Nasopharyngeal Carcinoma Burden and Its Attributable Risk Factors in China: Estimates and Forecasts from 1990 to 2050
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Statistical Analysis
2.3. Software
3. Results
3.1. Nasopharyngeal Carcinoma Burden in China
3.2. Joinpoint Regression on Time Trends of Nasopharyngeal Carcinoma Burden Analysis
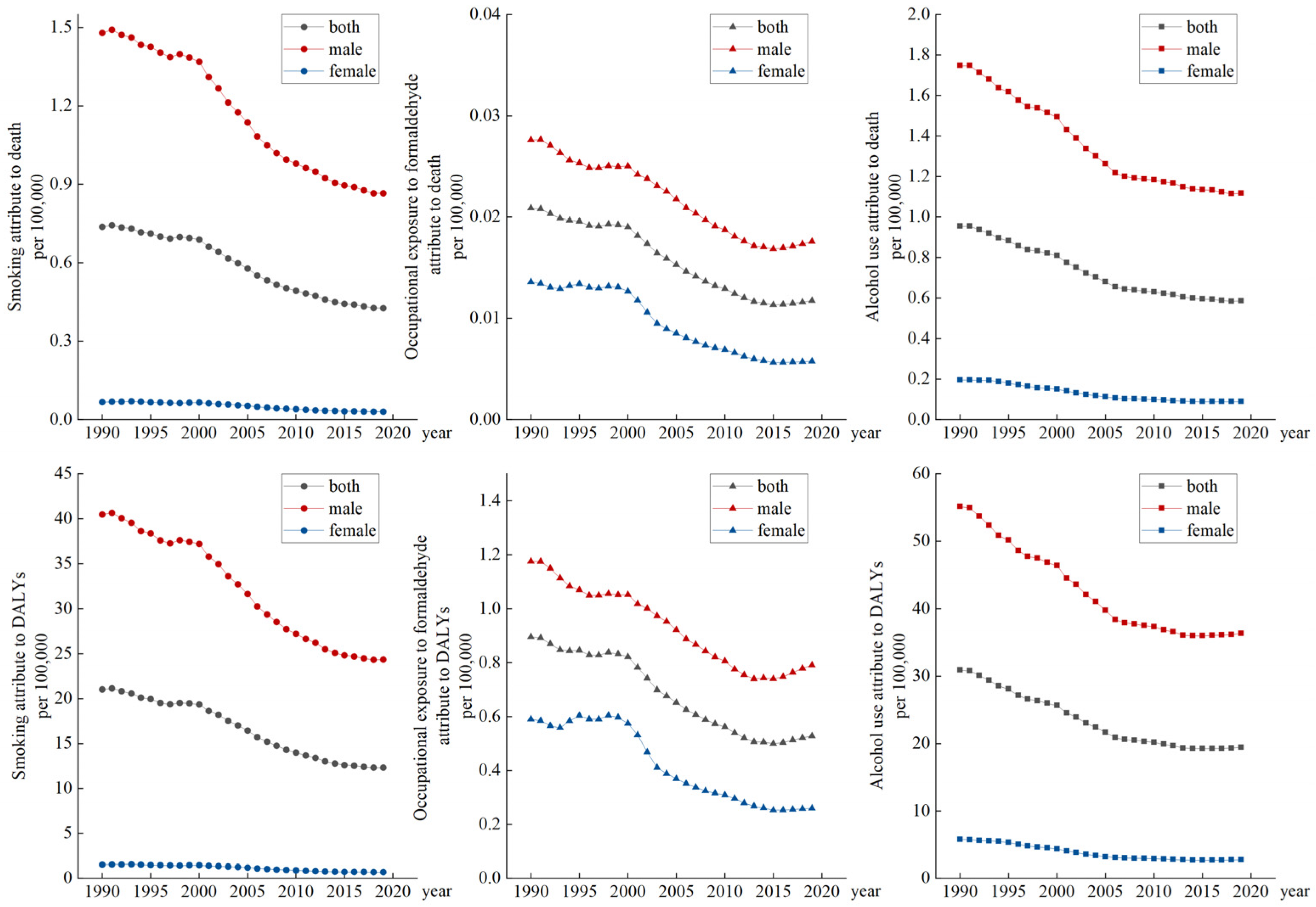
3.3. Impact of Different Risk Factors on Nasopharyngeal Carcinoma Burden
3.4. APC Model Analysis of Nasopharyngeal Carcinoma in China
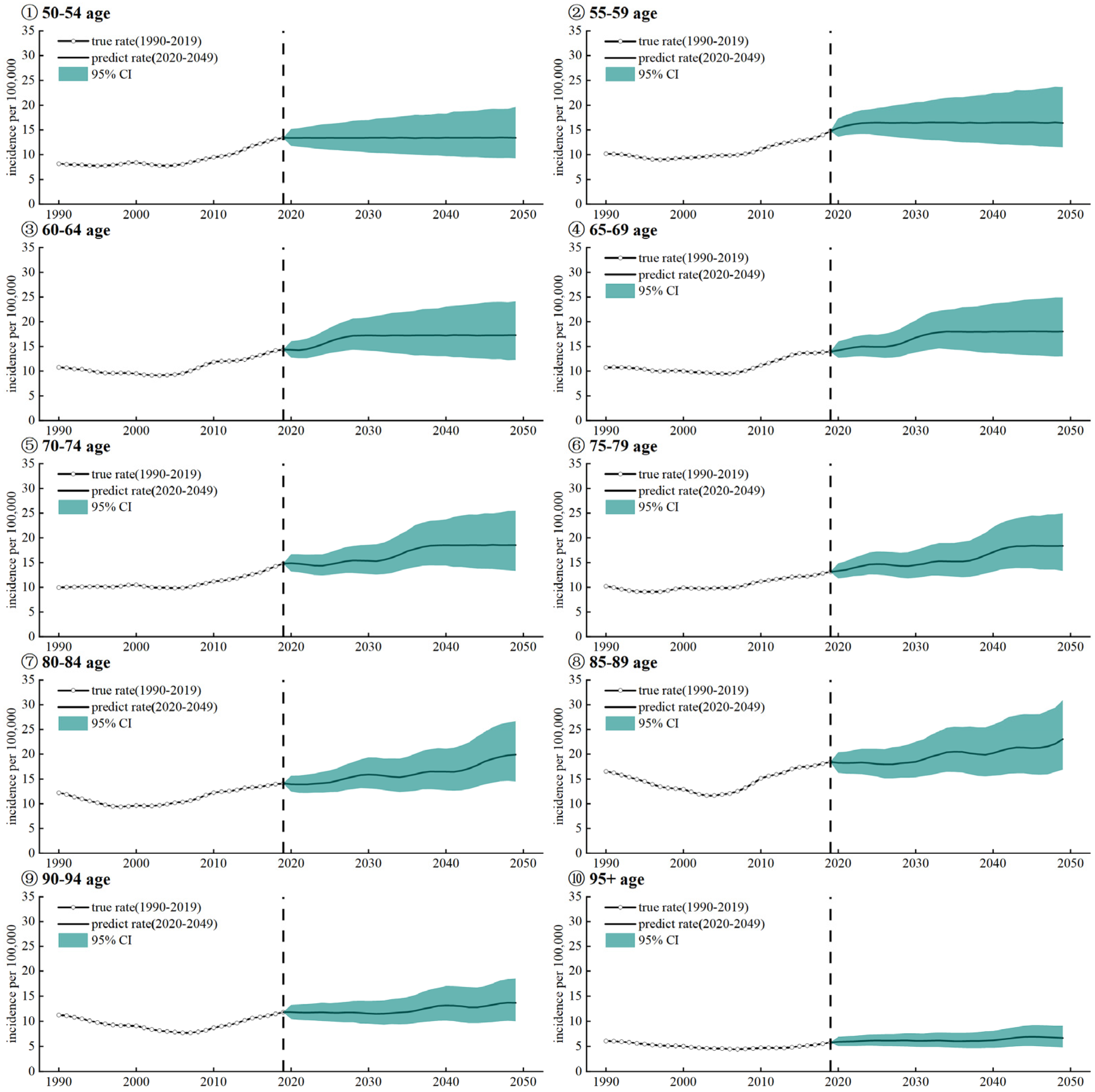
3.5. Prediction of Nasopharyngeal Carcinoma Incidence Rate in Different Age Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gu, Z.; Hu, D.; Cui, W.; Liu, H.; Zhang, C. A Clinical Study on the Factors Associated with Nasopharyngeal Carcinoma among the Chinese Population. Exp. Ther. Med. 2021, 21, 375. [Google Scholar] [CrossRef]
- Chen, Y.-P.; Chan, A.T.C.; Le, Q.-T.; Blanchard, P.; Sun, Y.; Ma, J. Nasopharyngeal Carcinoma. Lancet 2019, 394, 64–80. [Google Scholar] [CrossRef] [PubMed]
- Reffai, A.; Mesmoudi, M.; Derkaoui, T.; Ghailani Nourouti, N.; Barakat, A.; Sellal, N.; Mallick, P.; Bennani Mechita, M. Epidemiological Profile and Clinicopathological, Therapeutic, and Prognostic Characteristics of Nasopharyngeal Carcinoma in Northern Morocco. Cancer Control 2021, 28, 107327482110505. [Google Scholar] [CrossRef]
- Zou, Y.; Yang, R.; Huang, M.-L.; Kong, Y.-G.; Sheng, J.-F.; Tao, Z.-Z.; Gao, L.; Chen, S.-M. NOTCH2 Negatively Regulates Metastasis and Epithelial-Mesenchymal Transition via TRAF6/AKT in Nasopharyngeal Carcinoma. J. Exp. Clin. Cancer Res. 2019, 38, 456. [Google Scholar] [CrossRef]
- Tse, K.-P.; Su, W.-H.; Chang, K.-P.; Tsang, N.-M.; Yu, C.-J.; Tang, P.; See, L.-C.; Hsueh, C.; Yang, M.-L.; Hao, S.-P.; et al. Genome-Wide Association Study Reveals Multiple Nasopharyngeal Carcinoma-Associated Loci within the HLA Region at Chromosome 6p21.3. Am. J. Hum. Genet. 2009, 85, 194–203. [Google Scholar] [CrossRef]
- Zhang, J.; Jia, L.; Tsang, C.M.; Tsao, S.W. EBV Infection and Glucose Metabolism in Nasopharyngeal Carcinoma. In Infectious Agents Associated Cancers: Epidemiology and Molecular Biology; Cai, Q., Yuan, Z., Lan, K., Eds.; Advances in Experimental Medicine and Biology; Springer Singapore: Singapore, 2017; Volume 1018, pp. 75–90. ISBN 978-981-10-5764-9. [Google Scholar]
- Chua, M.L.K.; Wee, J.T.S.; Hui, E.P.; Chan, A.T.C. Nasopharyngeal Carcinoma. Lancet 2016, 387, 1012–1024. [Google Scholar] [CrossRef]
- Ho, J.H.C.; Huang, D.P.; Fong, Y.Y. Salted fish and nasopharyngeal carcinoma in southern chinese. Lancet 1978, 312, 626. [Google Scholar] [CrossRef]
- Jia, W.-H.; Qin, H.-D. Non-Viral Environmental Risk Factors for Nasopharyngeal Carcinoma: A Systematic Review. Semin. Cancer Biol. 2012, 22, 117–126. [Google Scholar] [CrossRef]
- Jin, J.; Ouyang, Z.; Wang, Z. Association of Fruit and Vegetables with the Risk of Nasopharyngeal Cancer: Evidence from a Meta-Analysis. Sci. Rep. 2015, 4, 5229. [Google Scholar] [CrossRef]
- Yin, J.; Jin, W.; Mao, Y.; Wu, Q.; Qiu, J. Wood Dust Exposure and Risks of Nasopharyngeal Carcinoma: A Meta-Analysis. Eur. J. Public Health 2020, 30, 817–822. [Google Scholar] [CrossRef]
- Armstrong, R.W.; Imrey, P.B.; Lye, M.S.; Armstrong, M.J.; Yu, M.C.; Sani, S. Nasopharyngeal Carcinoma in Malaysian Chinese: Occupational Exposures to Particles, Formaldehyde and Heat. Int. J. Epidemiol. 2000, 29, 991–998. [Google Scholar] [CrossRef]
- Long, M.; Fu, Z.; Li, P.; Nie, Z. Cigarette Smoking and the Risk of Nasopharyngeal Carcinoma: A Meta-Analysis of Epidemiological Studies. BMJ Open 2017, 7, e016582. [Google Scholar] [CrossRef]
- Feng, R.; Chang, E.T.; Liu, Z.; Liu, Q.; Cai, Y.; Zhang, Z.; Chen, G.; Huang, Q.; Xie, S.; Cao, S.; et al. Body Mass Index, Body Shape, and Risk of Nasopharyngeal Carcinoma: A Population-based Case–Control Study in Southern China. Cancer Med. 2019, 8, 1835–1844. [Google Scholar] [CrossRef]
- Liu, Y.; Wen, J.; Huang, W. Exosomes in Nasopharyngeal Carcinoma. Clin. Chim. Acta 2021, 523, 355–364. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Tang, L.-L.; Chen, W.-Q.; Xue, W.-Q.; He, Y.-Q.; Zheng, R.-S.; Zeng, Y.-X.; Jia, W.-H. Global Trends in Incidence and Mortality of Nasopharyngeal Carcinoma. Cancer Lett. 2016, 374, 22–30. [Google Scholar] [CrossRef]
- Parascandola, M.; Xiao, L. Tobacco and the Lung Cancer Epidemic in China. Transl. Lung Cancer Res. 2019, 8, S21–S30. [Google Scholar] [CrossRef]
- Nam, J.-M.; McLaughlin, J.K.; Blot, W.J. Cigarette Smoking, Alcohol, and Nasopharyngeal Carcinoma: A Case-Control Study Among U.S. Whites. JNCI J. Natl. Cancer Inst. 1992, 84, 619–622. [Google Scholar] [CrossRef]
- Guo, X.; Johnson, R.C.; Deng, H.; Liao, J.; Guan, L.; Nelson, G.W.; Tang, M.; Zheng, Y.; de The, G.; O’Brien, S.J.; et al. Evaluation of Nonviral Risk Factors for Nasopharyngeal Carcinoma in a High-Risk Population of Southern China. Int. J. Cancer 2009, 124, 2942–2947. [Google Scholar] [CrossRef]
- Cammalleri, V.; Pocino, R.N.; Marotta, D.; Protano, C.; Sinibaldi, F.; Simonazzi, S.; Petyx, M.; Iavicoli, S.; Vitali, M. Occupational Scenarios and Exposure Assessment to Formaldehyde: A Systematic Review. Indoor Air 2022, 32, e12949. [Google Scholar] [CrossRef]
- Tan, L.P.; Tan, G.W.; Sivanesan, V.M.; Goh, S.L.; Ng, X.J.; Lim, C.S.; Kim, W.R.; Mohidin, T.B.B.M.; Mohd Dali, N.S.; Ong, S.H.; et al. Systematic Comparison of Plasma EBV DNA, Anti-EBV Antibodies and MiRNA Levels for Early Detection and Prognosis of Nasopharyngeal Carcinoma. Int. J. Cancer 2020, 146, 2336–2347. [Google Scholar] [CrossRef]
- Lam, W.K.J.; Chan, J.Y.K. Recent Advances in the Management of Nasopharyngeal Carcinoma. F1000Research 2018, 7, 1829. [Google Scholar] [CrossRef]
- Cao, S.-M.; Simons, M.J.; Qian, C.-N. The Prevalence and Prevention of Nasopharyngeal Carcinoma in China. Chin. J. Cancer 2011, 30, 114–119. [Google Scholar] [CrossRef]
- Tang, L.; Chen, Y.; Chen, C.; Chen, M.; Chen, N.; Chen, X.; Du, X.; Fang, W.; Feng, M.; Gao, J.; et al. The Chinese Society of Clinical Oncology (CSCO) Clinical Guidelines for the Diagnosis and Treatment of Nasopharyngeal Carcinoma. Cancer Commun. 2021, 41, 1195–1227. [Google Scholar] [CrossRef]
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer Incidence and Mortality Worldwide: Sources, Methods and Major Patterns in GLOBOCAN 2012: Globocan 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef]
- CI5—Home. Available online: https://ci5.iarc.fr/Default.aspx (accessed on 3 February 2023).
- Wei, K.-R.; Zheng, R.-S.; Zhang, S.-W.; Liang, Z.-H.; Li, Z.-M.; Chen, W.-Q. Nasopharyngeal Carcinoma Incidence and Mortality in China, 2013. Chin. J. Cancer 2017, 36, 90. [Google Scholar] [CrossRef]
- Torre, L.A.; Siegel, R.L.; Jemal, A. Lung Cancer Statistics. In Lung Cancer and Personalized Medicine; Ahmad, A., Gadgeel, S., Eds.; Advances in Experimental Medicine and Biology; Springer International Publishing: Cham, Switzerland, 2016; Volume 893, pp. 1–19. ISBN 978-3-319-24221-7. [Google Scholar]
- Thrift, A.P.; El-Serag, H.B. Burden of Gastric Cancer. Clin. Gastroenterol. Hepatol. 2020, 18, 534–542. [Google Scholar] [CrossRef]
- Machlowska, J.; Baj, J.; Sitarz, M.; Maciejewski, R.; Sitarz, R. Gastric Cancer: Epidemiology, Risk Factors, Classification, Genomic Characteristics and Treatment Strategies. IJMS 2020, 21, 4012. [Google Scholar] [CrossRef]
- Enzinger, P.C. Esophageal Cancer. N. Engl. J. Med. 2003, 349, 2241–2252. [Google Scholar] [CrossRef]
- Wu, S.-G.; Liao, X.-L.; He, Z.-Y.; Tang, L.-Y.; Chen, X.-T.; Wang, Y.; Lin, Q. Demographic and Clinicopathological Characteristics of Nasopharyngeal Carcinoma and Survival Outcomes According to Age at Diagnosis: A Population-Based Analysis. Oral Oncol. 2017, 73, 83–87. [Google Scholar] [CrossRef]
- Fles, R.; Bos, A.C.R.K.; Supriyati; Rachmawati, D.; Waliyanti, E.; Tan, I.B.; Haryana, S.M.; Schmidt, M.K.; Dewi, F.S.T. The Role of Indonesian Patients’ Health Behaviors in Delaying the Diagnosis of Nasopharyngeal Carcinoma. BMC Public Health 2017, 17, 510. [Google Scholar] [CrossRef] [PubMed]



| Measure | Sex | Trend 1 | Trend 2 | Trend 3 | Trend 4 | Trend 5 | Trend 6 | 1900–2019 AAPC (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Years | APC | Years | APC | Years | APC | Years | APC | Years | APC | Years | APC | |||
| Age-standardized incidence Rate | Both | 1990–1996 | −0.825 * | 1996–1999 | 2.105 | 1999–2003 | −0.598 | 2003–2006 | 2.033 | 2006–2009 | 6.701 * | 2009–2019 | 2.786 * | 1.804 (1.296–2.315) |
| Female | 1990–1996 | −0.760 * | 1996–1999 | 1.879 | 1999–2005 | −1.918 * | 2005–2010 | 4.166 * | 2010–2013 | −0.793 | 2013–2019 | 1.861 * | 0.639 (0.131–1.149) | |
| Male | 1990–1996 | −0.778 * | 1996–1999 | 2.018 * | 1999–2003 | 0.247 | 2003–2006 | 2.954 * | 2006–2010 | 6.825 * | 2010–2019 | 3.303 * | 2.326 (1.982–2.671) | |
| Age-standardized death Rate | Both | 1990–1997 | −2.484 * | 1997–2000 | −1.273 * | 2000–2007 | −4.052 * | 2007–2014 | −2.270 * | 2014–2019 | −1.107 * | NA | NA | −2.454 (−2.578–−2.329) |
| Female | 1990–1994 | −2.686 * | 1994–1997 | −4.433 * | 1997–2000 | −2.144 * | 2000–2007 | −5.744 * | 2007–2014 | −3.568 * | 2014–2019 | −1.078 * | −3.498 (−3.671–−3.325) | |
| Male | 1990–1996 | −1.993 * | 1996–2000 | −1.034 * | 2000–2007 | −3.417 * | 2007–2014 | −1.595 * | 2014–2019 | −1.097 * | NA | NA | −1.958 (−2.076–−1.84) | |
| Age-standardized DALY Rate | Both | 1990–1997 | −2.430 * | 1997–2000 | −1.172 | 2000–2003 | −4.704 * | 2003–2007 | −3.944 * | 2007–2014 | −2.360 * | 2014–2019 | −0.446 | −2.394 (−2.522–−2.265) |
| Female | 1990–2000 | −2.649 * | 2000–2003 | −7.583 * | 2003–2007 | −5.695 * | 2007–2014 | −3.672 * | 2014–2019 | −0.844 * | NA | NA | −3.536 (−3.788–−3.282) | |
| Male | 1990–1996 | −2.393 * | 1996–2000 | −0.903 * | 2000–2007 | −3.276 * | 2007–2014 | −1.777 * | 2014–2019 | −0.311 | NA | NA | −1.898 (−2.017–−1.779) | |
| Incidence | Female | Male | ||
|---|---|---|---|---|
| Coef. | p > z | Coef. | p > z | |
| Age (years) | ||||
| 50–54 | −1.429 (−1.618, −1.239) | 0.000 | −0.283 (−0.334, −0.232) | 0.000 |
| 55–59 | −0.604 (−0.779, −0.429) | 0.000 | −0.074 (−0.113, −0.034) | 0.000 |
| 60–64 | −0.134 (−0.312, 0.044) | 0.141 | −0.069 (−0.109, −0.029) | 0.001 |
| 65–69 | −0.417 (−0.597, −0.236) | 0.000 | −0.035 (−0.075, 0.004) | 0.078 |
| 70–74 | −0.016 (−0.197, 0.164) | 0.859 | −0.062 (−0.103, −0.021) | 0.003 |
| 75–79 | 0.04 (−0.141, 0.221) | 0.663 | −0.095 (−0.137, −0.053) | 0.000 |
| 80–84 | 0.192 (0.012, 0.373) | 0.037 | 0.012 (−0.026, −0.05) | 0.531 |
| 85–89 | 1.922 (1.744, 2.101) | 0.000 | 0.474 (0.448, 0.501) | 0.000 |
| 90–94 | 1.353 (1.177, 1.529) | 0.000 | 0.321 (0.293, 0.349) | 0.000 |
| 95+ | −0.908 (−1.092, −0.725) | 0.000 | −0.189 (−0.23, −0.148) | 0.000 |
| Period (year) | ||||
| 1992 | 0.899 (0.771, 1.027) | 0.000 | −0.113 (−0.142, −0.085) | 0.000 |
| 1997 | 0.161 (0.03, 0.293) | 0.016 | −0.046 (−0.074, −0.019) | 0.001 |
| 2002 | −0.318 (−0.45, −0.187) | 0.000 | −0.12 (−0.15, −0.091) | 0.000 |
| 2007 | −0.681 (−0.812, −0.55) | 0.000 | −0.109 (−0.139, −0.08) | 0.000 |
| 2012 | −0.253 (−0.382, −0.125) | 0.000 | 0.132 (0.108,0.155) | 0.000 |
| 2017 | 0.192 (0.056, 0.329) | 0.006 | 0.258 (0.235, 0.28) | 0.000 |
| Cohort (year) | ||||
| 1892–1896 | 1.42 (1.018, 1.823) | 0.000 | 0.364 (0.285, 0.444) | 0.000 |
| 1897–1901 | 1.128 (0.833, 1.423) | 0.000 | 0.136 (0.084, 0.187) | 0.000 |
| 1902–1906 | 0.782 (0.531, 1.034) | 0.000 | 0.034 (−0.008, 0.076) | 0.111 |
| 1907–1911 | 0.184 (−0.042, 0.411) | 0.111 | −0.038 (−0.081, 0.005) | 0.086 |
| 1912–1916 | −0.168 (−0.377, 0.041) | 0.115 | −0.134 (−0.177, −0.091) | 0.000 |
| 1917–1921 | −0.309 (−0.501, −0.116) | 0.002 | −0.078 (−0.115, −0.041) | 0.000 |
| 1922–1926 | −0.246 (−0.445, −0.048) | 0.015 | −0.032 (−0.066, 0.002) | 0.068 |
| 1927–1931 | −0.659 (−0.858, −0.459) | 0.000 | −0.029 (−0.065, 0.007) | 0.113 |
| 1932–1936 | −1.044 (−1.239, −0.848) | 0.000 | −0.117 (−0.161, −0.073) | 0.000 |
| 1937–1941 | −1.281 (−1.468, −1.095) | 0.000 | −0.119 (−0.164, −0.075) | 0.000 |
| 1942–1946 | −0.825 (−1.024, −0.626) | 0.000 | −0.089 (−0.134, −0.044) | 0.000 |
| 1947–1951 | −0.054 (−0.268, 0.161) | 0.624 | −0.013 (−0.059, 0.032) | 0.561 |
| 1952–1956 | 0.152 (−0.087, 0.39) | 0.212 | −0.02 (−0.069, 0.03) | 0.431 |
| 1957–1961 | 0.52 (0.237, 0.803) | 0.000 | 0.01 (−0.046, 0.065) | 0.729 |
| 1962–1966 | 0.399 (−0.07, 0.868) | 0.095 | 0.125 (0.034, 0.216) | 0.007 |
| Constance | 6.816 (6.742, 6.89) | 0.000 | 2.818 (2.803, 2.832) | 0.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, R.; He, Y.; Wei, B.; Lu, Y.; Zhang, J.; Zhang, N.; He, R.; Xue, H.; Zhu, B. Nasopharyngeal Carcinoma Burden and Its Attributable Risk Factors in China: Estimates and Forecasts from 1990 to 2050. Int. J. Environ. Res. Public Health 2023, 20, 2926. https://doi.org/10.3390/ijerph20042926
Zhang R, He Y, Wei B, Lu Y, Zhang J, Zhang N, He R, Xue H, Zhu B. Nasopharyngeal Carcinoma Burden and Its Attributable Risk Factors in China: Estimates and Forecasts from 1990 to 2050. International Journal of Environmental Research and Public Health. 2023; 20(4):2926. https://doi.org/10.3390/ijerph20042926
Chicago/Turabian StyleZhang, Ruhao, Yifei He, Bincai Wei, Yongbo Lu, Jingya Zhang, Ning Zhang, Rongxin He, Hao Xue, and Bin Zhu. 2023. "Nasopharyngeal Carcinoma Burden and Its Attributable Risk Factors in China: Estimates and Forecasts from 1990 to 2050" International Journal of Environmental Research and Public Health 20, no. 4: 2926. https://doi.org/10.3390/ijerph20042926
APA StyleZhang, R., He, Y., Wei, B., Lu, Y., Zhang, J., Zhang, N., He, R., Xue, H., & Zhu, B. (2023). Nasopharyngeal Carcinoma Burden and Its Attributable Risk Factors in China: Estimates and Forecasts from 1990 to 2050. International Journal of Environmental Research and Public Health, 20(4), 2926. https://doi.org/10.3390/ijerph20042926







