Inflammatory Biomarkers Differ among Hospitalized Veterans Infected with Alpha, Delta, and Omicron SARS-CoV-2 Variants
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cohort
2.2. Variables
2.2.1. Exposures
2.2.2. Laboratory Biomarkers
2.2.3. Other Variables
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Variant Determined Based on the Genetic Sequencing | |||||
|---|---|---|---|---|---|
| Alpha | Delta | Omicron | Total | ||
| Variant determined based on the date | Alpha | 42 | 2 | 2 | 46 |
| Delta | 18 | 2031 | 48 | 2097 | |
| Omicron | 0 | 0 | 527 | 527 | |
| Total | 60 | 2033 | 577 | 2670 | |
| Alpha | Delta | Omicron | |
|---|---|---|---|
| Precision | 0.913 | 0.969 | 1.000 |
| Negative Predictive Value | 0.993 | 0.997 | 0.977 |
| Sensitivity | 0.700 | 0.999 | 0.913 |
| Specificity | 0.998 | 0.896 | 1.000 |
| Accuracy | 0.992 | 0.975 | 0.981 |
Appendix B
References
- Rubin, E.J.; Baden, L.R.; Morrissey, S. Audio Interview: Understanding the Omicron Variant of SARS-CoV-2. N. Engl. J. Med. 2022, 386, e27. [Google Scholar] [CrossRef] [PubMed]
- Hachmann, N.P.; Miller, J.; Collier, A.Y.; Ventura, J.D.; Yu, J.; Rowe, M.; Bondzie, E.A.; Powers, O.; Surve, N.; Hall, K.; et al. Neutralization Escape by SARS-CoV-2 Omicron Subvariants BA.2.12.1, BA.4, and BA.5. N. Engl. J. Med. 2022, 387, 86–88. [Google Scholar] [CrossRef]
- Wolter, N.; Jassat, W.; Walaza, S.; Welch, R.; Moultrie, H.; Groome, M.; Amoako, D.G.; Everatt, J.; Bhiman, J.N.; Scheepers, C.; et al. Early assessment of the clinical severity of the SARS-CoV-2 omicron variant in South Africa: A data linkage study. Lancet 2022, 399, 437–446. [Google Scholar] [CrossRef] [PubMed]
- Ulloa, A.C.; Buchan, S.A.; Daneman, N.; Brown, K.A. Estimates of SARS-CoV-2 Omicron Variant Severity in Ontario, Canada. JAMA 2022, 327, 1286–1288. [Google Scholar] [CrossRef] [PubMed]
- Hui, K.P.Y.; Ho, J.C.W.; Cheung, M.C.; Ng, K.C.; Ching, R.H.H.; Lai, K.L.; Kam, T.T.; Gu, H.; Sit, K.Y.; Hsin, M.K.Y.; et al. SARS-CoV-2 Omicron variant replication in human bronchus and lung ex vivo. Nature 2022, 603, 715–720. [Google Scholar] [CrossRef]
- Peacock, T.P.; Brown, J.C.; Zhou, J.; Thakur, N.; Sukhova, K.; Newman, J.; Kugathasan, R.; Yan, A.W.C.; Furnon, W.; De Lorenzo, G.; et al. The altered entry pathway and antigenic distance of the SARS-CoV-2 Omicron variant map to separate domains of spike protein. bioRxiv 2022. [Google Scholar] [CrossRef]
- Petrilli, C.M.; Jones, S.A.; Yang, J.; Rajagopalan, H.; O’Donnell, L.; Chernyak, Y.; Tobin, K.A.; Cerfolio, R.J.; Francois, F.; Horwitz, L.I. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ 2020, 369, m1966. [Google Scholar] [CrossRef]
- Stringer, D.; Braude, P.; Myint, P.K.; Evans, L.; Collins, J.T.; Verduri, A.; Quinn, T.J.; Vilches-Moraga, A.; Stechman, M.J.; Pearce, L.; et al. The role of C-reactive protein as a prognostic marker in COVID-19. Int. J. Epidemiol. 2021, 50, 420–429. [Google Scholar] [CrossRef]
- Bhargava, A.; Kim, T.; Quine, D.B.; Hauser, R.G. A 20-year evaluation of LOINC in the United States’ largest integrated health system. Arch. Pathol. Lab. Med. 2020, 144, 478–484. [Google Scholar] [CrossRef]
- Park, C.; Razjouyan, J.; Hanania, N.A.; Helmer, D.A.; Naik, A.D.; Lynch, K.E.; Amos, C.I.; Sharafkhaneh, A. Elevated Risk of Chronic Respiratory Conditions within 60 Days of COVID-19 Hospitalization in Veterans. Healthcare 2022, 10, 300. [Google Scholar] [CrossRef]
- Razjouyan, J.; Helmer, D.A.; Li, A.; Naik, A.D.; Amos, C.I.; Bandi, V.; Sharafkhaneh, A. Differences in COVID-19-related testing and healthcare utilization by race and ethnicity in the veterans health administration. J. Racial. Ethn. Health Disparities 2022, 9, 519–526. [Google Scholar] [CrossRef]
- Razjouyan, J.; Helmer, D.A.; Lynch, K.E.; Hanania, N.A.; Klotman, P.E.; Sharafkhaneh, A.; Amos, C.I. Smoking status and factors associated with COVID-19 in-hospital mortality among US veterans. Nicotine Tob. Res. 2022, 24, 785–793. [Google Scholar] [CrossRef]
- Hadfield, J.; Megill, C.; Bell, S.M.; Huddleston, J.; Potter, B.; Callender, C.; Sagulenko, P.; Bedford, T.; Neher, R.A. Nextstrain: Real-time tracking of pathogen evolution. Bioinformatics 2018, 34, 4121–4123. [Google Scholar]
- Chakraborty, C.; Sharma, A.R.; Bhattacharya, M.; Mallik, B.; Nandi, S.S.; Lee, S.-S. Comparative genomics, evolutionary epidemiology, and RBD-hACE2 receptor binding pattern in B.1.1.7 (Alpha) and B.1.617.2 (Delta) related to their pandemic response in UK and India. Infect. Genet. Evol. 2022, 101, 105282. [Google Scholar] [CrossRef] [PubMed]
- Paudel, S.; Dahal, A.; Bhattarai, H.K. Temporal Analysis of SARS-CoV-2 Variants during the COVID-19 Pandemic in Nepal. COVID 2021, 1, 423–434. [Google Scholar]
- Orkaby, A.R.; Nussbaum, L.; Ho, Y.L.; Gagnon, D.; Quach, L.; Ward, R.; Quaden, R.; Yaksic, E.; Harrington, K.; Paik, J.M.; et al. The Burden of Frailty Among U.S. Veterans and Its Association With Mortality, 2002–2012. J. Gerontol. A Biol. Sci. Med. Sci. 2019, 74, 1257–1264. [Google Scholar] [CrossRef]
- Merad, M.; Blish, C.A.; Sallusto, F.; Iwasaki, A. The immunology and immunopathology of COVID-19. Science 2022, 375, 1122–1127. [Google Scholar] [CrossRef] [PubMed]
- Ponti, G.; Maccaferri, M.; Ruini, C.; Tomasi, A.; Ozben, T. Biomarkers associated with COVID-19 disease progression. Crit. Rev. Clin. Lab. Sci. 2020, 57, 389–399. [Google Scholar] [CrossRef]
- Suzuki, R.; Yamasoba, D.; Kimura, I.; Wang, L.; Kishimoto, M.; Ito, J.; Morioka, Y.; Nao, N.; Nasser, H.; Uriu, K.; et al. Attenuated fusogenicity and pathogenicity of SARS-CoV-2 Omicron variant. Nature 2022, 603, 700–705. [Google Scholar] [CrossRef]
- Jassat, W.; Abdool Karim, S.S.; Mudara, C.; Welch, R.; Ozougwu, L.; Groome, M.J.; Govender, N.; von Gottberg, A.; Wolter, N.; Wolmarans, M.; et al. Clinical severity of COVID-19 in patients admitted to hospital during the omicron wave in South Africa: A retrospective observational study. Lancet Glob. Health 2022, 10, e961–e969. [Google Scholar] [CrossRef]
- Fall, A.; Eldesouki, R.E.; Sachithanandham, J.; Morris, C.P.; Norton, J.M.; Gaston, D.C.; Forman, M.; Abdullah, O.; Gallagher, N.; Li, M.; et al. The displacement of the SARS-CoV-2 variant Delta with Omicron: An investigation of hospital admissions and upper respiratory viral loads. EBioMedicine 2022, 79, 104008. [Google Scholar] [CrossRef] [PubMed]
- Madhi, S.A.; Kwatra, G.; Myers, J.E.; Jassat, W.; Dhar, N.; Mukendi, C.K.; Nana, A.J.; Blumberg, L.; Welch, R.; Ngorima-Mabhena, N.; et al. Population Immunity and Covid-19 Severity with Omicron Variant in South Africa. N. Engl. J. Med. 2022, 386, 1314–1326. [Google Scholar] [CrossRef] [PubMed]
- Ledford, H. How severe are Omicron infections? Nature 2021, 600, 577–578. [Google Scholar] [CrossRef] [PubMed]
- Skarbinski, J.; Wood, M.S.; Chervo, T.C.; Schapiro, J.M.; Elkin, E.P.; Valice, E.; Amsden, L.B.; Hsiao, C.; Quesenberry, C.; Corley, D.A.; et al. Risk of severe clinical outcomes among persons with SARS-CoV-2 infection with differing levels of vaccination during widespread Omicron (B.1.1.529) and Delta (B.1.617.2) variant circulation in Northern California: A retrospective cohort study. Lancet Reg. Health Am. 2022, 12, 100297. [Google Scholar] [CrossRef]
- Menni, C.; Valdes, A.M.; Polidori, L.; Antonelli, M.; Penamakuri, S.; Nogal, A.; Louca, P.; May, A.; Figueiredo, J.C.; Hu, C.; et al. Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: A prospective observational study from the ZOE COVID Study. Lancet 2022, 399, 1618–1624. [Google Scholar] [CrossRef]
- Bhattacharyya, R.P.; Hanage, W.P. Challenges in Inferring Intrinsic Severity of the SARS-CoV-2 Omicron Variant. N. Engl. J. Med. 2022, 386, e14. [Google Scholar] [CrossRef]
- Altarawneh, H.N.; Chemaitelly, H.; Ayoub, H.H.; Tang, P.; Hasan, M.R.; Yassine, H.M.; Al-Khatib, H.A.; Smatti, M.K.; Coyle, P.; Al-Kanaani, Z.; et al. Effects of Previous Infection and Vaccination on Symptomatic Omicron Infections. N. Engl. J. Med. 2022, 387, 21–34. [Google Scholar] [CrossRef]
- Katz, M.J.; Jump, R.L.P. Omicron infection milder in nursing home residents. Lancet Healthy Longev. 2022, 3, e314–e315. [Google Scholar] [CrossRef]
- Auvigne, V.; Vaux, S.; Strat, Y.L.; Schaeffer, J.; Fournier, L.; Tamandjou, C.; Montagnat, C.; Coignard, B.; Levy-Bruhl, D.; Parent du Chatelet, I. Severe hospital events following symptomatic infection with Sars-CoV-2 Omicron and Delta variants in France, December 2021-January 2022: A retrospective, population-based, matched cohort study. EClinicalMedicine 2022, 48, 101455. [Google Scholar] [CrossRef]
- Krutikov, M.; Stirrup, O.; Nacer-Laidi, H.; Azmi, B.; Fuller, C.; Tut, G.; Palmer, T.; Shrotri, M.; Irwin-Singer, A.; Baynton, V.; et al. Outcomes of SARS-CoV-2 omicron infection in residents of long-term care facilities in England (VIVALDI): A prospective, cohort study. Lancet Healthy Longev. 2022, 3, e347–e355. [Google Scholar] [CrossRef]
- Pranata, R.; Henrina, J.; Lim, M.A.; Lawrensia, S.; Yonas, E.; Vania, R.; Huang, I.; Lukito, A.A.; Suastika, K.; Kuswardhani, R.A.T.; et al. Clinical frailty scale and mortality in COVID-19: A systematic review and dose-response meta-analysis. Arch. Gerontol. Geriatr. 2021, 93, 104324. [Google Scholar] [CrossRef] [PubMed]
- Brownlee, J. One-vs-Rest and One-vs-One for Multi-Class Classification. Machine Learning Mastery. 2020. Available online: https://machinelearningmastery.com/one-vs-rest-and-one-vs-one-for-multi-class-classification/ (accessed on 6 January 2023).
| Alpha | Delta | Omicron | |
|---|---|---|---|
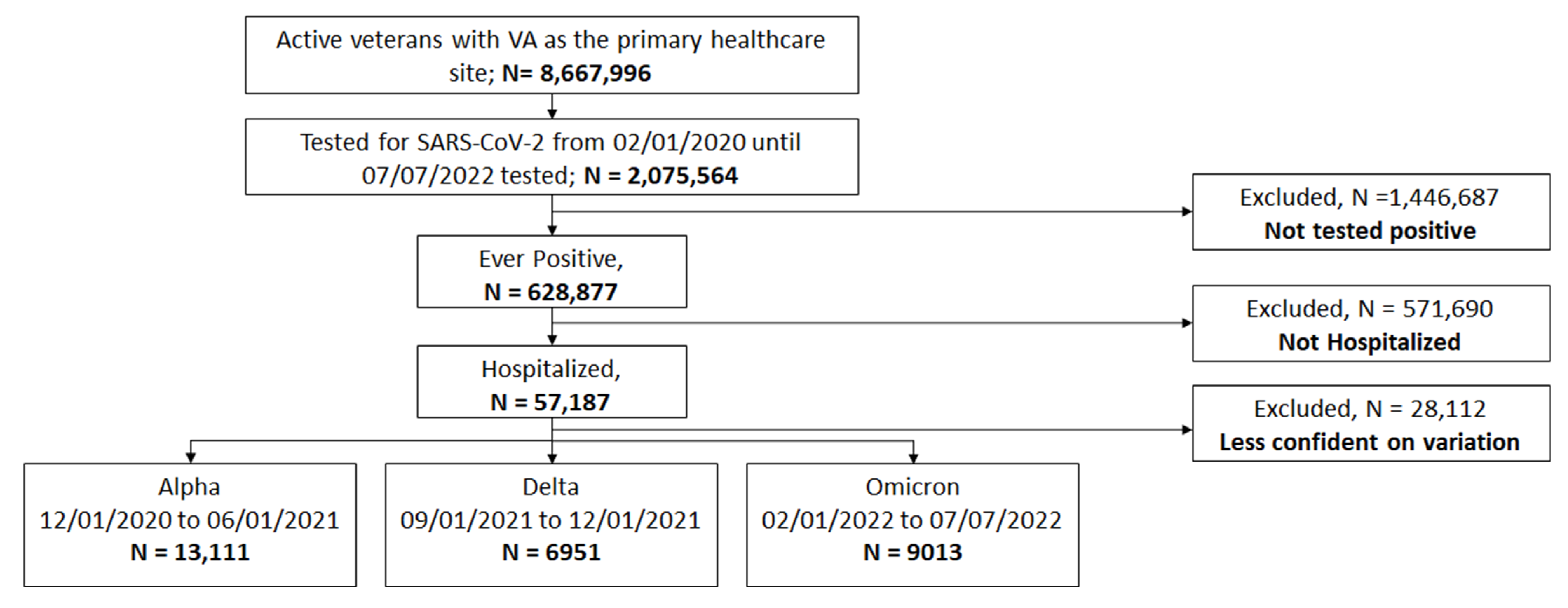
| N | 13,111 (45.1) | 6951 (23.9) | 9013 (31.0) |
| Age: M (SD) | 68.5(13.9) | 67.6 (14.1) | 70.1 (14.3) |
| Age 19–50, N (%) | 1298 (9.9) | 807 (11.6) | 849 (9.4) |
| Age 50–65, N (%) | 2955 (22.5) | 1603 (23.1) | 1603 (17.8) |
| Age 65–75, N (%) | 4624 (35.3) | 2409 (34.7) | 2927 (32.5) |
| Age 75–85, N (%) | 2708 (20.7) | 1464 (21.1) | 2387 (26.5) |
| Age ≥ 85, N (%) | 1526 (11.6) | 668 (9.6) | 1247 (13.8) |
| Sex, Male, N (%) | 12,418 (94.7) | 6563 (94.4) | 8542 (94.8) |
| Race, N (%) | |||
| White | 8421 (64.2) | 5097 (73.3) | 6375 (70.7) |
| Black | 3461 (26.4) | 1252 (18.0) | 1825 (20.2) |
| Other | 1229 (9.4) | 602 (8.7) | 813 (9.0) |
| Ethnicity-Hispanic, N (%) | 1114 (8.5) | 469 (6.7) | 781 (8.7) |
| BMI, Kg/m2, M (SD) | 29.8 (7.1) | 29.5 (7.1) | 28.0 (6.8) |
| BMI < 18.5, N (%) | 372 (2.8) | 233 (3.4) | 414 (4.6) |
| BMI 18.5–30, N (%) | 6939 (52.9) | 3696 (53.2) | 5688 (63.1) |
| BMI ≥ 30, N (%) | 5800 (44.2) | 3022 (43.5) | 2911 (32.3) |
| Comorbid Conditions | |||
| CCI, M (SD) | 3.0 (2.7) | 2.7 (2.6) | 3.3 (2.9) |
| CCI ≥ 2, N (%) | 8378 (63.9) | 4069 (58.5) | 6043 (67.0) |
| Frailty, M (SD) | 0.3 (0.2) | 0.2 (0.2) | 0.1 (0.2) |
| Robust | 2309 (20.2) | 1462 (24.3) | 3992 (60.7) |
| Prefrail | 2469 (21.6) | 1334 (22.1) | 629 (9.6) |
| Frail | 6669 (58.3) | 3232 (53.6) | 1952 (29.7) |
| Any vaccine record | 1467 (11.2) | 3298 (47.4) | 6458 (71.7) |
| Laboratory Tests | |||
| C-reactive protein, N (N = 14,916) | 7570 (50.8) | 4011 (26.9) | 3335 (22.4) |
| C-reactive protein, mg/L, M(IQR) | 12.6 (4.5, 47.1) | 13.3 (5.1, 48.2) | 8.7 (2.5, 31.2) |
| Ferritin, N (N = 13,859) | 7073 (51.0) | 3411 (24.6) | 3375 (24.4) |
| Ferritin, ng/mL, M(IQR) | 432.9 (206.8, 811.0) | 460.5 (216.4, 926.4) | 233.0 (109.0, 494.6) |
| Alanine aminotransferase, N (N = 20,923) | 9897 (47.3) | 5187 (24.8) | 5839 (27.9) |
| Alanine aminotransferase, U/L, M(IQR) | 25.0 (17.0, 39.0) | 27.0 (18.0, 41.0) | 20.0 (14.0, 31.0) |
| Aspartate aminotransferase, N (N = 20,884) | 9918 (47.5) | 5187 (24.8) | 5779 (27.7) |
| Aspartate aminotransferase, U/L, M(IQR) | 32.0 (22.0, 47.0) | 34.0 (23.0, 51.0) | 24.0 (18.0, 37.0) |
| Lactate dehydrogenase, N (N = 11,127) | 5962 (53.6) | 2807 (25.2) | 2358 (21.2) |
| Lactate dehydrogenase, IU/L, M(IQR) | 267.0 (199.0, 369.0) | 284.0 (206.0, 406.0) | 203.0 (161.0, 281.0) |
| Albumin, N (N = 23,159) | 10,777 (46.5) | 5766 (24.9) | 6616 (28.6) |
| Albumin, g/dL, M(IQR) | 3.2 (2.8, 3.5) | 3.2 (2.8, 3.5) | 3.3 (2.9, 3.6) |
| Odds Ratio (95%Confidence Interval) | |||||||
|---|---|---|---|---|---|---|---|
| Abnormality Status | Variation Status, N (%) | Alpha vs. Omicron | Delta vs. Omicron | ||||
| Alpha | Delta | Omicron | Unadjusted | Adjusted † | Unadjusted | Adjusted † | |
| Inflammatory Markers | |||||||
| C-reactive protein | 6540 (86.4) | 3562 (88.8) | 2669 (80.0) | 2.29 * (2.14, 2.45) | 1.94 * (1.75, 2.15) | 2.30 * (2.18, 2.44) | 1.85 * (1.64, 2.09) |
| Ferritin | 4344 (61.4) | 2168 (63.6) | 1357 (40.2) | 1.54 * (1.45, 1.65) | 1.44 * (1.30, 1.60) | 1.91 * (1.81, 2.02) | 1.40 * (1.24, 1.58) |
| Liver Inflammation Markers | |||||||
| Alanine aminotransferase | 1701 (17.2) | 996 (19.2) | 853 (14.6) | 1.49 * (1.38, 1.60) | 1.41 * (1.26, 1.58) | 1.60 * (1.50, 1.70) | 1.25 * (1.09, 1.43) |
| Aspartate aminotransferase | 3607 (36.4) | 2212 (42.6) | 1490 (25.8) | 1.55 * (1.44, 1.67) | 1.53 * (1.37, 1.72) | 1.69 * (1.59, 1.80) | 1.36 * (1.19, 1.56) |
| Lactate dehydrogenase | 3796 (63.7) | 1833 (65.3) | 992 (42.1) | 1.85 * (1.73, 1.98) | 1.69 * (1.52, 1.88) | 2.31 * (2.18, 2.45) | 1.79 * (1.58, 2.03) |
| Liver Metabolic Function | |||||||
| Albumin | 6857 (63.6) | 3685 (63.9) | 3741 (56.5) | 1.66 * (1.52, 1.80) | 1.44 * (1.26, 1.63) | 1.61 * (1.50, 1.73) | 1.19 * (1.02, 1.38) |
| Variation Status, N (%) | Odds Ratio (95%Confidence Interval) | ||||||
|---|---|---|---|---|---|---|---|
| Alpha | Delta | Omicron | Alpha vs. Omicron | Delta vs. Omicron | |||
| Unadjusted | Adjusted † | Unadjusted | Adjusted † | ||||
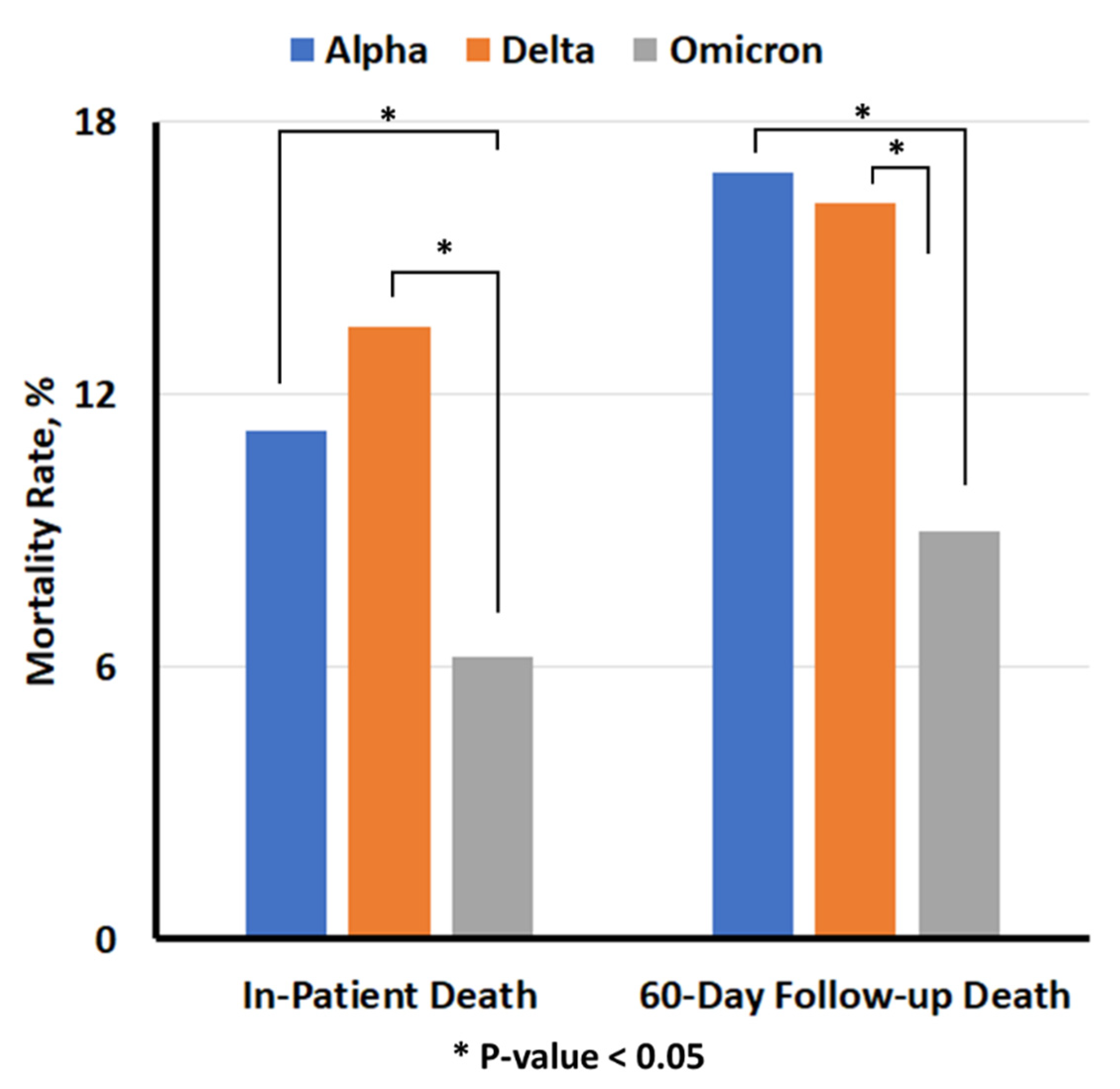
| In-hospital Mortality | 1471 (11.2) | 939 (13.5) | 557 (6.2) | 2.17 * (1.89, 2.49) | 1.68 * (1.47, 1.91) | 2.37 * (2.12, 2.65) | 1.92 * (1.73, 2.12) |
| 60-day follow-up Mortality | 2214 (16.9) | 1127 (16.2) | 815 (9.0) | 1.85 * (1.63, 2.08) | 1.81 * (1.62, 2.02) | 1.95 * (1.77, 2.14) | 2.04 * (1.88, 2.23) |
| Stratifying Analysis based on vaccination records | |||||||
| Mortality in any-Vax | 2 (0.1) | 348 (10.6) | 374 (5.8) | NA | NA | 1.92 * (1.65, 2.24) | 1.49 * (1.21, 1.83) |
| 60-day follow-up Mortality | 5 (0.3) | 432 (13.1) | 559 (8.7) | NA | NA | 1.59 * (1.39, 1.82) | 1.27 * (1.06, 1.51) |
| All | Vaccinated | |||
|---|---|---|---|---|
| OR (95%CI) | Beta | OR (95%CI) | Beta | |
| Abnormal CRP | 1.24 (1.14, 1.36) * | 0.22 | 1.26 (1.06, 1.50) * | 0.23 |
| Omicron | Reference | Reference | Reference | Reference |
| Delta | 2.10 (1.83, 2.41) * | 0.74 | 1.45 (1.18, 1.78) * | 0.37 |
| Alpha | 1.61 (1.41, 1.84) * | 0.48 | NA | NA |
| Age < 50 | Reference | Reference | Reference | Reference |
| age 50–65 | 1.99 (1.40, 2.85) * | 0.69 | 0.94 (0.40, 2.18) | −0.07 |
| age 65–75 | 4.06 (2.88, 5.74) * | 1.40 | 1.81 (0.82, 4.00) | 0.60 |
| age 75–85 | 5.73 (4.04, 8.12) * | 1.74 | 2.85 (1.30, 6.28) * | 1.05 |
| age ≥ 85 | 8.64 (6.06, 12.32) * | 2.16 | 4.08 (1.84, 9.03) * | 1.41 |
| Sex-Male | 1.52 (1.15, 2.00) * | 0.42 | 2.57 (1.13, 5.86) * | 0.94 |
| Race-White | Reference | Reference | Reference | Reference |
| Race-Black | 0.90 (0.80, 1.00) | −0.11 | 0.83 (0.65, 1.07) | −0.18 |
| Race-Other | 1.06 (0.91, 1.24) | 0.06 | 0.86 (0.60, 1.21) | −0.15 |
| Ethnicity | ||||
| BMI 18.5–30 | Reference | Reference | Reference | Reference |
| BMI < 18.5 | 1.78 (1.47, 2.15) * | 0.58 | 2.50 (1.82, 3.44) * | 0.92 |
| BMI ≥ 30 | 0.98 (0.90, 1.08) | −0.02 | 0.83 (0.68, 1.02) | −0.18 |
| CCI ≥ 2 | 1.11 (1.00, 1.23) * | 0.10 | 1.56 (1.21, 2.01) * | 0.45 |
| Frailty Status -Robust | Reference | Reference | Reference | Reference |
| Frailty Status -prefrail | 1.61 (1.37, 1.89) * | 0.48 | 1.21 (0.85, 1.74) | 0.19 |
| Frailty Status -frail | 1.67 (1.44, 1.93) * | 0.51 | 1.83 (1.44, 2.33) * | 0.60 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, C.; Tavakoli-Tabasi, S.; Sharafkhaneh, A.; Seligman, B.J.; Hicken, B.; Amos, C.I.; Chou, A.; Razjouyan, J. Inflammatory Biomarkers Differ among Hospitalized Veterans Infected with Alpha, Delta, and Omicron SARS-CoV-2 Variants. Int. J. Environ. Res. Public Health 2023, 20, 2987. https://doi.org/10.3390/ijerph20042987
Park C, Tavakoli-Tabasi S, Sharafkhaneh A, Seligman BJ, Hicken B, Amos CI, Chou A, Razjouyan J. Inflammatory Biomarkers Differ among Hospitalized Veterans Infected with Alpha, Delta, and Omicron SARS-CoV-2 Variants. International Journal of Environmental Research and Public Health. 2023; 20(4):2987. https://doi.org/10.3390/ijerph20042987
Chicago/Turabian StylePark, Catherine, Shahriar Tavakoli-Tabasi, Amir Sharafkhaneh, Benjamin J. Seligman, Bret Hicken, Christopher I. Amos, Andrew Chou, and Javad Razjouyan. 2023. "Inflammatory Biomarkers Differ among Hospitalized Veterans Infected with Alpha, Delta, and Omicron SARS-CoV-2 Variants" International Journal of Environmental Research and Public Health 20, no. 4: 2987. https://doi.org/10.3390/ijerph20042987
APA StylePark, C., Tavakoli-Tabasi, S., Sharafkhaneh, A., Seligman, B. J., Hicken, B., Amos, C. I., Chou, A., & Razjouyan, J. (2023). Inflammatory Biomarkers Differ among Hospitalized Veterans Infected with Alpha, Delta, and Omicron SARS-CoV-2 Variants. International Journal of Environmental Research and Public Health, 20(4), 2987. https://doi.org/10.3390/ijerph20042987








