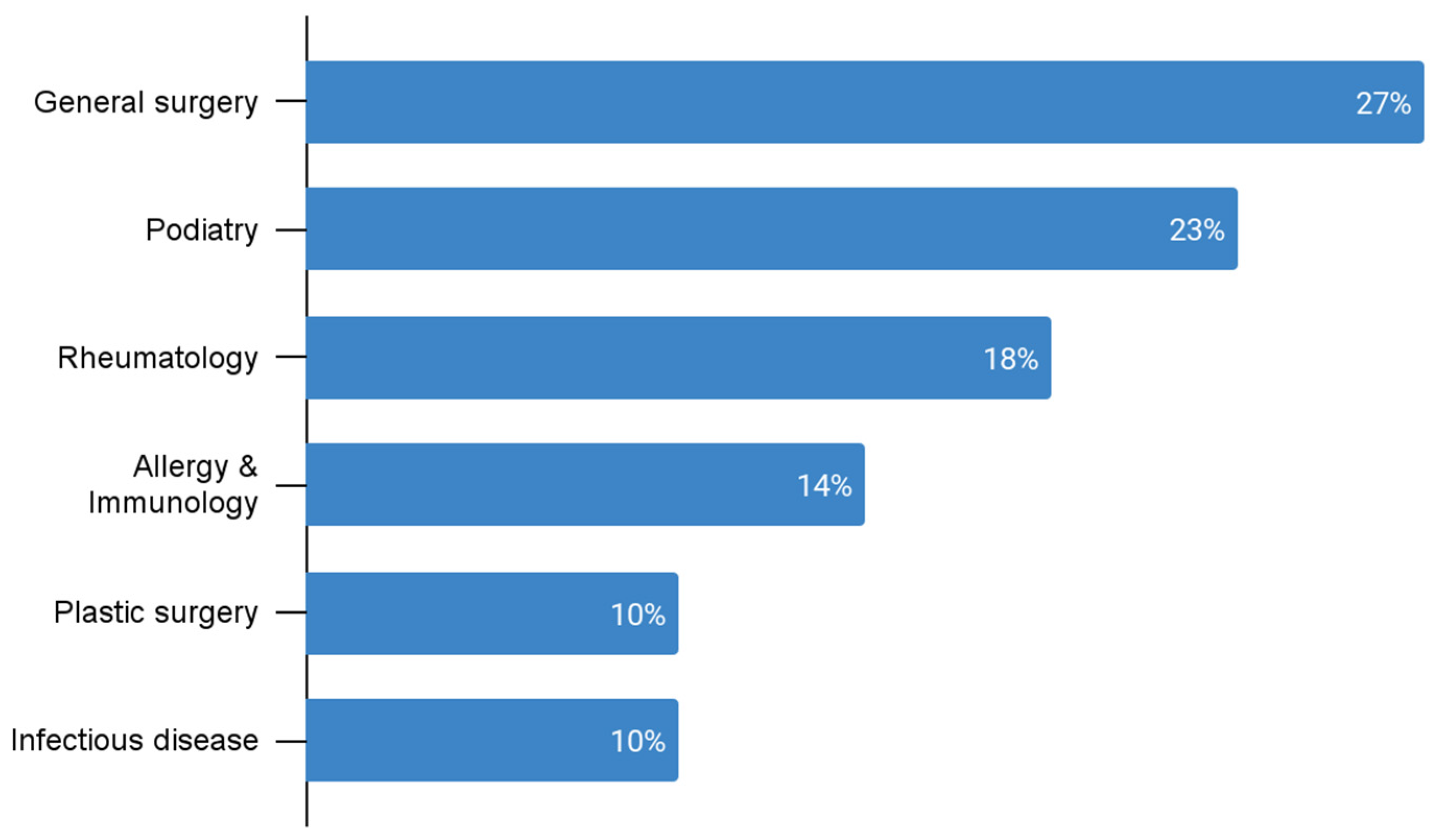
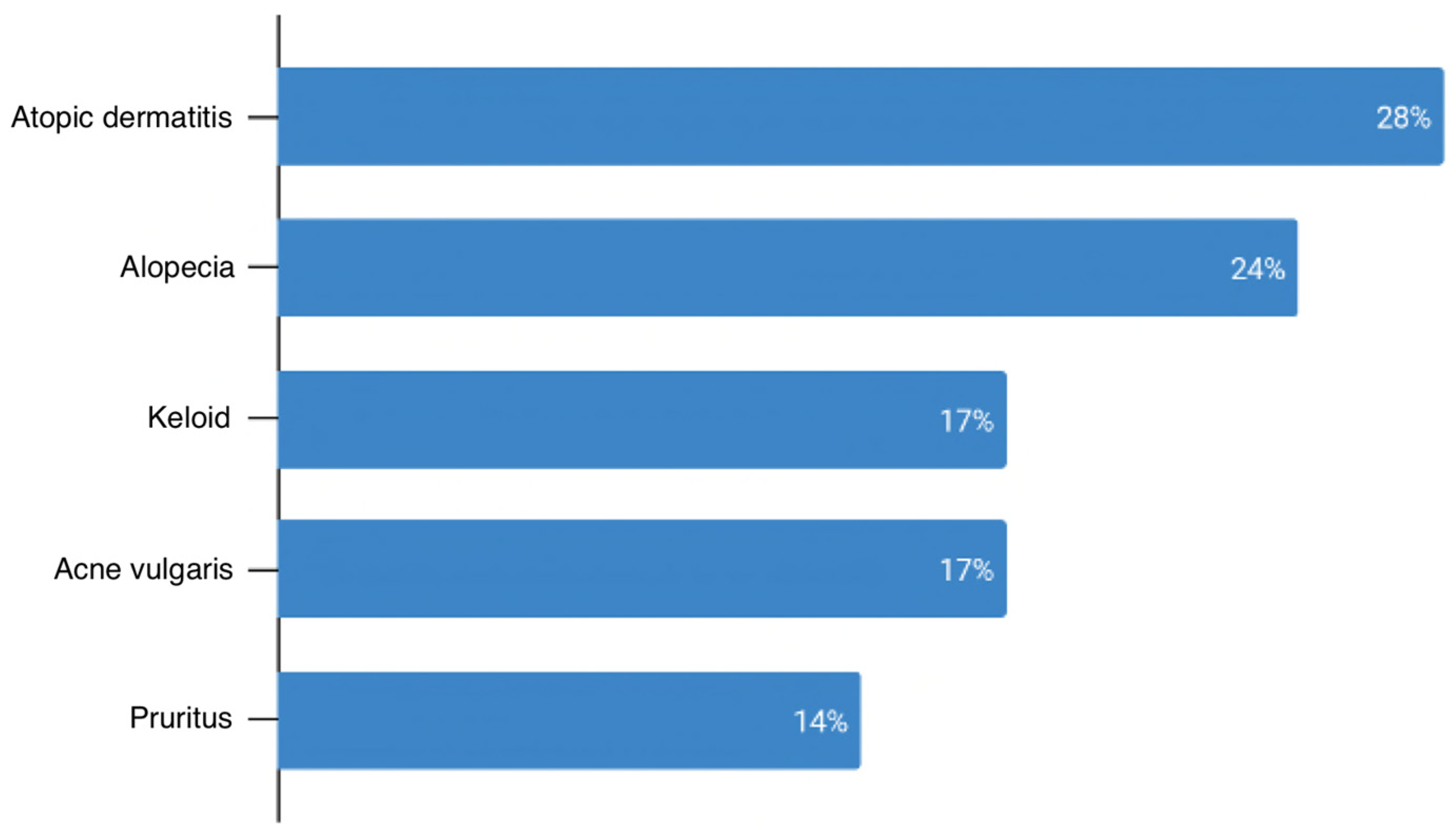
3.2. Diagnosis and Management
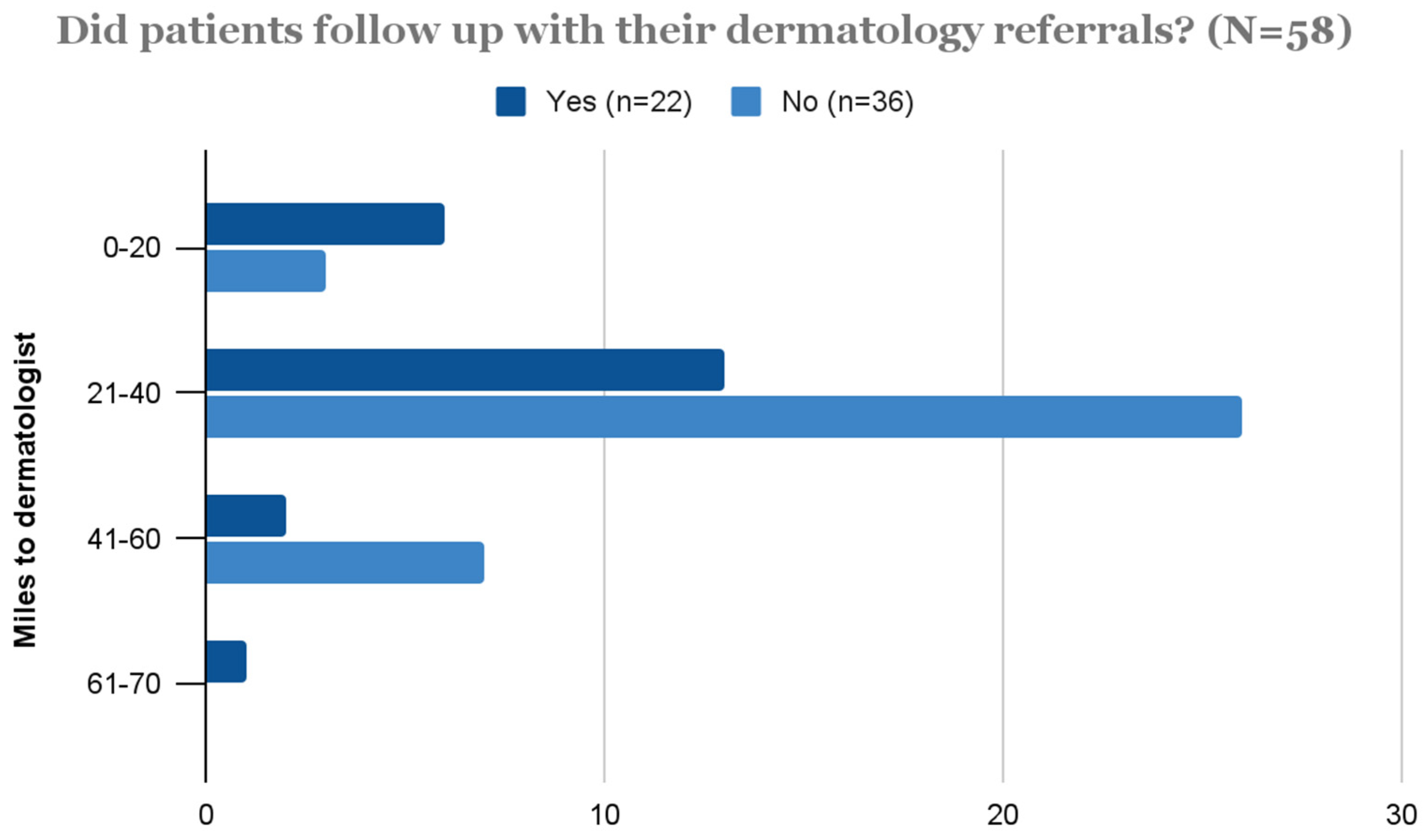
3.3. Outcome
4. Discussion
5. Conclusions and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lantigua, J. As data shows more Americans in poverty, Belle Glade looks for ideas from eastern Palm Beach County. The Palm Beach Post, 18 September 2011. [Google Scholar]
- USAD. Belle Glade, FL. Available online: https://datausa.io/profile/geo/belle-glade-fl/ (accessed on 23 January 2023).
- Lewis, H.; Becevic, M.; Myers, D.; Helming, D.; Mutrux, R.; Fleming, D.A.; Edison, K.E. Dermatology ECHO—An innovative solution to address limited access to dermatology expertise. Rural Remote Health 2018, 18, 4415. [Google Scholar] [CrossRef] [PubMed]
- Lawson, C.N.; Hollinger, J.; Sethi, S.; Rodney, I.; Sarkar, R.; Dlova, N.; Callender, V.D. Updates in the understanding and treatments of skin & hair disorders in women of color. Int. J. Womens Dermatol. 2017, 3, S21–S37. [Google Scholar] [PubMed]
- Davis, S.A.; Narahari, S.; Feldman, S.R.; Huang, W.; Pichardo-Geisinger, R.O.; McMichael, A.J. Top dermatologic conditions in patients of color: An analysis of nationally representative data. J. Drugs Dermatol. 2012, 11, 466–473. [Google Scholar] [PubMed]
- Spiewak, R. Pesticides as a cause of occupational skin diseases in farmers. Ann. Agric. Environ. Med. 2001, 8, 1–5. [Google Scholar] [PubMed]
- Guo, Y.L.; Wang, B.J.; Lee, C.C.; Wang, J.D. Prevalence of Dermatoses and Skin Sensitisation Associated with Use of Pesticides in Fruit Farmers of Southern Taiwan. Occup. Environ. Med. 1996, 53, 427–431. [Google Scholar] [CrossRef] [PubMed]
- Vlachos, C.; Henning, M.A.S.; Gaitanis, G.; Faergemann, J.; Saunte, D.M. Critical Synthesis of Available Data in Malassezia Folliculitis and a Systematic Review of Treatments. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 1672–1683. [Google Scholar] [CrossRef] [PubMed]
- Charles, A.J. Original Article: Superficial Cutaneous Fungal Infections in Tropical Countries. Dermatol. Ther. 2009, 22, 550–559. [Google Scholar] [CrossRef] [PubMed]
- Sharma, B.; Skarma, N. Superficial Mycoses, a Matter of Concern: Global and Indian Scenario-an Updated Analysis. Mycoses 2021, 8, 890–908. [Google Scholar] [CrossRef] [PubMed]
- Runeman, B. Skin Interaction with Absorbent Hygiene Products. Clin. Dermatol. 2008, 26, 45–51. [Google Scholar] [CrossRef] [PubMed]
- CDC. Pesticide-Related Illness and Injury, Acute 2010 Case Definition; CDC: Atlanta, GA, USA, 2021. Available online: Ndc.services.cdc.gov/case-definitions/pesticide-related-illness-and-injury-acute-2010/ (accessed on 23 January 2023).
- Mitchell, R. End the Injustice of Sugarcane Burning. The Palm Beach Post, 12 February 2022. [Google Scholar]
- Mancebo, S.E.; Wang, S.Q. Recognizing the impact of ambient air pollution on skin health. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 2326–2332. [Google Scholar] [CrossRef] [PubMed]
- Acharya, P.; Mathur, M.C. Oxidative stress in alopecia areata: A systematic review and meta-analysis. Int. J. Dermatol. 2020, 59, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Sperling, L.C.; Darling, T.N. Central centrifugal cicatricial alopecia: A common but under-recognized and under-treated disease finally comes of age. J. Cutan. Pathol. 2022, 49, 204–206. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.W.Y.; Hill, C.; Ricks, M.L.; Bennet, J.; Oriol, N.E. The scope and impact of mobile health clinics in the United States: A literature review. Int. J. Equity Health 2017, 16, 178. [Google Scholar] [CrossRef] [PubMed]
- Chuchu, N.; Dinnes, J.; Takwoingi, Y.; Matin, R.N.; Bayliss, S.E.; Davenport, C.; Moreau, J.F.; Bassett, O.; Godfrey, K.; O’Sullivan, C.; et al. Teledermatology for diagnosing skin cancer in adults. Cochrane Database Syst. Rev. 2018, 12, CD013193. [Google Scholar] [CrossRef] [PubMed]
- Canadian Health Services Research Foundation. Evidence boost for quality: Visiting-specialist services to improve access and outcomes for isolated populations. Healthc. Policy 2008, 3, 78–82. [Google Scholar]
| Variable | n (%) or M ± SD |
|---|---|
| Sex | |
| Female | 568 (61) |
| Male | 367 (39) |
| Age | 48 ± 14 |
| Race | |
| American Indian or Alaska Native | 1 (0.1) |
| Asian | 5 (0.5) |
| Black or African-American | 463 (50) |
| Hispanic or Latino | 400 (43) |
| Native Hawaiian or Other Pacific Islander | 1 (0.1) |
| White | 64 (7) |
| Unreported | 1 (0.1) |
| Variable | n (%) or M ± SD |
|---|---|
| Top 10 patient diagnoses (n = 726) | |
| Fungal infection | 257 (35) |
| Dermatitis, unspecified | 173 (24) |
| Pruritus | 93 (13) |
| Benign skin growth | 55 (8) |
| Skin cancer concern | 36 (5) |
| Alopecia | 29 (4) |
| Autoimmune skin disorder | 29 (4) |
| Acne vulgaris | 21 (3) |
| Skin and soft tissue infection | 17 (2) |
| Scabies | 16 (2) |
| Top 5 Actions taken by Physician (n = 935) | |
| Medication prescribed | 680 (73) |
| Referral provided | 200 (21) |
| Labs Ordered | 54 (6) |
| OTC product recommended | 34 (4) |
| In-office procedure performed * | 32 (3) |
| Top 5 Medications prescribed (n = 831) | |
| Anti-fungal | 441 (53) |
| Corticosteroid | 175 (21) |
| Anti-bacterial | 116 (14) |
| Antihistamine | 68 (8) |
| Anti-inflammatory | 31 (4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asbeck, S.M.; Imo, B.U.; Okobi, O.E.; Dorcé-Medard, J. The Dermatologic Care Needs of a Rural Community in South Florida. Int. J. Environ. Res. Public Health 2023, 20, 3071. https://doi.org/10.3390/ijerph20043071
Asbeck SM, Imo BU, Okobi OE, Dorcé-Medard J. The Dermatologic Care Needs of a Rural Community in South Florida. International Journal of Environmental Research and Public Health. 2023; 20(4):3071. https://doi.org/10.3390/ijerph20043071
Chicago/Turabian StyleAsbeck, Sara M., Brenda U. Imo, Okelue E. Okobi, and Jennifer Dorcé-Medard. 2023. "The Dermatologic Care Needs of a Rural Community in South Florida" International Journal of Environmental Research and Public Health 20, no. 4: 3071. https://doi.org/10.3390/ijerph20043071
APA StyleAsbeck, S. M., Imo, B. U., Okobi, O. E., & Dorcé-Medard, J. (2023). The Dermatologic Care Needs of a Rural Community in South Florida. International Journal of Environmental Research and Public Health, 20(4), 3071. https://doi.org/10.3390/ijerph20043071






