Abstract
There is an increasing motivation to implement pharmacist-led screening services in community pharmacies. This study aims to develop tools to support the pharmacist in the context of a diabetes and cardiovascular disease risk assessment service. Our development involved a multistep process using a user-centred approach, including a need assessment phase (14 patients, 17 pharmacists) and a creative design phase, followed by the evaluation of the materials (10 patients, 16 pharmacists). Three following themes covering educational needs emerged from stakeholders’ discussions: “content”, “layout”, and “form”, with three additional themes regarding the practical organisation: “software”, “awareness”, and “referral”. Based on the need assessment, tools for patient education purposes and awareness campaigns were created. During the development, special attention was paid to the writing style and structure with less text and more graphical colourful elements to suit patients with different health literacy and educational levels. The evaluation phase allowed researchers to observe participants engaging with the materials. Overall, participants were satisfied with the tools. The contents were considered valuable and relevant. However, adaptations were necessary to ensure their understanding and long-term usability. Finally, future research is required to evaluate the materials’ impact on patients’ behaviour towards their identified risk factors and ensure their effectiveness.
1. Introduction
Worldwide, healthcare systems are challenged with the rising rates of non-communicable chronic diseases (NCDs), such as diabetes and cardiovascular diseases, due to the ageing of the population, poor lifestyle behaviour and environmental factors. Their economic burden is projected to intensify in the future with devastating, long-term economic consequences for individuals and their households due to increased disabilities and premature death while being associated with heightened demand and expenditure of healthcare services and treatment [1]. This growing clinical and socio-economic burden greatly impacts people’s quality of life and consequently represents a significant challenge for optimal healthcare provision [2]. To lessen their impact, health systems need both individual and collective approaches that focus on reducing the modifiable risks associated with these diseases. Preventive strategies, such as early screening and chronic disease management services can help encourage individuals to take the actions necessary to achieve their healthcare goals. In that regard, health promotion, both to patients with or at risk of chronic diseases, in the form of tailored patient education, positively impacts the patient’s knowledge and understanding of the risks involved with their health status [3]. As such, community pharmacists, by their high accessibility, long opening hours, and the provision of pharmaceutical care without an appointment, are ideally placed for these services [4].
Recently, there has been increased interest in broadening the role of community pharmacists beyond the traditional medication dispenser to progressively shift to a provider of services and information [5,6]. Moreover, the increasing healthcare demands have led pharmacists to undertake more advanced clinical roles targeted to improve health outcomes, such as medication reviews, immunisations, health promotion, and patient education through patient and collaborative care [5,6]. Several systematic reviews have reported the positive impact of pharmacist interventions on patients’ therapeutic, safety and humanistic outcomes among different conditions, such as hypertension and diabetes mellitus [7,8,9,10]. These interventions usually involved medication review, education concerning health promotion, diseases and medication understanding, and specific risk reduction activities. Outcomes included a significantly improved quality of life, reduced disease risk, and premature mortality [7,8,9,10]. Therefore, pharmacists must now learn and possess specific knowledge and skill competencies to align with their new role of service provider along with other healthcare practitioners through collaborative practice.
In Belgium, the role of pharmacists is evolving more slowly, compared to their neighbouring countries despite an intrinsic motivation to play a more active role in primary care, chronic disease management and health promotion. Moreover, even if there is increasing research demonstrating the impact of pharmacist-led preventive services worldwide [11], evidence on how to provide a risk evaluation in community pharmacies is still limited. With that purpose, the Association of Pharmacists in Belgium (APB) conducted a six-month pilot project among a sample of pharmacies in the Brussels capital region. To facilitate the implementation and conduct of the pilot project, two universities collaborated to evaluate the feasibility of offering diabetes and cardiovascular disease screening services in community pharmacies. An implementation study was conducted to identify the contextual factors facilitating or hindering a successful implementation within community pharmacies and to explore the experiences of pharmacists and patients. Overall, the service was perceived as easy to perform and feasible in practice but will require external and financial support to guarantee its effectiveness and a sustainable, successful implementation [12].
Evidence shows that more vulnerable groups, such as the elderly and patients with chronic diseases, are most at risk of having insufficient health literacy while being the ones with the greatest healthcare needs and expenses [13,14]. Delivering services, such as a risk assessment, was an excellent opportunity for pharmacists to initiate a dialogue with their patients on their health and provide support in the management of their risk factors. Therefore, alongside the implementation study, the research team developed material and tools to support pharmacists in implementing the project and help them in counselling their patients, especially patients with limited health literacy. This paper aims to present an overview of the multistep process, using a user-centred approach, to design and develop tools for a diabetes and cardiovascular disease risk assessment service in community pharmacies.
2. Materials and Methods
2.1. Study Design
The development procedure was inspired by the basic steps for developing health education tools using a user-centred approach [11,12]. The development of the materials involved a multistep process, including a need assessment phase involving a literature review and discussions with stakeholders, and a creative design phase followed by the evaluation of the materials created. Figure 1 illustrates the different stages of the development process.
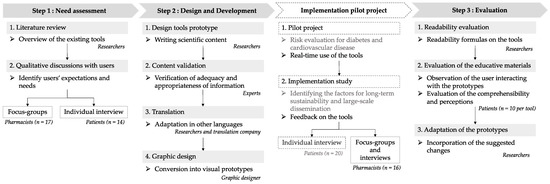
Figure 1.
Overview of the different stages of the development and design process. Notes: Descriptive details on the methodology of the risk assessment project and the results of the implementation study (dotted lines in the graph) are presented in a separate article [12].
2.2. Need Assessment Phase
Initially, an assessment was undertaken to identify the needs of patients and pharmacists in the context of a risk evaluation in community pharmacies. First, a literature review and web research on the different tools regarding screening for diabetes and cardiovascular diseases were conducted. We intended to obtain information on the content, layout and variability of materials, questionnaires and tools to perform screening, or deliver patient education for the targeted diseases. Secondly, qualitative discussions with pharmacists and patients were organised to explore and expand on their needs by discussing the possible implementation of a risk evaluation service in community pharmacies and generating ideas using existing tools as a starting point.
Semi-structured focus groups were organised with pharmacists. Two methods were used for the recruitment. The researchers sent an email to pharmacists who are involved in internships with pharmacy students and the local pharmacists’ organisations to their members. To boost recruitment, researchers also delivered handouts in community pharmacies. During the focus groups, participants received a bundle of folders, existing tools and games illustrating possible topics and modes of presentation to elicit concrete opinions about content, layout, and usability. Following a joint discussion, participants prioritised the tools according to their preferences and needs.
Additionally, semi-structured individual phone interviews with patients were also carried out. Patients were recruited through an online post on a Facebook group and the patient’s community of a general practitioner via a WhatsApp group. The semi-structured interviews were conducted in French or Dutch, according to the patient’s preference, discussing their perception of the risk evaluation service and how they would like to receive counselling. Pharmacists and patients were eligible to participate if they were respectively practising and residing in the Brussels capital region and were able to speak, read, and understand French or Dutch. Patients also had to meet the inclusion criteria of the risk assessment pilot project (aged between 25–65 years old with no history of diabetes, cardiovascular or renal diseases). Data were collected from February to May 2020 until saturation, meaning no new information was collected during the last focus group and the last two interviews.
Semi-structured interviews and focus groups were audio recorded, transcribed ad-verbatim, and analysed using thematic analysis. Pharmacists’ and patients’ transcriptions were coded separately. Three researchers conducted the analysis and discussed every couple of interviews to converge nodes into an iterative coding tree and to ensure agreement on the conclusions. The data analysis was organised and managed using QSR International’s NVivo software 12 [15].
2.3. Creative Design and Development
Subsequently to the focus groups and interviews, the different tools and content to be created were defined. Considering the project resources before the launch of a pilot project simulating the risk evaluation in a sample of community pharmacies in the Brussels capital region, tools were selected to be developed into prototypes to answer the needs of pharmacists and patients.
Preliminary drafts were prepared in English for every tool and adjusted by experts for scientific validation. The drafts were translated into Dutch and French by the researchers. To validate the translation, a sample of 2 × 3 native speakers verified the language and grammatical correctness of the written text. The drafts were then sent to a translation company for an Arabic translation, as requested for additional language during the stakeholders’ discussions. Hereafter, they were adapted to designed prototypes by a graphic designer. In that way, the textual manuscripts were converted into visual prototypes. Additionally, a software developer from the Association of Pharmacists Belgium produced and designed a web tool to guide pharmacists during the risk evaluation.
2.4. Evaluation
In order to evaluate the acceptability and usability of the different tools, the creative design phase was followed by an implementation phase of the prototypes. The tools were printed, distributed, and used during the six months risk assessment pilot project within the community pharmacies. During the implementation study, semi-structured focus groups and face-to-face interviews with 16 participating pharmacists were organised to discuss the conduct of the project, including the use of the different tools by the pharmacists.
In addition to the implementation phase, the understanding and perception of the patient’s education materials were evaluated. Firstly, the readability index (RI), related to the level of schooling necessary to understand a given text, was assessed by the researchers using readability formulas on the French documents: the Simple Measure Of Gobbledygook (SMOG) [16], the Flesch–Kincaid grade level (FKGL) [17], the Coleman–Liau index (CLI) [18] and the FOG index. However, research shows that statistical tests of readability alone do not seem to be sufficient to ensure that information is understood [19]. Thereby, the understanding of the educational materials and the presentation of the information was evaluated with participants representative of the population targeted by the documents. Face-to-face interviews were conducted observing the users interacting with the prototypes. The interviews followed a semi-structured individual interview guide inspired by European Commission guidelines for the readability of the labels of medicines [20], the Gibson et al. questionnaire for the health education database [21] and the patient education materials assessment tool [22]. Questionnaires can be consulted in the Supplementary Materials. The interview covered the general impression of the materials, user perception, comprehensibility of the contents, reader-friendliness, layout/design, length, and amount of illustrations.
All of the interviews were audio-recorded and transcribed ad verbatim. Pharmacists’ and patients’ transcriptions were coded separately and analysed to identify positive and negative perceptions, leading to adjustments.
3. Results
3.1. Need Assessment
There is considerable variability in the content and quality of diabetes and cardiovascular disease patient education materials [23,24]. Studies have shown that patient education material on diabetes and cardiovascular disease prevention should feature different themes, including basic knowledge of the diseases, their complications, self-monitoring, medication taking, and how to manage risk factors through healthy eating and physical activity [25,26]. However, studies have yet to define the ideal characteristics of a comprehensive patient education program in clinical practice [27].
During our qualitative study, three focus groups were conducted with 17 pharmacists, and 14 phone interviews were conducted with patients. Three themes covering educational needs emerged from the analysis of patients’ interviews and pharmacists’ focus groups: “content”, “layout”, and “form”. In addition, an additional theme regarding “training” emerged from the pharmacists’ focus groups. Details on the themes derived from the analysis and illustrative quotes can be found in Appendix A.
In general, patients and pharmacists agreed that information should address explanations of diabetes and cardiovascular diseases, their complications, their associated risk factors and lifestyle advice on preventing them. All groups found that the delivery of patient education was of utmost importance and should be individualised with concrete reachable objectives on a voluntary basis without being guilt-inducing. In that regard, training in motivational techniques was mentioned during the focus groups to help the patient achieve their goals, besides training in nutrition and multidisciplinary collaboration. Verbal explanation and counselling should be associated with visual aid and educative materials that the patients can take back home. Different layout possibilities were discussed. All agreed that educational material should be well-structured, reader-friendly and not too long. A popular recommendation was to use less text and more graphical and colourful elements.
Three additional themes emerged covering the practical organisation of the risk evaluation: “software”, “awareness”, and “referral”. Patients and pharmacists agreed that eye-catching awareness campaigns, including a set of items (e.g., flyers, animation videos, posters, etc.), should be developed to inform the target population of the possibility of being screened in community pharmacies. Additionally, developing software to record patients’ data for follow-up and to keep a schedule of appointments was also advised to facilitate the conduct of the risk evaluation. Finally, how to refer high-risk patients for a medical follow-up was discussed with pharmacists and patients. Even if the transfer of patients’ outcomes of the risk evaluation through an online platform to the general practitioners was preferred by pharmacists, mixed opinions were reported by the patients with a preference for a printout of their results.
3.2. Creative Design Phase and Development
Following the discussions with patients and pharmacists, we created a set of tools based on the assessed needs and project resources. Firstly, patient education materials were developed, including folders, a flip-over album, and a lifestyle advice booklet. The overview of the content of the patient education materials can be seen in Table 1.

Table 1.
Topics covered in the patient education materials.
The flip-over album was a patient education support intended to be displayed on the pharmacist’s counter and used as a visual aid to the pharmacist’s verbal counselling. On one side of the album, the patient could look at graphs, images, and pictograms to support the spoken words of the pharmacist, while the latter could look at the other side, which presented textual key information to be delivered. Two other documents to take back home to help patients who may benefit from written material were created. Folders were aimed to be distributed to patients with an identified risk of developing diabetes or cardiovascular diseases but contained only specific information focusing on the targeted diseases. However, a patient lifestyle booklet centred on a healthy lifestyle rather than disease management could be given to any patient. The booklet was divided into four following chapters with concrete pieces of advice on: “healthy eating”, “healthy body”, and “healthy mind” associated with a calendar to motivate patients to implement new healthy habits into their life.
During the development of the materials, special attention was paid to the writing style, trying to shorten words, substituting medical jargon for general terms, and using clear, direct, positive, personal, and conversational writing when possible. The active voice was also used to keep the text shorter and make it easier to read. Similarly, the design was carefully thought through using style and size of print that can influence the readability, colours, heading and bold writing to emphasise the important information.
In addition to the educative materials, a set of visibility tools was created to increase awareness of the risk evaluation program within the community pharmacies. To that purpose, flyers, posters, counter mats, and written questionnaires were delivered to pharmacists in two to four languages of their choice to put up and distribute according to their preferences. A handout to inform other practitioners on the purpose of the evaluation and write patients’ risk assessment results was developed. Finally, the Association of Belgian Pharmacies developed a web tool, available to the participating pharmacists exclusively online, to guide pharmacists through the risk evaluation questions, enter patients’ answers, and determine the assessed risk outcome for the targeted diseases. An electronic version of the educative materials and handout with their result could also be transferred by email at the patients’ request.
3.3. Evaluation
The readability tests, performed by the researchers, resulted in high variability in scores depending on the tests. None of our three patient education tools received a readability score between 7 and 8, as recommended by the National Institutes of Health (Figure 2). The folder on cardiovascular disease received the highest score throughout the tests, which means it would require a higher level of education to be easily read and thus is less accessible to the targeted population.
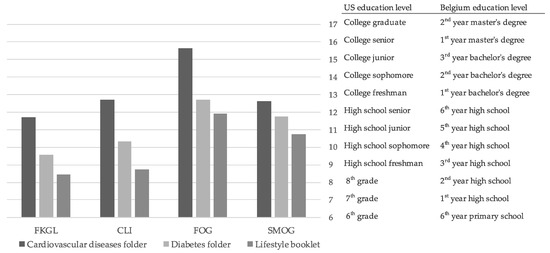
Figure 2.
Readability evaluation of materials.
However, since the readability tests are developed for the English language, they were used as tools for information and were supplemented with an evaluation of the understanding of the target population, as recommended by the French National Authority for Health (HAS) [19]. Therefore, semi-structured interviews were conducted with 10 participants per material during the evaluation phase, which allowed us to identify misunderstood words and sentences, and adjust in consequences. An overview of participants’ characteristics can be seen in Table 2. An overview of the responses to the closed questions to the evaluation questionnaire can be found in Appendix B.

Table 2.
Overview of the participants’ characteristics.
Participants had an overall positive impression of the educative materials, and the contents were considered useful and relevant. In particular, the illustrations of the diseases and risk factors were perceived as important information for laypeople and help participants in their understanding of the diseases. Patients appreciated the right balance between texts, illustrations, and moderate length, which was considered reader-friendly and thus maintained their eagerness to read. Moreover, the participants appreciated the reassuring and caring tone of the booklet. Suitable amounts of information were presented, and the contents were generally regarded as easy to understand and advice feasible in practice. Participants reported learning new information (e.g., nutriscore, nutrition advice) and ideas (e.g., new way to stay active, to manage stress) they could implement in their daily life.
The evaluation phase allowed researchers to observe how users read and manipulate the material. Thereby, they observed that the topics in the folders were not read in the order it was intended, which led to a reorganisation of the layout topics. This step also offered suggestions for modifications and improvements. Some issues focused on readability (minor adjustments in colours and font size), variability of representation (e.g., diversity in age groups or ethnicity) and minor adjustments in graphs and illustrations to improve understanding.
In addition, four focus groups and three face-to-face interviews with 16 pharmacists were organised to discuss the use of the tools during the risk assessment pilot project. An overview of pharmacists’ characteristics can be seen in Table 3.

Table 3.
Overview of the pharmacists’ characteristics.
Pharmacists appreciated the flip-over album as text-heavy presentations were avoided, and illustrations were considered valuable to explain complex conditions, such as diabetes. They were satisfied with the graphics and the layout, which were described as colourful and attractive. Pharmacists reported using the album during nearly every patient risk evaluation, but they often considered the album too long for personal use. Not every page was presented to the patients. However, the variability of use greatly depended on patient profiles and pharmacists, which made it difficult to reduce the number of pages significantly. To bypass this matter, a tab system to directly access specific pages to navigate more easily or removable pages to rearrange according to preferences was advised.
Visibility materials reportedly generated curiosity among some patients, which helped promote awareness of the project alongside the active recruitment approach by the pharmacists and could help reach more patients that would benefit from the risk evaluation.
Finally, the web tool helped the conduct of the risk evaluation and was greatly appreciated by the pharmacists as it allowed pharmacists to navigate through the risk evaluation questions and enter answers easily. Using a web tool was also perceived as efficient to optimise their time on counselling. Minor technical issues were reported. Other adjustments were discussed (e.g., adding a scheduling tool) with the APB and implemented if possible.
4. Discussion
This research complements a first study in Belgium examining the feasibility of offering a risk-assessment service for diabetes and cardiovascular diseases in community pharmacies and the factors influencing its implementation. Descriptive details on the methodology of the risk assessment, results of the implementation study and its feasibility in practice were reported by Rondeaux et al. [12]. Our present study aimed to develop materials to support pharmacists in their new role of providing a risk assessment service to their patients. Research has emphasised the importance of involving patients and stakeholders in the development of patient education aids to ensure their acceptability and avoid the need for future redesigns [29,30]. We have developed a set of tools taking into consideration the desirable characteristics of patient education materials [22] that can be used permanently and on a larger scale by incorporating users’ involvement through a multi-step process.
First, the literature for patient education on diabetes and cardiovascular diseases was explored. Secondly, we assessed the needs of pharmacists and patients and then developed a set of tools. Overall, the topics included in our material aligned with previous studies examining the educational needs and preferences of patients with diabetes and cardiovascular diseases [25,26]. However, they were limited to prevention purposes and did not include disease management topics as they did not correspond to the purpose of a screening service. Different items were created to fit the variability of the patient’s profile according to the determined risk.
A major Danish study of health literacy revealed that people with chronic conditions had more difficulty understanding health information and engaging with healthcare providers than the general population [31]. Furthermore, people with low levels of education had lower health literacy than people with high levels of education [31]. We intended to develop materials that would provide education to patients with different needs, health literacy levels, and learning abilities. Thus, special attention was given to shortening words, substituting jargon for general terms, illustrating complex concepts with well-designed pictures, and using a large font with headings and emphasis on important information, as recommended by other research and guidelines [32,33]. A previous study focusing on low literacy patient education material suggested evaluating the different prototypes with participants, which proved to be valuable in our research [34]. In the lifestyle booklet, the participants found the contents easy to understand, the amount of information useful, and acknowledged the right balance between text and illustrations to maintain attention and eagerness to read. However, minor changes were necessary to improve socio-cultural representations and understanding of graphs. Observing participants manipulate and read the folders during the evaluation allowed the researchers to understand their reading process and reorganise the topics in the intended reading order. The layout album was reported as a valuable visual aid to support pharmacists’ counselling. This format aligns with the evidence that people learn more deeply by combining words and pictures than by words alone [35]. However, if the content did not need any revision, adaptations to the format were necessary to facilitate its use.
The materials were designed with the intent to raise awareness of the risk factors and lead patients toward healthier behaviours. Pharmacists’ material was focused on teaching basic knowledge of the targeted diseases, while the patient’s materials focused more on practical strategies for behaviour changes. Short-term, easily implementable steps to work toward achieving long-term goals may offer daily incentives to change. Thus, a brief intervention based on social cognitive theory to teach patients how to develop their action plans could help them to create their own short-term goals for sustained behaviour change [36].
Moreover, pharmacists have shared that training in motivational interviewing could be beneficial to delivering patient education in the context of the screening service. Motivational interviewing is a collaborative, patient-centred communication skill that can facilitate behaviour change by stimulating a patient’s internal motivation [37]. Pharmacist-led motivational interviewing has been shown to be beneficial to patients’ adherence [38,39,40]. In a systematic review and meta-analysis of motivational interviewing in healthcare settings, 64% of the studies showed an effect of using motivational techniques even in brief encounters of 15 min. Nonetheless, more than one encounter with the patient seemed to ensure the effectiveness of motivational interviewing [41]. It is evident that all of the information on diabetes and cardiovascular diseases cannot be delivered during only one session. Pharmacists have shared that multiple sessions could help increase and motivate patients’ adherence to their short-term goals. Therefore, an education program could potentially be scheduled to address all of the issues specific to a patient, even if some topics would be discussed at every meeting while others less frequently.
Furthermore, if the education materials were developed in the context of screening in community pharmacies, the content was not specific to the setting. As such, the designed materials could be used and distributed in other clinical settings by other healthcare practitioners. The education could then involve different practitioners (e.g., medical practitioners, dieticians, tobacco cessation specialists, etc.) with specific abilities and experience to better care for the patient in a multidisciplinary approach.
Finally, this research included both French- and Dutch-speaking pharmacists and patients from the Brussels capital region. As such, the results reflect the perceptions and use of the tools in a metropolitan, densely populated area. Participation was also voluntary and thus may have included more highly motivated pharmacists and patients, making it, therefore not representative of all populations. Additional testing and research should be conducted in other regions and with a bigger sample of participants. Moreover, the materials were revised after carrying out the modifications from the evaluation phase. The latter was conducted in French with only an evaluation of the French materials. If commentary and suggestions relative to graphs, layouts, and pictures may be similar, additional evaluation should be conducted regarding understanding the materials in other languages. Furthermore, an assessment of the materials’ impact on patients’ behaviour in regard to the management of their risk factors was beyond the scope of this study. Following the distribution of the patient education materials, a formal assessment of knowledge improvement would gauge the success of communicating the intended information. It is also crucial to assess changes in self-efficacy, outcome expectations, and behaviour, as knowledge improvement is not always associated with improved health outcomes [42]. Thereby, further research is necessary to ensure their effectiveness. It is also essential to frequently revise the health education materials according to the latest scientific innovations and new knowledge in that field.
5. Conclusions
In Belgium, pharmacists could take up a more active role in identifying, screening, and counselling patients at risk of diabetes and cardiovascular diseases. Our study presented the development and design of materials to support pharmacists in this new role using a user-centred approach that can guide future development processes.
We developed different tools to fit the diverse needs and profiles of patients. First, a set of visibility materials to increase awareness of the risk evaluation. Secondly, patient education materials, such as a flip-over album with graphic illustrations to support the verbal counselling of the pharmacists, folders on the basic knowledge of cardiovascular diseases and diabetes and a booklet containing small reachable advice to help the patient implement healthier habits. Additionally, a web tool was developed by APB to guide the pharmacists through the multi-step risk evaluation. Overall, participants were satisfied with the tools created. The contents were perceived valuable and relevant in practice. However, future research is required to evaluate the materials’ impact on patients’ behaviour towards their identified risk factors and to ensure their effectiveness.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20042819/s1. Questionnaire A—Evaluationof the patient booklet. Questionnaire B—Evaluation of the folders.
Author Contributions
Conceptualization, S.R., T.B., M.B. and C.D.V.; methodology, S.R., T.B., M.B. and C.D.V.; formal analysis, S.R., T.B., M.B. and D.E.O.E.G.; investigation, S.R., T.B., M.B. and D.E.O.E.G.; writing—original draft preparation, S.R.; writing—review and editing, T.B., M.B., D.D. and C.D.V.; supervision, C.D.V.; project administration, C.D.V. and D.D.; funding acquisition, C.D.V. and D.D. All authors have read and agreed to the published version of the manuscript.
Funding
APB financed the risk-assessment pilot project with its own resources. The researchers designing and developing the materials were funded by Innoviris, a public organisation funding and supporting research and innovation in the Brussels capital region. This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Saint-Luc-UCL (Belgium) (B40321836258) The research was approved on 27 January 2020. An amendment was also submitted in May 2020, which was approved on 13 July 2020.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
We are very grateful to the local professional organisations and our sponsors, the Association of Pharmacists Belgium (APB), Citylabs, the medical laboratory of the Cliniques universitaires Saint-Luc, the Federation of Associations of the General Practitioners of Brussels (FAMGB), the Scientific Society of General Practitioners (SSMG), the Union of Brussels pharmacists (UPB) and the Professional Union of French-speaking Dietitians (UPDLF), for their expertise and support during the project and study. We would also like to thank Stephan Van den Broucke and Sandrine Roussel for their coordination and partnership with the Innoviris project. We greatly thank OhMedias! for their expertise and outstanding work on the design of the materials. Finally, we thank the Fonds Van Buuren and the Fondation Jaumotte Demoulin, which offered a grant to S.R. to finalise her research and thesis.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Themes emerging from the qualitative analysis of the patients’ interviews and pharmacists’ focus groups.
Table A1.
Themes emerging from the qualitative analysis of the patients’ interviews and pharmacists’ focus groups.
| Dimensions | Themes | Sub-Themes | Illustrative Quotes |
|---|---|---|---|
| Patient education | Content | Explanation of the targeted diseases, their complications and how to take action | PA1: “… that it explains very clearly what diabetes is. What its causes and consequences are.” PA2: “For every single test that they do, they explain why they do them and what the category of results would possibly mean... and that I should take further action.” PA6: “… information like “watch out for this and that and that”, I think that’s useful.” PA7: “My diet and my lifestyle, I think I’m in good control of that, but I can imagine that if that weren’t the case, I would need guidance.” PA9: “For diabetes, things like what foods to avoid, for example, things like that… Or foods to favour, maybe times to eat, times not to eat.” PA10: “If you have to change that at the dietary level, so certain types of food or certain packaging things to look out for. Certain food rations. I don’t know all that… So one folder on everything that’s physical activity, then another on everything related to food.” PA13: “I expect there to be a predetermined solution depending on the risk factor... let’s say a printout document that can tell you what you eat, what lifestyle to live to be able to reduce your risk factor. “In order for you to be at a low risk, you need to do this, this, this and that”... Just to give people some idea of what to do.” |
| Checklist of reachable objectives to individualise patient education | FA1: “… perhaps we could have a sort of summary sheet and possibly ask them to read it and come back afterwards with the objectives they would set themselves. For example, “Set yourself one or two goals in this list and come back to see me next time” … a dialogue would take place, and we could slowly try to get them to change their habits.” FA2: “Something like a little sheet to tick off, what we set ourselves as objectives for next week. Let’s say “Come on, next week you won’t put any more sugar in your coffee”… it’s not much, but it’s within people’s reach.” FA3: “There are apps too. Like they could look at what they have on their watch (number of steps) and we can work from there” PA10: “Very concrete things! So, if I’m at risk and there are things that need to be changed, he/she should explain them to me…” PA9: “Small goals so that people don’t get completely discouraged and think “well, it’s impossible to do that anyway.” | ||
| Score table can help patients to visualise how they can decrease their risk | FA12: “You need tools that create a trigger to start the dialogue. Very concrete. A score...” FA14: “I think the SCORE table is very precise because it’s like I said, not just at risk or not at risk, it’s a very precise risk.” | ||
| Food pyramid and glycemic index table | FA3: “You need blood sugar tables too, I think. I have glycemic tables that I suggest to patients, saying “look at what you can eat... rice, this kind and not that kind...” FA7: “For some people, it’s going to be useful to bring along the nutrition triangle, though… You also need to have suitable material for that.” | ||
| Recipes | FA3: “Ideas for dishes, meals, that could be interesting. We could be inspired by what the Belgian Diabetes Association proposes, which provides good information.” FA7: “What is also very nice is bringing their recipes. Let’s say a cake but make it sugar-free cake or something like that.” PA6: “I always like recipe books. Actually, that’s a cool idea, like, a recipe book or something like that.” | ||
| Layout | Materials with pictograms, colourful and easy to understand | FA1: “Some pictograms, say what they can act on.” FA3: “(About the emoticon tool) It’s visual, and it could be used as a tool for what we talked about regarding the objectives. Saying, “Look, this is the tobacco you decided on, you’ve reduced that much...” FA3: “… with fairly clear images, more with pictograms… possibly, a sheet a little more detailed with glycemic indexes or have detachable sheets, well.” FA7: “It’s up to us to give them something worthwhile... and understandable, clear. Not too complicated.” FA10: “It should be as visual as possible so that it can be understood in all languages.” FA12: “You have to go as simple as possible with them. This kind of questionnaire with the little drawings is very good.” PA2: “From the position of pharmacist, they can’t do much more than just provide neutral, objective information in an understandable way.” | |
| All-in-one: easy to access/classify within the pharmacy. | FA1: “I think we need something really all-in-one, to say “this is what you can do” about diabetes, about physical activity, about diet...” FA2: “You need all-in-one tools that are not too sophisticated... I did my dissertation in tobacco on the ready-to-use kit for the pharmacist, for the management of smoking cessation. There is a display, there is a CO-meter, there are appointment cards with your pharmacist, there are appointment cards with your tabacologues. It’s all-in-one, ready-to-use...” FA7: “(About a display tool) Here, the advantage is that you have a file, you know where it is. It’s practical... Because we have a lot of information, but as you say, you need to classify it.” | ||
| Written information | FA7: “I would have liked something to give to the patient. For education... we’re not going to measure them unnecessarily, so when the patient goes out, they should take a little tool with them. Whether it’s a brochure or...“ PA3: “… preferably something that you can take home and that you can talk to your pharmacist about as well.” PA9: “Maybe having it on a folder or something, certainly something I can go back to in case I forget what they said.” PA10: “Not only orally, but that there should be concrete documents to take at home…” PA11: “I read everything by e-mail. So I think that by e-mail, it’s easier than the leaflets.” | ||
| Digital game | FA3: “Have you ever thought of having apps? People are all on their mobile phones, with an application where we could use some images too.” FA8: “They are more familiar with health applications.” FA9: “This generation, they are better at using their smartphone.” FA15: “An easy site. Like you show a food. You just have to click on it. It’s good. It’s not good. We’re talking about the basics… in the form of a game.” | ||
| Form | Pharmacist needs to address the motivational aspects without inducing guilt. | FA2: “Whether it’s for diabetes or to stop smoking, it’s the same struggle, you have to change your lifestyle... It’s not pleasant. So that means that the interview should not at all be guilt-inducing.” FA3: “For smoking cessation, the first thing they say is something like that: “I’ve already stopped”. “But no, don’t worry, the average is at least 8 attempts. There’s no problem, you’ll get there” and then step by step...” FA15: “It must above all be done in a constructive atmosphere.” PA2: “I also think that should come from a position that really doesn’t come across as patronising. With everything that is known about prevention and healthy lifestyles, I think the main focus should be on nudging and guiding people towards healthier choices and giving them the feeling that this comes from an autonomous movement and not from patronising.” PA9: “Being nuanced… focusing on a healthy eating, healthier living, but not saying “here, you should do hours of sport” or “you should do this or never eat that again”. It seems unreachable.” | |
| Do not overflow them with too much information. | FA2: “Not to overload them with information, at first. As time goes by, it will settle down, and we can eventually do a more important interview, more relaxed.” PA10: “… with a jargon that is not accessible to the average person, so not 30 pages of literature. I’ll never look at that. You don’t need too much. Because if you have too much, you do nothing.” | ||
| Training | Training in motivational techniques | FA2: “It’s a pity, unfortunately, that training in motivational interviewing is still not included in the curriculum! Whatever care we want to have in all the chronic diseases, it’s the motivational interview that’s the key.” FA8: “Just talking about being overweight is difficult.” FA17: “I always find it difficult to get the message across to them that they should move and eat better.” PA15: “It also comes down to the delivery of that result. How the pharmacist delivers. If they just print out a paper to give to me and say, “you have diabetes”, I’m not going to take them seriously. There needs to be that engagement from the pharmacist.” | |
| Training in nutrition for diabetes | FA1: “In relation to diabetes, obviously in this case, something targeted at diabetes.” FA2: “I would say a dietician, who would give some (training).” FA3: “Eventually you need to be prepared too at the nutritional level because in terms of pre-diabetes it is indeed through diet that you act… It’s true that we haven’t been trained in nutrition.” | ||
| Multidisciplinary training by specialists | FA1: “What you can do is, for example, take a multidisciplinary team from a hospital that looks after diabetic patients, in a diabetes care pathway, and ask them to come… A team that is really aware of the management of diabetics.” | ||
| Practical organisation of the risk evaluation | Awareness | Promotional material to promote the risk evaluation: video fragments, floor mat, web application, leaflets, posters, etc. | FA6: “Short explanatory videos, on the screen for when they are waiting.” FA6: “Window stickers!” FA7: “So at your feet, come to your diabetes... Yes, I think that’s cool too so a floor sticker.” FA12: “A printed bag system for example. That could be quite good… You have to do flyers, bags, posters, etc. Maybe a kit to send out to the pharmacy and then everyone chooses what they want to use… A carpet on the floor could also be good idea.” FA14: “It’s a whole thing. You need flyers for those who can read. You have to talk to those who don’t. We have screens that show advertising.” PA3: “If there’s a poster up, you can recognise some of the characteristics of a disease that you might yourself suffer from...” PA4: “Something very noncommittal, that you can just give it to people. Putting up posters, leaflets, and if people have questions, they can take it with them and look at it at their leisure.” PA5: “It’s mainly mothers who go to the pharmacist. So, if you want to reach a whole family, I think leaflets might help.” PA6: “Some fragments on television, like “talk to your pharmacist about it”... but I think it’s important that you have a reminder in the pharmacy itself. Something that catches the eye and that says: “you can discuss it here with your pharmacist.” PA8: “A poster on the windows of my pharmacy saying: “Do you want to know if you are at risk of having diabetes?” for example. “Take 30 min with your pharmacist”. Well yes, then I would do it more easily anyway.” |
| Software | A software for schedule and follow-up | FA2: “The pharmacist must have a tool, an agenda. There are medical diaries, online like doctors have, with the confidentiality space that would eventually managed with slots.” FA3: “it would be worth having a dashboard to have an overview. Here are the patients I referred and here are the others who were borderline, whom I absolutely must follow up because they don’t need to be referred, but they’re still at a risk.” | |
| Referral | Referral to specialists who can focus on specific lifestyle habits | FA1: “I think that a partnership with doctors, with medical centers, with dieticians, with physiotherapists, I think it’s ideal because I believe that we need to be able to collaborate with other providers.” FA1: “You have to keep in mind that, you are part of a team that would allow you to be completed by all the care providers in the area. And that’s also important, it’s also to have a list of physiotherapists, dieticians, etc. in the neighbourhood.” FA12: “… or give us a list with the contact details of dieticians who practice in Brussels”. PA8: “I think that can go along the same lines at a GP’s...So actually you can suggest the same thing, or you’re even sent to a dietician.” | |
| Leaflet with the results stapled | FA2: “At one point we had a bone densitometry machine at the pharmacy, and we had made a little leaflet saying, here we are, what is osteoporosis, the 10 questions to ask your GP… it could just as well be diabetes.” FA3: “We’ll need a standard accompanying document.” FA7: “You have to have a document to show that you’ve looked at it, that you’ve done this with the patient and that you’ve discovered that there’s a moderate risk and that you’ve given the patient advice. And give this document to the patient so that he can pass it on to his doctor if he wants.” PA10: “I would still like to go and have the results in person, even only to have them myself. That’s important, and because I like to have control over the information that is circulated.” PA11: “I would prefer the pharmacist to write me a kind of little letter... a little summary of the analysis and he gives it to me and I pass it on to my doctor.” | ||
| Online platform | FA3: “For the (e-health) platform, it is still an additional task. PA6: “… via the pharmacist, which is an official channel, right? And nowadays there’s a lot more communication between pharmacists and doctors anyway.” PA7: “The first thing that comes to my mind is that there is such a platform with all the documents that the doctor needs, so e.g., the results of a fingerprick test. that would be a good option I think.” |
Appendix B

Table A2.
Results of the evaluation questionnaire regarding the perceptions on purpose, content, and layout of the patient education tools.
Table A2.
Results of the evaluation questionnaire regarding the perceptions on purpose, content, and layout of the patient education tools.
| Diabetes Folder | Cardiovascular Diseases Folder | Lifestyle Patient Booklet | Score a | |||||
|---|---|---|---|---|---|---|---|---|
| Mean Score by Item (n = 10) | Min | Max | ||||||
| Objectives | ||||||||
| At first glance, it attracted my attention | 28 | (70%) | 18 | (45%) | 37 | (93%) | 0 | 40 |
| It held my attention | 31 | (78%) | 34 | (85%) | 37 | (93%) | 0 | 40 |
| It is useful | 33 | (83%) | 32 | (80%) | 39 | (98%) | 0 | 40 |
| I would recommend it to a friend or relative to read | 32 | (80%) | 29 | (73%) | 35 | (88%) | 0 | 40 |
| Content | ||||||||
| I believe what is written | 38 | (95%) | 39 | (98%) | 37 | (93%) | 0 | 40 |
| What it says is important | 37 | (93%) | 38 | (95%) | 33 | (83%) | 0 | 40 |
| It reminds me of some things I need to think about | 33 | (83%) | 36 | (90%) | 37 | (93%) | 0 | 40 |
| It gives me new ideas or leads to implement. | 15 | (38%) | 17 | (43%) | 31 | (78%) | 0 | 40 |
| It breaks down the advice into achievable steps for me | 35 | (88%) | 0 | 40 | ||||
| It changes some of my thinking | 24 | (60%) | 9 | (23%) | 19 | (48%) | 0 | 40 |
| It could change how I do things | 23 | (58%) | 19 | (48%) | 29 | (73%) | 0 | 40 |
| Layout | ||||||||
| It is easy to read | 35 | (88%) | 32 | (80%) | 37 | (93%) | 0 | 40 |
| It is easy to understand | 38 | (95%) | 34 | (85%) | 38 | (95%) | 0 | 40 |
| I like the illustrations | 31 | (78%) | 27 | (68%) | 38 | (95%) | 0 | 40 |
| The illustrations are easy to understand | 37 | (93%) | 30 | (75%) | 38 | (95%) | 0 | 40 |
Notes: a A Likert-scale was used to calculate the score with the following responses: strongly disagree = 0, disagree = 1, neutral = 2, agree = 3, strongly agree = 4. In case of an answer <4 to an item, the researcher asked an open question to investigate possibilities of improvement. Every item was associated with open questions to investigate possibilities of improvement.
References
- Nikolic, I.A.; Stanciole, A.E.; Zaydman, M. Chronic Emergency: Why NCDs Matter; World Bank: Washington, DC, USA, 2011. [Google Scholar]
- World Health Organization. Noncommunicable Diseases Country Profiles 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Dineen-Griffin, S.; Garcia-Cardenas, V.; Williams, K.; Benrimoj, S.I. Helping patients help themselves: A systematic review of self-management support strategies in primary health care practice. PLoS ONE 2019, 14, e0220116. [Google Scholar] [CrossRef] [PubMed]
- Tsuyuki, R.T.; Beahm, N.P.; Okada, H.; Al Hamarneh, Y.N. Pharmacists as accessible primary health care providers: Review of the evidence. Can. Pharm. J. Rev. Des Pharm. Du Can. 2018, 151, 4–5. [Google Scholar] [CrossRef] [PubMed]
- Agomo, C.O. The role of community pharmacists in public health: A scoping review of the literature. J. Pharm. Health Serv. Res. 2012, 3, 25–33. [Google Scholar] [CrossRef]
- Anderson, C.; Zhan, K.; Boyd, M.; Mann, C. The role of pharmacists in general practice: A realist review. Res. Soc. Adm. Pharm. 2019, 15, 338–345. [Google Scholar] [CrossRef] [PubMed]
- George, P.P.; Molina, J.A.; Cheah, J.; Chan, S.C.; Lim, B.P. The evolving role of the community pharmacist in chronic disease management—A literature review. Ann. Acad. Med. Singap. 2010, 39, 861–867. [Google Scholar] [CrossRef]
- Chisholm-Burns, M.A.; Lee, J.K.; Spivey, C.A.; Slack, M.; Herrier, R.N.; Hall-Lipsy, E.; Zivin, J.G.; Abraham, I.; Palmer, J.; Martin, J.R.; et al. US pharmacists’ effect as team members on patient care: Systematic review and meta-analyses. Med. Care 2010, 48, 923–933. [Google Scholar] [CrossRef]
- Tan, E.C.; Stewart, K.; Elliott, R.A.; George, J. Pharmacist services provided in general practice clinics: A systematic review and meta-analysis. Res. Soc. Adm. Pharm. 2014, 10, 608–622. [Google Scholar] [CrossRef]
- Rotta, I.; Salgado, T.M.; Silva, M.L.; Correr, C.J.; Fernandez-Llimos, F. Effectiveness of clinical pharmacy services: An overview of systematic reviews (2000–2010). Pharm. Weekbl. 2015, 37, 687–697. [Google Scholar] [CrossRef]
- San-Juan-Rodriguez, A.; Newman, T.V.; Hernandez, I.; Swart, E.C.; Klein-Fedyshin, M.; Shrank, W.H.; Parekh, N. Impact of community pharmacist-provided preventive services on clinical, utilization, and economic outcomes: An umbrella review. Prev. Med. 2018, 115, 145–155. [Google Scholar] [CrossRef]
- Rondeaux, S.; Braeckman, T.; Beckwé, M.; Biset, N.; Maesschalck, J.; Duquet, N.; De Wulf, I.; Devroey, D.; De Vriese, C. Diabetes and Cardiovascular Diseases Risk Assessment in Community Pharmacies: An Implementation Study. Int. J. Environ. Res. Public Health 2022, 19, 8699. [Google Scholar] [CrossRef]
- Dewalt, D.A.; Berkman, N.D.; Sheridan, S.; Lohr, K.N.; Pignone, M.P. Literacy and health outcomes: A systematic review of the literature. J. Gen. Intern. Med. 2004, 19, 1228–1239. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low Health Literacy and Health Outcomes: An Updated Systematic Review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef] [PubMed]
- QSR International Pty Ltd.; Nvivo (Version 12). 2018. Available online: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home (accessed on 29 December 2022).
- Contreras, A.; García-Alonso, R.; Echenique, M.; Daye-Contreras, F. The SOL formulas for converting SMOG readability scores between health education materials written in Spanish, English, and French. J. Health Commun. 1999, 4, 21–29. [Google Scholar]
- Kincaid, J.; Fishburne, R.; Rogers, R.; Chissom, B. Research Branch Report 8–75; Naval Air Station: Memphis, TN, USA, 1975. [Google Scholar]
- Coleman, M.; Liau, T.L. A computer readability formula designed for machine scoring. J. Appl. Psychol. 1975, 60, 283–284. [Google Scholar] [CrossRef]
- HAS. Guide méthodologique—Élaboration d’un document écrit d’information à l’intention des patients et des usagers du système de santé. Oncologie 2006, 8, 182–196. [Google Scholar] [CrossRef]
- European Commission. Guideline on the Readability of the Labelling and Package Leaflet of Medicinal Products for Human Use; European Commission: Brussels, Belgium, 2009.
- Gibson, P.A.; Ruby, C.; Craig, M.D. A health/patient education database for family practice. Bull. Med. Libr. Assoc. 1991, 79, 357–369. [Google Scholar]
- Shoemaker, S.J.; Wolf, M.S.; Brach, C. Development of the Patient Education Materials Assessment Tool (PEMAT): A new measure of understandability and actionability for print and audiovisual patient information. Patient Educ. Couns. 2014, 96, 395–403. [Google Scholar] [CrossRef]
- Thakurdesai, P.A.; Kole, P.L.; Pareek, R. Evaluation of the quality and contents of diabetes mellitus patient education on Internet. Patient Educ. Couns. 2004, 53, 309–313. [Google Scholar] [CrossRef]
- Hill-Briggs, F.; Smith, A.S. Evaluation of Diabetes and Cardiovascular Disease Print Patient Education Materials for Use With Low–Health Literate Populations. Diabetes Care 2008, 31, 667–671. [Google Scholar] [CrossRef]
- Dube, L.; Van den Broucke, S.; Housiaux, M.; Dhoore, W.; Rendall-Mkosi, K. Type 2 diabetes self-management education programs in high and low mortality developing countries: A systematic review. Diabetes Educ. 2015, 41, 69–85. [Google Scholar] [CrossRef]
- Labrunée, M.; Pathak, A.; Loscos, M.; Coudeyre, E.; Casillas, J.-M.; Gremeaux, V. Therapeutic education in cardiovascular diseases: State of the art and perspectives. Ann. Phys. Rehabil. Med. 2012, 55, 322–341. [Google Scholar] [CrossRef] [PubMed]
- Coppola, A.; Sasso, L.; Bagnasco, A.; Giustina, A.; Gazzaruso, C. The role of patient education in the prevention and management of type 2 diabetes: An overview. Endocrine 2015, 53, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Lindstrom, J.; Tuomilehto, J. The diabetes risk score: A practical tool to predict type 2 diabetes risk. Diabetes Care 2003, 26, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Montori, V.M.; Breslin, M.; Maleska, M.; Weymiller, A.J. Creating a Conversation: Insights from the Development of a Decision Aid. PLOS Med. 2007, 4, e233. [Google Scholar] [CrossRef]
- Elwyn, G.; Kreuwel, I.; Durand, M.A.; Sivell, S.; Joseph-Williams, N.; Evans, R.; Edwards, A. How to develop web-based decision support interventions for patients: A process map. Patient Educ. Couns. 2011, 82, 260–265. [Google Scholar] [CrossRef]
- Friis, K.; Lasgaard, M.; Osborne, R.H.; Maindal, H.T. Gaps in understanding health and engagement with healthcare providers across common long-term conditions: A population survey of health literacy in 29 473 Danish citizens. BMJ Open 2016, 6, e009627. [Google Scholar] [CrossRef]
- Houts, P.S.; Doak, C.C.; Doak, L.G.; Loscalzo, M.J. The role of pictures in improving health communication: A review of research on attention, comprehension, recall, and adherence. Patient Educ. Couns. 2006, 61, 173–190. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. CDC Clear Communication Index, A Tool for Developing and Assessing CDC Public Communication Products; CDC: Atlanta, GA, USA, 2019.
- Seligman, H.K.; Wallace, A.S.; DeWalt, D.A.; Schillinger, D.; Arnold, C.L.; Shilliday, B.B.; Delgadillo, A.; Bengal, N.; Davis, T.C. Facilitating behavior change with low-literacy patient education materials. Am. J. Health Behav. 2007, 31, S69–S78. [Google Scholar] [CrossRef]
- Mayer, R.; Mayer, R.E. The Cambridge Handbook of Multimedia Learning; Cambridge University Press: Cambridge, UK, 2005. [Google Scholar]
- Whitlock, E.P.; Orleans, C.T.; Pender, N.; Allan, J. Evaluating primary care behavioral counseling interventions: An evidence-based approach. Am. J. Prev. Med. 2002, 22, 267–284. [Google Scholar] [CrossRef]
- Salvo, M.C.; Cannon-Breland, M.L. Motivational interviewing for medication adherence. J. Am. Pharm. Assoc. 2015, 55, e354–e363. [Google Scholar] [CrossRef]
- Spears, J.; Erkens, J.; Misquitta, C.; Cutler, T.; Stebbins, M. A Pharmacist-Led, Patient-Centered Program Incorporating Motivational Interviewing for Behavior Change to Improve Adherence Rates and Star Ratings in a Medicare Plan. J. Manag. Care Spéc. Pharm. 2019, 26, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Ekong, G.; Chou, C.; Lakin, J.; Hardin, A.; Fox, B.; Hunt, C.; Kavookjian, J. Pharmacist-led motivational interviewing for diabetes medication adherence in a worksite wellness program. J. Am. Pharm. Assoc. 2020, 60, e224–e229. [Google Scholar] [CrossRef]
- Toljamo, T.; Kaukonen, M.; Nieminen, P.; Kinnula, V.L. Early detection of COPD combined with individualized counselling for smoking cessation: A two-year prospective study. Scand. J. Prim. Health Care 2010, 28, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Rubak, S.; Sandbaek, A.; Lauritzen, T.; Christensen, B. Motivational interviewing: A systematic review and meta-analysis. Br. J. Gen. Pract. 2005, 55, 305–312. [Google Scholar] [PubMed]
- Pignone, M.; DeWalt, D.A.; Sheridan, S.; Berkman, N.; Lohr, K.N. Interventions to improve health outcomes for patients with low literacy. J. Gen. Intern. Med. 2005, 20, 185–192. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).