Mortality and Years of Life Lost Due to Brain and Other Central Nervous System Cancer in Wuhan, China, from 2010 to 2019
Abstract
1. Introduction
2. Methods
2.1. Study Area and Data Sources
2.2. Study Metrics
2.3. Decomposition of Changes in Deaths
2.4. BAPC Model
2.5. Statistical Analysis
3. Results
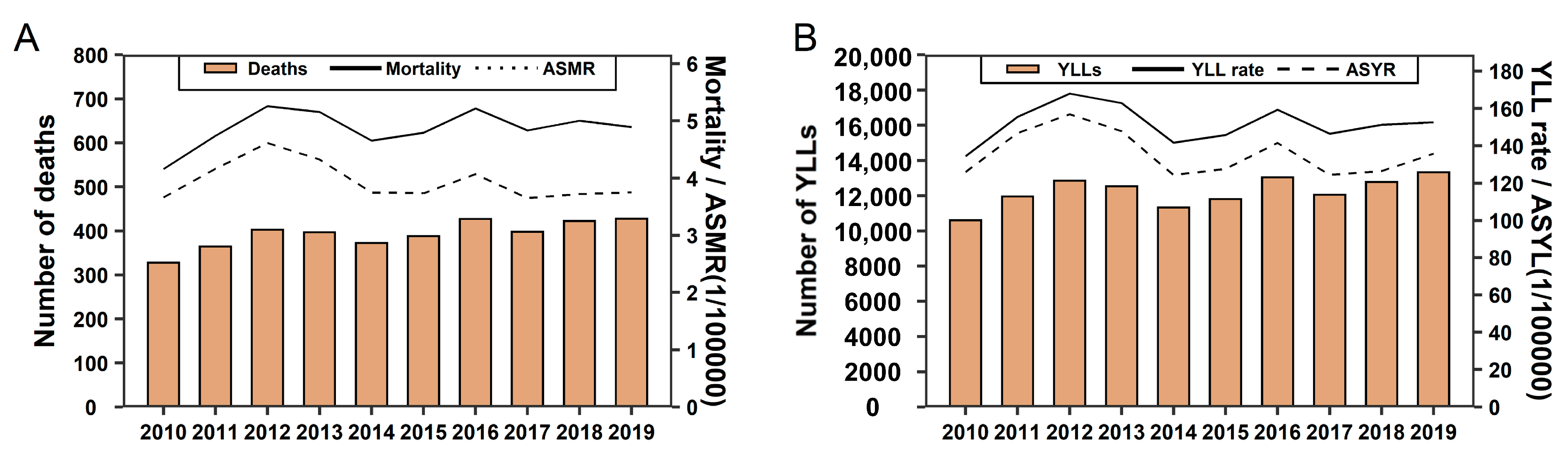
3.1. Temporal Trends of CNS Cancer Burden from 2010 to 2019 and the Forecast for the Next Five Years
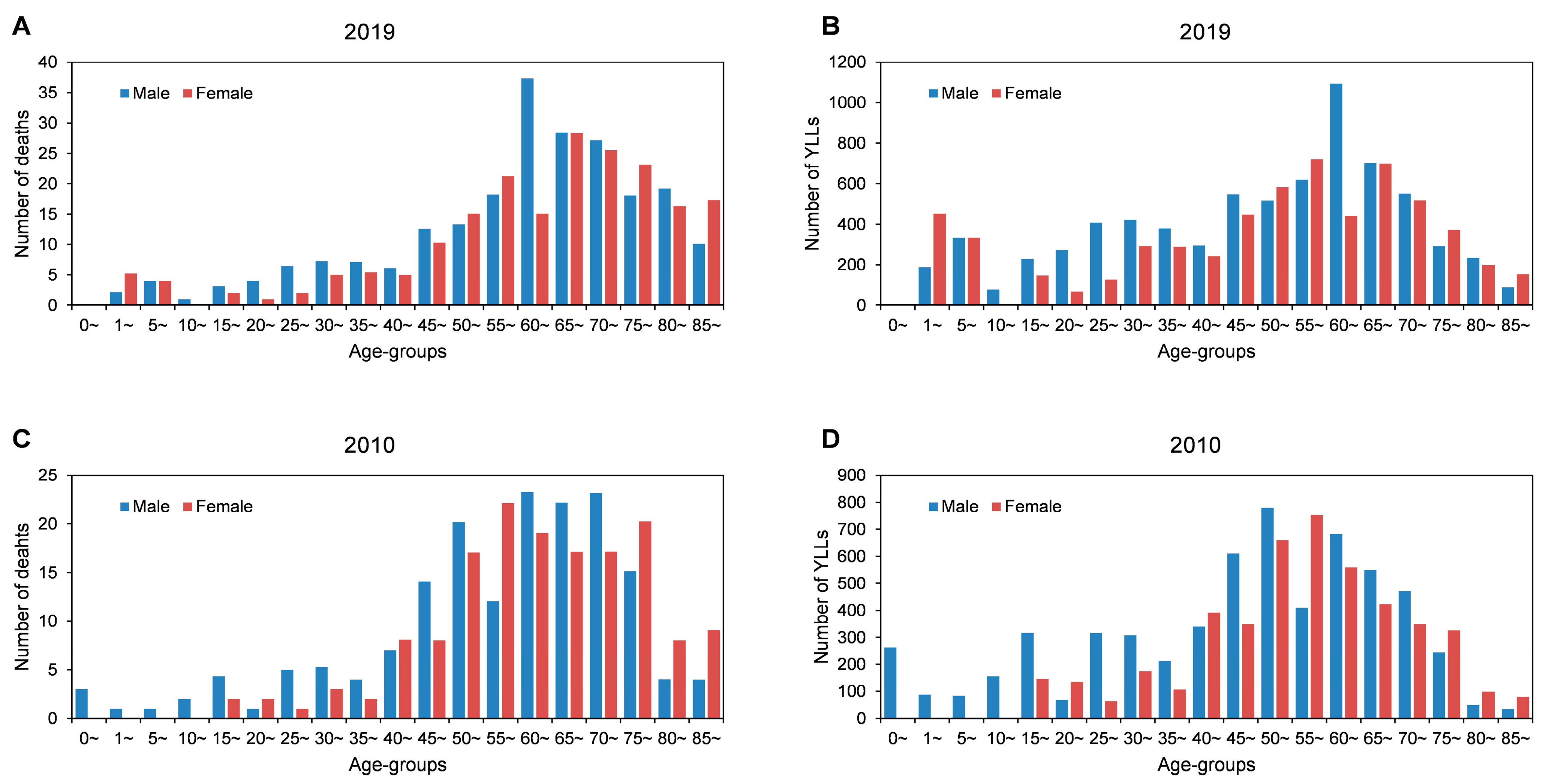
3.2. Age and Gender Distribution of CNS Cancer Burden
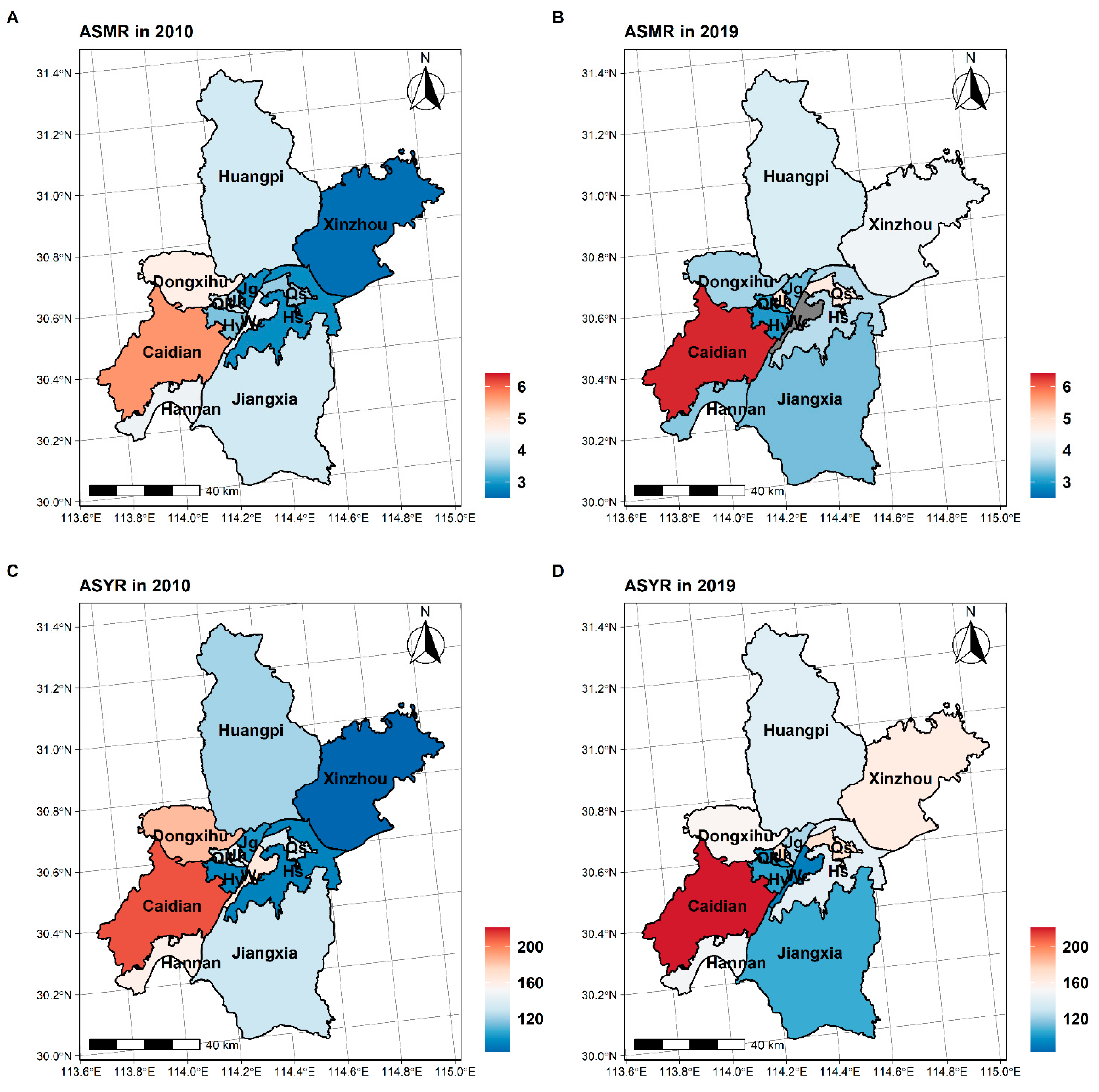
3.3. Spatial Distribution of CNS Cancer Burden
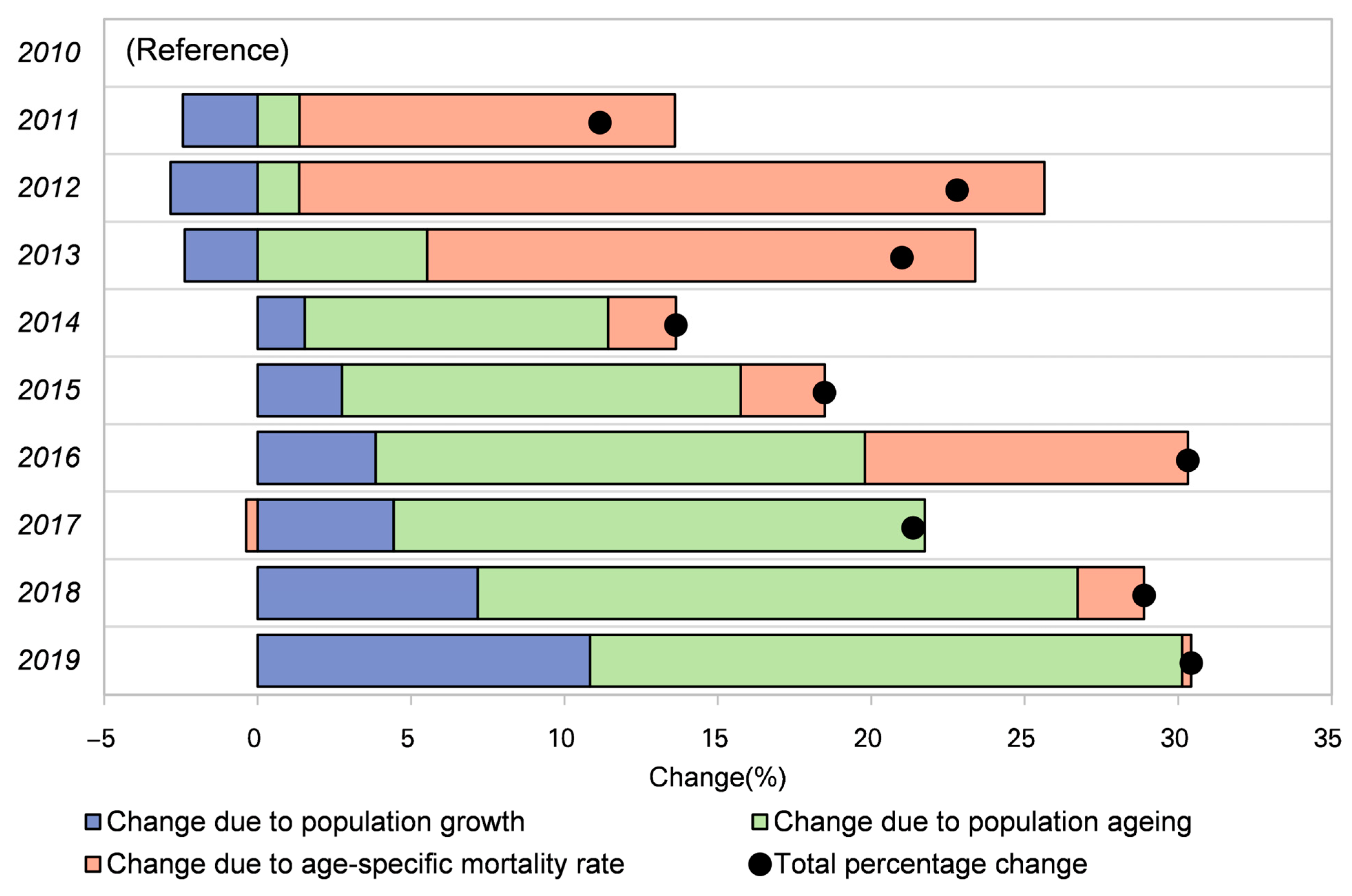
3.4. Decomposition Analysis of Change in Mortality from 2010 to 2019
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Louis, D.N.; Perry, A.; Wesseling, P.; Brat, D.J.; Cree, I.A.; Figarella-Branger, D.; Hawkins, C.; Ng, H.K.; Pfister, S.M.; Reifenberger, G.; et al. The 2021 WHO Classification of Tumors of the Central Nervous System: A summary. Neuro Oncol. 2021, 23, 1231–1251. [Google Scholar] [CrossRef]
- Global Burden of Disease 2019 Cancer Collaboration; Kocarnik, J.M.; Compton, K.; Dean, F.E.; Fu, W.; Gaw, B.L.; Harvey, J.D.; Henrikson, H.J.; Lu, D.; Pennini, A.; et al. Cancer Incidence, Mortality, Years of Life Lost, Years Lived with Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019. JAMA Oncol. 2022, 8, 420. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer Statistics, 2021. CA Cancer J. Clin. 2021, 71, 7–33, Erratum in CA Cancer J. Clin. 2021, 71, 359. [Google Scholar] [CrossRef]
- Allemani, C.; Matsuda, T.; Di Carlo, V.; Harewood, R.; Matz, M.; Nikšić, M.; Bonaventure, A.; Valkov, M.; Johnson, C.J.; Estève, J.; et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 2018, 391, 1023–1075. [Google Scholar] [CrossRef]
- Gupta, T.; Achari, R.; Chatterjee, A.; Chen, Z.-P.; Mehta, M.; Bouffet, E.; Jalali, R. Comparison of Epidemiology and Outcomes in Neuro-Oncology Between the East and the West: Challenges and Opportunities. Clin. Oncol. 2019, 31, 539–548. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.; Cao, S.; Xu, R. Cancer incidence, mortality, and burden in China: A time-trend analysis and comparison with the United States and United Kingdom based on the global epidemiological data released in 2020. Cancer Commun. 2021, 41, 1037–1048. [Google Scholar] [CrossRef]
- Cao, M.; Li, H.; Sun, D.; Chen, W. Cancer burden of major cancers in China: A need for sustainable actions. Cancer Commun. 2020, 40, 205–210. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- de Robles, P.; Fiest, K.M.; Frolkis, A.D.; Pringsheim, T.; Atta, C.; Germaine-Smith, C.S.; Day, L.; Lam, D.; Jette, N. The worldwide incidence and prevalence of primary brain tumors: A systematic review and meta-analysis. Neuro Oncol. 2014, 17, 776–783. [Google Scholar] [CrossRef]
- Guo, K.; Yin, P.; Wang, L.; Ji, Y.; Li, Q.; Bishai, D.; Liu, S.; Liu, Y.; Astell-Burt, T.; Feng, X.; et al. Propensity score weighting for addressing under-reporting in mortality surveillance: A proof-of-concept study using the nationally representative mortality data in China. Popul. Health Metrics 2015, 13, 16. [Google Scholar] [CrossRef]
- Macken, C.A. The life table and its applications. Math. Biosci. 1986, 82, 235–236. [Google Scholar] [CrossRef]
- Sun, L.; Zhou, Y.; Zhang, M.; Li, C.; Qu, M.; Cai, Q.; Meng, J.; Fan, H.; Zhao, Y.; Hu, D. Association of Major Chronic Noncommunicable Diseases and Life Expectancy in China, 2019. Healthcare 2022, 10, 296. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Dwyer-Lindgren, L.; Lofgren, K.T.; Rajaratnam, J.K.; Marcus, J.R.; Levin-Rector, A.; E Levitz, C.; Lopez, A.D.; Murray, C.J. Age-specific and sex-specific mortality in 187 countries, 1970–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2071–2094. [Google Scholar] [CrossRef]
- GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1459–1544. [Google Scholar] [CrossRef]
- Roth, G.A.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- Gupta, P.D. Standardization and Decomposition of Rates: A User’s Manual; US Department of Commerce, Economics and Statistics Administration, Bureau: Washington, DC, USA, 1993.
- Yin, P.; Brauer, M.; Cohen, A.J.; Wang, H.; Li, J.; Burnett, R.T.; Stanaway, J.D.; Causey, K.; Larson, S.; Godwin, W.; et al. The effect of air pollution on deaths, disease burden, and life expectancy across China and its provinces, 1990–2017: An analysis for the Global Burden of Disease Study 2017. Lancet Planet. Health 2020, 4, e386–e398. [Google Scholar] [CrossRef]
- GBD 2016 Lower Respiratory Infections Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect. Dis. 2018, 18, 1191–1210. [Google Scholar] [CrossRef]
- Wang, W.; Yin, P.; Wang, L.J.; Liu, Y.N.; Liu, J.M.; Qi, J.L.; You, J.L.; Lin, L.; Zhou, M.G. Analysis on all-cause mortality rate and life expectancy in China 2005–2018. Zhonghua liu Xing Bing xue za zhi = Zhonghua Liuxingbingxue Zazhi 2021, 42, 1420–1428. [Google Scholar] [CrossRef]
- Hou, X.; Song, Z.; Zhang, F.; Liu, Z.; Long, W.; Long, Z.; Zhou, M.; Wang, E.; Yin, P.; Zhu, M. Burden of brain and other central nervous system cancer in China, 1990–2019: A systematic analysis of observational data from the global burden of disease study 2019. BMJ Open 2022, 12, e059699. [Google Scholar] [CrossRef]
- Li, C.-Y.; Ye, Y.-C.; Liang, G.-Y.; Zhang, W.-H.; Zhang, Z.-Y.; Liu, X.-Q.; Liang, Y.; Xu, F.-L.; Li, J.; Xiang, J.-L. Cancer Incidence and Mortality Survey in Wuwei, Gansu Province, Northwestern China from 2003 to 2012. Chin. Med. J. 2016, 129, 636–644. [Google Scholar] [CrossRef]
- He, Y.; Liang, D.; Li, D.; Shi, J.; Jin, J.; Zhai, J.; Wen, D.; Shan, B. Cancer incidence and mortality in Hebei province, 2013. Medicine 2017, 96, e7293. [Google Scholar] [CrossRef] [PubMed]
- Khanolkar, A.R.; Ljung, R.; Talbäck, M.; Brooke, H.L.; Carlsson, S.; Mathiesen, T.; Feychting, M. Socioeconomic position and the risk of brain tumour: A Swedish national population-based cohort study. J. Epidemiol. Community Health 2016, 70, 1222–1228. [Google Scholar] [CrossRef] [PubMed]
- Cote, D.J.; Ostrom, Q.T.; Ms, H.G.; Duncan, K.R.; Crevecoeur, T.S.; Kruchko, C.; Smith, T.R.; Stampfer, M.J.; Barnholtz-Sloan, J.S. Glioma incidence and survival variations by county-level socioeconomic measures. Cancer 2019, 125, 3390–3400. [Google Scholar] [CrossRef]
- Ostrom, Q.T.; Cioffi, G.; Waite, K.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2014–2018. Neuro Oncol. 2021, 23, iii1–iii105. [Google Scholar] [CrossRef]
- Le Rhun, E.; Weller, M. Sex-specific aspects of epidemiology, molecular genetics and outcome: Primary brain tumours. ESMO Open 2020, 5, e001034. [Google Scholar] [CrossRef]
- Costa, A.R.; de Oliveira, M.L.; Cruz, I.; Gonçalves, I.; Cascalheira, J.; Santos, C.R. The Sex Bias of Cancer. Trends Endocrinol. Metab. 2020, 31, 785–799. [Google Scholar] [CrossRef]
- Johnson, K.J.; Cullen, J.; Barnholtz-Sloan, J.S.; Ostrom, Q.T.; Langer, C.E.; Turner, M.C.; McKean-Cowdin, R.; Fisher, J.L.; Lupo, P.J.; Partap, S.; et al. Childhood Brain Tumor Epidemiology: A Brain Tumor Epidemiology Consortium Review. Cancer Epidemiol. Biomark. Prev. 2014, 23, 2716–2736. [Google Scholar] [CrossRef] [PubMed]
- Kaderali, Z.; Lamberti-Pasculli, M.; Rutka, J.T. The changing epidemiology of paediatric brain tumours: A review from the Hospital for Sick Children. Child’s Nerv. Syst. 2008, 25, 787–793. [Google Scholar] [CrossRef]
- McNeill, K.A. Epidemiology of Brain Tumors. Neurol. Clin. 2016, 34, 981–998. [Google Scholar] [CrossRef]
- Morgan, L.L. The epidemiology of glioma in adults: A “state of the science” review. Neuro Oncol. 2015, 17, 623–624. [Google Scholar] [CrossRef]
- National Bureau of Statistics China Statistical Yearbook (Online Version), 1999–2022. Available online: http://www.stats.gov.cn/tjsj/ndsj/ (accessed on 21 September 2022).
- Patel, A.P.; Fisher, J.L.; Nichols, E.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; Abraha, H.N.; Agius, D.; Alahdab, F.; Alam, T.; et al. Global, regional, and national burden of brain and other CNS cancer, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 376–393. [Google Scholar] [CrossRef]
- Dicker, D. GBD 2017 Mortality Collaborators Global, regional, and national age-sex-specific mortality and life expectancy, 1950-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1684–1735. [Google Scholar] [CrossRef]
- Ostrom, Q.T.; Francis, S.S.; Barnholtz-Sloan, J.S. Epidemiology of Brain and Other CNS Tumors. Curr. Neurol. Neurosci. Rep. 2021, 21, 1–12. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, J.; Liu, Y.; Wen, H.; Yan, Y.; Yang, N.; Guo, Y.; Dai, J.; Yu, C. Mortality and Years of Life Lost Due to Brain and Other Central Nervous System Cancer in Wuhan, China, from 2010 to 2019. Int. J. Environ. Res. Public Health 2023, 20, 3544. https://doi.org/10.3390/ijerph20043544
Chen J, Liu Y, Wen H, Yan Y, Yang N, Guo Y, Dai J, Yu C. Mortality and Years of Life Lost Due to Brain and Other Central Nervous System Cancer in Wuhan, China, from 2010 to 2019. International Journal of Environmental Research and Public Health. 2023; 20(4):3544. https://doi.org/10.3390/ijerph20043544
Chicago/Turabian StyleChen, Jiahao, Yan Liu, Haoyu Wen, Yaqiong Yan, Niannian Yang, Yan Guo, Juan Dai, and Chuanhua Yu. 2023. "Mortality and Years of Life Lost Due to Brain and Other Central Nervous System Cancer in Wuhan, China, from 2010 to 2019" International Journal of Environmental Research and Public Health 20, no. 4: 3544. https://doi.org/10.3390/ijerph20043544
APA StyleChen, J., Liu, Y., Wen, H., Yan, Y., Yang, N., Guo, Y., Dai, J., & Yu, C. (2023). Mortality and Years of Life Lost Due to Brain and Other Central Nervous System Cancer in Wuhan, China, from 2010 to 2019. International Journal of Environmental Research and Public Health, 20(4), 3544. https://doi.org/10.3390/ijerph20043544







