Non-Cardiac Chest Pain as a Persistent Physical Symptom: Psychological Distress and Workability
Abstract
1. Introduction
2. Materials and Methods
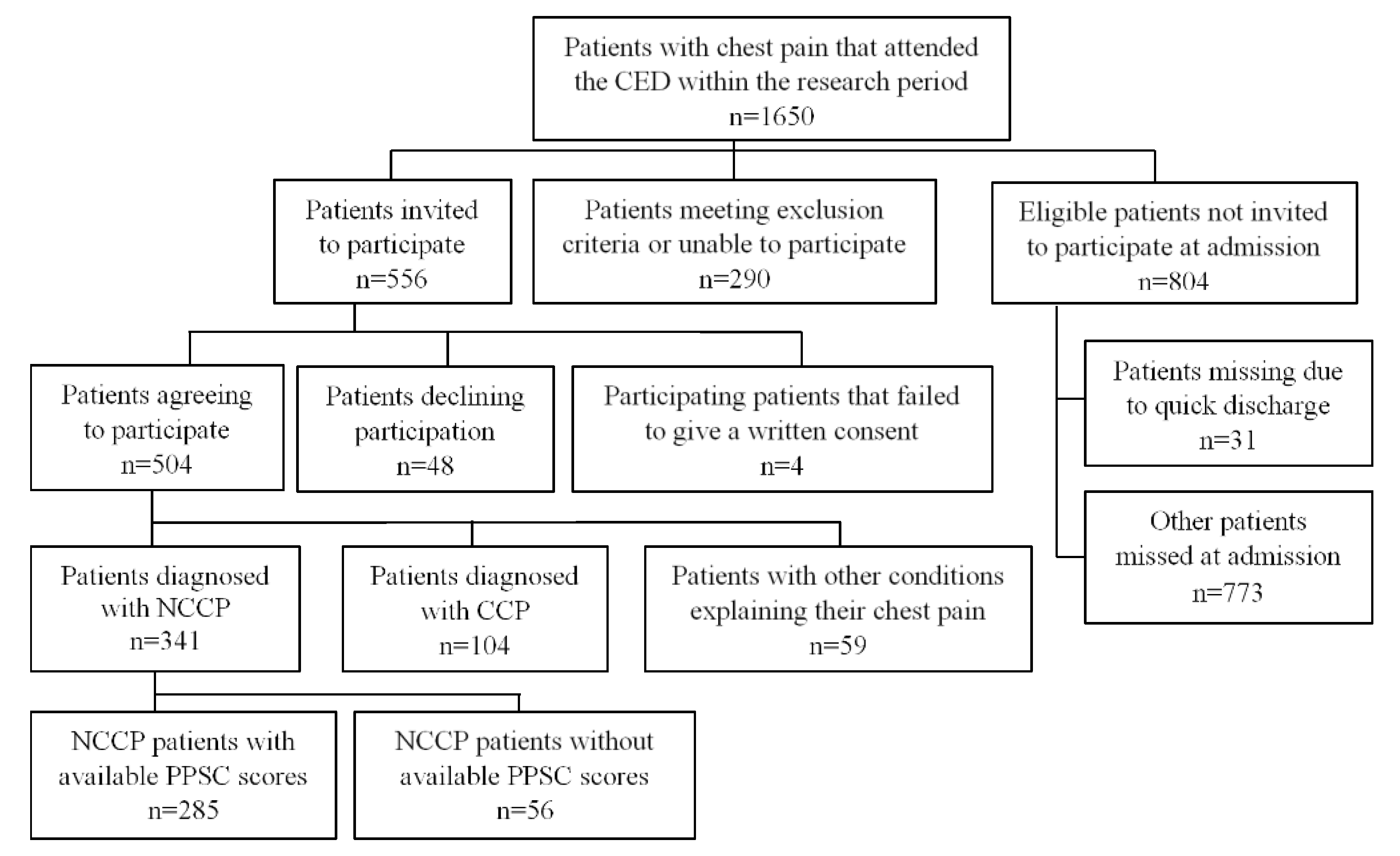
2.1. Participants
2.2. Measures
2.2.1. Psychological Measurements
2.2.2. Medical Diagnosis
2.2.3. Background Information
2.3. Procedure
2.4. Data Analysis
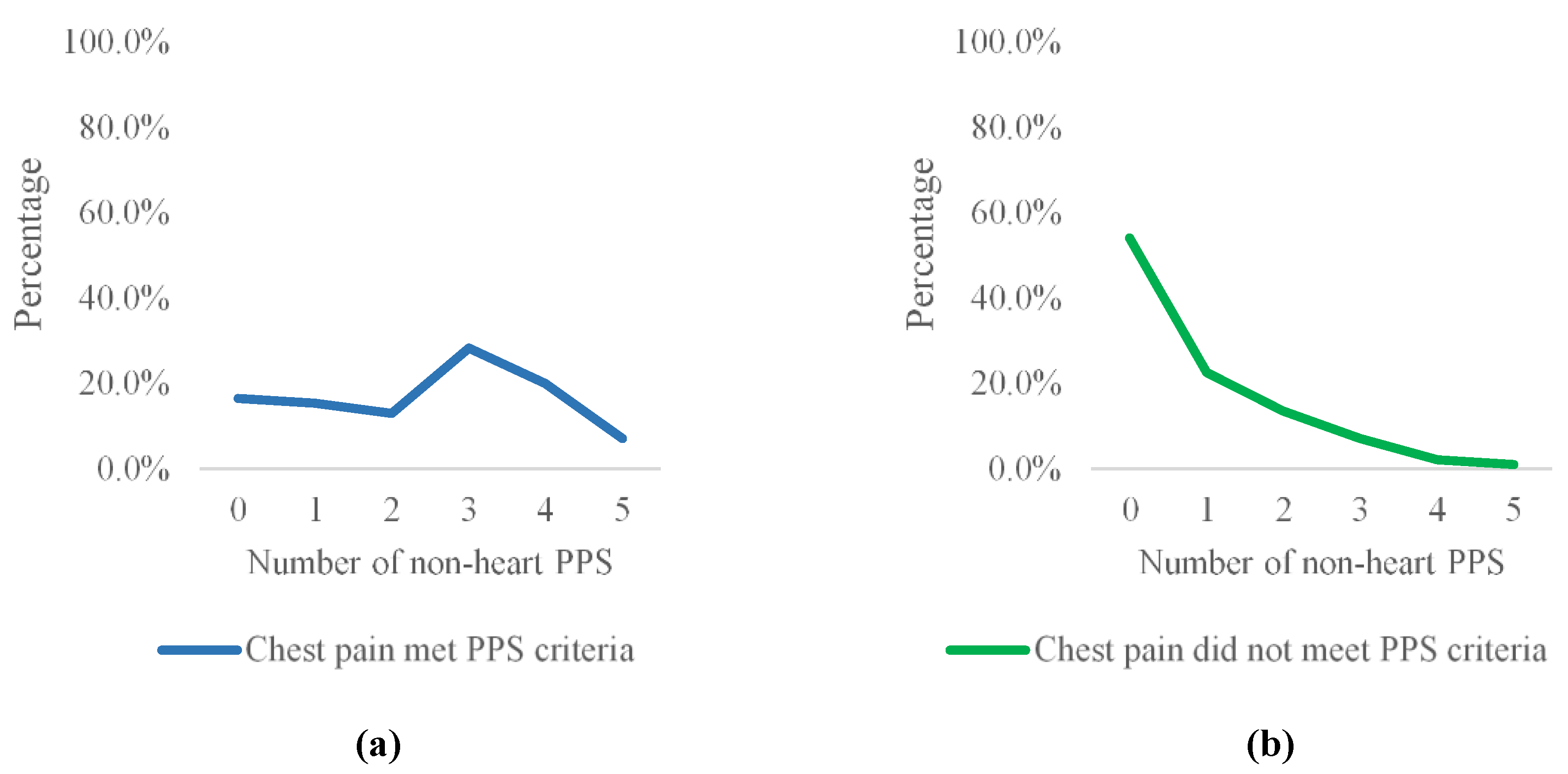
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Campbell, K.A.; Madva, E.N.; Villegas, A.C.; Beale, E.E.; Beach, S.R.; Wasfy, J.H.; Albanese, A.M.; Huffman, J.C. Non-Cardiac Chest Pain: A Review for the Consultation-Liaison Psychiatrist. Psychosomatics 2017, 58, 252–265. [Google Scholar] [CrossRef] [PubMed]
- Eslick, G.D.; Jones, M.; Talley, N. Non-Cardiac Chest Pain: Prevalence, Risk Factors, Impact and Consulting--A Population-Based Study. Aliment. Pharmacol. Ther. 2003, 17, 1115–1124. [Google Scholar] [CrossRef] [PubMed]
- Frieling, T. Non-Cardiac Chest Pain. Visc. Med. 2018, 34, 92–96. [Google Scholar] [CrossRef]
- Fass, R.; Dickman, R. Non-Cardiac Chest Pain: An Update. Neurogastroenterol. Motil. Off. J. Eur. Gastrointest. Motil. Soc. 2006, 18, 408–417. [Google Scholar] [CrossRef]
- Debney, M.T.; Fox, K.F. Rapid Access Cardiology—A Nine Year Review. QJM Int. J. Med. 2012, 105, 231–234. [Google Scholar] [CrossRef] [PubMed]
- Dumville, J.C.; MacPherson, H.; Griffith, K.; Miles, J.N.V.; Lewin, R.J. Non-Cardiac Chest Pain: A Retrospective Cohort Study of Patients Who Attended a Rapid Access Chest Pain Clinic. Fam. Pract. 2007, 24, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Mayou, R.; Bryant, B.; Forfar, C.; Clark, D. Non-Cardiac Chest Pain and Benign Palpitations in the Cardiac Clinic. Br. Heart J. 1994, 72, 548–553. [Google Scholar] [CrossRef]
- Stallone, F.; Twerenbold, R.; Wildi, K.; Reichlin, T.; Rubini Gimenez, M.; Haaf, P.; Fuechslin, N.; Hillinger, P.; Jaeger, C.; Kreutzinger, P.; et al. Prevalence, Characteristics and Outcome of Non-Cardiac Chest Pain and Elevated Copeptin Levels. Heart Br. Card. Soc. 2014, 100, 1708–1714. [Google Scholar] [CrossRef]
- Jonsbu, E.; Dammen, T.; Morken, G.; Lied, A.; Vik-Mo, H.; Martinsen, E.W. Cardiac and Psychiatric Diagnoses among Patients Referred for Chest Pain and Palpitations. Scand. Cardiovasc. J. 2009, 43, 256–259. [Google Scholar] [CrossRef]
- Chambers, J.B.; Marks, E.M.; Russell, V.; Hunter, M.S. A Multidisciplinary, Biopsychosocial Treatment for Non-Cardiac Chest Pain. Int. J. Clin. Pract. 2015, 69, 922–927. [Google Scholar] [CrossRef]
- Webster, R.; Norman, P.; Goodacre, S.; Thompson, A. The Prevalence and Correlates of Psychological Outcomes in Patients with Acute Non-Cardiac Chest Pain: A Systematic Review. Emerg. Med. J. EMJ 2012, 29, 267–273. [Google Scholar] [CrossRef]
- Dammen, T.; Ekeberg, Ø.; Arnesen, H.; Friis, S. Health-Related Quality of Life in Non-Cardiac Chest Pain Patients with and without Panic Disorder. Int. J. Psychiatry Med. 2008, 38, 271–286. [Google Scholar] [CrossRef] [PubMed]
- Webster, R.; Norman, P.; Goodacre, S.; Thompson, A.R.; McEachan, R.R.C. Illness Representations, Psychological Distress and Non-Cardiac Chest Pain in Patients Attending an Emergency Department. Psychol. Health 2014, 29, 1265–1282. [Google Scholar] [CrossRef] [PubMed]
- Eslick, G.D.; Talley, N.J. Non-Cardiac Chest Pain: Predictors of Health Care Seeking, the Types of Health Care Professional Consulted, Work Absenteeism and Interruption of Daily Activities. Aliment. Pharmacol. Ther. 2004, 20, 909–915. [Google Scholar] [CrossRef]
- Eslick, G.D.; Talley, N.J. Natural History and Predictors of Outcome for Non-Cardiac Chest Pain: A Prospective 4-Year Cohort Study. Neurogastroenterol. Motil. 2008, 20, 989–997. [Google Scholar] [CrossRef]
- Carson, A.J.; Ringbauer, B.; Stone, J.; McKenzie, L.; Warlow, C.; Sharpe, M. Do Medically Unexplained Symptoms Matter? A Prospective Cohort Study of 300 New Referrals to Neurology Outpatient Clinics. J. Neurol. Neurosurg. Psychiatry 2000, 68, 207–210. [Google Scholar] [CrossRef] [PubMed]
- Kirmayer, L.J.; Groleau, D.; Looper, K.J.; Dao, M.D. Explaining Medically Unexplained Symptoms. Can. J. Psychiatry Rev. Can. Psychiatr. 2004, 49, 663–672. [Google Scholar] [CrossRef]
- Nimnuan, C.; Hotopf, M.; Wessely, S. Medically Unexplained Symptoms: An Epidemiological Study in Seven Specialities. J. Psychosom. Res. 2001, 51, 361–367. [Google Scholar] [CrossRef]
- Reid, S.; Wessely, S.; Crayford, T.; Hotopf, M. Medically Unexplained Symptoms in Frequent Attenders of Secondary Health Care: Retrospective Cohort Study. BMJ 2001, 322, 767. [Google Scholar] [CrossRef]
- Roca, M.; Gili, M.; Garcia-Garcia, M.; Salva, J.; Vives, M.; Garcia Campayo, J.; Comas, A. Prevalence and Comorbidity of Common Mental Disorders in Primary Care. J. Affect. Disord. 2009, 119, 52–58. [Google Scholar] [CrossRef]
- Budtz-Lilly, A.; Vestergaard, M.; Fink, P.; Carlsen, A.H.; Rosendal, M. The Prognosis of Bodily Distress Syndrome: A Cohort Study in Primary Care. Gen. Hosp. Psychiatry 2015, 37, 560–566. [Google Scholar] [CrossRef] [PubMed]
- Harris, A.M.; Orav, E.J.; Bates, D.W.; Barsky, A.J. Somatization Increases Disability Independent of Comorbidity. J. Gen. Intern. Med. 2009, 24, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Rask, M.T.; Rosendal, M.; Fenger-Grøn, M.; Bro, F.; Ørnbøl, E.; Fink, P. Sick Leave and Work Disability in Primary Care Patients with Recent-Onset Multiple Medically Unexplained Symptoms and Persistent Somatoform Disorders: A 10-Year Follow-up of the FIP Study. Gen. Hosp. Psychiatry 2015, 37, 53–59. [Google Scholar] [CrossRef]
- Broddadottir, E.; Flovenz, S.O.; Gylfason, H.F.; Pormar, P.; Einarsson, H.; Salkovskis, P.; Sigurdsson, J.F. “I’m So Tired”: Fatigue as a Persistent Physical Symptom among Working People Experiencing Exhaustion Disorder. Int. J. Environ. Res. Public Health 2021, 18, 8657. [Google Scholar] [CrossRef] [PubMed]
- Hoedeman, R.; Krol, B.; Blankenstein, N.; Koopmans, P.C.; Groothoff, J.W. Severe MUPS in a Sick-Listed Population: A Cross-Sectional Study on Prevalence, Recognition, Psychiatric Co-Morbidity and Impairment. BMC Public Health 2009, 9, 440. [Google Scholar] [CrossRef]
- den Boeft, M.; Twisk, J.W.R.; Hoekstra, T.; Terluin, B.; Penninx, B.W.J.H.; van der Wouden, J.C.; Numans, M.E.; van der Horst, H.E. Medically Unexplained Physical Symptoms and Work Functioning over 2 Years: Their Association and the Influence of Depressive and Anxiety Disorders and Job Characteristics. BMC Fam. Pract. 2016, 17, 46. [Google Scholar] [CrossRef]
- Hoedeman, R.; Blankenstein, A.H.; Krol, B.; Koopmans, P.C.; Groothoff, J.W. The Contribution of High Levels of Somatic Symptom Severity to Sickness Absence Duration, Disability and Discharge. J. Occup. Rehabil. 2010, 20, 264–273. [Google Scholar] [CrossRef]
- Loengaard, K.; Bjorner, J.B.; Fink, P.K.; Burr, H.; Rugulies, R. Medically Unexplained Symptoms and the Risk of Loss of Labor Market Participation—A Prospective Study in the Danish Population. BMC Public Health 2015, 15, 844. [Google Scholar] [CrossRef]
- Amland, A.; Malterud, K.; Werner, E.L. Patients with Persistent Medically Unexplained Physical Symptoms: A Descriptive Study from Norwegian General Practice. BMC Fam. Pract. 2014, 15, 107. [Google Scholar] [CrossRef]
- Momsen, A.H.; Nielsen, C.V.; Nielsen, M.B.D.; Rugulies, R.; Jensen, C. Work Participation and Health-Related Characteristics of Sickness Absence Beneficiaries with Multiple Somatic Symptoms. Public Health 2016, 133, 75–82. [Google Scholar] [CrossRef]
- Barsky, A.J.; Orav, E.J.; Bates, D.W. Somatization Increases Medical Utilization and Costs Independent of Psychiatric and Medical Comorbidity. Arch. Gen. Psychiatry 2005, 62, 903. [Google Scholar] [CrossRef] [PubMed]
- Budtz-Lilly, A.; Vestergaard, M.; Fink, P.; Carlsen, A.H.; Rosendal, M. Patient Characteristics and Frequency of Bodily Distress Syndrome in Primary Care: A Cross-Sectional Study. Br. J. Gen. Pract. 2015, 65, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Konnopka, A.; Kaufmann, C.; König, H.-H.; Heider, D.; Wild, B.; Szecsenyi, J.; Herzog, W.; Heinrich, S.; Schaefert, R. Association of Costs with Somatic Symptom Severity in Patients with Medically Unexplained Symptoms. J. Psychosom. Res. 2013, 75, 370–375. [Google Scholar] [CrossRef]
- Castell, B.D.; Kazantzis, N.; Moss-Morris, R.E. Cognitive Behavioral Therapy and Graded Exercise for Chronic Fatigue Syndrome: A Meta-Analysis. Clin. Psychol. Sci. Pract. 2011, 18, 311–324. [Google Scholar] [CrossRef]
- Glombiewski, J.A.; Sawyer, A.T.; Gutermann, J.; Koenig, K.; Rief, W.; Hofmann, S.G. Psychological Treatments for Fibromyalgia: A Meta-Analysis. Pain 2010, 151, 280–295. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, B.; Burell, G.; Anderberg, U.-M.; Svärdsudd, K. Cognitive Behaviour Therapy in Women with Fibromyalgia: A Randomized Clinical Trial. Scand. J. Pain 2015, 9, 11–21. [Google Scholar] [CrossRef]
- Laird, K.T.; Tanner-Smith, E.E.; Russell, A.C.; Hollon, S.D.; Walker, L.S. Comparative Efficacy of Psychological Therapies for Improving Mental Health and Daily Functioning in Irritable Bowel Syndrome: A Systematic Review and Meta-Analysis. Clin. Psychol. Rev. 2017, 51, 142–152. [Google Scholar] [CrossRef]
- Ljótsson, B.; Hesser, H.; Andersson, E.; Lackner, J.M.; El Alaoui, S.; Falk, L.; Aspvall, K.; Fransson, J.; Hammarlund, K.; Löfström, A.; et al. Provoking Symptoms to Relieve Symptoms: A Randomized Controlled Dismantling Study of Exposure Therapy in Irritable Bowel Syndrome. Behav. Res. Ther. 2014, 55, 27–39. [Google Scholar] [CrossRef]
- Pike, A.; Hearn, L.; Williams, A.C. Effectiveness of Psychological Interventions for Chronic Pain on Health Care Use and Work Absence: Systematic Review and Meta-Analysis. Pain 2016, 157, 777–785. [Google Scholar] [CrossRef]
- White, P.; Goldsmith, K.; Johnson, A.; Potts, L.; Walwyn, R.; DeCesare, J.; Baber, H.; Burgess, M.; Clark, L.; Cox, D.; et al. Comparison of Adaptive Pacing Therapy, Cognitive Behaviour Therapy, Graded Exercise Therapy, and Specialist Medical Care for Chronic Fatigue Syndrome (PACE): A Randomised Trial. Lancet 2011, 377, 823–836. [Google Scholar] [CrossRef]
- Salkovskis, P.M. Psychological Treatment of Noncardiac Chest Pain: The Cognitive Approach. Am. J. Med. 1992, 92, 114S–121S. [Google Scholar] [CrossRef]
- Alberts, N.M.; Hadjistavropoulos, H.D.; Jones, S.L.; Sharpe, D. The Short Health Anxiety Inventory: A Systematic Review and Meta-Analysis. J. Anxiety Disord. 2013, 27, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Salkovskis, P.M. The Health Anxiety Inventory: Development and Validation of Scales for the Measurement of Health Anxiety and Hypochondriasis. Psychol. Med. 2002, 32, 843–853. [Google Scholar] [CrossRef]
- Viðarsson, J.V. Health Anxiety and Medically Unexplained Symptoms: Psychometric Properties of Two Translated Questionnaires. Master’s Thesis, Reykjavik University, Reykjavik, Iceland, 2016. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Pálsdóttir, V.E. The Validity of the Patient Health Questionnaire (PHQ) within Icelandic Primary Care. Cand. Psych. Thesis, University of Iceland, Reykjavík, Iceland, 2007. [Google Scholar]
- Kroenke, K.; Spitzer, R.L. The PHQ-9: A New Depression Diagnostic and Severity Measure. Psychiatr. Ann. 2002, 32, 509–515. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The Gad-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Ingólfsdóttir, R. Psychometric Properties of the Icelandic Version of the Generalized Anxiety Disorder-7; Háskólinn í: Reykjavík, Iceland, 2014. [Google Scholar]
- Ehring, T.; Zetsche, U.; Weidacker, K.; Wahl, K.; Schönfeld, S.; Ehlers, A. The Perseverative Thinking Questionnaire (PTQ): Validation of a Content-Independent Measure of Repetitive Negative Thinking. J. Behav. Ther. Exp. Psychiatry 2011, 42, 225–232. [Google Scholar] [CrossRef]
- Dimsdale, J.; Sharma, N.; Sharpe, M. What Do Physicians Think of Somatoform Disorders? Psychosomatics 2011, 52, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Wessely, S.; Nimnuan, C.; Sharpe, M. Functional Somatic Syndromes: One or Many? Lancet 1999, 354, 936–939. [Google Scholar] [CrossRef]
- Wessely; White, P.D. There Is Only One Functional Somatic Syndrome. Br. J. Psychiatry 2004, 185, 95–96. [Google Scholar] [CrossRef]
- Mourad, G.; Strömberg, A.; Johansson, P.; Jaarsma, T. Depressive Symptoms, Cardiac Anxiety, and Fear of Body Sensations in Patients with Non-Cardiac Chest Pain, and Their Relation to Healthcare-Seeking Behavior: A Cross-Sectional Study. Patient 2016, 9, 69–77. [Google Scholar] [CrossRef] [PubMed]
| Demographic Variables | NCCP Patients | NCCP Patients with Heart Related PPS | NCCP Patients without Heart Related PPS | χ2 |
|---|---|---|---|---|
| Gender | ||||
| Male | 154 (54.0%) | 48 (56.5%) | 106 (53.0%) | 0.29 |
| Female | 131 (46.0%) | 37 (43.5%) | 94 (47.0%) | |
| Education completed | ||||
| Primary school | 60 (21.8%) | 24 (28.9%) | 36 (18.8%) | 7.86 * |
| Secondary school | 102 (37.1%) | 35 (42.2%) | 67 (34.9%) | |
| University degree | 113 (41.1%) | 24 (28.9%) | 89 (46.4%) * | |
| Relationship status | ||||
| Single, separated or widowed | 66 (23.9%) | 26 (32.1%) | 40 (20.5%) * | 4.22 * |
| Married or cohabiting | 210 (76.1) | 55 (67.9%) | 155 (79.5%) * | |
| M (SD) | M (SD) | M (SD) | T | |
| Age | 49.84 (10.68) | 48.07 (12.66) | 50.60 (9.65) | 1.646 |
| Measure | All NCCP Patients | Heart-Related PPS Criteria Met | Heart-Related PPS Criteria Not Met | Significance | Effect Size |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | χ2 | OR | |
| Inactivity | 27 (10.1%) | 14 (18.2%) | 13 (6.8%) | 7.751 * | 3.03 |
| Inability to work | 22 (8.2%) | 11 (14.3%) | 11 (5.8%) | 5.231 * | 2.71 |
| SHAI ≥18 | 17 (6.2%) | 10 (12.2%) | 7 (3.6%) | 7.217 * | 3.67 |
| GAD-7 ≥10 | 40 (14.4) | 17 (20.7%) | 23 (11.8%) | 3.732 | 1.96 |
| PHQ-9 ≥10 | 47 (17.0%) | 29 (34.9%) | 18 (9.3%) | 26.949 * | 5.22 |
| M (SD) | M (SD) | M (SD) | t | r | |
| SHAI Mean (SD) | 8.79 (5.52) | 10.88 (6.83) | 7.90 (4.60) | −3.615 * | 0.32 |
| GAD-7 Mean (SD) | 4.70 (5.02) | 6.77 (5.81) | 3.83 (4.38) | −4.112 * | 0.35 |
| PHQ-9 Mean (SD) | 6.50 (3.98) | 8.47 (4.57) | 5.65 (3.38) | −5.059 * | 0.42 |
| PTQ Mean (SD) | 14.54 (12.44) | 18.68 (13.68) | 12.78 (11.46) | −3.427 * | 0.29 |
| Total number of non-heart-related PPS | 1.31 (1.46) | 2.41 (1.55) | 0.84 (1.13) | −8.493 * | 0.61 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flóvenz, S.Ó.; Salkovskis, P.; Svansdóttir, E.; Karlsson, H.D.; Andersen, K.; Sigurðsson, J.F. Non-Cardiac Chest Pain as a Persistent Physical Symptom: Psychological Distress and Workability. Int. J. Environ. Res. Public Health 2023, 20, 2521. https://doi.org/10.3390/ijerph20032521
Flóvenz SÓ, Salkovskis P, Svansdóttir E, Karlsson HD, Andersen K, Sigurðsson JF. Non-Cardiac Chest Pain as a Persistent Physical Symptom: Psychological Distress and Workability. International Journal of Environmental Research and Public Health. 2023; 20(3):2521. https://doi.org/10.3390/ijerph20032521
Chicago/Turabian StyleFlóvenz, Sigrún Ólafsdóttir, Paul Salkovskis, Erla Svansdóttir, Hróbjartur Darri Karlsson, Karl Andersen, and Jón Friðrik Sigurðsson. 2023. "Non-Cardiac Chest Pain as a Persistent Physical Symptom: Psychological Distress and Workability" International Journal of Environmental Research and Public Health 20, no. 3: 2521. https://doi.org/10.3390/ijerph20032521
APA StyleFlóvenz, S. Ó., Salkovskis, P., Svansdóttir, E., Karlsson, H. D., Andersen, K., & Sigurðsson, J. F. (2023). Non-Cardiac Chest Pain as a Persistent Physical Symptom: Psychological Distress and Workability. International Journal of Environmental Research and Public Health, 20(3), 2521. https://doi.org/10.3390/ijerph20032521







