Voice Assistants as Consultants for Male Patients with Sexual Dysfunction: A Reliable Option?
Abstract
1. Introduction
2. Materials and Methods
2.1. Device Selection
2.2. Identification of Question Pool
2.3. Collection of Answers, Data Interpretation, and Outcomes
2.4. Statistics
3. Results
3.1. Recognition of Questions
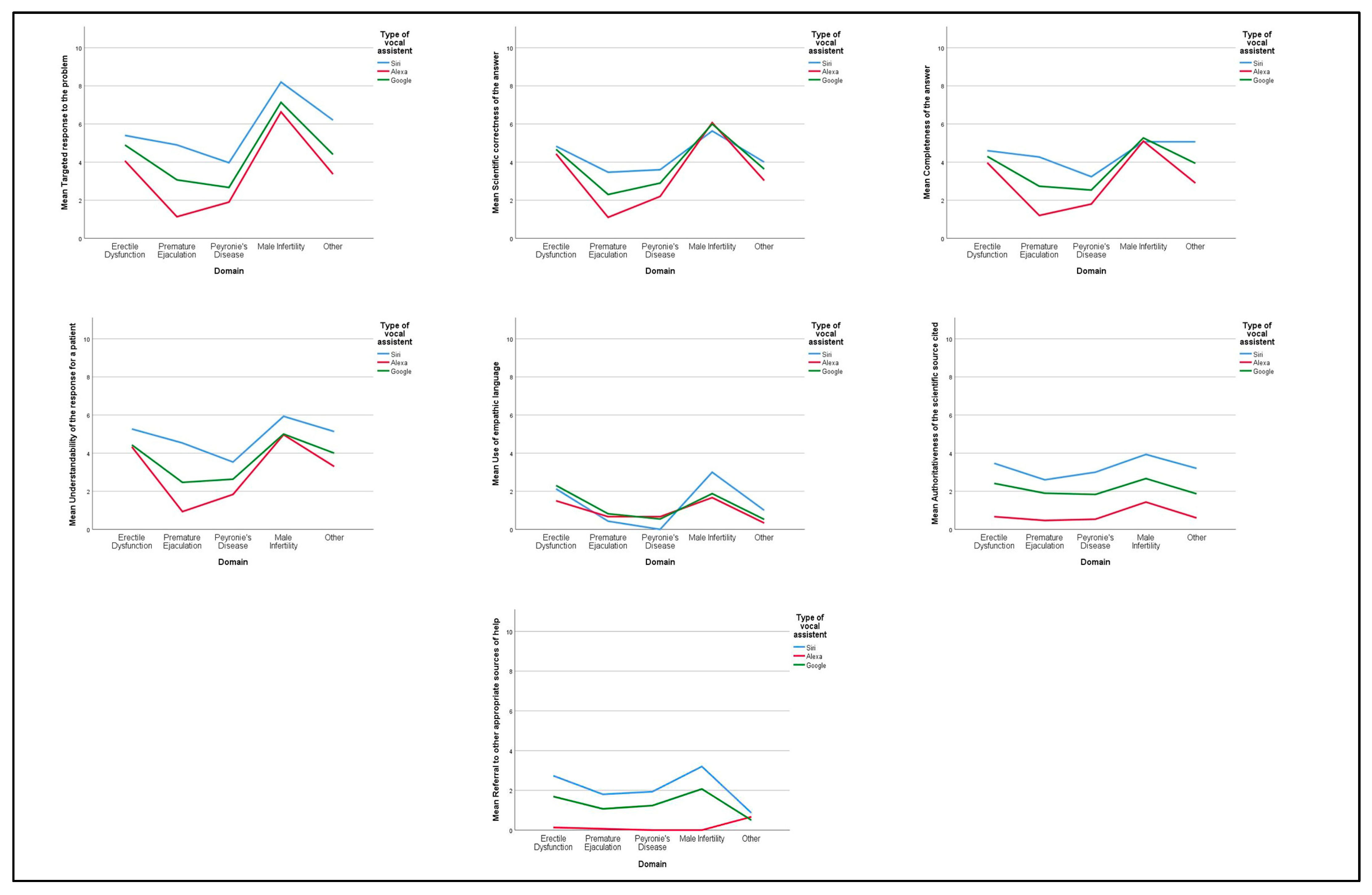
3.2. Quality and Characteristics of the Answers
4. Discussion
4.1. Our Findings and Available Literature
4.2. Strengths and Limitations
4.3. Future Perspectives
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eurostat. One in Two EU Citizens Look for Health Information Online. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/edn-20210406-1 (accessed on 10 November 2022).
- Lee, K.; Hoti, K.; Hughes, J.D.; Emmerton, L.M. Consumer Use of “Dr Google”: A Survey on Health Information-Seeking Behaviors and Navigational Needs. J. Med. Internet Res. 2015, 17, e288. [Google Scholar] [CrossRef] [PubMed]
- Stukus, D.R. How Dr Google Is Impacting Parental Medical Decision Making. Immunol. Allergy Clin. N. Am. 2019, 39, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Tonsaker, T.; Bartlett, G.; Trpkov, C. Health information on the Internet: Gold mine or minefield? Can. Fam. Physician 2014, 60, 407–408. [Google Scholar]
- Dutsinma, F.L.I.; Pal, D.; Funilkul, S.; Chan, J.H. A Systematic Review of Voice Assistant Usability: An ISO 9241-11 Approach. SN Comput. Sci. 2022, 3, 267. [Google Scholar] [CrossRef]
- IBM. NLP vs. NLU vs. NLG: The Differences between Three Natural Language Processing Concepts. Available online: https://www.ibm.com/blogs/watson/2020/11/nlp-vs-nlu-vs-nlg-the-differences-between-three-natural-language-processing-concepts/ (accessed on 10 November 2022).
- PCmag. Which Mobile Voice Assistant Is Used the Most? Available online: https://www.pcmag.com/news/which-mobile-voice-assistant-is-used-the-most (accessed on 10 November 2022).
- Insideri Intelligence. How Big Is the Voice Assistant Market? Available online: https://www.insiderintelligence.com/content/how-big-voice-assistant-market (accessed on 10 November 2022).
- Alagha, E.C.; Helbing, R.R. Evaluating the quality of voice assistants’ responses to consumer health questions about vaccines: An exploratory comparison of Alexa, Google Assistant and Siri. BMJ Health Care Inform. 2019, 26, e100075. [Google Scholar] [CrossRef]
- Miner, A.S.; Milstein, A.; Schueller, S.; Hegde, R.; Mangurian, C.; Linos, E. Smartphone-Based Conversational Agents and Responses to Questions About Mental Health, Interpersonal Violence, and Physical Health. JAMA Intern. Med. 2016, 176, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Russo, G.I.; Di Mauro, M.; Cocci, A.; Cacciamani, G.; Cimino, S.; Serefoglu, E.C.; Albersen, M.; Capogrosso, P.; Fode, M.; EAU-YAU Men’s Health Working Group. Consulting “Dr Google” for sexual dysfunction: A contemporary worldwide trend analysis. Int. J. Impot. Res. 2019, 32, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Litras, A.; Latreille, S.; Temple-Smith, M. Dr Google, porn and friend-of-a-friend: Where are young men really getting their sexual health information? Sex. Health 2015, 12, 488–494. [Google Scholar] [CrossRef]
- Strategy Analytics. Strategy Analytics: Another Record Quarter for Smart Speakers in 3Q21, Though Supply Chain Woes are on the Horizon. Available online: https://news.strategyanalytics.com/press-releases/press-release-details/2021/Strategy-Analytics-Another-Record-Quarter-for-Smart-Speakers-in-3Q21-Though-Supply-Chain-Woes-are-on-the-Horizon/default.aspx (accessed on 10 November 2022).
- Alonso-Isa, M.; García-Gómeza, B.; García-Rojo, E.; Medina-Polo, J.; Manfredi, C.; Rodríguez-Antolín, A.; Romero-Otero, J. Penile prosthesis implantation in the COVID era. Post-surgery follow-up and management of complications. Rev. Int. Androl. 2021, 20, 62–67. [Google Scholar] [PubMed]
- Manfredi, C.; Fortier, E.; Faix, A.; Martínez-Salamanca, J.I. Penile Implant Surgery Satisfaction Assessment. J. Sex. Med. 2021, 18, 868–874. [Google Scholar] [CrossRef]
- Garrido-Abad, P.; Senra-Bravo, I.; Manfredi, C.; Fernández-Pascual, E.; Linares-Espinós, E.; Fernández-Arjona, M.; Varillas-Delgado, D.; Martínez-Salamanca, J.I. Combination therapy with topical alprostadil and phosphodiesterase-5 inhibitors after failure of oral therapy in patients with erectile dysfunction: A prospective, two-arm, open-label, non-randomized study. Int. J. Impot. Res. 2022, 34, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Romero-Otero, J.; Manfredi, C.; Wilson, S.K. The good, the bad, and the ugly about surgical approaches for inflatable penile prosthesis implantation. Int. J. Impot. Res. 2020, 34, 128–137. [Google Scholar] [CrossRef]
- Arcaniolo, D.; Bellastella, G.; Manfredi, C.; Terribile, M.; Giordano, D.R.; Quattrone, C.; La Rocca, R.; De Sio, M.; Verze, P.; Mirone, V. Is topical alprostadil an usable and reliable alternative to intracavernous injection for penile dynamic duplex ultrasonography? Andrologia 2020, 52, e13480. [Google Scholar] [CrossRef] [PubMed]
- Verze, P.; Capece, M.; Creta, M.; La Rocca, R.; Persico, F.; Spirito, L.; Cardi, A.; Mirone, V. Efficacy and safety of low-intensity shockwave therapy plus tadalafil 5 mg once daily in men with type 2 diabetes mellitus and erectile dysfunction: A matched-pair comparison study. Asian J. Androl. 2020, 22, 379–382. [Google Scholar] [PubMed]
- Spirito, L.; Manfredi, C.; La Rocca, R.; Napolitano, L.; Di Girolamo, A.; Capece, M.; Trama, F.; Sciorio, C.; Sokolakis, I.; Creta, M.; et al. Daily low-dose tadalafil may reduce the penile curvature progression rate in patients with acute Peyronie’s disease: A retrospective comparative analysis. Int. J. Impot. Res. 2022. ahead of print. [Google Scholar] [CrossRef]
- Verze, P.; La Rocca, R.; Spirito, L.; Califano, G.; Venturino, L.; Napolitano, L.; Cardi, A.; Arcaniolo, D.; Rosati, C.; Palmieri, A.; et al. Premature Ejaculation patients and their partners: Arriving at a clinical profile for a real optimization of the treatment. Arch. Ital. Urol. Androl. 2021, 93, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Trama, F.; Illiano, E.; Iacono, F.; Ruffo, A.; Di Lauro, G.; Aveta, A.; Crocetto, F.; Manfredi, C.; Costantini, E. Use of penile shear wave elastosonography for the diagnosis of Peyronie’s Disease: A prospective case-control study. Basic Clin. Androl. 2022, 16, 15. [Google Scholar] [CrossRef]
- Crocetto, F.; Barone, B.; Manfredi, C.; Trama, F.; Romano, L.; Romeo, M.; Russo, G.; Sicignano, E.; Persico, F.; Aveta, A.; et al. Are Insulin Resistance and Non-Alcoholic Fatty Liver Disease Associated With Peyronie’s Disease? A Pilot Study. J. Physiol. Pharmacol. 2022, 73, 1. [Google Scholar]
- Krishnappa, P.; Manfredi, C.; Sinha, M.; Arcaniolo, D.; Matippa, P.; Moncada, I. Penile Modeling in Peyronie’s Disease: A Systematic Review of the Literature. Sex. Med. Rev. 2022, 10, 434–450. [Google Scholar] [CrossRef]
- García-Rojo, E.; García-Gómez, B.; Pérez-De la Blanca, R.S.; Manfredi, C.; Alonso-Isa, M.; Medina-Polo, J.; Rodriguez-Antolín, R.; Romero-Otero, J. Role of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in Peyronie’s disease: A new diagnostic approach to predict the stage of the disease? Asian J. Androl. 2021, 23, 325–329. [Google Scholar]
- Verze, P.; Sokolakis, I.; Manfredi, C.; Collà Ruvolo, C.; Hatzichristodoulou, G.; Romero-Otero, J. Penile prosthesis implant in the management of Peyronies’ disease: A systematic review of the literature. Minerva Urol. Nephrol. 2021, 73, 196–214. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Pascual, E.; Manfredi, C.; Torremadé, J.; Peinado-Ibarra, F.; Sarquella-Geli, J.; Romero-Otero, J.; García-Baquero, R.; Fraile-Poblador, A.; Roselló-Barbará, M.; Campos-Juanatey, F.; et al. Multicenter Prospective Study of Grafting with Collagen Fleece TachoSil in Patients With Peyronie’s Disease. J. Sex. Med. 2020, 17, 2279–2286. [Google Scholar] [CrossRef] [PubMed]
- Capece, M.; Arcaniolo, D.; Manfredi, C.; Palmieri, A.; De Sio, M.; Verze, P.; Fusco, F.; Longo, N.; Mirone, V. Second cycle of intralesional Collagenase Clostridium hystoliticum for Peyronie’s disease using the modified shortened protocol: Results from a retrospective analysis. Andrologia 2020, 52, e13527. [Google Scholar] [CrossRef]
- García-Rojo, E.; García-Gómez, B.; Manfredi, C.; Alonso-Isa, M.; Medina-Polo, J.; Carpintero-Miguel, M.; Romero-Otero, J. Efficacy and safety of dorsal penile nerve block before collagenase of clostridium histolyticum injections in Peyronie’s disease patients: Results from a prospective pilot study. Andrologia 2020, 52, e13740. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Pascual, E.; Manfredi, C.; Cocci, A.; Quintana-Franco, L.M.; Egui-Rojo, M.A.; Carballido-Rodríguez, J.; Martínez-Salamanca, J.I. A Novel Penile Splint as Early Traction Therapy After Grafting Techniques for Peyronie’s Disease. J. Sex. Med. 2020, 17, 1819–1824. [Google Scholar] [CrossRef]
- Manfredi, C.; Arcaniolo, D.; Amicuzi, U.; Spirito, L.; Napolitano, L.; Crocerossa, F.; Paoletta, M.; Gisone, S.; Cirillo, P.; Crocetto, F.; et al. Impact of extracorporeal shockwave therapy for erectile dysfunction and Peyronie’s disease on reproductive and hormonal testicular function. Andrology 2022, 10, 1368–1375. [Google Scholar] [CrossRef]
- Fusco, G.M.; Cirillo, L.; Abate, M.; Morra, S.; Morgera, V.; Barone, B.; Crocetto, F.; Cacace, G.; Di Bello, F.; Spirito, L.; et al. Male infertility, what Mobile Health Applications “know”: Quality analysis and adherence to European Association of Urology Guidelines. Arch. Ital. Urol. Androl. 2022, 94, 470–475. [Google Scholar] [CrossRef]
- Zaccaro, C.; Subirà, D.; López-Diez, I.; Manfredi, C.; Ascensios-Vargas, J.P.; Moncada-Iribarren, I. History and future perspectives of male aesthetic genital surgery. Int. J. Impot. Res. 2022, 34, 327–331. [Google Scholar] [CrossRef]
- Romero-Otero, J.; Manfredi, C. Take-home messages on male genital aesthetic surgery. Int. J. Impot. Res. 2022, 34, 404–405. [Google Scholar] [CrossRef]
- Califano, G.; Arcaniolo, D.; Collà Ruvolo, C.; Manfredi, C.; Smarrazzo, F.; Cilio, S.; Verze, P. Glans penis augmentation: When, how, and why? Int. J. Impot. Res. 2022, 34, 343–346. [Google Scholar] [CrossRef]
- Manfredi, C.; Romero-Otero, J.; Djinovic, R. Penile girth enhancement procedures for aesthetic purposes. Int. J. Impot. Res. 2022, 34, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Romero-Otero, J.; Manfredi, C.; Ralph, D.; Osmonov, D.; Verze, P.; Castiglione, F.; Serefoglu, E.C.; Bozzini, G.; García-Gómez, B. Non-invasive and surgical interventions of penile enhancement for aesthetic or therapeutic purposes: A systematic review. BJU Int. 2021, 127, 269–291. [Google Scholar] [CrossRef] [PubMed]
- Stizzo, M.; Manfredi, C.; Spirito, L.; Sciorio, C.; Romero-Otero, J.; Martinez Salamanca, J.I.; Crocetto, F.; Verze, P.; Imbimbo, C.; Fusco, F.; et al. Hyperbaric oxygen therapy as adjuvant treatment for surgical site infections after male-to-female gender affirmation surgery: A ten-year experience. Andrology 2022, 10, 1310–1316. [Google Scholar] [CrossRef] [PubMed]
- Manfredi, C.; García-Gómez, B.; Arcaniolo, D.; García-Rojo, E.; Crocerossa, F.; Autorino, R.; Gratzke, C.; De Sio, M.; Romero-Otero, J. Impact of Surgery for Benign Prostatic Hyperplasia on Sexual Function: A Systematic Review and Meta-analysis of Erectile Function and Ejaculatory Function. Eur. Urol. Focus 2022, 8, 1711–1732. [Google Scholar] [CrossRef]
- Di Bello, F.; Creta, M.; Napolitano, L.; Califano, G.; Passaro, F.; Morra, S.; Di Giovanni, A.; Fusco, G.M.; Cirillo, L.; Abate, M.; et al. Male Sexual Dysfunction and Infertility in Spinal Cord Injury Patients: State-of-the-Art and Future Perspectives. J. Pers. Med. 2022, 12, 873. [Google Scholar] [CrossRef]
- Crocetto, F.; Arcaniolo, D.; Napolitano, L.; Barone, B.; La Rocca, R.; Capece, M.; Caputo, V.F.; Imbimbo, C.; De Sio, M.; Calace, F.P.; et al. Impact of Sexual Activity on the Risk of Male Genital Tumors: A Systematic Review of the Literature. Int. J. Environ. Res. Public Health 2021, 18, 8500. [Google Scholar] [CrossRef]
- Schoentgen, N.; Califano, G.; Manfredi, C.; Romero-Otero, J.; Ouzaid, I.; Hermieu, J.F.; Xylinas, E.; Verze, P. Is it worth starting sexual rehabilitation before radical prostatectomy? Results from a systematic review of the literature. Front. Surg. 2021, 8, 648345. [Google Scholar] [CrossRef]
- Terribile, M.; Stizzo, M.; Manfredi, C.; Quattrone, C.; Bottone, F.; Giordano, D.R.; Bellastella, G.; Arcaniolo, D.; De Sio, M. 46, XX Testicular Disorder of Sex Development (DSD): A Case Report and Systematic Review. Medicina 2019, 55, 371. [Google Scholar] [CrossRef]
- Spirito, L.; Manfredi, C.; Carrano, R.; Trinchieri, A.; Salemi, F.; Sciorio, C.; Mirone, V.; Verze, P. Impact of Kidney Transplantation on Male Sexual Function: Results from a Ten-Year Retrospective Study. J. Sex. Med. 2020, 17, 2191–2197. [Google Scholar] [CrossRef]
- Manfredi, C.; Arcaniolo, D.; Spatafora, P.; Crocerossa, F.; Fusco, F.; Verze, P.; Fiori, C.; Damiano, R.; Cindolo, L.; De Sio, M.; et al. Emerging minimally invasive transurethral treatments for benign prostatic hyperplasia: A systematic review with meta-analysis of functional outcomes and description of complications. Minerva Urol. Nephrol. 2021, 74, 389–399. [Google Scholar] [CrossRef]
- Hong, G.; Folcarelli, A.; Less, J.; Wang, C.; Erbasi, N.; Lin, S. Voice Assistants and Cancer Screening: A Comparison of Alexa, Siri, Google Assistant, and Cortana. Ann. Fam. Med. 2021, 19, 447–449. [Google Scholar] [CrossRef] [PubMed]
- Wilson, N.; MacDonald, E.J.; Mansoor, O.D.; Morgan, J. In bed with Siri and Google Assistant: A comparison of sexual health advice. BMJ 2017, 359, j5635. [Google Scholar] [CrossRef] [PubMed]
| VA | Condition | Recognition of Question | ||
|---|---|---|---|---|
| Yes n (%) | No n (%) | Total n (%) | ||
| Siri | ED | 28 (93.3) | 2 (6.7) | 30 (100) |
| PE | 24 (80.0) | 6 (20.0) | 30 (100) | |
| PD | 20 (66.7) | 10 (33.3) | 30 (100) | |
| Male Infertility | 30 (100) | 0 (0.0) | 30 (100) | |
| Other | 23 (76.7) | 7 (23.3) | 30 (100) | |
| Total | 125 (83.3) | 25 (16.7) | 150 (100) | |
| Alexa | ED | 28 (93.3) | 2 (6.7) | 30 (100) |
| PE | 12 (40.0) | 18 (60.0) | 30 (100) | |
| PD | 10 (33.3) | 20 (66.7) | 30 (100) | |
| Male Infertility | 28 (93.3) | 2 (6.7) | 30 (100) | |
| Other | 18 (60.0) | 12 (40.0) | 30 (100) | |
| Total | 96 (64.0) | 54 (36.0) | 150 (100) | |
| Google Assistant | ED | 28 (93.3) | 2 (6.7) | 30 (100) |
| PE | 18 (60.0) | 12 (40.0) | 30 (100) | |
| PD | 15 (50.0) | 15 (50.0) | 30 (100) | |
| Male Infertility | 29 (96.7) | 1 (3.3) | 30 (100) | |
| Other | 21 (70.0) | 9 (30.0) | 30 (100) | |
| Total | 111 (74.0) | 39 (26.0) | 150 (100) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Napolitano, L.; Barone, B.; Spirito, L.; Trama, F.; Pandolfo, S.D.; Capece, M.; García-Rojo, E.; Fernández-Pascual, E.; Crocetto, F.; Fusco, F.; et al. Voice Assistants as Consultants for Male Patients with Sexual Dysfunction: A Reliable Option? Int. J. Environ. Res. Public Health 2023, 20, 2612. https://doi.org/10.3390/ijerph20032612
Napolitano L, Barone B, Spirito L, Trama F, Pandolfo SD, Capece M, García-Rojo E, Fernández-Pascual E, Crocetto F, Fusco F, et al. Voice Assistants as Consultants for Male Patients with Sexual Dysfunction: A Reliable Option? International Journal of Environmental Research and Public Health. 2023; 20(3):2612. https://doi.org/10.3390/ijerph20032612
Chicago/Turabian StyleNapolitano, Luigi, Biagio Barone, Lorenzo Spirito, Francesco Trama, Savio Domenico Pandolfo, Marco Capece, Esther García-Rojo, Esaú Fernández-Pascual, Felice Crocetto, Ferdinando Fusco, and et al. 2023. "Voice Assistants as Consultants for Male Patients with Sexual Dysfunction: A Reliable Option?" International Journal of Environmental Research and Public Health 20, no. 3: 2612. https://doi.org/10.3390/ijerph20032612
APA StyleNapolitano, L., Barone, B., Spirito, L., Trama, F., Pandolfo, S. D., Capece, M., García-Rojo, E., Fernández-Pascual, E., Crocetto, F., Fusco, F., De Sio, M., Arcaniolo, D., & Manfredi, C. (2023). Voice Assistants as Consultants for Male Patients with Sexual Dysfunction: A Reliable Option? International Journal of Environmental Research and Public Health, 20(3), 2612. https://doi.org/10.3390/ijerph20032612










